Abstract
Purpose
In recent years, the need for a more appropriate prescription of medications in the older population has emerged as a significant public health concern. In this study, we aimed to evaluate the prevalence of potentially inappropriate medications (PIM) in hospitalized adults aged ≥ 75.
Patients and methods
This was a retrospective descriptive observational study of patients at 16 hospitals in Spain. The study population included inpatients aged ≥ 75 admitted during a 7-day period (May 10 to 16, 2021). Data were obtained from the pharmacy databases of the participating hospitals. The list of PIMs was based on the Beers, STOPP-START, EU-PIM and PRISCUS criteria.
Results
A total of 4,183 patients were included. PIMs were detected in 23.5% (N = 1,126) of the cohort. The prevalence rates at the participating hospitals ranged from 10% to 42.5%. The PIM/patient ratio was 1.2. The most common PIMs were midazolam, dexketoprofen, diazepam, and doxazosin, all of which (except for doxazosin) were more common in women. Benzodiazepines accounted for 70% of all PIMs. In 35% of cases, the PIMs were initiated before hospital admission. Of the 818 PIMs initiated during hospitalization, the two most common were benzodiazepines (49%) and anti-inflammatory drugs (25%). At discharge, only 4.9% of the PIMs initiated during the hospital stay were still prescribed.
Conclusion
In this population of older hospitalized patients, the overall prevalence of PIMs was moderate. However, the prevalence rate at the participating hospitals was highly variable. In most cases, PIMs prescribed prior to hospitalization for chronic conditions were not withdrawn during the hospital stay. No significant increase in PIMs was observed from pre-admission to post-discharge.
These findings underscore the need for multidisciplinary interventions to optimize the pharmaceutical treatment in older adults in the hospital setting to reduce the consequences of PIMs in patients.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12877-024-05308-3.
Keywords: Inappropriate prescribing, Aged, Inpatients, Patient discharge
Introduction
In recent decades, prescription drug use has increased substantially around the world. Polypharmacy, defined as the chronic use of five or more drugs, is present in approximately 40% of adults over age 65 years [25, 28, 30]. In adults over 75 years of age, the prevalence of polypharmacy at hospital admission can be as high as 90% [32].
Multimorbidity, the concomitant presence of multiple chronic conditions, is common in older adults, which is why pharmacotherapy plays an important role in the treatment of these patients [9]. Although polypharmacy is often necessary and beneficial in older adults, there is a growing concern over the increasing prevalence of this practice, which is associated with potentially dangerous drug interactions, poor adherence, a greater risk of falls, higher overall costs of care, and increased mortality [13, 23]. Furthermore, due to the physiological changes associated with age, changes in the pharmacokinetics and pharmacodynamics of these drugs may increase the risk of adverse effects in patients who take multiple medications [45].
In older adults, polypharmacy is associated with the use of potentially inappropriate medications (PIM), which has been defined as medications whose risks outweigh the clinical benefits, particularly when safer or more effective alternatives are available [35]. In general, these drugs should be avoided in all patients, but particularly in older adults [1]. Inappropriate prescribing in the elderly has emerged as a significant public health concern [16]. The practice of potentially inappropriate prescribing (PIP)—defined as the prescription of medications that may not benefit patients and/or that do not adhere to clinical guidelines—is widespread. For example, a study conducted in the primary care setting found that the prevalence of PIP in adults aged > 64 is as high as 33% [21]. The widespread practice of PIP is concerning given the association with all-cause mortality, hospital readmission, functional decline, and other deleterious effects in hospitalized older patients [27].
In older adults, the estimate prevalence of PIMs ranges from 16 to 42% [8, 41, 42]. PIMs have been associated with an increased risk of hospitalization, a decrease in physical function, and even death in vulnerable populations; they have also been associated with incident disability and hospitalization in healthy older adults [22, 29]. In addition, studies show that elderly individuals exposed to two or more PIMs have a higher risk of developing adverse health outcomes than patients exposed to only one PIM [47].
In this context, several different tools have been developed to help clinicians identify PIMs, including the Beers criteria [1], the STOPP/START criteria [33], and the PRISCUS list [26]. All of these tools have the same purpose: to help healthcare professionals to identify medications whose risks outweigh their clinical benefits in order to reduce older patients’ exposure to these drugs. These tools can also be used to analyze drug prescription patterns in this population.
The prevalence of PIMs is highly variable and influenced by a wide range of factors, including the following: 1) the specific population and prescribing practices in a given country; 2) the setting (community, hospital, nursing home, primary care, etc.); 3) the individual healthcare center and characteristics of the clinical staff; and 4) the tool or criteria used to identify the PIMs. In this regard, it is evident that any intervention designed to reduce or avoid the use of PIMs must be adapted to suit the specific situation. This is particularly important in older hospitalized patients, who have a higher risk of developing drug-related problems [14, 20].
In this context, the present study had three aims: 1) determine the prevalence of PIMs among hospitalized patients age ≥ 75 at a representative sample of hospitals, 2) identify most common; and 3) explore the prescription dynamics.
Material and methods
This was a retrospective descriptive observational study involving 16 hospitals located in four different autonomous communities (regions) in Spain (Catalonia, Basque Country, Navarra, Madrid). All of these hospitals are members of the MAPAC-MPC (Mejora de la Adecuación de la Práctica Asistencial y Clínica) network, whose aim is to improve the appropriateness of healthcare practice and clinical care across the national health care system [4].
The study population included all patients aged ≥ 75 admitted to the participating hospitals during the 7-day period from May 10 to May 16, 2021. Patients admitted to the emergency room for more than 16 h were also included in the study.
The patients’ clinical and sociodemographic data, together with data on the drugs administered during hospitalization, were obtained from electronic prescription records of the pharmacy departments of the participating centres. The following variables were collected: hospital (name, location); hospital department; sociodemographic data (age, sex); date of admission; date of discharge; PIMs received during hospitalization (the specific drugs for each patient); and mortality (during hospitalization or within one month of discharge). Anonymized data from each patient were introduced to the Clinapsis® application, an online application for the design and management of epidemiologic and clinical studies (https://www.recercasantpau.cat/en/clinical-research/clinapsis/). Afterwards, study team members from the MAPAC-MPC network of each centre validated the detected PIMs and revised: 1) If they were already part of the patients’ pre-admission medication; 2) If they were still present upon discharge, and 3) If they were still prescribed one month after discharge. This revision was possible because in almost all Spanish regions there is a common online healthcare prescription platform that allows clinicians working in the public National Healthcare System to access information regarding a patient’s ambulatory pharmacological treatment, with start and end dates, as well as to consult changes in prescriptions and find out if a treatment was considered chronic (≥ 3 months).
The list of PIMs used in the present study was based on a document by the Medication Management Department of the Catalan Health Service on potentially inappropriate medications on older adults [40], which includes medications that comply with at least one of the following criteria: a) Being included in at least two of internationally-recognized lists of PIM (Beers [2], STOPP-START [34], EU-PIM [37] and PRISCUS [19]); b) Having an explicit contraindication in their technical datasheet against use in older adults; c) Having a specific alert in the Spanish Agency for Medicines and Health Products (AEMPS, a state agency attached to the Spanish Ministry of Health). From this list, we then identified all the drugs included in the pharmacological guidelines of the participating hospitals. The final list contained a total of 56 PIMs. For additional details, see Supplementary Table 1.
The overall prevalence of PIMs at the participating hospitals—defined as at least one PIM per patient admitted during the study week—was evaluated. We then determined the mean number of PIMs per patient during the study period and the most commonly prescribed drugs by sex and hospital department. For PIMs detected during hospitalization, we determined in which setting they were initiated (i.e., pre-admission or during hospitalization) and whether they remained prescribed one month after hospital discharge. For each PIM, we identified the work setting of the prescribing physician (primary care, hospital, intermediate care center, other) and type of medication chronic vs. non-chronic. A secondary analysis that included only the patients who were still alive at one-month post-discharge was performed. That analysis excluded all patients who died during hospitalization or within the first month after discharge.
Due to the descriptive nature of the study, no sample size estimation was considered necessary. Nevertheless, we used the GranMo calculator to calculate the theoretically needed sample size [15]. Based on that calculation, we estimated that a minimum sample size of 400 patients was needed considering an infinite population, 5% precision, 95% confidence interval (CI) and PIM prevalence of 50%. The final sample size (1,126 patients receiving at least one PIM) was considered sufficient to perform the analysis.
For the descriptive analyses, we calculated frequencies, proportions, means, ranges, standard deviation (SD), and cross-tabulations. The Mann–Whitney test was applied to test for statistically significant differences between numerical independent data. The Chi-square test was used to test for significant differences between categorical data. The cut-off for statistical significance was set at p < 0.05. Microsoft Excel and the IBM-SPSS statistical software program (V. 26.0) were used to perform the statistical analyses.
The study was approved by the Ethics Committee for Research with Medicinal Products (CEIM) of the Fundació de Gestió Sanitària de l’Hospital de la Santa Creu i Sant Pau. Informed consent has been waived by the CEIM of the Fundació de Gestió Sanitària de l’Hospital de la Santa Creu i Sant Pau, with reference code IIBSP-MAP-2021-146, as this was a retrospective observational study, using secondary and anonymized data, in the context of improving the appropriateness of healthcare. The study fully adhered to the principles of the Declaration of Helsinki.
Results
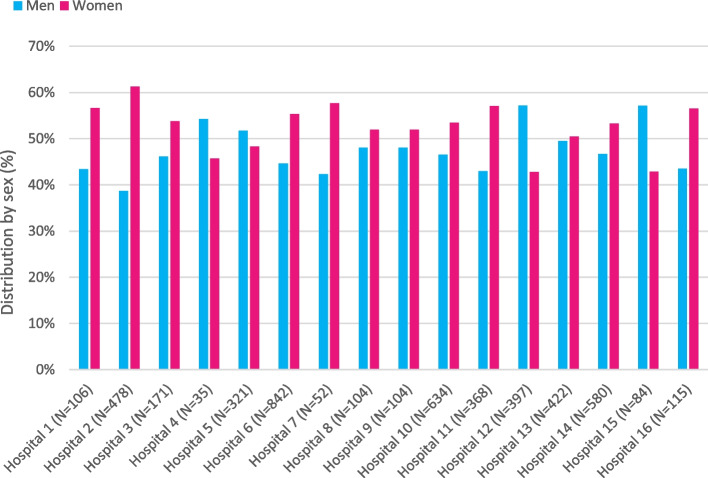
A total of 4,813 patients aged ≥ 75 years admitted to the 16 participating hospitals during the study week were included in the study. Of these, 53.2% were women (range 42.8%-61.3%). Figure 1 provides a detailed distribution of the participants across the participating hospitals.
Fig. 1.
Patients admitted during the week of the study by sex and hospital
PIMs were detected in 23.5% (N = 1,126) of the sample (23% of the men and 24% of the women). The mean age of the women with PIMs was 83.6 ± 5.1 years (range 75–103) versus 82.2 ± 5.8 years (range 75–96) in the men (p = 0.001). During hospitalization, 197 (17.5%) of the patients with PIMs died (90 women, 107 men).
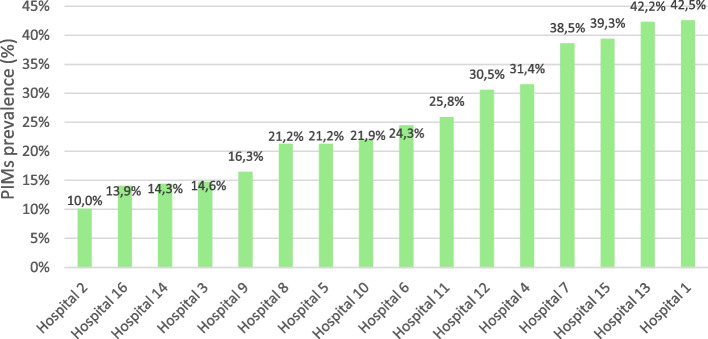
The prevalence rates at the participating hospitals ranged from 10% to 42.5% (Fig. 2). A total of 1,407 PIMs (35 different drugs) were detected during the study week (see Supplementary Table 2). The PIM to patient ratio was 1.2 (as some patients—15% of the sample—received more than one PIM).
Fig. 2.
Prevalence of potentially inappropriate medications (PIMs) by hospital
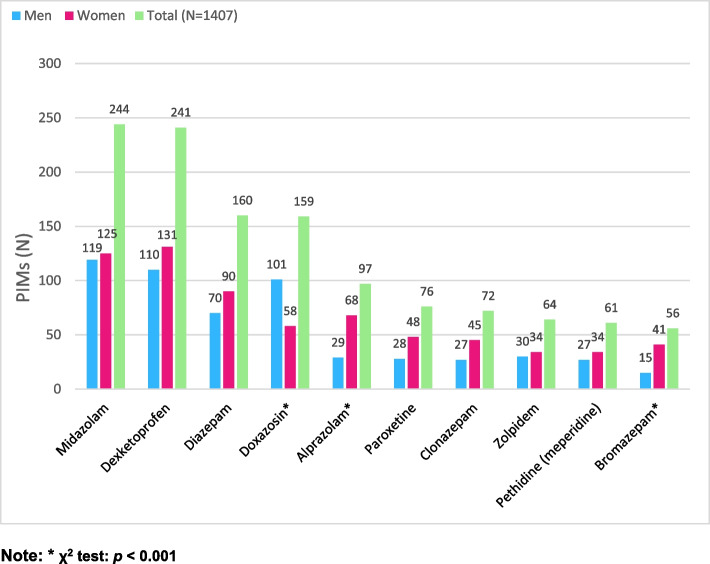
Of the 56 drugs on the PIM list, the following 10 accounted for 90% of all PIMs: midazolam (N = 244), dexketoprofen (N = 241), diazepam (N = 160), doxazosin (N = 159), alprazolam (N = 97), paroxetine (N = 76), clonazepam (N = 72), zolpidem (N = 64), pethidine (N = 61), and bromazepam (N = 56). These drugs were more common in women, with a significant difference for alprazolam and bromazepam (p < 0.001). The only two drugs that were significantly more common in men were doxazosin and pentoxifylline (p < 0.001) (Fig. 3). Given the high intrahospital mortality rate in the PIM group (N = 173, 15.4%), we conducted a sensitivity analysis that excluded all PIMs detected in those patients. That analysis showed the same PIM distribution, except for midazolam, which as only the 4th most common PIM in the secondary analysis.
Fig. 3.
Top ten most common potentially inappropriate medications (PIMs)
In terms of the distribution of PIMs by hospital department, the following six departments accounted for 55% of all PIMs: Internal Medicine (N = 269); Emergency Department (N = 150); General and Digestive Surgery (N = 114); Orthopedics (N = 92); Cardiology (N = 72); and Geriatrics (N = 68). Midazolam was the most commonly prescribed PIM in the Internal Medicine, Geriatrics, Oncology, and Respiratory Medicine departments. By contrast, dexketoprofen was the most frequently prescribed PIM in the Orthopedics, Anesthesia, Emergency, Urology, and General and Digestive Surgery departments.
Data on the pre- and post-admission period were reported by 14 hospitals (missing information from two hospitals). A total of 1,267 PIMs corresponding to 1,026 patients were studied to determine in which setting the PIMs were initiated (i.e., pre-admission or during hospitalization) and whether the PIMs remained prescribed one month after hospital discharge. Thirty five percent of these PIMs were initiated prior to hospital admission (Algorithm 1), most of which (88%) were medications for chronic conditions. In 75% of cases, the prescriber was a primary care physician. Benzodiazepines accounted for 70% of the PIMs initiated prior to hospital admission. Of the PIMs initiated during the hospital stay (N = 818), 49% were benzodiazepines (mainly midazolam and diazepam) and 25% were anti-inflammatory drugs (mainly dexketoprofen).
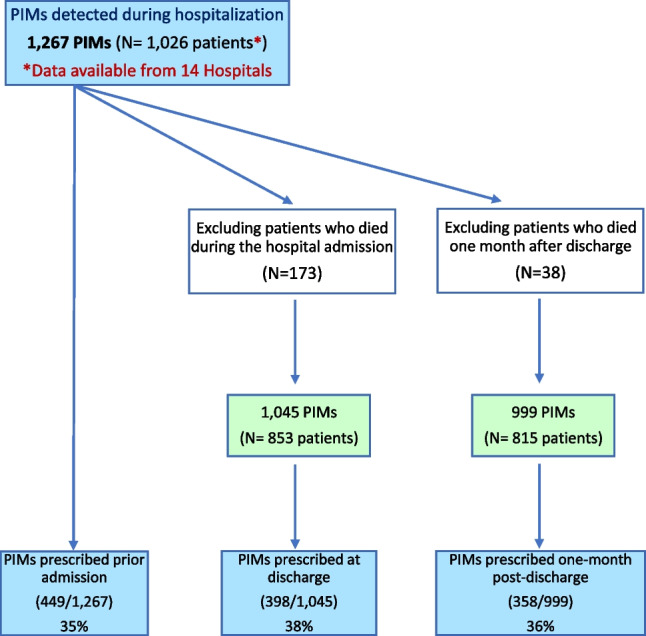
Algorithm 1. PIMs detected during hospitalization; PIMs detected prior to admission; and PIMs prescribed at discharge and at one month post-discharge
To determine the PIMs that were still prescribed one month after hospital discharge, we first excluded all patients who died during hospitalization or within one month of discharge (N = 211). That analysis showed that 38% of the PIMs were still present at hospital discharge and 36% were still present at one month. Considering only the PIMs that were started during the hospital stay (N = 818), only 40 (4.9%) were still prescribed at discharge and only 21 (2.6%) at one month (Table 1).
Table 1.
Potentially inappropriate medications (PIMs) first prescribed during hospitalization and then continued at discharge and at one month
| PIMs prescribed during hospitalization (818/1,267a) | PIMs prescribed during hospitalization and at discharge (40/818) | PIMs prescribed during hospitalization, at discharge, and at one-month post-discharge (21/818) | ||||
|---|---|---|---|---|---|---|
| N | (%) | N | (%) | N | (%) | |
| TOTAL | 818 | (64.6) | 40 | (4.9) | 21 | (2.6) |
| Dexketoprofen | 209 | (16.5) | 5 | (0.6) | 0 | (0.0) |
| Midazolam | 202 | (15.9) | 0 | (0.0) | 0 | (0.0) |
| Diazepam | 78 | (6.2) | 6 | (0.7) | 2 | (0.2) |
| Doxazosin | 67 | (5.3) | 11 | (1.3) | 6 | (0.7) |
| Pethidine (meperidine) | 59 | (4.7) | 0 | (0.0) | 0 | (0.0) |
| Alprazolam | 40 | (3.2) | 1 | (0.1) | 1 | (0.1) |
| Clorazepate | 31 | (2.4) | 2 | (0.2) | 0 | (0.0) |
| Clonazepam | 27 | (2.1) | 8 | (1.0) | 7 | (0.9) |
| Paraffin | 25 | (2.0) | 1 | (0.1) | 1 | (0.1) |
| Zolpidem | 21 | (1.7) | 3 | (0.4) | 3 | (0.4) |
| Bromazepam | 18 | (1.4) | 0 | (0.0) | 0 | (0.0) |
| Diclofenac | 13 | (1.0) | 0 | (0.0) | 0 | (0.0) |
| Indomethacin | 6 | (0.5) | 0 | (0.0) | 0 | (0.0) |
| Fluoxetine | 5 | (0.4) | 0 | (0.0) | 0 | (0.0) |
| Paroxetine | 5 | (0.4) | 3 | (0.4) | 1 | (0.1) |
| Nifedipine | 4 | (0.3) | 0 | (0.0) | 0 | (0.0) |
| Clobazam | 2 | (0.2) | 0 | (0.0) | 0 | (0.0) |
| Pentoxifylline | 2 | (0.2) | 0 | (0.0) | 0 | (0.0) |
| Clonidine | 1 | (0.1) | 0 | (0.0) | 0 | (0.0) |
| Phenobarbital | 1 | (0.1) | 0 | (0.0) | 0 | (0.0) |
| Medazepam with amitriptyline | 1 | (0.1) | 0 | (0.0) | 0 | (0.0) |
| Prasugrel | 1 | (0.1) | 0 | (0.0) | 0 | (0.0) |
a Data available from 14 of the 16 participating hospitals
Discussion
The main aim of this study was to describe the use of PIMs among older adults in a representative sample of hospitals in Spain. The prevalence of PIMs at these 16 hospitals was considered moderate (23.5%), although the prevalence rate varied widely (from 10% to 42.5%) among the participating hospitals. Overall, the prevalence of PIMs was similar in men and women. However, of the 10 most commonly prescribed PIMs, eight were more common in women. The only two that were more common in men were pentoxifylline and doxazosin (a drug indicated for prostate hypertrophy).
In the literature, the prevalence of PIMs varies highly depending on the setting, the patients’ characteristics, the geographical region, and the criteria used to define PIMs, among other factors. In general, however, the reported prevalence is high. Interestingly, the prevalence is usually higher in nursing homes than in hospitals or in the community setting [11]. A systematic review was performed to assess the prevalence of PIP (all care settings) in older adults in Central and Eastern Europe, finding a median prevalence of 34.6% (range 6.5%-95.8%), however, as the authors of that review noted, the certainty of evidence was very low due to the risk of bias, imprecision, and inconsistency [5]. Thomas et al. carried out a systematic review to determine the prevalence of PIMs in adults over age 64. All of the studies included in that review used either the STOPP/START or Beers criteria. The prevalence of PIMs in studies that used the STOPP criteria was 42.8% in the community setting and 51.8% in the hospital setting. By contrast, in the studies that applied the Beers criteria, the prevalence rates in both settings were higher (58% and 55.5%, respectively) [43]. In the systematic review by Hill-Taylor et al., the prevalence of PIMs (STOPP criteria) was highly variable, ranging from 21.4% to 79%. However, as the authors emphasized, this large range should be interpreted cautiously due to the heterogeneity—in terms of the study population and study designs—of the studies included in that review [18]. A recent review involving > 370 million older outpatients from 17 countries reported a pooled PIM prevalence of 36.7% (95% CI: 33.4%-40.0%) worldwide and a prevalence of 35.0% (95% CI: 28.5%-41.8%) in Europe [44]. Another recent systematic review assessed the prevalence of PIMs in nursing homes, with prevalence rates ranging from 67.8% to 87.7% (STOPP criteria) [12].
In acute hospitalized patients, estimated prevalence rates for PIMs (STOPP criteria) range from 16 to 77% at the international level, and from 25 to 58% in Spain [11]. In recent years, several studies in Spain—mostly single center studies—have reported prevalence rates in hospitalized older patients ranging from 27 to 93% [3, 6, 10, 24]. In this context, the prevalence rate (23.5%) observed in our study falls within the lower range of those previous reports. The reason for this could be due to the use of different criteria to define PIM (different tools, domains, versions, etc.), the selection of patients with polypharmacy in some studies, the duration of the hospital stay, or that single center studies are not representative, among other reasons.
In the 16 hospitals included in our study, the most common PIMs were midazolam, dexketoprofen, diazepam, and doxazosin. In general, the most commonly used PIMs were psychotropic drugs, a finding that is consistent with previous reports showing that benzodiazepines are the most commonly prescribed PIMs in Spain in both inpatient and outpatient settings [38].
Two of the most common PIMs in our study were midazolam and dexketoprofen. Since midazolam is commonly administered in end-of-life situations and dexketoprofen in acute or postoperative cases (i.e., in the emergency room or surgical department), the initiation of both of these drugs during hospitalization is to be expected. In line with the prescribing patterns for those drugs, our data show that neither drug was prescribed before hospital admission; rather, they were both initiated during hospitalization.
Of the total number of PIMs (N = 1,407), 35% had been prescribed before hospital admission, mostly drugs indicated for the treatment of chronic conditions. Among these drugs, the use of benzodiazepines was particularly notable, a finding that is in line with previous studies carried out in Spain showing that the prevalence of anxiolytics, hypnotics, and sedatives in patients aged ≥ 75 is as high as 30% [7, 17]. At one-month post-discharge, the prevalence of PIMs remained virtually unchanged from the baseline (pre-admission) rate, which suggests that patients continued taking the same PIMs they had been taking before admission.
By contrast, of the PIMs that were first prescribed in the hospital, only 2.6% were still present at one-month after hospital discharge, indicating that the participating hospitals discontinued these PIMs prior to or shortly after discharge, which reflects an appropriate approach to the management of PIMs in these patients. We believe that the present study provides useful information about the prescription dynamics for PIMs in hospitalized older patients in our country. Our findings show that the PIMs prescribed prior to admission were not withdrawn during the hospital stay. Importantly, despite the temporary increase in PIMs during hospitalization, this did not lead to a significant increase in PIMs after discharge even though some studies have found a higher risk of increased PIM use after hospital admission [36].
In this study, we found that the patients’ regular (pre-admission) medications were maintained during hospitalization and after discharge. Although this could be considered a positive finding, it can also be seen as a missed opportunity to optimize the use of chronic medications in older patients. In other words, the hospital admission period could be an appropriate setting to review the regular medications taken by older patients, particularly given the availability of hospital pharmacists and/or multidisciplinary teams, who can consult directly with the patients and their family and closely monitor any medication-related changes. In addition, hospitals have clinical decision support systems in place to assist in this review process. In fact, many hospitals review benzodiazepine prescriptions in the acute care setting [31]. It is also important that hospital clinicians coordinate changes in medications after discharge with the patient’s primary care physician, especially because these physicians are the source of most prescriptions and responsible for coordinating the patient's treatment.
PIMs have been associated with a wide range of health- and system-related outcomes [46, 47]. In the hospital setting, PIP has been associated with a 91% increase in the risk of adverse drug event-related hospital admissions, a 60% increase in functional decline, a 26% increase in adverse drug reactions and drug-related events, and an increase in the risk of falls [27]. PIM use has also been associated with higher costs of hospitalization, increased health care expenses, and a greater number of visits to the emergency department for adverse drug events, regardless of the specific PIMs, health service, perspective, and/or screening tools used to identify the PIMs [39]. For all these reasons, in older inpatients, it is important to determine the prevalence of PIMs, the most common PIMs, and prescription patterns for chronic conditions both before and after admission. In this regard, the present study provides valuable data that help to better characterize these prescription patterns. Moreover, these data could be used to develop interventions to optimize treatment and deprescribe PIMs in older patients in the hospital setting.
The present study has several limitations. It is known that PIMs can include medications that are considered appropriate in some cases but inappropriate in others (e.g., comorbidities, impaired kidney function, concurrent treatments) or are considered inappropriate only when used long-term. Although these medications may be considered inappropriate, in many cases the tradeoff between risks and benefits must be assessed on an individual basis. Because of this, one limitation of the present study is that no information was collected regarding the prescription’s indications and that no individualized assessments were performed, which could imply that the use of some of these drugs was not inappropriate in all cases (e.g., midazolam in hospitalized patients requiring sedation towards the end-of-life). Another limitation is the lack of data on prescribing omissions, which could also be of interest. A final limitation is that we did not use a standardized list of PIMs, but rather one tailored to our country. Consequently, our findings may not be generalizable to other settings and/or countries.
The main strength of this study is the large number of participating hospitals (N = 16) covering a wide geographic area in Spain, which makes the study largely representative of the real-world conditions facing hospitalized older patients in Spain. Important, all hospitals used the same list of PIMs, thus ensuring data homogeneity. Another strength is that we considered prescriptions made before, during, and after hospitalization, and also determined when those prescriptions were first made (i.e., prior to or during admission) and the indication (acute vs. chronic). We also evaluated whether patients continued taking these drugs at hospital discharge and thereafter.
Conclusion
The results of this large multicenter study (16 hospitals) in Spain show a moderate prevalence for PIMs in this sample of older (≥ 75 years) hospitalized patients. However, prevalence rates at the participating hospitals were highly variable, ranging from 10% to 42.5%. There were no significant differences in prevalence rates between men and women. The most common PIMs were benzodiazepines, dexketoprofen, and doxazosin. In most cases, patients taking PIMs for chronic conditions prior to hospital admission continued to receive those same medications during the hospital stay. We did not observe any significant hospitalization-related increase in PIMs after discharge. The use of a unified PIMs list, incorporating validated criteria from Beers, STOPP-START, EU-PIM and PRISCUS tested in randomized controlled trials with relevant geriatric endpoints, has been essential to ensure consistency across hospitals. This study provides valuable data that could be used to plan multidisciplinary interventions in the hospital to optimize the pharmacological treatment of older adults and to improve the transition between primary and specialized care, thereby helping to reduce the negative effects of PIMs in this vulnerable population.
Supplementary Information
Acknowledgements
a Members of MAPAC-MPC Network:
Hospital de la Santa Creu i Sant Pau: Ignasi Bolíbar, Xavier Bonfill, Elisabeth Carreras, Ascensión García, Noé Garín, Ignasi Gich, Teresa Puig, M. Jesús Quintana, Carolina Requeijo, Laura Samsó, Ivan Sola, Gerard Urrútia.
CST-Consorci Sanitari de Terrassa: Santiago Castejón-Hernández, Mariona Roca Andreu, Verónica E. Ruiz Fernández, Antonio Sánchez Hidalgo.
Hospital de la Vall D’Hebron: Patricia Marrero, Dimelza Osorio, Maria Queralt Gorgas, Karla Salas-Gama.
Hospital Germans Trias i Pujol: Ignasi García-Olivé, Adrián Vilariño.
Hospital Gregorio Marañón: Irene Bretón Lesmes, Nicolás M. González-Senac, José Luis Revuelta Herrero.
Complex Hospitalari Universitari Moisès Broggi: Pedro Armario, Laura Losa López.
Parc Sanitari Sant Joan de Déu: Susana Álvarez Gómez, Beatriz del Pino Gaya.
Hospital de Cruces: Jaime Barroso Castro, Amaya Calleja Bueno, Monike de Miguel Gascón, Maialen Duque Rodriguez, Belén Moñino Blazquez, Jose Ignacio Pijoan Zubizarreta, Laura Serrano de Lucas.
Hospital Universitario de Navarra: Maite Sarobe-Carricas.
Hospital Donosti: María Asunción Aranguren Redondo, Iratxe Urreta-Barallobre.
Hospital San Eloy: Jaione Bilbao Aguirregomezcorta, Maria Lourdes Vivanco Gómez.
Hospital Universitario Basurto: Ana Aguirrezabal Arredondo, Montserrat Alonso Diez, Milagros Álvarez Lavín, Elixabete Ardanza Aramburu, Zuriñe Baskaran Kaltzagorta, Iker Elguezabal Ortuzar, Julia Fernández Uria, Isabel Fontán Basañez, Maialen Inclán Conde, Irune Loizaga Diaz, Ana Revuelta Amallo, Elena Ruiz de Velasco Artaza, Estíbaliz Tamayo Orbegozo, Clara Vila Gallego.
Hospital Zumárraga: Miren Arrieta Bernaras, Mª Isabel Fernández González, Elena Olloquiegui Biurrarena, José Luis Salsamendi Pérez.
Navarre Health Service (SNS-O): Juan Erviti, Marta Gutiérrez-Valencia, Leire Leache, Luis Carlos Saiz.
Hospital Sant Rafael: Celia González-Guerrero.
Authors’ contributions
TP, LL, NG-S, EC, MG-V, LL and NG made substantial contributions to the study conceptualization, design and methodology. TP and EC were responsible for project administration. TP, LL, NG-S, EC, MG-V, LL, JLR-H, PM-A, MdM, AAA, AA, AV, VER, IF, JB, CG-G, BdP and NG participated in the research data collection. TP, LL, NG-S, EC, MG-V, LL, and NG wrote the original draft of the manuscript. TP, LL, NG-S, EC, MG-V, LL, JLR-H, PM-A, MdM, AAA, AA, AV, VER, IF, JB, CG-G, BdP and NG helped to review and edit the manuscript. All authors approved the final version of the manuscript.
Funding
The authors declare that they have not received any funding for the research.
Availability of data and materials
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Declarations
Ethics approval and consent to participate
The study was approved by the Ethics Committee for Research with Medicinal Products (CEIM) of the Fundació de Gestió Sanitària de l’Hospital de la Santa Creu i Sant Pau. Informed consent has been waived by the Ethics Committee for Research with Medicinal Products (CEIM) of the Fundació de Gestió Sanitària de l’Hospital de la Santa Creu i Sant Pau, with reference code IIBSP-MAP-2021-146, as this was a retrospective observational study, using secondary and anonymized data, in the context of improving the appropriateness of healthcare. The study fully adhered to the principles of the Declaration of Helsinki. No written informed consent was deemed necessary for this study, according to the Ethics Committee for Research with Medicinal Products (CEIM) of the Fundació de Gestió Sanitària de l’Hospital de la Santa Creu i Sant Pau.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
T. Puig, Email: tpuig@santpau.cat
on behalf of the MAPAC-MPC Network:
T. Puig, N. M. González-Senac, E. Carreras, M. Gutiérrez-Valencia, J. L. Revuelta-Herrero, M. de Miguel, A. Aguirrezabal Arredondo, A. Aranguren, A. Vilariño, V. E. Ruiz, I. Fernández, J. Bilbao, C. González-Guerrero, B. del Pino, N. Garin, Ignasi Bolíbar, Xavier Bonfill, Ascensión García, Ignasi Gich, M Jesús Quintana, Carolina Requeijo, Laura Samsó, Ivan Sola, Gerard Urrútia, Santiago Castejón-Hernández, Mariona Roca Andreu, Antonio Sánchez Hidalgo, Patricia Marrero, Dimelza Osorio, Maria Queralt Gorgas, Karla Salas-Gama, Ignasi García-Olivé, Irene Bretón Lesmes, Pedro Armario, Laura Losa López, Susana Álvarez Gómez, Jaime Barroso Castro, Amaya Calleja Bueno, Maialen Duque Rodriguez, Belén Moñino Blazquez, Jose Ignacio Pijoan Zubizarreta, Laura Serrano de Lucas, Maite Sarobe-Carricas, Iratxe Urreta-Barallobre, Maria Lourdes Vivanco Gómez, Montserrat Alonso Diez, Milagros Álvarez Lavín, Elixabete Ardanza Aramburu, Zuriñe Baskaran Kaltzagorta, Iker Elguezabal Ortuzar, Julia Fernández Uria, Isabel Fontán Basañez, Maialen Inclán Conde, Irune Loizaga Diaz, Ana Revuelta Amallo, Elena Ruiz de Velasco Artaza, Estíbaliz Tamayo Orbegozo, Clara Vila Gallego, Miren Arrieta Bernaras, Elena Olloquiegui Biurrarena, José Luis Salsamendi Pérez, Juan Erviti, and Luis Carlos Saiz
References
- 1.American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2023 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2023. 10.1111/jgs.18372. Epub ahead of print.
- 2.American Geriatrics Society 2019 Updated AGS Beers Criteria® for Potentially Inappropriate Medication Use in Older Adults. J Am Geriatr Soc. 2019;67(4):674–94. 10.1111/jgs.15767. Epub 2019 Jan 29. [DOI] [PubMed]
- 3.Baré, M., Lleal, M., Sevilla-Sánchez, D., Ortonobes, S., Herranz, S., Ferrandez, O., Corral-Vázquez, C., Molist, N., Nazco, G. J., Martín-González, C., Márquez, M. Á., & Group, O. B. O. T. M. S. (2023). Sex differences in multimorbidity, inappropriate medication and adverse outcomes of inpatient care: MoPIM cohort study. Int J Environ Res Public Health. 20(4). 10.3390/ijerph20043639. [DOI] [PMC free article] [PubMed]
- 4.Bonfill X. Conceptos básicos para entender y mejorar la adecuación clínica. Educ Méd. 2023;24(3). 10.1016/j.edumed.2023.100813.
- 5.Brkic J, Fialova D, Okuyan B, Kummer I, Sesto S, Capiau A, Hadziabdic MO, Tachkov K, Bobrova V. Prevalence of potentially inappropriate prescribing in older adults in Central and Eastern Europe: a systematic review and synthesis without meta-analysis. Sci Rep. 2022;12(1):16774. 10.1038/s41598-022-19860-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Caro Teller J, Ortiz Perez S, Gonzalez Sevilla M, Jimenez Cerezo M, Gonzalez Gomez C, Ferrari Piquero J. Influence of a pharmaceutical intervention program on the use of potentially inappropriate medications in elderly patients. Eur J Clin Pharm. 2018;20(4):197–203. [Google Scholar]
- 7.Cebrino J, Portero de la Cruz S. Polypharmacy and associated factors: a gender perspective in the elderly Spanish population (2011–2020). Front Pharmacol. 2023;14:1189644. 10.3389/fphar.2023.1189644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Davidoff AJ, Miller GE, Sarpong EM, Yang E, Brandt N, Fick DM. Prevalence of potentially inappropriate medication use in older adults using the 2012 Beers criteria. J Am Geriatr Soc. 2015;63(3):486–500. 10.1111/jgs.13320. Epub 2015 Mar 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Davies LE, Spiers G, Kingston A, Todd A, Adamson J, Hanratty B. Adverse outcomes of polypharmacy in older people: systematic review of reviews. J Am Med Dir Assoc. 2020;21(2):181–7. 10.1016/j.jamda.2019.10.022. Epub 2020 Jan 8. [DOI] [PubMed] [Google Scholar]
- 10.de Agustín Sierra L, Rodríguez Salazar J, Jiménez-Muñoz AB, Molina Hernández MJ, Bermejo Bescós P, Iglesias Peinado I, García Díaz B. Potentially inappropriate medication in acute hospitalized elderly patients with polypharmacy: an observational study comparing PRISCUS, STOPP, and Beers criteria. Eur J Clin Pharmacol. 2021;77(5):757–66. 10.1007/s00228-020-03022-8. [DOI] [PubMed] [Google Scholar]
- 11.Delgado Silveira E, Montero Errasquín B, Muñoz García M, Vélez-Díaz-Pallarés M, Lozano Montoya I, Sánchez-Castellano C, Cruz-Jentoft AJ. Improving drug prescribing in the elderly: a new edition of STOPP/START criteria. Rev Esp Geriatr Gerontol. 2015;50(2):89–96. 10.1016/j.regg.2014.10.005. [DOI] [PubMed] [Google Scholar]
- 12.Díaz Planelles, I., Navarro-Tapia, E., García-Algar, Ó., & Andreu-Fernández, V. Prevalence of potentially inappropriate prescriptions according to the new STOPP/START criteria in nursing homes: a systematic review. Healthcare (Basel, Switzerland). 2023;11(3). 10.3390/healthcare11030422. [DOI] [PMC free article] [PubMed]
- 13.Fried TR, O’Leary J, Towle V, Goldstein MK, Trentalange M, Martin DK. Health outcomes associated with polypharmacy in community-dwelling older adults: a systematic review. J Am Geriatr Soc. 2014;62(12):2261–72. 10.1111/jgs.13153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Garin N, Sole N, Lucas B, Matas L, Moras D, Rodrigo-Troyano A, Gras-Martin L, Fonts N. Drug related problems in clinical practice: a cross-sectional study on their prevalence, risk factors and associated pharmaceutical interventions. Sci Rep. 2021;11(1):883. 10.1038/s41598-020-80560-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.GranMo. Sample size calculator. https://www.imim.es/ofertadeserveis/software-public/granmo. Accessed 2023 June 9.
- 16.Gutiérrez-Valencia M, Martínez-Velilla N, Vilches-Moraga A. Polypharmacy in older people: time to take action. Eur Geriatr Med. 2019F;10(1):1–3. 10.1007/s41999-018-0140-5. Epub 2018 Nov 30. [DOI] [PubMed] [Google Scholar]
- 17.Gutiérrez-Valencia M, Aldaz Herce P, Lacalle-Fabo E, Contreras Escámez B, Cedeno-Veloz B, Martínez-Velilla N. Prevalence of polypharmacy and associated factors in older adults in Spain: Data from the National Health Survey 2017. Med Clin. 2019. 10.1016/j.medcli.2018.12.013. [DOI] [PubMed]
- 18.Hill-Taylor B, Sketris I, Hayden J, Byrne S, O’Sullivan D, Christie R. Application of the STOPP/START criteria: a systematic review of the prevalence of potentially inappropriate prescribing in older adults, and evidence of clinical, humanistic and economic impact. J Clin Pharm Ther. 2013;38(5):360–72. 10.1111/jcpt.12059. [DOI] [PubMed] [Google Scholar]
- 19.Holt S, Schmiedl S, Thürmann PA. Potentially inappropriate medications in the elderly: the PRISCUS list. Dtsch Arztebl Int. 2010;107(31-32):543–51. 10.3238/arztebl.2010.0543. Epub 2010 Aug 9. [DOI] [PMC free article] [PubMed]
- 20.Krähenbühl-Melcher A, Schlienger R, Lampert M, Haschke M, Drewe J, Krähenbühl S. Drug-related problems in hospitals: a review of the recent literature. Drug Saf. 2007;30:379–407. 10.2165/00002018-200730050-00003. [DOI] [PubMed] [Google Scholar]
- 21.Liew TM, Lee CS, Goh SKL, Chang ZY. The prevalence and impact of potentially inappropriate prescribing among older persons in primary care settings: multilevel meta-analysis. Age Ageing. 2020; 49(4):570–9. 10.1093/ageing/afaa057. [DOI] [PubMed]
- 22.Lockery JE, Collyer TA, Woods RL, Orchard SG, Murray A, Nelson MR, Stocks NP, Wolfe R, Moran C, Ernst ME; ASPREE Investigator Group. Potentially inappropriate medication use is associated with increased risk of incident disability in healthy older adults. J Am Geriatr Soc. 2023. 10.1111/jgs.18353. Epub ahead of print. [DOI] [PMC free article] [PubMed]
- 23.Maher RL, Hanlon J, Hajjar ER. Clinical consequences of polypharmacy in elderly. Expert Opin Drug Saf. 2014;13(1):57–65. 10.1517/14740338.2013.827660. Epub 2013 Sep 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Marín-Gorricho, R., Lozano, C., Torres, C., Ramalle-Gómara, E., Hurtado-Gómez, M. F., Pérez-Zuazo, R., & Molpeceres-García Del Pozo, J. Impact of pharmaceutical care in polymedicated patients admitted to a geriatric ward. An Sist Sanit Navar. 2022;45(1). 10.23938/ASSN.0990. [DOI] [PMC free article] [PubMed]
- 25.Martin-Pérez M, et al. Prevalencia de polifarmacia en la población mayor de 65 años en España: análisis de las Encuestas Nacionales de Salud 2006 y 2011/12. Rev Esp Geriatr Gerontol. 2017;52:2–8. [DOI] [PubMed] [Google Scholar]
- 26.Mathes T, Sönnichsen A, Pieper D, Klager E, Moussa M, Thürmann PA. Potentially Inadequate Medications in the Elderly: PRISCUS 2.0—First Update of the PRISCUS List. Dtsch Arztebl Int. 2023;120(Forthcoming):3–10. 10.3238/arztebl.m2022.0377. [DOI] [PMC free article] [PubMed]
- 27.Mekonnen AB, Redley B, de Courten B, Manias E. Potentially inappropriate prescribing and its associations with health-related and system-related outcomes in hospitalized older adults: a systematic review and meta-analysis. Br J Clin Pharmacol. 2021;87(11):4150–72. 10.1111/bcp.14870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Morin L, Johnell K, Laroche M-L, Fastbom J, Wastesson JW. The epidemiology of polypharmacy in older adults: register based prospective cohort study. Clin Epidemiol. 2018;10:289–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Muhlack DC, Hoppe LK, Weberpals J, Brenner H, Schöttker B. The association of potentially inappropriate medication at older age with cardiovascular events and overall mortality: a systematic review and meta-analysis of cohort studies. J Am Med Dir Assoc. 2017;18(3):211–20. 10.1016/j.jamda.2016.11.025. [DOI] [PubMed]
- 30.National Center for Health Statistics (US). Health, United States, 2016: with chartbook on long-term trends in health. Hyattsville (MD): National Center for Health Statistics (US); 2017 May. Report No.: 2017–1232. [PubMed]
- 31.Neville HL, Granter C, Adibi P, Belliveau J, Isenor JE, Bowles SK. Interventions to reduce benzodiazepine and sedative-hypnotic drug use in acute care hospitals: a scoping review. Res Social Adm Pharm. 2022M;18(5):2874–86. 10.1016/j.sapharm.2021.07.004. Epub 2021 Jul 6. [DOI] [PubMed] [Google Scholar]
- 32.Olmos R, Garcia O, Velasco J, de la Rubia A. Prevalence of polypharmacy in older hospitalized patients. Eur J Hosp Pharm. 2012;19(242):3–243. [Google Scholar]
- 33.O’Mahony D, Cherubini A, Guiteras AR, et al. STOPP/START criteria for potentially inappropriate prescribing in older people: version 3. Eur Geriatr Med. 2023. 10.1007/s41999-023-00777-y. [DOI] [PMC free article] [PubMed]
- 34.O'Mahony D, O'Sullivan D, Byrne S, O'Connor MN, Ryan C, Gallagher P. STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing. 2015;44(2):213–8. 10.1093/ageing/afu145. [DOI] [PMC free article] [PubMed]
- 35.Pagès A, Rouch L, Costa N, Cestac P, De Souto Barreto P, Rolland Y, Vellas B, Molinier L, Juillard-Condat B, Mapt/Dsa Group. Potentially inappropriate medication prescribing detected by computer algorithm among older patients: results from the MAPT study. Pharmacy (Basel). 2021;9(4):189. 10.3390/pharmacy9040189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pérez T, Moriarty F, Wallace E, McDowell R, Redmond P, Fahey T. Prevalence of potentially inappropriate prescribing in older people in primary care and its association with hospital admission: longitudinal study. BMJ. 2018;14(363):k4524. 10.1136/bmj.K4524.PMID:30429122;PMCID:PMC6233705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Renom-Guiteras A, Meyer G, Thürmann PA. The EU(7)-PIM list: a list of potentially inappropriate medications for older people consented by experts from seven European countries. Eur J Clin Pharmacol. 2015;71(7):861–75. 10.1007/s00228-015-1860-9. Epub 2015 May 14. [DOI] [PMC free article] [PubMed]
- 38.Salgueiro, E., Elizarde, B. C., Elola, A. I., García-Pulido, B., Nicieza-García, M. L., & Manso, G. The most common STOPP/START criteria in Spain. A review of the literature. Rev Esp Geriatr Gerontol. 2018;53(5):274–278. 10.1016/j.regg.2018.03.001. [DOI] [PubMed]
- 39.Schiavo G, Forgerini M, Lucchetta RC, Silva GO, Mastroianni PDC. Cost of adverse drug events related to potentially inappropriate medication use: a systematic review. J Am Pharm Assoc: JAPhA. 2022;62(5):1463–1476.e14. 10.1016/j.japh.2022.04.008. [DOI] [PubMed] [Google Scholar]
- 40.Servei Català de la Salut, Gerència del Medicament. Fàrmacs potencialment inapropiats per a persones d’edat avançada. Barcelona: Servei Català de la Salut; 2020. https://catsalut.gencat.cat/web/.content/minisite/catsalut/proveidors_professionals/medicaments_farmacia/catsalut-entitats/transversals/farmacs-pot-inapropiats-pacients-ed-avancada-v2020.pdf. [Google Scholar]
- 41.Simon SR, Chan KA, Soumerai SB, Wagner AK, Andrade SE, Feldstein AC, Lafata JE, Davis RL, Gurwitz JH. Potentially inappropriate medication use by elderly persons in U.S. Health Maintenance Organizations, 2000–2001. J Am Geriatr Soc. 2005;53(2):227–32. 10.1111/j.1532-5415.2005.53107. [DOI] [PubMed] [Google Scholar]
- 42.Sloane PD, Zimmerman S, Brown LC, Ives TJ, Walsh JF. Inappropriate medication prescribing in residential care/assisted living facilities. J Am Geriatr Soc. 2002;50(6):1001–11. 10.1046/j.1532-5415.2002.50253.x. [DOI] [PubMed] [Google Scholar]
- 43.Thomas RE, Thomas BC. A systematic review of studies of the STOPP/START 2015 and American Geriatric Society Beers 2015 criteria in patients ≥ 65 years. Curr Aging Sci. 2019;12(2):121–54. 10.2174/1874609812666190516093742. [DOI] [PubMed] [Google Scholar]
- 44.Tian F, Chen Z, Zeng Y, Feng Q, Chen X. Prevalence of use of potentially inappropriate medications among older adults worldwide: a systematic review and meta-analysis. JAMA Netw Open. 2023;6(8). 10.1001/jamanetworkopen.2023.26910. [DOI] [PMC free article] [PubMed]
- 45.Turnheim K. When drug therapy gets old: pharmacokinetics and pharmacodynamics in the elderly. Exp Gerontol. 2003;38(8):843–53. 10.1016/s0531-5565(03)00133-5. [DOI] [PubMed] [Google Scholar]
- 46.Weeda ER, AlDoughaim M, Criddle S. Association between potentially inappropriate medications and hospital encounters among older adults: a meta-analysis. Drugs Aging. 2020;37(7):529–37. 10.1007/s40266-020-00770-1. [DOI] [PubMed] [Google Scholar]
- 47.Xing XX, Zhu C, Liang HY, Wang K, Chu YQ, Zhao LB, Jiang DC, Wang YQ, Yan SY. Associations between potentially inappropriate medications and adverse health outcomes in the elderly: a systematic review and meta-analysis. Ann Pharmacother. 2019;53(10):1005–19. 10.1177/1060028019853069. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analysed during this study are included in this published article [and its supplementary information files].