Abstract
Background
Rheumatic heart disease (RHD) is a major global health issue because of its potential to cause heart failure. While RHD has been reported more frequently in women, this case report highlights the clinical manifestations, diagnosis, and management of rheumatic multivalvular disease in a young Asian male.
Case summary
A 46-year-old Asian man with a history of percutaneous mitral valvuloplasty (PMV) was admitted with dyspnoea and generalized oedema that severely hindered his quality of life. Transthoracic and transoesophageal echocardiography revealed severe mitral stenosis, left atrial appendage (LAA) thrombus, and severe tricuspid regurgitation due to RHD. Following a comprehensive evaluation by a multidisciplinary team, we advised mitral valve replacement, LAA thrombectomy, and tricuspid valve annuloplasty based on the detailed imaging of the valve anatomy and the patient’s low surgical risk. Surgical intervention led to considerable improvement in the patient’s symptoms, enabling a return to routine activities.
Discussion
This case highlights the chronic nature of RHD and its potential to cause heart failure. This report emphasizes the need for regular follow-up in patients with a history of RHD to detect potential complications and ensure timely management. The successful outcome in this case underscores the importance of a team-based approach for managing complex valvular heart disease.
Keywords: Rheumatic heart disease, Mitral stenosis, Tricuspid regurgitation, Young Asian male, Case report
Learning points.
Rheumatic heart disease (RHD) can manifest as multivalvular disease, and the use of advanced techniques, including 3D imaging, is necessary for accurate diagnosis.
The prevalence of RHD is low in developed countries but remains high in developing countries; globally, it constitutes a significant proportion of young patients with heart failure. A guideline-based multidisciplinary approach plays a crucial role in the treatment of complex rheumatic valvular heart disease.
Long-term management and patient education are essential aspects of patient care. Patients with RHD should be informed that it is a chronic and progressive condition, and regular follow-up and timely management are important.
Introduction
Globally, 40.5 million people have rheumatic heart disease (RHD).1 Rheumatic heart disease occurs predominantly in women (70%–80%) and is often first diagnosed during pregnancy, wherein the increased blood volume can precipitate heart failure.2,3 Although its prevalence has declined in developed countries, globalization, migration, and refugee crises have made RHD a global health problem that is not confined to developing countries.4,5 Rheumatic heart disease predominantly affects the mitral valve (MV), followed by the aortic valve (AV), with rare tricuspid valve (TV) involvement.6 Herein, we report the surgical treatment of a young East Asian patient with heart failure due to severe mitral stenosis (MS) and tricuspid regurgitation (TR) caused by RHD.
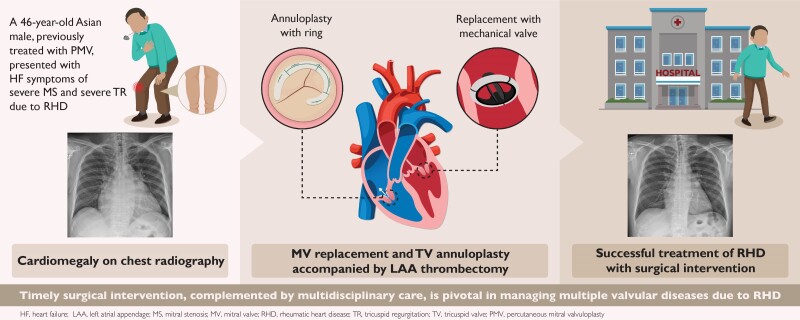
Summary figure
Case description
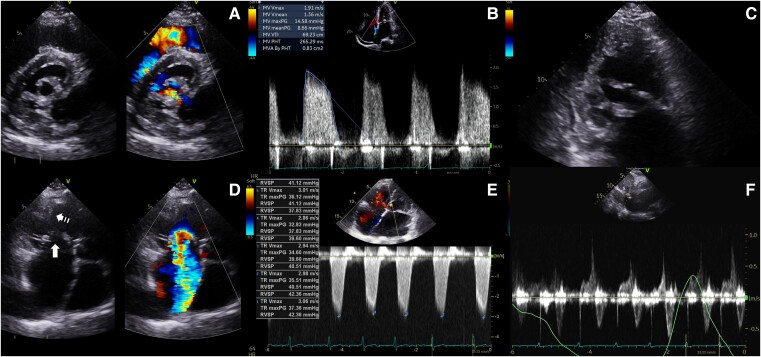
A 46-year-old man visited our hospital with generalized oedema and dyspnoea. His New York Heart Association class was III, and physical examination revealed grade 3 pitting oedema in both legs. He had undergone percutaneous mitral valvuloplasty (PMV) 15 years ago for severe MS but did not have regular follow-ups because his symptoms improved after PMV. Chest radiography revealed cardiomegaly; moreover, the NT-pro-brain natriuretic peptide level was elevated to 1031.0 pg/mL (normal range < 83.9 pg/mL for age < 55 years). Transthoracic echocardiography (TTE) revealed diastolic doming and commissural fusion with a fibro-thickened MV, consistent with rheumatic MS. The mean transvalvular pressure gradient (PG) was 8.7 mmHg, with a Wilkins score of 11 (Figure 1A and B; Supplementary material online, Video S1). This score comprised 3 points for leaflet mobility, 3 for leaflet thickening, 4 for subvalvular thickening, and 1 for calcification (Figure 1C). The opening motion of the AV was unimpeded, and the peak velocity was 1.4 m/s. Simultaneously, the TV had fibro-thickened leaflets and hypertrophied papillary muscles, indicating rheumatic involvement. The thickened leaflets did not close properly, causing severe TR, as evidenced by a dilated annulus measuring 47 mm, vena contracta width of 15 mm, dense TR Doppler signal (Figure 1C and D; Supplementary material online, Video S2), and systolic flow reversal at the hepatic vein (Figure 1E). The effective regurgitant orifice area (EROA), calculated using the proximal isovelocity surface area method, was 77.4 mm2, and the regurgitant volume was 71.8 mL, both of which indicated severe TR. The right ventricular systolic pressure (RVSP) was elevated at 51 mmHg. The patient presented with concomitant severe rheumatic MS and TR, with a Wilkins score > 8, indicating the need for surgical intervention. However, he opted for PMV again and did not wish to undergo surgery.
Figure 1.
Pre-operative transoesophageal echocardiography demonstrates a thickened and fused mitral valve with an elevated PG of 8.7 mmHg (A and B). The distal parts of the mitral valve chordae are also thickened, reflecting subvalvular involvement indicative of rheumatic heart disease (C). Additionally, the tricuspid valve leaflets (arrow) and papillary muscles (dotted arrow) show thickening (D). The estimated right ventricular systolic pressure is elevated to 57 mmHg (E). Systolic flow reversal is observed in the hepatic vein (F). MV, mitral valve; PG, pressure gradient; RHD, rheumatic heart disease; RVSP, right ventricular systolic pressure; TOE, transoesophageal echocardiography; TV, tricuspid valve.
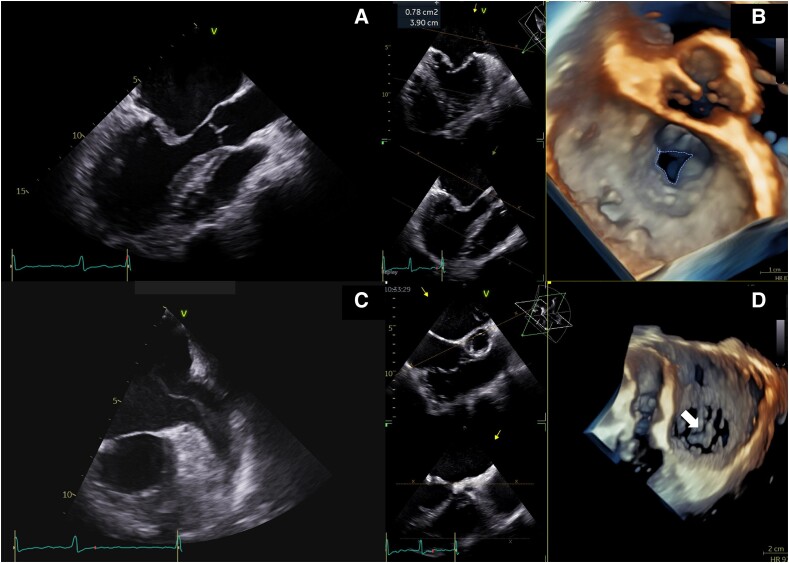
We performed transoesophageal echocardiography (TOE) to further characterize the valvular pathology and provide the patient with comprehensive clinical information to weigh his decision. Transoesophageal echocardiography revealed further rheumatic features, including thickening and fusion of the MV and valve area of 0.78 cm² (Figure 2A and B; Supplementary material online, Video S3). Spontaneous echo contrast and a hypoechogenic layer suggesting a thrombus were observed in the left atrium (LA) and left atrial appendage (LAA) (Figure 2C). The TV showed thickening and annular dilatation, causing severe regurgitation with a clearly visible coaptation gap on 3D imaging (Figure 2D; Supplementary material online, Video S4). A multidisciplinary heart team specializing in heart failure, cardiac imaging, cardiothoracic surgery, and anaesthesiology determined the further treatment strategy including MV replacement based on the high Wilkins score and presence of an LAA thrombus. Annuloplasty was planned for the TV instead of valve replacement to prevent annular dilatation causing coaptation failure. Our team emphasized that PMV alone is inadequate for managing heart failure caused by multivalvular disease. Eventually, the patient agreed to undergo open-heart surgery.
Figure 2.
Transoesophageal echocardiography provides clearer visualization of rheumatic heart disease. The mitral valve leaflets are thickened and fused (A). Additionally, the mitral valve area, measured via planimetry in the 3D enface view, is 0.78 cm2, indicating severe stenosis (B). Severe swelling is noted in the left atrium and left atrial appendage (C). The tricuspid valve is thickened, and a coaptation gap is visible on the 3D image (arrow) (D). LA, left atrium; LAA, left atrial appendage; MV, mitral valve; RHD, rheumatic heart disease; TV, tricuspid valve.
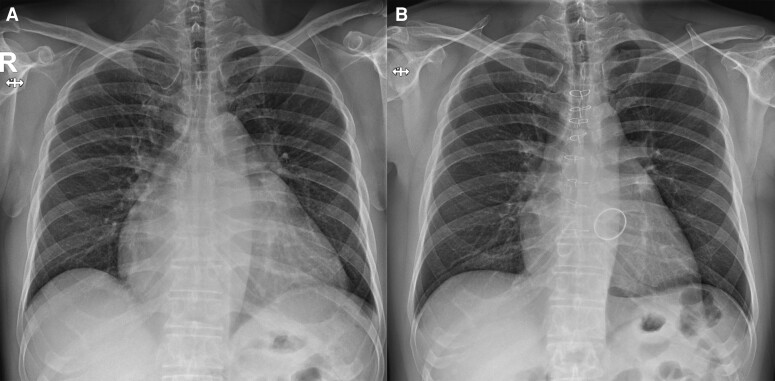
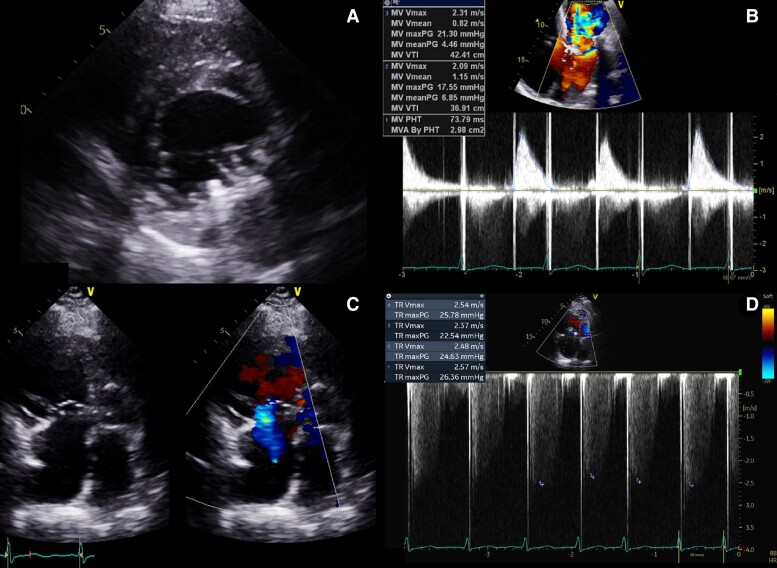
Mitral valve replacement with a 31 mm Master mechanical prosthesis (Abbott, Burlington, MA, USA) and TV annuloplasty with a 34 mm MC3 ring (Edwards Lifesciences, Irvine, CA, USA) were performed. The presence of a thrombus in the LAA necessitated thrombectomy and internal obliteration. Follow-up TTE revealed optimal performance of the mechanical MV with a reduced mean PG (4.9 mmHg) (Figure 3A and B; Supplementary material online, Video S5). Mild TR remained, with an RVSP of 35 mmHg (Figure 3D; Supplementary material online, Video S6). Post-operative chest radiography revealed a reduction in cardiomegaly (Figure 4). The patient’s weight remained stable at 80 kg, and oedema in both legs resolved. He was discharged on post-operative day 10 and is currently undergoing outpatient follow-up.
Figure 3.
Chest radiography on admission (A) and before discharge (B). The heart size has decreased after surgery, and the mechanical mitral valve and tricuspid annuloplasty ring are visible. MV, mitral valve.
Figure 4.
Post-operative transoesophageal echocardiography imaging. The well-functioning mechanical mitral valve with a mean diastolic pressure gradient of 4.9 mmHg is observed (A and B). The tricuspid valve annulus diameter decreases from 47 to 40 mm after annuloplasty, and regurgitation improves to a mild degree (C). The estimated right ventricular systolic pressure is reduced from 51 to 35 mmHg (D). MV, mitral valve; RVSP, right ventricular systolic pressure; TTE, transoesophageal echocardiography; TV, tricuspid valve.
Discussion
Rheumatic heart disease is a neglected disease relative to its burden and remains the leading cause of heart failure among children and young adults worldwide.1,2 Rheumatic heart disease often results from cumulative valve damage due to recurrent minimally symptomatic episodes of acute rheumatic fever. Consequently, the initial RHD symptoms manifest later in life (30–50 years of age).1,7,8 Although RHD predominantly affects females, the reasons for the sex-related differences in prevalence rates remain unclear.6,7 We report a rare case of a man with RHD who first experienced dyspnoea in his thirties. After PMV, he discontinued follow-up assessments as his symptoms improved. However, a persistent inflammatory response due to rheumatic fever can continue damaging the valves; thus, a single PMV procedure may be insufficient to cure RHD. Furthermore, no specific medical treatment has been established to retard disease progression; hence, regular monitoring of valvular function and its potential complications, including heart failure and infective endocarditis, is essential.7,8
According to the guidelines, clinically significant moderate-to-severe MS is defined by an MV area < 1.5 cm², measured using planimetry from echocardiography.9 Our patient’s MV area was 0.78 cm², indicating anatomically severe MS, but there was a discrepancy because the transvalvular PG was <10 mmHg. El Sabbagh et al.10 reported that the severe low-gradient MS population had greater male predominance and often exhibited lower stroke volumes. Conditions, including atrial fibrillation, which reduce effective filling of the left ventricle (LV), may decrease the gradient across the MV despite a significantly reduced valve area.
In our patient, the lower PG can be attributed to low flow conditions, potentially due to atrial fibrillation or reduced stroke volume (stroke volume index = 23 mL/m²). Additionally, the decreased LV stroke volume index, despite a preserved LV ejection fraction, can be explained by the decline in right ventricular stroke volume due to severe TR.
The management of RHD, especially the multivalvular disease phenotype, necessitates team-based decision-making owing to limited treatment-related data.9,11 The TV is comparatively less affected by RHD than the MV.6 Over 90% of severe TR cases are secondary; however, in this patient, RHD caused thickening of the valve and surrounding structures and annular dilatation, leading to combined primary and secondary TR. Nonetheless, our cardiology team identified coaptation failure as the primary issue using 3D imaging. Furthermore, the current guidelines suggest that whenever possible, annuloplasty with prosthetic rings is preferable for valve replacement.9 Our team chose annuloplasty instead of TV replacement, eliciting successful outcomes. Furthermore, 3D TOE is pivotal for accurate assessment of valvular lesion severity and recommendation for surgical treatment over PMV for severe MS alone. Kim et al.12 suggested that MV replacement may be preferable when there is no clear indication of a suitable morphology for PMV. Additionally, the presence of an LAA thrombus necessitates further surgical intervention, reflecting the importance of a comprehensive pre-operative evaluation to prevent potential embolic complications.
This case report of a young Asian man diagnosed with RHD manifesting as severe MS and TR provides clinical insights into the challenges and considerations in managing complex valvular heart diseases. It highlights the role of cutting-edge diagnostic techniques including 3D echocardiography and a multidisciplinary approach for successful outcomes.
Lead author biography

Kyu-Yong Ko, MD, graduated in 2009 from Inha University, South Korea. He completed his fellowship at Severance Hospital in 2022 and currently serves as an assistant professor at Inje University’s Ilsan Paik Hospital. His clinical interests include cardiovascular imaging, with a focus on echocardiography, and heart failure.
Supplementary Material
Contributor Information
Kyu-Yong Ko, Division of Cardiology, Department of Internal Medicine, Ilsan Paik Hospital, Inje University College of Medicine, 170 Juwha-ro, Ilsanseo-gu, Goyang-si, Gyeonggi-do 10380, Republic of Korea.
Sung Eun Kim, Division of Cardiology, Department of Internal Medicine, Ilsan Paik Hospital, Inje University College of Medicine, 170 Juwha-ro, Ilsanseo-gu, Goyang-si, Gyeonggi-do 10380, Republic of Korea.
Ji-Won Hwang, Division of Cardiology, Department of Internal Medicine, Ilsan Paik Hospital, Inje University College of Medicine, 170 Juwha-ro, Ilsanseo-gu, Goyang-si, Gyeonggi-do 10380, Republic of Korea.
Sung Woo Cho, Division of Cardiology, Department of Internal Medicine, Ilsan Paik Hospital, Inje University College of Medicine, 170 Juwha-ro, Ilsanseo-gu, Goyang-si, Gyeonggi-do 10380, Republic of Korea.
Jae-Jin Kwak, Division of Cardiology, Department of Internal Medicine, Ilsan Paik Hospital, Inje University College of Medicine, 170 Juwha-ro, Ilsanseo-gu, Goyang-si, Gyeonggi-do 10380, Republic of Korea.
Supplementary material
Supplementary material is available at European Heart Journal – Case Reports online.
Ethical statement and statement of consent: This report was approved by the Institutional Review Board of the Inje University Ilsan Paik Hospital (no. 2024-03-024). The authors confirm that written consent for submission and publication of this case report including the images and associated text have been obtained from the patient in line with COPE guidelines.
Funding: None declared.
Data availability
The data underlying this article are available in the article and in its online Supplementary material.
References
- 1. Ghamari SH, Abbasi-Kangevari M, Moghaddam SS, Aminorroaya A, Rezaei N, Shobeiri P, et al. Rheumatic heart disease is a neglected disease relative to its burden worldwide: findings from global burden of disease 2019. J Am Heart Assoc 2022;11:e025284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Silbiger JJ. Advances in rheumatic mitral stenosis: echocardiographic, pathophysiologic, and hemodynamic considerations. J Am Soc Echocardiogr 2021;34:709–722.e1. [DOI] [PubMed] [Google Scholar]
- 3. He VY, Condon JR, Ralph AP, Zhao Y, Roberts K, de Dassel JL, et al. Long-term outcomes from acute rheumatic fever and rheumatic heart disease: a data-linkage and survival analysis approach. Circulation 2016;134:222–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Watkins DA, Johnson CO, Colquhoun SM, Karthikeyan G, Beaton A, Bukhman G, et al. Global, regional, and national burden of rheumatic heart disease, 1990–2015. N Engl J Med 2017;377:713–722. [DOI] [PubMed] [Google Scholar]
- 5. Abouzeid M, Wyber R, La Vincente S, Sliwa K, Zühlke L, Mayosi B, et al. Time to tackle rheumatic heart disease: data needed to drive global policy dialogues. Glob Public Health 2019;14:456–468. [DOI] [PubMed] [Google Scholar]
- 6. Zühlke L, Engel ME, Karthikeyan G, Rangarajan S, Mackie P, Cupido B, et al. Characteristics, complications, and gaps in evidence-based interventions in rheumatic heart disease: the Global Rheumatic Heart Disease Registry (the REMEDY study). Eur Heart J 2015;36:1115–1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Marijon E, Mirabel M, Celermajer DS, Jouven X. Rheumatic heart disease. Lancet 2012;379:953–964. [DOI] [PubMed] [Google Scholar]
- 8. Watkins DA, Beaton AZ, Carapetis JR, Karthikeyan G, Mayosi BM, Wyber R, et al. Rheumatic heart disease worldwide: JACC scientific expert panel. J Am Coll Cardiol 2018;72:1397–1416. [DOI] [PubMed] [Google Scholar]
- 9. Vahanian A, Beyersdorf F, Praz F, Milojevic M, Baldus S, Bauersachs J, et al. 2021 ESC/EACTS guidelines for the management of valvular heart disease: developed by the task force for the management of valvular heart disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J 2022;43:561–632.34453165 [Google Scholar]
- 10. El Sabbagh A, Reddy YN, Barros-Gomes S, Borlaug BA, Miranda WR, Pislaru SV, et al. Low-gradient severe mitral stenosis: hemodynamic profiles, clinical characteristics, and outcomes. J Am Heart Assoc 2019;8:e010736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Members WC, Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP III, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol 2021;77:e25–e197. [DOI] [PubMed] [Google Scholar]
- 12. Kim D-Y, Cho I, Kim K, Gwak SY, Ha KE, Lee HJ, et al. Outcomes of severe mitral stenosis with the revised severity criteria: mitral valve replacement vs percutaneous mitral valvuloplasty. Can J Cardiol 2024;40:100–109. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article are available in the article and in its online Supplementary material.