Abstract
Introduction
Previous studies have predominantly explored the relationship of the glymphatic system with motor symptoms in Parkinson’s disease (PD); however, research on non-motor symptoms remains limited. Therefore, this study investigated the association between glymphatic function and non-motor symptoms, including cognitive impairment and sleep disorders, in PD patients.
Methods
This study recruited 49 PD patients and 38 healthy controls (HC). Glymphatic function was evaluated using enlarged perivascular spaces (EPVS) in the basal ganglia (BG) region and diffusion tensor image analysis along the perivascular space (DTI-ALPS) index. Cognition, sleep, anxiety, and depression scales were assessed in all participants. According to the scale scores, PD patients were further divided into several groups to identify the presence of non-motor symptoms. Differences in EPVS numbers and ALPS index between PD subgroups and HC group were compared. Spearman correlation analysis was performed to investigate the association between the PD non-motor symptoms and ALPS index. Additionally, receiver operating characteristic (ROC) curves analysis was conducted for ALPS index to predict cognitive impairment and insomnia in PD patients.
Results
PD patients with and without non-motor symptoms all showed more EPVS numbers than the controls, and the EPVS numbers in PD patients with cognitive impairment were also greater than those without. Notably, except for the depression subgroup, PD patients with non-motor symptoms showed significantly lower ALPS index than the controls. The Montreal Cognitive Assessment (MoCA) scores were positively correlated, whereas the Parkinson’s Disease Sleep Scale (PDSS)-2 and REM Sleep Behavior Disorder Screening Questionnaire (RBDSQ) scores were negatively correlated with the ALPS index in PD patients (r=0.3618, P=0.0053; r=−0.4146, P=0.0015; r=−0.2655, P=0.0326, respectively). The ALPS index proved to be predictive of cognitive impairment and insomnia in PD patients (AUC=0.7733, P=0.001; AUC=0.7993, P=0.0004, respectively).
Conclusion
Glymphatic function is closely associated with cognition and sleep of PD patients.
Keywords: glymphatic system, parkinson’s disease, non-motor symptoms, cognition, sleep
Introduction
As the population ages, the incidence of Parkinson’s disease (PD) continues to rise, making it a highly prevalent neurodegenerative disease. The clinical manifestations of PD encompass motor and non-motor symptoms. Motor symptoms include static tremors, bradykinesia, muscle rigidity, and gait abnormalities, while non-motor symptoms involve sleep disorders, cognitive impairment, anxiety, depression, and hyposmia.1–5 Although motor symptoms of PD have been extensively investigated, data on non-motor symptoms are limited. However, non-motor symptoms are prevalent among PD patients, often manifesting at any stage of the disease, sometimes even before the onset of motor symptoms.6 Among these, cognitive impairment, sleep disorders, anxiety, and depression substantially impact patients’ quality of life, exacerbating prognosis and placing substantial burdens on both families and society.
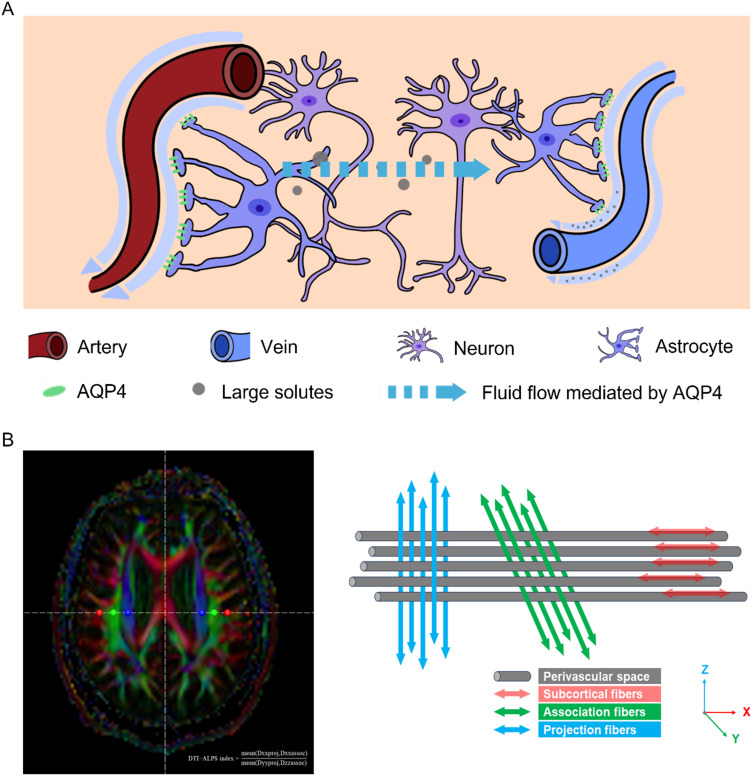
The pathogenesis of PD primarily involves the misfolding of α-synuclein (a-syn), leading to the formation of Lewy bodies.7 However, the glymphatic system is involved in clearing metabolic waste and pathogenic proteins such as a-syn and β-amyloid (Aβ) from the brain.8 The glymphatic system was first proposed in 2012 by Iliff et al,9 delineating its role in facilitating cerebrospinal fluid influx from the subarachnoid space into the brain parenchyma along periarterial spaces, mediated by aquaporin-4 (AQP4) in astrocyte end-feet, followed by fluid exchange with cerebral interstitial fluid, and eventual discharge through perivenous spaces (Figure 1A). In terms of both structure and function, the perivascular space (PVS) serves as a crucial pathway within the glymphatic system.9,10 The widening of PVS is possibly caused by obstruction of metabolic waste such as a-syn, perivascular inflammation due to macrophages, and increased arterial stiffness, and leads to weakened arterial pulsation and ultimately impairs the glymphatic clearance.11–14 Recent advancements in non-invasive functional magnetic resonance imaging (fMRI), particularly diffusion tensor image analysis along the perivascular space (DTI-ALPS), have enabled the study of glymphatic function in various diseases such as Alzheimer’s disease,15 and PD.16
Figure 1.
Schematic diagram of the glymphatic system and DTI-ALPS methodology. (A) As described in the introduction section, the glymphatic system drives the bulk fluid flow from periarterial spaces to perivenous spaces to clear large solutes. (B) On the left, colored FA map shows ROIs on the subcortical fibers (red), association fibers (green), and projection fibers (blue) in bilateral hemispheres. On the right, the spatial relationships among the perivascular space, subcortical fibers (red; x-axis), association fibers (green; y-axis), and projection fibers (blue; z-axis) are showed. The formula of the DTI-ALPS index is showed on the left side.
Similarly, despite the growing body of research on the glymphatic system and PD, investigations have predominantly focused on motor symptoms, with limited exploration of non-motor symptoms. We previously reported a correlation between the glymphatic system and motor symptoms in PD patients but did not specifically investigate non-motor symptoms, and we also found that the increase in numbers of enlarged perivascular spaces (EPVS) was most pronounced in the basal ganglia (BG) region in PD patients.17 Some studies have found that cognitive decline18 as well as sleep disorders19 are all associated with glymphatic function. Wang et al also demonstrated a predictive relationship between glymphatic function and cognitive impairment in chronic insomnia patients.20 Pang et al showed that glymphatic function could potentially predict conversion from mild cognitive impairment to dementia in PD patients.21 Interestingly, Gnarra et al found that maintaining the lateral head position during the crucial sleep stages is beneficial for improving the glymphatic function in PD patients.22 Yue et al indicated the interplay between the glymphatic system and neurotoxic proteins in PD and related disorders.23 The accumulation of a-syn within the different brain regions due to glymphatic dysfunction may cause different PD non-motor symptoms. For instance, the increased deposition of a-syn and Aβ in the brain cortex or hippocampus is possibly associated with cognitive decline in PD. Therefore, we hypothesize and validate that non-motor symptoms such as cognitive impairment and sleep disorders in PD patients may also correlate with glymphatic function. This study aims to combine the BG-EPVS numbers and ALPS index to explore the relationship between glymphatic function and common non-motor symptoms in PD, including cognitive impairment, sleep disorders, anxiety, and depression. Our findings may provide novel insights into the relationship between glymphatic function and PD symptoms.
Materials and Methods
Study Participants
From November 2021 to September 2022, we recruited 49 PD patients who met the UK Brain Bank PD diagnostic criteria and collected information on patients’ age, sex, history of smoking and drinking, disease duration, types and doses of anti-Parkinson’s medications, Hoehn and Yahr (H-Y) staging, and the Unified Parkinson’s Disease Rating Scale (UPDRS) II, III scale score. While some patients were hospitalized, the majority were recruited either via telephone or outpatient visits. All the patients recruited by different pathways need to meet the inclusion and exclusion criteria. Furthermore, all the PD patients were enrolled continuously in the time frame. During the same period, healthy controls (HC) were recruited from the health checkups in outpatient clinic. We ultimately included 38 age- and sex- matched individuals continuously. The exclusion criteria were as follows: participants with (1) severe cognitive impairment or psychiatric abnormalities that prevent the completion of all assessment scales; (2) conditions such as stroke, traumatic brain injury, or Alzheimer’s disease that may affect glymphatic function; (3) Parkinson’s syndrome, such as vascular Parkinsonism and drug-induced Parkinsonism; (4) Parkinson’s superposition syndrome, such as multiple system atrophy and progressive supranuclear palsy; (5) contraindications for cranial MRI examinations; and (6) incomplete data. This study was conducted according to the Declaration of Helsinki. In addition, our study was approved by the Ethics Committee of the Affiliated Suzhou Hospital of Nanjing Medical University (Ethics Approval Number: K-2021-071-K01), and written informed consent was obtained from all participants.
Clinical Evaluation
An experienced neurologist, blinded to participants’ clinical information, conducted specialized assessments on all PD patients. The H-Y staging was used to assess the disease status, whereas the UPDRS II and III scores were used to evaluate daily living abilities and motor function. Patients abstained from anti-Parkinson’s medications for at least 12 hours before assessment to ensure that they were in the “off” state. Two additional trained neurologists, also blinded to clinical data, conducted neuropsychological and sleep assessments on all participants. Based on internationally recognized criteria and previous studies,24–27 patients were further divided into groups to identify the presence of non-motor symptoms. The specific details are as follows: (1) Cognitive function was assessed using the Montreal Cognitive Assessment (MoCA) scale, with scores ≥26 indicating normal cognition (PD-NC group) and scores <26 indicating cognitive impairment (PD-CI group). (2) Nighttime sleep quality was assessed using the Parkinson’s Disease Sleep Scale-2 (PDSS-2), with scores <15 indicating absence of insomnia (PD-NI group) and scores ≥15 indicating presence of insomnia (PD-I group). (3) Daytime sleepiness was assessed using the Epworth Sleepiness Scale (ESS), with scores <10 indicating absence of excessive daytime sleepiness (PD-NEDS group) and scores ≥10 indicating presence of excessive daytime sleepiness (PD-EDS group). (4) Rapid eye movement sleep behavior disorders (RBD) were assessed using the REM Sleep Behavior Disorder Screening Questionnaire (RBDSQ), with scores <5 indicating absence of RBD (PD-NRBD group) and scores ≥5 indicating presence of RBD (PD-RBD group). (5) Anxiety was assessed using the Hamilton Anxiety Rating Scale (HAMA), with scores <14 indicating absence of anxiety (PD-NA group) and scores ≥14 indicating presence of anxiety (PD-A group). (6) Depression was assessed using the Hamilton Depression Rating Scale-17 (HAMD-17), with scores <17 indicating absence of depression (PD-ND group) and scores ≥17 indicating presence of depression (PD-D group).
MRI
PD patients refrained from anti-Parkinson’s medications for at least 12 hours prior to MRI examination. MRI scans were obtained for all participants using the 3.0 T Siemens Skyra instrument equipped with a 20-channel head coil. Participants’ heads were immobilized using a foam pillow, and they were instructed to relax, and close their eyes during the scan. Vital signs including respiration rate, pulse rate, and blood pressure were recorded for all participants before the examination. The imaging parameters were: A 3D T1 magnetization-prepared rapid gradient echo sequence (T1-MPRAGE): repetition time (TR)/ echo time (TE)=2300 ms/2.98 ms, field of view (FOV)=256 × 256 mm2, slice thickness=1.1 mm, and slice gap=0 mm; DTI (b=1000 s/mm2, b=2000 s/mm2): TR/ TE =6600 ms/94 ms, FOV=230 × 230 mm2, voxel size=1.9 × 1.9×5.0 mm3, slice thickness=5 mm with no slice gap, 30 diffusion directions, and bandwidth=1576 Hz/Px; T1WI: TR/ TE =2000 ms/9 ms, FOV=220 × 220 mm2, and slice thickness=5 mm; T2WI: TR/ TE =3800 ms/99 ms, FOV=220 × 220 mm2, and slice thickness=5 mm; FLAIR: TR/ TE =8000 ms/81 ms, FOV=220 × 220 mm2, and slice thickness=5 mm.
The assessment of EPVS was performed by a trained radiologist who was blinded to the clinical information. EPVS are fluid cavities that surround the cerebral blood vessels with cerebrospinal fluid signal on T1WI, T2WI and FLAIR images. They appear linear when running parallel to blood vessels, and round or ovoid when perpendicular, with diameters between 2 and 3 mm. We calculated the EPVS numbers in the BG region for each participant. The numbers of EPVS were assessed in each side of the brain, with EPVS spanning multiple levels counted only once. Then, the total numbers of EPVS in bilateral BG regions for each participant were obtained to reflect the glymphatic function.
DTI-ALPS Processing
DTI-ALPS processing was conducted using the FMRIB Software Library (FSL; http://www.fmrib.ox.ac.uk/FSL/), as described in previous studies.28,29 DTI-ALPS data were processed by an experienced radiologist blinded to clinical data. Initially, DTI images were converted from raw data to 4D NIfTI format using dcm2nii. Subsequently, geometric distortions caused by head motion and eddy currents were corrected using the eddy_correct command in FSL. The fdt_rotate_bvecs command was employed to match the corrected gradient direction table. Additionally, scalp and skull removal was performed to obtain a brain tissue mask. The tensor was reconstructed from DTI images using the dtifit command to generate colored fractional anisotropy (FA) maps. Along the level of the lateral ventricles, the perivascular spaces and subcortical fibers run parallel to the left-right direction, perpendicular to the lateral ventricles, which serve as the x-axis. Association fibers primarily run along the anterior-posterior direction (ie, the y-axis), while projection fibers run along the superior-inferior direction (ie, the z-axis). The perivascular spaces, projection fibers, and association fibers are mutually perpendicular. Using fsleyes, spherical regions of interest (ROIs) with a diameter of 4 mm were placed on the projection and association fibers, as well as the subcortical fibers, at mirrored positions in bilateral hemispheres. Within these ROIs, the diffusion coefficients (Dxx, Dyy, and Dzz) of the projection and association fibers were extracted in the x, y, and z directions (Figure 1B).
The DTI-ALPS index was calculated separately for the left and right hemispheres as follows:
DTI-ALPS index = mean (Dxxproj, Dxxassoc) / mean (Dyyproj, Dzzassoc). The average value of both sides was taken to represent the glymphatic function.
Statistical Analysis
Data were analyzed using GraphPad Prism software (GraphPad Inc, San Diego, CA, USA, version 9). A sample size estimation was calculated based on a likely sample proportion having the tested trait (P) of 1.7%,30 with 95% confidence interval (ɑ=0.05) and a 5% margin of error of the estimate. According to these parameters and the statistical formula  , the minimum required sample size was n=26. Continuous variables were expressed as mean ± standard deviation. Comparison between two groups was performed using a t-test, whereas analysis of variance (ANOVA) was used for comparisons among the PD subgroups and HC group. Post-hoc analysis was conducted using Tukey’s test for multiple comparisons. Categorical data were presented as percentages. Comparisons between two groups were conducted using the chi-square test. Spearman correlation analysis with correlation coefficient and 95% confidence interval was utilized to assess the relationship between non-motor symptoms and the ALPS index. For the PD subgroups with differences in the ALPS index, further analysis was performed using receiver operating characteristic (ROC) curves with sensitivity and specificity to evaluate the predictive efficacy of the ALPS index for clinical non-motor symptoms. Statistical significance was set at P<0.05.
, the minimum required sample size was n=26. Continuous variables were expressed as mean ± standard deviation. Comparison between two groups was performed using a t-test, whereas analysis of variance (ANOVA) was used for comparisons among the PD subgroups and HC group. Post-hoc analysis was conducted using Tukey’s test for multiple comparisons. Categorical data were presented as percentages. Comparisons between two groups were conducted using the chi-square test. Spearman correlation analysis with correlation coefficient and 95% confidence interval was utilized to assess the relationship between non-motor symptoms and the ALPS index. For the PD subgroups with differences in the ALPS index, further analysis was performed using receiver operating characteristic (ROC) curves with sensitivity and specificity to evaluate the predictive efficacy of the ALPS index for clinical non-motor symptoms. Statistical significance was set at P<0.05.
Results
Demographic Characteristics and Basic Clinical Information
No significant differences were observed in age (P=0.2006), sex (P=0.4843), smoking (P=0.4658), drinking (P=0.4002), respiratory rate (P=0.1595), pulse rate (P=0.2933), systolic blood pressure (P=0.4250), and diastolic blood pressure (P=0.3916) between PD patients and healthy controls, indicating comparability. Similarly, no significant difference was noted in ESS scores (P=0.2350). The MoCA score was significantly lower in the PD group than in the HC group (P<0.0001), while the PDSS-2, RBDSQ, HAMA, and HAMD scores were higher (all P<0.0001). (Table 1).
Table 1.
Demographic Characteristics and Basic Clinical Information
| PD whole (n=49) | HC whole (n=38) | T or χ2 value | P value | |
|---|---|---|---|---|
| Age (years) | 71.71±7.49 | 70.34±7.57 | 0.8438 | 0.2006 |
| Sex (male) | 46.94% | 47.37% | 0.0020 | 0.4843 |
| Smoking | 24.49% | 23.68% | 0.0080 | 0.4658 |
| Drinking | 16.33% | 18.42% | 0.0660 | 0.4002 |
| Disease duration (years) |
4.80±3.09 | — | — | — |
| LEDD(mg) | 569.74±240.97 | — | — | — |
| Respiratory rate | 18.84±1.33 | 18.55±1.29 | 1.0030 | 0.1595 |
| Pulse rate | 77.63±9.69 | 78.71±8.37 | 0.5458 | 0.2933 |
| Systolic blood pressure | 125.67±8.30 | 125.34±7.80 | 0.1896 | 0.4250 |
| Diastolic blood pressure | 71.06±8.23 | 70.58±7.90 | 0.2760 | 0.3916 |
| UPDRS II | 14.00±6.67 | — | — | — |
| UPDRS III | 25.98±10.15 | — | — | — |
| H-Y stage | 2.51±1.13 | — | — | — |
| MoCA | 25.02±2.93 | 27.47±1.54 | 4.6770 | <0.0001*** |
| PDSS-2 | 14.96±3.86 | 8.53±3.62 | 7.9230 | <0.0001*** |
| ESS | 5.59±4.20 | 5.03±2.64 | 0.7257 | 0.2350 |
| RBDSQ | 4.10±1.93 | 1.55±1.35 | 6.9340 | <0.0001*** |
| HAMA | 11.22±4.28 | 6.68±4.13 | 4.9860 | <0.0001*** |
| HAMD-17 | 12.45±5.53 | 7.16±5.01 | 4.6090 | <0.0001*** |
Notes: ***indicates p value < 0.001.
Abbreviations: PD: Parkinson’s disease, HC: healthy controls, LEDD: levodopa equivalent daily dose, UPDRS: unified Parkinson’s disease rating scale, H-Y: Hoehn-Yahr, MoCA: Montreal cognitive assessment, PDSS: Parkinson’s disease sleep scale, ESS: Epworth sleepiness scale, RBDSQ: REM sleep behavior disorder screening questionnaire, HAMA: Hamilton anxiety rating scale, HAMD: Hamilton depression rating scale.
The Incidence Rates of Cognitive Impairment, Insomnia, Excessive Daytime Sleepiness (EDS), RBD, Anxiety and Depression in PD Patients
Among all PD patients, 24 had cognitive impairment (incidence rate: 48.98%). Additionally, 28 patients (57.14%) had insomnia (sleep disorders indicated by high PDSS-2 scores), 13 (26.53%) had EDS, 23 (46.94%) had RBD, 16 (32.65%) had anxiety, and 18 (36.73%) had depression. (Table 2).
Table 2.
The Incidence Rates of CI, Insomnia, EDS, RBD, Anxiety and Depression in PD Patients
| CI | Insomnia | EDS | RBD | Anxiety | Depression | |
|---|---|---|---|---|---|---|
| With | 24 | 28 | 13 | 23 | 16 | 18 |
| Without | 25 | 21 | 36 | 26 | 33 | 31 |
| Incidence rate | 48.98% | 57.14% | 26.53% | 46.94% | 32.65% | 36.73% |
Abbreviations: CI: Cognitive impairment, EDS: Excessive daytime sleepiness, RBD: REM sleep behavior disorder.
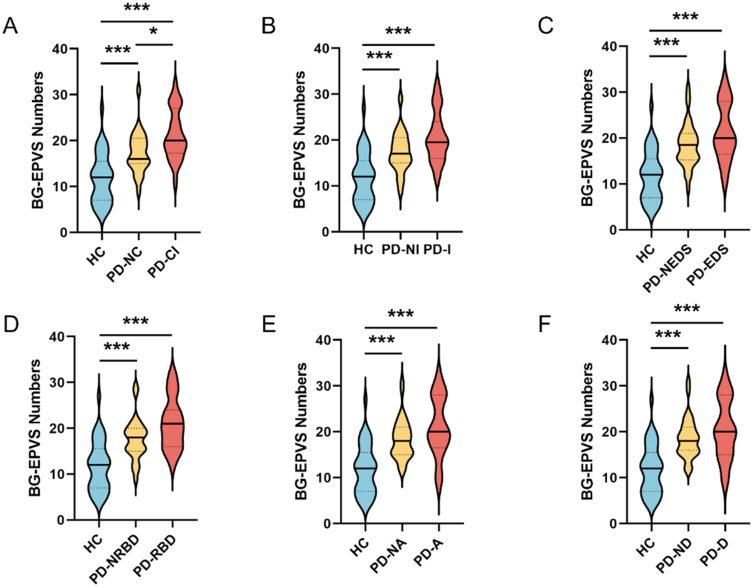
Comparisons of EPVS Numbers Among PD Subgroups and HC Groups
The EPVS numbers in the PD-CI and PD-NC group were all significantly higher than in the HC group (P<0.0001, P=0.0002, respectively); moreover, the EPVS numbers were greater in the PD-CI group than in the PD-NC group (P=0.0275, Figure 2A). When compared with the control group, the PD-I and PD-NI group all showed significant increases in EPVS numbers (P<0.0001, P=0.0005, respectively); however, no significant difference was observed in the EPVS numbers between the PD-I and PD-NI group (P=0.0829, Figure 2B). Similarly, the PD-EDS and PD-NEDS group all exhibited more EPVS numbers compared to the HC group (all P<0.0001); however, there was no significant difference in the EPVS numbers between the PD-EDS and PD-NEDS group (P=0.2323, Figure 2C). Likewise, the PD-RBD and PD-NRBD group all displayed greater numbers of EPVS than the HC group (all P<0.0001); however, no significant difference was noted in the EPVS numbers between the PD-RBD and PD-NRBD group (P=0.0621, Figure 2D). The same trend was detected in the anxiety subgroup, with the PD-A and PD-NA group all showing significantly more EPVS numbers than the HC group (all P<0.0001), but no significant difference in the EPVS numbers between the PD-A and PD-NA group (P=0.2228, Figure 2E). This pattern was consistent in the depression subgroup, with the PD-D and PD-ND group all exhibiting significantly higher numbers of EPVS compared to the control group (all P<0.0001), and no significant difference between the PD-D and PD-ND group (P=0.4625, Figure 2F).
Figure 2.
Comparisons of the BG-EPVS numbers in different groups using violin graphs.(A) Comparisons of the BG-EPVS numbers among the PD-NC, PD-CI, and HC groups. (B) Comparisons of the BG-EPVS numbers among the PD-NI, PD-I, and HC groups. (C) Comparisons of the BG-EPVS numbers among the PD-NEDS, PD-EDS, and HC groups. (D) Comparisons of the BG-EPVS numbers among the PD-NRBD, PD-RBD, and HC groups. (E) Comparisons of the BG-EPVS numbers among the PD-NA, PD-A, and HC groups. (F) Comparisons of the BG-EPVS numbers among the PD-ND, PD-D, and HC groups. *indicates p value < 0.05; **indicates p value < 0.01; ***indicates p value < 0.001.
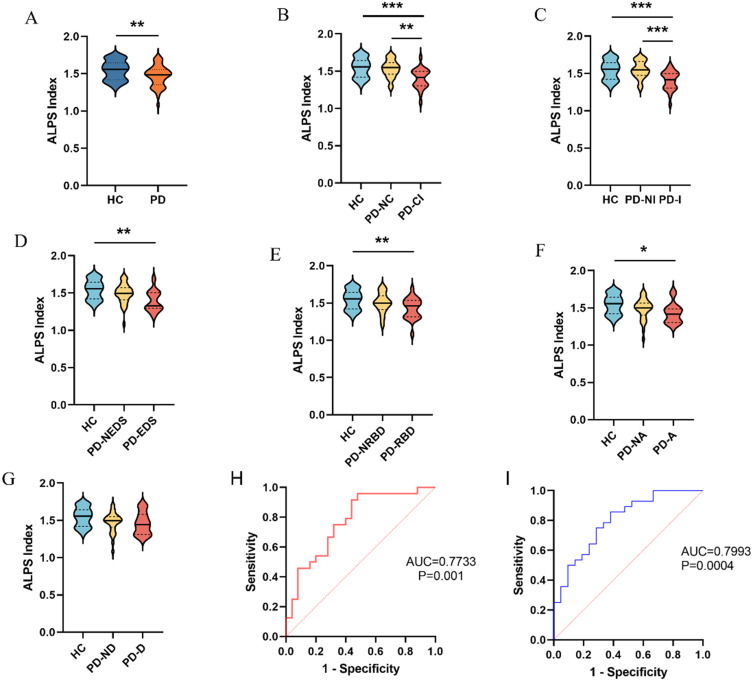
Comparisons of ALPS Index Among PD Subgroups and HC Groups and Predictive Capability of the ALPS Index for the Occurrence of Cognitive Impairment and Insomnia in PD Patients
As the formula for ALPS index calculation mentioned in detail in the Methods section, the capability for water molecules to diffuse in the direction of perivascular space represented by ALPS index can reflect glymphatic function. The ALPS index was significantly lower in the PD group than in the HC group (P=0.0041; Figure 3A). No significant difference was noted in the ALPS index between the PD-NC and HC group (P=0.8874); however, the ALPS index was significantly lower in the PD-CI group than in the PD-NC and HC group (P=0.0015, P<0.0001, respectively; Figure 3B). Similarly, no significant difference was observed in the ALPS index between the PD-NI and HC group (P=0.9976); however, the ALPS index in the PD-I group was significantly lower than that in the PD-NI and HC group (P=0.0005, P<0.0001, respectively; Figure 3C). The ALPS indices all showed no significant differences between the PD-NEDS group and PD-EDS or HC group (P=0.0598, P=0.2023, respectively); however, the ALPS index in the PD-EDS group was significantly lower than that in the HC group (P=0.0017; Figure 3D). Likewise, no significant differences were identified in the ALPS indices in the PD-RBD or HC group compared to that in the PD-NRBD group (P=0.1431, P=0.3851, respectively); however, the ALPS index in the PD-RBD group was significantly lower than that in the HC group (P=0.0035; Figure 3E). Similarly, the ALPS indices all displayed no significant differences between the PD-A or HC group and PD-NA group (P=0.4013, P=0.1381, respectively); however, the ALPS index in the PD-A group was lower than that in the HC group (P=0.0146; Figure 3F). In contrast, no significant differences were found in the ALPS indices between the PD-ND or PD-D group and the HC group (P=0.0683, P=0.0687, respectively), nor between the PD-ND and PD-D group (P=0.9408; Figure 3G).
Figure 3.
Comparisons of the ALPS index in different groups using violin graphs, and ROC curves analyses for the ALPS index to predict cognitive impairment and insomnia (A) Comparison of the ALPS index between the PD and HC group. (B) Comparisons of the ALPS index among the PD-NC, PD-CI, and HC groups. (C) Comparisons of the ALPS index among the PD-NI, PD-I, and HC groups. (D) Comparisons of the ALPS index among the PD-NEDS, PD-EDS, and HC groups. (E) Comparisons of the ALPS index among the PD-NRBD, PD-RBD, and HC groups. (F) Comparisons of the ALPS index among the PD-NA, PD-A, and HC groups. (G) Comparisons of the ALPS index among the PD-ND, PD-D, and HC groups. (H) ROC curve was used to evaluate the diagnostic accuracy of the ALPS index to discriminate PD patients with and without cognitive impairment. (I) ROC curve was used to evaluate the diagnostic accuracy of the ALPS index to discriminate PD patients with and without insomnia. *indicates p value < 0.05; **indicates p value < 0.01; ***indicates p value < 0.001.
Given the significant differences in the ALPS index between the PD-NC and PD-CI group as well as the PD-NI and PD-I group, further ROC curve analyses were conducted. The ALPS index predicted the occurrence of cognitive impairment in PD patients with an area under the curve (AUC) of 0.7733, optimal cutoff value of 1.542, sensitivity of 95.8%, specificity of 52%, and P=0.001 (Figure 3H). Similarly, the ALPS index predicted the occurrence of insomnia in PD patients with an AUC of 0.7993, optimal cutoff value of 1.529, sensitivity of 85.7%, specificity of 61.9%, and P=0.0004 (Figure 3I).
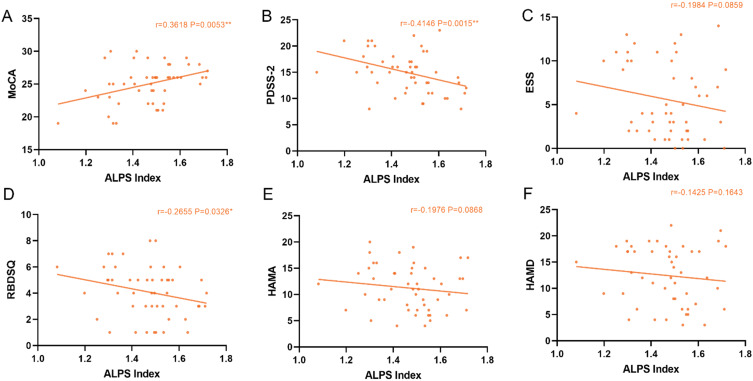
Correlations between cognitive impairment, insomnia, EDS, RBD, anxiety, depression and ALPS index in PD patients.
The MoCA score in PD patients showed a significant positive correlation with the ALPS index (r=0.3618, P=0.0053, 95% CI=0.0813~0.5892; Figure 4A), while the PDSS-2 score exhibited a significant negative correlation with the ALPS index (r=−0.4146, P=0.0015, 95% CI=−0.6283~-0.1426; Figure 4B). However, no significant correlation was observed between the ESS score and ALPS index in PD patients (r=−0.1984, P=0.0859, 95% CI=−0.4610~0.0962; Figure 4C). The RBDSQ score in PD patients was negatively correlated with the ALPS index (r=−0.2655, P=0.0326, 95% CI=−0.5150~0.0255; Figure 4D). However, no significant correlation was found between the HAMA score and ALPS index (r=−0.1976, P=0.0868, 95% CI=−0.4604~0.0970; Figure 4E) or between the HAMD score and ALPS index (r=−0.1425, P=0.1643, 95% CI=−0.4145~0.1528; Figure 4F) in PD patients.
Figure 4.
Correlations between cognitive impairment, insomnia, EDS, RBD, anxiety, depression and ALPS index in PD patients. (A–F) Correlations of the MoCA, PDSS-2, ESS, RBDSQ, HAMA, and HAMD scores with ALPS index in PD group. *indicates p value < 0.05; **indicates p value < 0.01; ***indicates p value < 0.001.
Discussion
In our previous study, we used non-invasive fMRI to assess glymphatic system in PD patients and found that glymphatic function was impaired and correlated with motor symptoms, and we also showed that ALPS index was negatively associated with EPVS numbers in PD. In the present study, we used the average ALPS index and total BG-EPVS numbers of bilateral hemispheres, which better represent the glymphatic function of the whole brain, to investigate their relationship with some non-motor symptoms in PD patients. We found that PD patients with cognitive impairment or insomnia (sleep disorders indicated by high PDSS-2 scores) exhibited more pronounced decline in glymphatic function. Cognitive function in PD patients was positively correlated with the ALPS index, while insomnia scores were negatively correlated with the ALPS index. Furthermore, the ALPS index was predictive of cognitive impairment and insomnia in PD patients.
Our study findings revealed that compared with the healthy controls, PD patients exhibited significantly reduced cognitive function, along with pronounced symptoms of insomnia, RBD, anxiety, and depression. However, no significant difference was observed in EDS. The PDSS-2 scores in the controls were primarily focused on difficulties in falling asleep, early awakenings, and overall sleep quality, while lacking motor and other non-motor symptoms in the night. Therefore, in our study, the PDSS-2 score in the HC group was significantly lower than that in the PD group, while the EDS score was not significantly different. Our findings also showed that the incidence rates of insomnia, cognitive impairment, and RBD were relatively higher.
We found that EPVS numbers in PD patients with and without non-motor symptoms were all higher than the healthy controls, and PD patients with cognitive impairment showed more EPVS numbers than those without. Our findings suggest that EPVS numbers significantly increase in PD patients and may become more pronounced as the non-motor symptoms progress, especially in cognitive decline. Likewise, Donahue et al showed significant increase in EPVS in PD patients.31 Chen et al studied PD patients and found that the EPVS numbers in basal ganglia area were independently correlated with cognitive decline,32 consistent with our results. Fang et al discovered that PD patients with fewer EPVS numbers also have lower a-syn and Tau levels in their cerebrospinal fluid.33 Tau protein is closely associated with cognitive function, which may be the reason why the change of EPVS numbers was most pronounced in the cognitive subgroup in our study. These findings support that PVS is a crucial channel for the glymphatic clearance and EPVS numbers may reflect glymphatic function in part in PD patients. From the above, it can be seen that our results also suggest that the progression of non-motor symptoms in PD exacerbates the glymphatic function. Lara et al showed that the EPVS numbers also increase with age.34 The other potential mechanisms for EPVS presence and glymphatic system abnormalities may be as follows: EPVS are correlated with hypertension biomarkers and more severe arterial stiffness,13,35 and the flow of cerebrospinal fluid is propelled by arterial pulsation and reduced in hypertension status.14 Therefore, age, hypertension and cerebrovascular lesions are possible reasons.
We found that the ALPS index was significantly lower in PD patients than in the HC group, suggesting that PD patients may have impaired global glymphatic function. Qin et al36 also discovered that the average bilateral ALPS index was significantly lower in PD patients than in the controls, consistent with our results. The difference in ALPS index among the cognitive subgroups is similar to that among the insomnia subgroups in our study. Chen et al37 studied PD patients and found that both the mild cognitive impairment and dementia groups had significantly lower ALPS index than the control group, while the cognitively normal and control groups showed no significant differences in ALPS index. Due to exclusion of patients with severe cognitive impairment in our study, we did not divide the cognitive impairment group into mild cognitive impairment and dementia groups yet obtained similar results as those of Chen et al.37 Gu et al38 assessed the sleep status in PD patients using the Pittsburgh Sleep Quality Index (PSQI) scale and found that both PD patients with good and poor sleep exhibited significantly lower ALPS index than the controls, which slightly differs from our results. The reason for this discrepancy may be that we used the PDSS-2 to assess the sleep quality in PD patients, which, compared with the PSQI scale, places greater emphasis on nocturnal motor and non-motor symptoms. Therefore, we did not observe a significant decrease in the ALPS index among PD patients without insomnia compared with that in the controls. EDS and RBD are two other types of sleep abnormalities in PD patients. We found that PD patients with EDS or RBD all exhibited significantly lower ALPS index than the controls. This finding corresponds with the relationship observed between PDSS-2 scores and glymphatic function. Si et al29 also conducted subgroup analyses of non-motor symptoms in PD patients and similarly found that those with EDS or RBD showed significantly lower ALPS indices than the controls. Regarding anxiety and depression, we revealed that PD patients with anxiety exhibited lower ALPS index than the controls, while those with depression only showed a decline trend in ALPS index without statistical difference. Shen et al39 discovered that the ALPS index was negatively correlated with HAMA and HAMD scores in PD patients; however, He et al40 found no such correlation. This discrepancy may be related to the reasons such as sample size and use of anxiolytic or antidepressant medications. In summary, PD patients with non-motor symptoms showed lower ALPS index compared to controls. These findings correspond with the results that PD patients with non-motor symptoms displayed more EPVS numbers than the controls mentioned before. In our study, although PD patients without non-motor symptoms showed increases in EPVS numbers compared to the control group, the ALPS indices displayed only decreasing trends without statistical differences, implying that EPVS may occur before the glymphatic dysfunction. However, we found that, compared with PD patients without insomnia, PD patients with insomnia only showed an increasing trend in EPVS numbers with no statistical difference, while the ALPS index significantly decreased, suggesting that factors other than EPVS may also influence the ALPS index. It can be seen that the relationship between the glymphatic system and non-motor symptoms in PD is complex and requires further researches from multiple centers to be clarified.
Combining the ALPS index with EPVS numbers, our findings once again suggest that as non-motor symptoms of PD progress, particularly in cognition and sleep, the impairment of glymphatic function becomes more pronounced. We believe that sleep disorders may decrease glymphatic function, while impairment of glymphatic function leads to the accumulation of pathogenic proteins in the brain, resulting in cognitive impairment. Xie et al41 found that a notable expansion of the interstitial space in the brain of mice during anesthesia or natural sleep was accompanied by a significant increase in cerebrospinal fluid exchange with the interstitial fluid, resulting in more efficient clearance of Aβ. This finding suggests that glymphatic function is markedly enhanced during sleep states. Aβ and Tau, two pathogenic proteins, are believed to contribute to the pathogenesis of cognitive impairment. Chen et al discovered that the decline in cognitive ability in PD patients is related to changes of the levels of Aβ and Tau in cerebrospinal fluid caused by impaired glymphatic function, and these two toxic proteins may interact with each other.32 Previous studies have reported that reduced clearance of Aβ can increase deposition of α-syn, promoting the pathological progression of PD, with both having a synergistic effect similarly.42 Zhang et al provided evidence for the interaction between the glymphatic function and α-syn in PD model mice.43 In their study, they confirmed that the decline in glymphatic clearance aggravates α-syn deposition and α-syn accumulation further causes the reduced AQP4 expression or polarization to suppress the glymphatic clearance. Furthermore, they conducted odor discrimination test and rotarod test in the model mice, and found that AQP4 deficiency significantly accelerated the olfactory deficit and the movement disorder. Therefore, it is speculated that the occurrence of cognitive impairment and sleep disorders in PD patients is associated with excessive deposition of those toxic proteins in the brain due to decreased glymphatic function. Siow et al44 found that a decrease in ALPS index was significantly correlated with reduction in gray matter volume in brain regions associated with cognitive function, such as the medial frontal lobe, hippocampus, and posterior insula. This finding indicates that the hippocampus and some brain regions are relatively more sensitive to the effects of glymphatic dysfunction. From the above, it can be seen that the glymphatic function, sleep, and cognition indeed mutually influence each other.
Our results in the correlations between cognition, sleep and the ALPS index further underscore the association between glymphatic dysfunction and the progression of cognitive impairment and sleep disorders in PD. Bae et al45 also reported a correlation between the ALPS index and cognitive function in PD patients, while Cai et al28 observed a negative correlation between the ALPS index and PDSS-2 scores in PD patients. The findings regarding the correlation between MoCA scores, PDSS-2 scores, and the ALPS index in our study are similar to those reported in these previous studies. We did not observe a significant correlation between ESS scores and the ALPS index, consistent with the findings of Qin et al.36 The reasons for this lack of correlation may be that EDS in PD patients is related to several factors, such as alterations in the sleep-wake cycle, nocturnal sleep quality, and side effects of anti-Parkinson’s medications such as dopamine receptor agonists. Si et al29 investigated the glymphatic function in patients with idiopathic RBD and PD and found a negative correlation between RBD-HK II scores and the ALPS index in RBD patients but did not observe such a correlation in PD patients. However, our study indicated a weak negative correlation between RBDSQ scores and the ALPS index in PD patients. The utilization of the RBDSQ scales in our study and the high prevalence of RBD in PD patients, reaching 46.94%, may explain why our results differ from those of Si et al.29 However, this also suggests a possible association between glymphatic function and RBD symptoms in PD patients, which needs further confirmation by large-scale and multi-center studies combined with polysomnography. The possible mechanism underlying RBD occurrence in PD patients is an excessive deposition of α-syn in the cerebrospinal fluid.46 Besides imaging parameters such as DTI-ALPS index, other serum biomarkers may also correlate with non-motor symptoms in PD. Tang et al found that serum Glial cell-derived neurotrophic factor (GDNF) coupling brain structural and functional changes underlies cognition in PD patients.47 We will attempt to analyze the serum biomarkers such as GDNF in PD in our future study.
The present study has some limitations. First, this study was conducted at a single center with a limited sample, which may introduce selection bias and affect the results. Second, we only investigated some non-motor symptoms of PD. Finally, we excluded patients with severe cognitive impairment and did not conduct polysomnography examinations in PD patients. Therefore, further study including other non-motor symptoms such as hyposmia and constipation with a larger sample in multi-center is needed. Additionally, we may study patients with severe cognitive decline and perform polysomnography examinations in PD patients in future research.
Conclusions
Our study suggests correlations between glymphatic function and cognition, sleep, anxiety and depression in PD patients, particularly evident in cognitive impairment and sleep disorders. PD patients with cognitive decline, insomnia or RBD display more worse glymphatic function. The potential mechanism may be that PD patients with above non-motor symptoms show certain changes of the levels of a-syn, Tau and Aβ in their cerebrospinal fluid caused by decline in glymphatic clearance. We will investigate the association between the glymphatic function and relevant biomarkers such as a-syn in PD patients in future study. The glymphatic system may also serve as a potential intervention target for PD non-motor symptoms.
Acknowledgments
We would like to thank the PD patients and healthy controls who spent their time to participate in this study.
Funding Statement
This work was supported by the Suzhou Science and Technology Research Project (SKJY2021121).
Data Sharing Statement
The data that support the findings of our study are available from the corresponding author upon reasonable request.
Disclosure
The authors declare that they have no conflicts of interest.
References
- 1.Prete M, Cellini N, Ronconi L, Di Rosa E. Cognitive reserve moderates the relationship between sleep difficulties and executive functions in patients with Parkinson’s disease. Sleep Med. 2023;111:82–85. doi: 10.1016/j.sleep.2023.09.009 [DOI] [PubMed] [Google Scholar]
- 2.Wang H, Zhao Y, Schrag A. Development of anxiety in early Parkinson’s disease: a clinical and biomarker study. Eur J Neurol. 2023;30(9):2661–2668. doi: 10.1111/ene.15890 [DOI] [PubMed] [Google Scholar]
- 3.Niu L, Yao C, Zhang C, et al. Sex- and age-specific prevalence and risk factors of depressive symptoms in Parkinson’s disease. J Neural Transm. 2023;130(10):1291–1302. doi: 10.1007/s00702-023-02658-x [DOI] [PubMed] [Google Scholar]
- 4.Ryu DW, Yoo SW, Choi KE, Oh YS, Kim JS. Correlation of olfactory function factors with cardiac sympathetic denervation in Parkinson’s disease. J Neurol. 2023. [DOI] [PubMed] [Google Scholar]
- 5.Li L, Wang Z, You Z, Huang J. Prevalence and influencing factors of depression in patients with Parkinson’s disease. Alpha Psychiatry. 2023;24(6):234–238. doi: 10.5152/alphapsychiatry.2023.231253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Menkü BE, Akın S, Tamdemir SE, Genis B, Altıparmak T, Cosar B. Diagnostic transitions from primary psychiatric disorders to underlying medical conditions: a 5-year retrospective survey from a university hospital sample. Alpha Psychiatry. 2024;25(2):226–232. doi: 10.5152/alphapsychiatry.2024.231274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mehra S, Sahay S, Maji SK. α-Synuclein misfolding and aggregation: implications in Parkinson’s disease pathogenesis. Biochim Biophys Acta Proteins Prot. 2019;1867(10):890–908. doi: 10.1016/j.bbapap.2019.03.001 [DOI] [PubMed] [Google Scholar]
- 8.Natale G, Limanaqi F, Busceti CL, et al. Glymphatic system as a gateway to connect neurodegeneration from periphery to CNS. Front Neurosci. 2021;15:639140. doi: 10.3389/fnins.2021.639140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Iliff JJ, Wang M, Liao Y, et al. A paravascular pathway facilitates CSF flow through the brain parenchyma and the clearance of interstitial solutes, including amyloid β. Sci Transl Med. 2012;4(147):147ra111. doi: 10.1126/scitranslmed.3003748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Verghese JP, Terry A, de Natale ER, Politis M. Research evidence of the role of the glymphatic system and its potential pharmacological modulation in neurodegenerative diseases. J Clin Med. 2022;11(23):6964. doi: 10.3390/jcm11236964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brown R, Benveniste H, Black SE, et al. Understanding the role of the perivascular space in cerebral small vessel disease. Cardiovasc Res. 2018;114(11):1462–1473. doi: 10.1093/cvr/cvy113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shulyatnikova T, Hayden MR. Why are perivascular spaces important? Medicina (Kaunas). 2023;59(5). doi: 10.3390/medicina59050917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bae JH, Kim JM, Park KY, Han SH. Association between arterial stiffness and the presence of cerebral small vessel disease markers. Brain Behav. 2021;11(1):e01935. doi: 10.1002/brb3.1935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mestre H, Tithof J, Du T, et al. Flow of cerebrospinal fluid is driven by arterial pulsations and is reduced in hypertension. Nat Commun. 2018;9(1):4878. doi: 10.1038/s41467-018-07318-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hsu JL, Wei YC, Toh CH, et al. Magnetic resonance images implicate that glymphatic alterations mediate cognitive dysfunction in Alzheimer disease. Ann Neurol. 2023;93(1):164–174. doi: 10.1002/ana.26516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ma X, Li S, Li C, et al. Diffusion tensor imaging along the perivascular space index in different stages of Parkinson’s disease. Front Aging Neurosci. 2021;13:773951. doi: 10.3389/fnagi.2021.773951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Meng JC, Shen MQ, Lu YL, et al. Correlation of glymphatic system abnormalities with Parkinson’s disease progression: a clinical study based on non-invasive fMRI. J Neurol. 2024;271(1):457–471. doi: 10.1007/s00415-023-12004-6 [DOI] [PubMed] [Google Scholar]
- 18.Xu S, Wang J, Sun K, et al. Cognitive impairment in chronic kidney disease is associated with glymphatic system dysfunction. Kidney Dis (Basel). 2023;9(5):384–397. doi: 10.1159/000530635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee DA, Lee HJ, Park KM. Glymphatic dysfunction in isolated REM sleep behavior disorder. Acta Neurol Scand Apr. 2022;145(4):464–470. doi: 10.1111/ane.13573 [DOI] [PubMed] [Google Scholar]
- 20.Wang C XX, Teng QC. MRI-visible enlarged perivascular spaces: imaging marker to predict cognitive impairment in older chronic insomnia patients. Eur Radiol. 2022;32(8):5446–5457. doi: 10.1007/s00330-022-08649-y [DOI] [PubMed] [Google Scholar]
- 21.Pang H, Wang J, Yu Z, et al. Glymphatic function from diffusion-tensor MRI to predict conversion from mild cognitive impairment to dementia in Parkinson’s disease. J Neurol. 2024;271(8):5598–5609. doi: 10.1007/s00415-024-12525-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gnarra O, Calvello C, Schirinzi T, et al. Exploring the association linking head position and sleep architecture to motor impairment in Parkinson’s disease: an exploratory study. J Pers Med. 2023;13(11). doi: 10.3390/jpm13111591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yue Y, Zhang X, Lv W, Lai HY, Shen T. Interplay between the glymphatic system and neurotoxic proteins in Parkinson’s disease and related disorders: current knowledge and future directions. Neural Regen Res. 2024;19(9):1973–1980. doi: 10.4103/1673-5374.390970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kobak Tur E, Ari BC. Mild cognitive impairment in patients with Parkinson´s disease and the analysis of associated factors. Neurol Res. 2023;45(12):1161–1168. doi: 10.1080/01616412.2023.2258038 [DOI] [PubMed] [Google Scholar]
- 25.Suzuki K, Miyamoto T, Miyamoto M, et al. Evaluation of cutoff scores for the Parkinson’s disease sleep scale-2. Acta Neurol Scand. 2015;131(6):426–430. doi: 10.1111/ane.12347 [DOI] [PubMed] [Google Scholar]
- 26.Videnovic A, Noble C, Reid KJ, et al. Circadian melatonin rhythm and excessive daytime sleepiness in Parkinson disease. JAMA Neurol. 2014;71(4):463–469. doi: 10.1001/jamaneurol.2013.6239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stiasny-Kolster K, Mayer G, Schäfer S, Möller JC, Heinzel-Gutenbrunner M, Oertel WH. The REM sleep behavior disorder screening questionnaire--a new diagnostic instrument. Mov Disord. 2007;22(16):2386–2393. doi: 10.1002/mds.21740 [DOI] [PubMed] [Google Scholar]
- 28.Cai X, Chen Z, He C, et al. Diffusion along perivascular spaces provides evidence interlinking compromised glymphatic function with aging in Parkinson’s disease. CNS Neurosci Ther. 2023;29(1):111–121. doi: 10.1111/cns.13984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Si X, Guo T, Wang Z, et al. Neuroimaging evidence of glymphatic system dysfunction in possible REM sleep behavior disorder and Parkinson’s disease. NPJ Parkinsons Dis. 2022;8(1):54. doi: 10.1038/s41531-022-00316-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liu QW, Mao CJ, Lu ZH, et al. Sarcopenia is associated with non-motor symptoms in Han Chinese patients with Parkinson’s disease: a cross-sectional study. BMC Geriatr. 2023;23(1):494. doi: 10.1186/s12877-023-04188-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Donahue EK, Murdos A, Jakowec MW, et al. Global and regional changes in perivascular space in idiopathic and familial Parkinson’s disease. Mov Disord. 2021;36(5):1126–1136. doi: 10.1002/mds.28473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chen H, Wan H, Zhang M, Wardlaw JM, Feng T, Wang Y. Perivascular space in Parkinson’s disease: association with CSF amyloid/tau and cognitive decline. Parkinsonism Relat Disord. 2022;95:70–76. doi: 10.1016/j.parkreldis.2022.01.002 [DOI] [PubMed] [Google Scholar]
- 33.Fang Y, Gu LY, Tian J, et al. MRI-visible perivascular spaces are associated with cerebrospinal fluid biomarkers in Parkinson’s disease. Aging (Albany NY). 2020;12(24):25805–25818. doi: 10.18632/aging.104200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lara FR, Scruton AL, Pinheiro A, et al. Aging, prevalence and risk factors of MRI-visible enlarged perivascular spaces. Aging. 2022;14(17):6844–6858. doi: 10.18632/aging.204181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sibilia F, Sheikh-Bahaei N, Mack WJ, Choupan J. Perivascular spaces in Alzheimer’s disease are associated with inflammatory, stress-related, and hypertension biomarkers. bioRxiv. 2023. doi: 10.1101/2023.06.02.543504 [DOI] [Google Scholar]
- 36.Qin Y, He R, Chen J, et al. Neuroimaging uncovers distinct relationships of glymphatic dysfunction and motor symptoms in Parkinson’s disease. J Neurol. 2023;270(5):2649–2658. doi: 10.1007/s00415-023-11594-5 [DOI] [PubMed] [Google Scholar]
- 37.Chen HL, Chen PC, Lu CH, et al. Associations among cognitive functions, plasma DNA, and diffusion tensor image along the perivascular space (DTI-Alps) in patients with Parkinson’s disease. Oxid Med Cell Longev. 2021;2021:4034509. doi: 10.1155/2021/4034509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gu L, Dai S, Guo T, et al. Noninvasive neuroimaging provides evidence for deterioration of the glymphatic system in Parkinson’s disease relative to essential tremor. Parkinsonism Relat Disord. 2023;107:105254. doi: 10.1016/j.parkreldis.2022.105254 [DOI] [PubMed] [Google Scholar]
- 39.Shen T, Yue Y, Ba F, et al. Diffusion along perivascular spaces as marker for impairment of glymphatic system in Parkinson’s disease. NPJ Parkinsons Dis. 2022;8(1):174. doi: 10.1038/s41531-022-00437-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.He P, Shi L, Li Y, et al. The association of the glymphatic function with Parkinson’s disease symptoms: neuroimaging evidence from longitudinal and cross-sectional studies. Ann Neurol. 2023;94(4):672–683. doi: 10.1002/ana.26729 [DOI] [PubMed] [Google Scholar]
- 41.Xie L, Kang H, Xu Q, et al. Sleep drives metabolite clearance from the adult brain. Science. 2013;342(6156):373. doi: 10.1126/science.1241224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Köppen J, Schulze A, Machner L, et al. Amyloid-beta peptides trigger aggregation of alpha-synuclein in vitro. Molecules. 2020;25(3):580. doi: 10.3390/molecules25030580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhang Y, Zhang C, He XZ, et al. Interaction between the glymphatic system and α-synuclein in Parkinson’s disease. Mol Neurobiol Apr. 2023;60(4):2209–2222. doi: 10.1007/s12035-023-03212-2 [DOI] [PubMed] [Google Scholar]
- 44.Siow TY, Toh CH, Hsu JL, et al. Association of sleep, neuropsychological performance, and gray matter volume with glymphatic function in community-dwelling older adults. Neurology. 2022;98(8):e829–e838. doi: 10.1212/WNL.0000000000013215 [DOI] [PubMed] [Google Scholar]
- 45.Bae YJ, Kim JM, Choi BS, et al. Glymphatic function assessment in Parkinson’s disease using diffusion tensor image analysis along the perivascular space. Parkinsonism Relat Disord. 2023;114:105767. doi: 10.1016/j.parkreldis.2023.105767 [DOI] [PubMed] [Google Scholar]
- 46.Hu Y, Yu SY, Zuo LJ, et al. Parkinson disease with REM sleep behavior disorder: features, α-synuclein, and inflammation. Neurology. 2015;84(9):888–894. doi: 10.1212/WNL.0000000000001308 [DOI] [PubMed] [Google Scholar]
- 47.Tang C, Sun R, Xue K, et al. Distinct serum GDNF coupling with brain structural and functional changes underlies cognitive status in Parkinson’s disease. CNS Neurosci Ther. 2024;30(3):e14461. doi: 10.1111/cns.14461 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of our study are available from the corresponding author upon reasonable request.