Abstract
Dentin dysplasia (DD) is a rare clinical entity that can affect deciduous dentition alone, or both deciduous and permanent dentition. It is a developmental disorder that can be classified as DD type I or type II. This case report describes a rare case of DD type I in a 19-year-old patient, highlighting the clinical presentation and the radiographic features of the condition, confirmed by ground sectioning and microscopic examination of extracted teeth. The case report also describes the management of this patient using zygoma and endosteal implants.
Keywords: atypical dentin, implant, rootless teeth, permanent dentition, dentin dysplasia
Introduction
Chamberlain was the first person to describe the absence of root formation in teeth and coined the term "rootless teeth" [1]. Dentin dysplasia (DD) is a hereditary developmental anomaly of defective dentin formation. It is further subclassified into DD type I and type II [2]. The type I variant of DD typically affects root formation, with a normal-appearing crown. DD type II has similar clinical features to dentinogenesis imperfecta. In contrast to the type I variant, root formation is unaffected in DD type II [2,3]. The simultaneous presence of both subtypes has also been reported in the literature [4]. The defective root formation in DD type I causes mobility of teeth and may lead to premature exfoliation. In this case report, we describe the case of a 19-year-old male patient who presented with the above condition at our Outpatient Department (OPD).
Case presentation
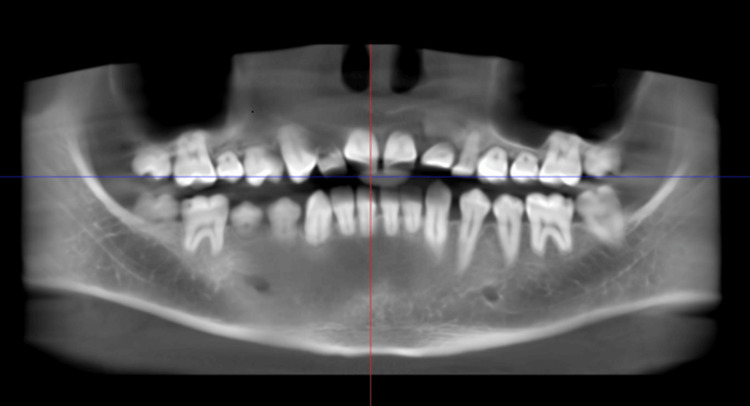
A 19-year-old male patient reported to the Oral and Maxillofacial Surgery OPD with a complaint of generalized teeth mobility. The patient did not provide any relevant medical or family history. After examining the patient, a provisional diagnosis of juvenile periodontitis was made. However, upon evaluating the orthopantomogram (OPG), a rudimentary or complete absence of root formation was noted in all the teeth, with no evidence of bone loss. Hence, a developmental disorder was suspected as the cause of the rootless teeth. Based on these findings, a diagnosis of DD was made. To rule out the possibility of any associated syndrome, the patient was advised to undergo serum alkaline phosphatase and calcium testing, as well as a full-mouth cone-beam computed tomography (CBCT). The patient’s blood investigation reports were within normal limits (Figures 1-3).
Figure 1. Right-sided preoperative occlusion of the patient.
Image credit: Dr. Gauri Sharma
Figure 2. Left-sided preoperative occlusion of the patient.
Image credit: Dr. Gauri Sharma
Figure 3. CBCT of the patient showing generalized shortening of roots with normal crowns, which is consistent with dentin dysplasia.
Image credit: Dr. Gauri Sharma
CBCT: Cone-beam computed tomography
The surgical team advised the patient to undergo the extraction of all teeth, followed by rehabilitation via an implant-supported prosthesis. The treatment plan consisted of placing two pterygoid/zygoma implants, three to four endosteal implants in the maxillary arch, and eight endosteal implants in the mandibular arch, with delayed loading.
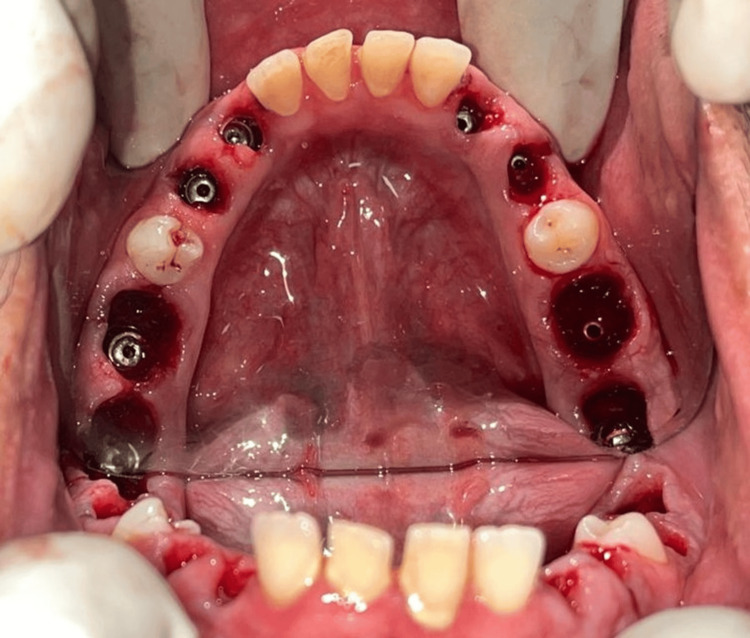
The placement of eight immediate mandibular implants was done first, and the surgery was uneventful. The patient was recalled after five days for the placement of implants in the maxillary arch (Figure 4).
Figure 4. Intraoperative view of eight endosteal implants placed in the mandibular arch.
All the mandibular teeth were extracted after the implant placements.
Image credit: Dr. Ankita Pathak
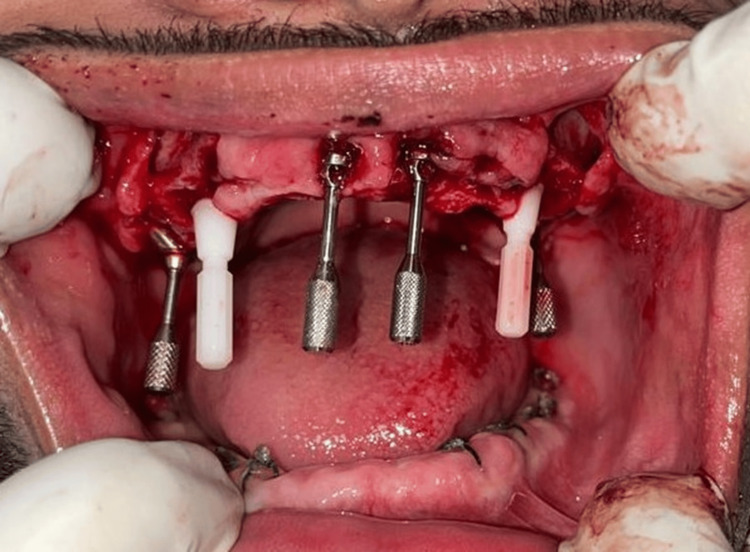
The implant surgery for the upper arch was initiated by placing a pterygoid implant in the right quadrant. However, the implant failed to engage with adequate torque. Therefore, the decision was made to use zygoma implants instead of pterygoid implants. Two zygoma implants, along with four endosteal implants in the canine-premolar region, were placed. The patient was recalled after seven days for suture removal and review. Meanwhile, the patient was prescribed calcium and vitamin D3 tablets once a week for 12 weeks (Figures 5-6).
Figure 5. Intraoperative view of the maxillary arch of the patient showing two zygoma implants and four endosteal implants.
Image credit: Dr. Ankita Pathak
Figure 6. Extracted teeth of the patient showing the abnormal anatomical pattern of the roots.
Image credit: Dr. Ankita Pathak
The second stage of implant surgery was performed after four months. The post-operative X-rays showed good adaptation and osseointegration of all the implants with the bone. The patient was recalled after seven days for suture removal and prosthesis placement (Figures 7-8).
Figure 7. Postoperative PNS X-ray of the patient.
Image credit: Dr. Bhushan Mundada
PNS: Paranasal sinus
Figure 8. Postoperative OPG of the patient.
Image credit: Dr. Bhushan Mundada
OPG: Orthopantomogram
Discussion
DD is a rare clinical entity that has an incidence of 1 in 100,000 live births [5]. It can be associated with other systemic conditions, such as skeletal sclerosis, Ehler-Danlos syndrome, and Brachio-Skeleto-Genital syndrome [6-8]. Differential diagnosis of DD includes other developmental anomalies of dentin formation, such as dentinogenetic imperfecta and regional odontodysplasia [9]. The exact pathophysiology of DD remains largely unknown. The difficulty in diagnosing DD can be due to its low incidence rate [5] and a lack of previous clinical experience, which may lead to a delay in reaching a correct diagnosis.
The management of DD is case-based, and the age of the patient seems to be a key influential factor. When diagnosed earlier, the treatment strategies are directed toward the retention of teeth for as long as possible. Akhil Jose et al. managed DD in 11-year-old patients symptomatically, using restorations for small caries and extraction of only the unrestorable teeth. They advocate preventive measures, such as oral prophylaxis, to control tooth mobility and intercept premature exfoliation. They suggest definitive management in the form of implant-supported prostheses after a patient is 18 years of age [2].
Implant-supported rehabilitation of patients with DD has been previously attempted [3,10-12]. The use of sinus lift procedures to counteract bone loss in the maxillary arch has been a time-tested method [3,10,11]. In contrast with this approach, we placed bilateral zygoma implants, which negated the need for sinus lift surgery. This greatly reduced the operating time, overall discomfort for the patient, and engagement in good cortical bone, with a minimum chance of resorption in the post-operative phase. To the best of our knowledge, this is the first case in which sinus lift surgery has not been performed in favor of zygoma implants in a patient with DD.
Due to reduced masticatory forces, bone resorption is frequently encountered in DD cases. Consequently, implant osseointegration and its success rate become unpredictable. To achieve optimal bony support, iliac bone grafting has been performed either in the lower arch or in both arches in the past. Additional measures, such as xenograft placement and platelet-rich plasma (PRP), have been tried to aid in the preservation of grafts and accelerate new bone formation [10,11]. We did not perform bone grafting, as the patient had adequate bone height, while the efficacy of PRP in accelerating bone formation is still debatable.
In the present case, all the implants showed good osteointegration, after four months of placement.
Conclusions
The treatment of patients with DD depends on the age of the patient and the clinical severity of the disease. Adequate oral hygiene maintenance and dietary supplementation must be established and maintained for the retention of teeth to help children keep their natural teeth for as long as possible. In patients who have attained complete tooth eruption and skeletal maturity, oral rehabilitation must be planned to ensure proper quality of life and psychological well-being. Implant-supported rehabilitation preceded by sinus lift surgeries has been attempted in the past. The novel strategy of placing zygoma implants, which eliminates the need for sinus lift procedures, has been utilized for the initial instance in a patient with DD. This is a promising approach for the management of such patients and holds potential for further evaluation in the future.
Disclosures
Human subjects: Consent was obtained or waived by all participants in this study.
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following:
Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work.
Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
Author Contributions
Concept and design: Gauri Sharma, Bhushan Mundada, Rozina Vishnani, Deepankar Shukla, Ankita Pathak
Acquisition, analysis, or interpretation of data: Gauri Sharma, Bhushan Mundada, Rozina Vishnani, Nitin Bhola, Deepankar Shukla, Ankita Pathak
Drafting of the manuscript: Gauri Sharma, Bhushan Mundada, Rozina Vishnani, Ankita Pathak
Critical review of the manuscript for important intellectual content: Gauri Sharma, Bhushan Mundada, Rozina Vishnani, Nitin Bhola, Deepankar Shukla, Ankita Pathak
Supervision: Bhushan Mundada, Rozina Vishnani, Nitin Bhola, Deepankar Shukla
References
- 1.Management of dentin dysplasia and facial disharmony. Chamberlain BB, Hayward JR. https://doi.org/10.1111/j.1754-4505.1983.tb01615.x. Spec Care Dentist. 1983;3:113–116. doi: 10.1111/j.1754-4505.1983.tb01615.x. [DOI] [PubMed] [Google Scholar]
- 2.Dentin dysplasia type I: a rare case report. Akhil Jose EJ, Palathingal P, Baby D, Thachil JM. J Oral Maxillofac Pathol. 2019;23:309. doi: 10.4103/jomfp.JOMFP_132_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reviving a smile: a multidisciplinary approach to dentin dysplasia. Kr AV, Raja K, Krishnan RK, Vijayakumar P, Kalaimani AP. Cureus. 2024;16:0. doi: 10.7759/cureus.59697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Radiographic manifestations of an unusual combination type I and type II dentin dysplasia. Ciola B, Bahn SL, Goviea GL. Oral Surg Oral Med Oral Pathol. 1978;3:17–22. doi: 10.1016/0030-4220(78)90101-9. [DOI] [PubMed] [Google Scholar]
- 5.Dentin dysplasia type I - a rare entity. Malik S, Gupta S, Wadhwan V, Suhasini GP. J Oral Maxillofac Pathol. 2015;19:110. doi: 10.4103/0973-029X.157220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dentine dysplasia with sclerotic bone and skeletal anomalies inherited as an autosomal dominant trait. Morris ME, Augsburger RH. Oral Surg Oral Med Oral Pathol. 1977;2:67–83. doi: 10.1016/0030-4220(77)90163-3. [DOI] [PubMed] [Google Scholar]
- 7.The Ehlers-Danlos syndrome. Abnormalities of the enamel, dentine, cementum and the dental pulp: an histological examination of 13 teeth from 6 patients. Barabas GM. https://pubmed.ncbi.nlm.nih.gov/5255791/ Br Dent J. 1969;126:509–515. [PubMed] [Google Scholar]
- 8.The branchio-skeleto-genital syndrome. A new hereditary syndrome. el-Sahy NI, Waters WR. Plast Reconstr Surg. 1971;48:542–550. doi: 10.1097/00006534-197112000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Rootless teeth: dentin dysplasia type I. Fulari SG, Tambake DP. Contemp Clin Dent. 2013;4:520–522. doi: 10.4103/0976-237X.123063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dentin dysplasia type I: a challenge for treatment with dental implants. Depprich RA, Ommerborn MA, Handschel JG, Naujoks CD, Meyer U, Kübler NR. Head Face Med. 2007;3:31. doi: 10.1186/1746-160X-3-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dentin dysplasia type I treated with onlay bone grafting, sinus augmentation, and osseointegrated implants. Muñoz-Guerra MF, Naval-Gías L, Escorial V, Sastre-Pérez J. Implant Dent. 2006;15:248–253. doi: 10.1097/01.id.0000234638.60877.1b. [DOI] [PubMed] [Google Scholar]
- 12.Dentin dysplasia type I—report of a case treated with dental implants. Sekerci AE, Sahman H, Etoz OA, Gumus HO, Albayrak H, Nazlim S, Sisman Y. Indian J Dent. 2011;2:160–164. [Google Scholar]