Abstract
Laparoscopic adjustable gastric banding (LAGB) is a bariatric procedure that was introduced in the early 1990s and offers a minimally invasive and reversible option for weight loss. Initially popular due to its simplicity and effectiveness, LAGB’s long-term success has been limited by complications such as port-site infection, pouch dilatation, and gastric band erosion. Herein, we describe a rare case of gastric band erosion found incidentally during endoscopy a decade after placement. The eroded band was successfully removed using a combined endoscopic and laparoscopic approach.
Keywords: laparoscopic gastric banding, gastric band erosion, bariatric surgery, weight loss, endoscopy
Introduction
Laparoscopic adjustable gastric banding (LAGB) was once a popular bariatric surgery option for individuals with extreme obesity. Its use rapidly declined around 2008 due to complication rates and the availability of better alternatives, such as sleeve gastrectomy.1-4 In 2020, LAGB was estimated to account for 1.2% of all bariatric surgeries in the United States of America, down from 35.4% observed in 2011.1,2 This minimally invasive procedure involves placing an adjustable silicone band around the upper portion of the stomach to restrict the amount of food ingested, thereby promoting progressive weight loss through early satiety.2,4
While LAGB offers several advantages, including reversibility and adjustability, it is not without complications. 5 Some of these include port-site infection, chronic abdominal pain, gastroesophageal reflux disease (GERD), gastric ulceration, band slippage, fluid leakage, pouch dilatation, and erosion of the band into the viscera.5-9 Gastric band erosion beyond 10 years after placement is infrequent, with a handful of cases reported to date. 1 Herein, we present a unique case of gastric band erosion discovered incidentally during endoscopy, 12 years after placement.
Case Summary
A 50-year-old female with a medical history of hypertension, iron-deficiency anemia, and GERD presented to our ambulatory surgical center for colorectal cancer screening. The patient had no prior colonoscopy and denied constipation, melena, hematochezia, excess flatulence, recent weight loss, or a family history of colorectal cancer. She also denied nausea, vomiting, acid reflux, dysphagia, odynophagia, or abdominal pain. Her surgical history was significant for LAGB at the age of 38 years due to morbid obesity. The vital signs were within the normal ranges, and the patient appeared comfortable. The abdomen was soft, obese, and non-tender and had no signs of trauma, palpable masses, or organomegaly. Preadmission tests were significant for a hemoglobin of 12.5 g/dL with a mean corpuscular volume (MCV) of 90.9 fL and a platelet count of 255 K/mm3. The home medications included ferrous sulfate 325 mg daily, pantoprazole 40 mg daily, and lisinopril 10 mg daily.
Colonoscopy showed one 4-mm polyp in the ascending colon, which was removed with cold biopsy forceps, and the histopathology revealed tubular adenoma. Esophagogastroduodenoscopy (EGD) showed a moderate Schatzki ring in the mid-esophagus, an adjustable gastric band eroding into the gastric fundus, and focal inflammation in the gastric body and gastric antrum (Figure 1). A computed tomography (CT) of the abdomen and pelvis with oral and intravenous contrast showed a small localized air pocket around the gastric band ligation consistent with the gastric band erosion noted on EGD. There was no evidence of localized abscess. The patient underwent a repeat EGD the next day with partial removal of the laparoscopic band. The isolated portion of the gastric band was grabbed using a Roth net retriever – 360 (STERIS Healthcare) and withdrawn with the scope through the mouth (Figure 2). This procedure was followed by laparoscopic transgastric removal of the remaining portion of the gastric band, partial gastrectomy, and intraoperative EGD.
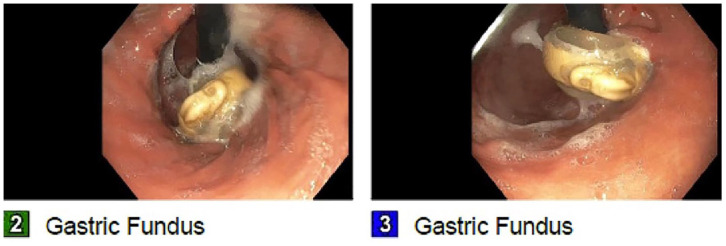
Figure 1.
Endoscopic images showing a moderate Schatzki ring and an adjustable gastric band eroding into the gastric fundus.
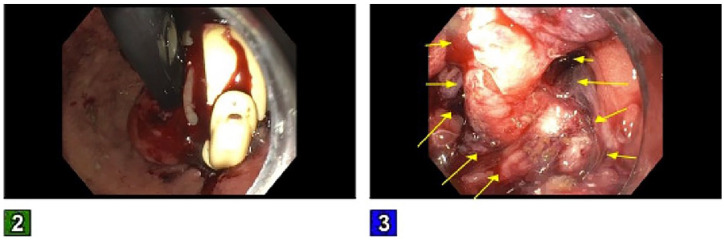
Figure 2.
Endoscopic images showing an eroded gastric band, which was partially removed endoscopically. There was edema, erosion, and inflammation at the cardia (yellow arrows); however, there was no overt luminal discontinuity.
A postoperative abdominal x-ray series was negative for extravasation from the stomach. The patient’s hemoglobin level remained stable during her admission and was discharged with a short course of amoxicillin–clavulanic acid. Two weeks after discharge, the patient was seen in our gastroenterology clinic and had no acute complaints.
Discussion
LAGB is a less-invasive bariatric procedure, with a lower risk of perioperative complications. However, long-term complications can occur, including band slippage, port-related problems, subphrenic abscesses, gastrointestinal bleeding, and band erosion.10,11 Gastric band erosion or band migration is a unique complication of LAGB, marked by the slow penetration of the band into the gastric lumen. This condition can remain silent for an extended period, often discovered incidentally during routine endoscopy. 12 The silent nature of this complication underscores the importance of regular follow-up and monitoring in patients who have undergone this procedure. 7 To date, there are no standardized guidelines for post-LABG monitoring in asymptomatic patients. 1
With an estimated incidence of 1.5% to 3.4%, band migration can occur from just a few months to years after placement, with a peak incidence observed within 2 years after the procedure.1,6,13 Few cases have been reported whereby gastric band erosion occurred after the 10-year mark. 1 The etiopathogenesis of gastric band erosion remains unclear, and it is postulated to be a multifactorial process. Band migration is thought to arise from a combination of mechanical stress, ischemia, and inflammation.1,3,4,8,10,12,14 Early on, erosion may be triggered by accidental injury to the gastric wall or small perforations due to infections. Over time, sustained pressure on the wall can lead to ischemia, or the body may react to the band as a foreign object, both of which can result in the formation of scar tissue and erosion of the gastric wall.
Gastric band migration can be asymptomatic and an incidental finding during routine endoscopy,12,15 like in our case. Some patients, however, may present with severe acid reflux, nausea, vomiting, acute dysphagia, early satiety, abdominal pain, or weight regain.2,6,13 Band erosion can be complicated by gastric perforation, bleeding, abscess formation, and migration of the band to other parts of the gastrointestinal tract.11,16 The gastric band is typically removed using an endoscopic, laparoscopic, or combined laparoscopic and endoscopic approach and, in extreme cases, via open laparotomy.5,6,16,17 In our case, the patient required a hybrid approach due to incomplete erosion of the band through the gastric tissue.
Conclusion
In summary, gastric band erosion is a rare and unique complication of LAGB that can be found incidentally during routine endoscopy in asymptomatic patients. This condition warrants prompt endoscopic or laparoscopic intervention to prevent distal migration and its associated complications. Guidelines for post-LABG surveillance in asymptomatic patients are needed to prevent life-threatening complications such as band migration.
Footnotes
Author Contributions: LB conceptualized the idea of this case report and crafted an outline. TV, RB, AK, and RY assisted with data curation, collection of pertinent patient information, and writing of the manuscript. KA and YC edited and proofread the final version of this case report.
Data Availability Statement: Further inquiries can be directed to the corresponding author.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics Approval: Our institution does not require IRB approval/waiver for case reports.
Informed Consent: Verbal informed consent was obtained from the patient for her anonymized information to be published in this article.
ORCID iD: Lefika Bathobakae  https://orcid.org/0000-0002-2772-6085
https://orcid.org/0000-0002-2772-6085
References
- 1. Makovich Z, Patel B. Late-onset gastric band erosion following heavy nonsteroidal anti-inflammatory drug use. ACG Case Rep J. 2024;11(4):e01343. doi: 10.14309/crj.0000000000001343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Faust TF, Schnittka E, Steadman MB, Cail GM, Rice BS. Management of laparoscopic adjustable gastric band erosion: a case report. Cureus. 2023;15(10):e47718. doi: 10.7759/cureus.47718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wong V, Choi C, Qiu H, Kaye A, Wang W. A rare case of an incidental near-complete gastric band erosion without perforation. Cureus. 2022;14(6):e25636. doi: 10.7759/cureus.25636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hota P, Caroline D, Gupta S, Agosto O. Laparoscopic adjustable gastric band erosion with intragastric band migration: a rare but serious complication. Radiol Case Rep. 2018;13(1):76-80. doi: 10.1016/j.radcr.2017.11.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Yoon CI, Pak KH, Kim SM. Early experience with diagnosis and management of eroded gastric bands. J Korean Surg Soc. 2012;82(1):18-27. doi: 10.4174/jkss.2012.82.1.18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Corvini M, Kang E, Weidner G, et al. Laparoscopic adjustable gastric band erosion into the stomach and colon. J Am Osteopath Assoc. 2018;118(7):479-481. doi: 10.7556/jaoa.2018.102 [DOI] [PubMed] [Google Scholar]
- 7. Hurley CM, Hechtl D, Ng KC, McHugh J, Sehgal R, Regan MC. Biofilm-sealed perforation of the gastric body: a rare sequela of gastric band erosion. J Surg Case Rep. 2019;2019(9):1-3. doi: 10.1093/jscr/rjz263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Spitali C, De Vogelaere K, Delvaux G. Removal of eroded gastric bands using a transgastric SILS device. Case Rep Surg. 2013;2013:1-3. doi: 10.1155/2013/852747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Petridis C, Neofytou K, Petrou A, et al. Acute appendicitis as a rare complication of gastric band. J Surg Case Rep. 2013;2013(10):1-2. doi: 10.1093/jscr/rjt084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Downes E, Baker K, Buicko JL, et al. Case report hematemesis from a left gastric artery pseudoaneurysm secondary to an adjustable laparoscopic gastric band. J Curr Surg. 2014;4(3):95-98. doi: 10.4021/jcs234w [DOI] [Google Scholar]
- 11. Evans G, Eagon JC, Kushnir V. Sengstaken-Blakemore tube as a rescue treatment for hemorrhagic shock secondary to laparoscopic adjustable gastric banding erosion. ACG Case Rep J. 2019;6(12):e00296. doi: 10.14309/crj.0000000000000296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Yun GY, Kim WS, Kim HJ, et al. Asymptomatic gastric band erosion detected during routine gastroduodenoscopy. Clin Endosc. 2016;49(3):294-297. doi: 10.5946/ce.2016.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Felinski M, Bajwa KS, Shah SK. Erosion of gastric band tubing presenting as port-site cellulitis. CRSLS. 2017;21(3):1-5. doi: 10.4293/crsls.2017.00022 [DOI] [Google Scholar]
- 14. Iacopini F, Di Lorenzo N, Altorio F, et al. Over-the-scope clip closure of two chronic fistulas after gastric band penetration. World J Gastroenterol. 2010;16(13):1665-1669. doi: 10.3748/wjg.v16.i13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. AlHabib R, Kayali N, Al Rashed A, et al. The silent band: not loud enough? asymptomatic gastric band erosion: a case report. J Surg. 2022;10(1):1-4. doi: 10.13188/2332-4139.1000051 [DOI] [Google Scholar]
- 16. Abeysekera A, Lee J, Ghosh S, et al. Migration of eroded laparoscopic adjustable gastric band causing small bowel obstruction and perforation. BMJ Case Rep. 2017;2017:1-3. doi: 10.1136/bcr-2017-219954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Deshmukh A, Desai PM, Ma C, et al. Endoscopic management of gastric band erosion: a systematic review and meta-analysis. Obes Surg. 2024;34(2):494-502. doi: 10.1007/s11695-023-06995-4 [DOI] [PubMed] [Google Scholar]