Abstract
Background
The life-threatening diseases known as ACS (acute coronary syndrome) continue to produce considerable rates of morbidity and mortality despite breakthroughs in therapy. The study determined clinical outcome and its predictors in patients at the University of Gondar Comprehensive and Specialized Hospital (UOGCSH), North West Ethiopia.
Design, setting, and participants
A retrospective cohort study design was employed at UOGCSH from January 31, 2018 to February 1, 2023. The hospital used a systematic random sampling procedure to select study participants from the medical records of patients in chronic cardiac follow-up clinics.
Main outcome measures
Exposures were optimal medical therapy (OMT) versus non-optimal medical therapy collected from May to August 2023. Descriptive and analytical statistics were employed to compare study groups. A binary logistic regression model was employed to identify candidate variables for further analysis. Cox's proportional hazard model and log-rank test were employed, with a P-value < 0.05 used to evaluate statistical significance. A five-year all-cause mortality after discharge estimate was displayed by using Kaplan–Meier curves.
Results
Among 422 patients with ACS [mean age, 61.56 (SD = 9.686) years; 54.7% male], of whom only 59.2% (250) received optimal medical therapy at discharge. Age ≥ 65, atrial fibrillation, chronic kidney diseases, and cardiogenic shock were negative independent predictors of optimal medical therapy. On the other hand, male sex was independently associated with the use of optimal medical therapy. All-cause mortality occurred in 16.6% (n = 70) and major adverse cardiac events occurred in 30.8% (n = 130) of patients with a 95% CI of 0.132–0.205 and 0.264–0.355, respectively. Multivariate analyses indicated that OMT was significantly associated with reduced all-cause mortality (aHR: 0.431, 95% CI: 0.222–0.835; P = 0.013).
Conclusion
This study revealed that the use of preventive OMT in patients discharged with acute coronary syndrome was associated with a reduction in all-cause mortality. However, the use of this OMT is suboptimal.
Keywords: Acute coronary syndrome, Clinical outcome, Optimal medical therapy, Gondar, Ethiopia
Introduction
One of the main causes of mortality globally, cardiovascular illnesses continue to have a significant impact on morbidity, mortality, and healthcare costs [1, 2]. The term "acute coronary syndrome" (ACS) explains a variety of illnesses that are indicative of an abrupt decrease in coronary blood flow and are therefore consistent with acute myocardial infarction [3, 4]. The formation of coronary atherosclerotic plaque, which causes intracoronary thrombosis and ischemia, is the most frequent cause of ACS. Prolonged cessation of coronary blood flow can result in myocyte necrosis or infarction [5, 6]. Despite advancements in therapy, ACS, which encompasses unstable angina and myocardial infarction (MI) with and without ST-segment elevation, remains a life-threatening condition with significant rates of morbidity and mortality [3]. It is estimated that there are 7 million cases of ACS worldwide, making it one of the most prevalent diseases globally [4, 5].
Among the most recent years for which information is available, cardiovascular disease continued to be the leading cause of death among the member nations of the European Society of Cardiology (ESC), accounting for slightly over 1.9 million deaths in men and slightly under 2.2 million deaths in women. These account for 45 percent of all deaths in the case of women and 39 percent in the case of males. The most frequent cause of CVD mortality, ischemic heart disease, accounts for 44% of fatalities from the condition in men and 38% in women [7]. The most prevalent illness in Africa is ACS, with a pooled estimate of 22% for all-cause mortality [6]. The situation is not different in Ethiopia; CVD prognosis is poor, and ACS is increasingly common and leading cause of cardiovascular death, ranging from between 1 and 20% [8]. According to a study conducted at Tikur Anbessa Specialized Hospital (27.4%) [9], and Mekelle (24.5%) [10] of patients died during hospitalization. However, in Ethiopia, there is no data known about optimal medical therapy among patients with the acute coronary syndrome after discharge and clinical outcomes after secondary prevention in patients with ACS.
Early prediction of outcomes is crucial for patients with acute coronary syndrome, as it can greatly improve their prognosis and help control the progression of the disease. While several cardiovascular risk markers have been identified, further research is needed to confirm their usefulness and diagnostic effectiveness [11, 12]. Available data suggests that inflammation plays a prominent role in all stages of coronary atherosclerosis [13]. Prior research has demonstrated that fibrinogen is involved in both the initiation and progression of inflammation by turning on the synthesis of pro-inflammatory proteins through the nuclear factor transcription pathway. In addition to the advancement of atherosclerosis by binding to glycoprotein receptors on platelet surfaces, promoting platelet aggregation [14, 15]. On the other hand, the negative inflammatory protein albumin has a negative correlation with erythrocyte aggregation. In patients with ACS, a decrease in serum albumin levels has been linked to higher mortality rates [16]. Furthermore, a study has revealed that individuals with ACS are more likely to develop poor outcomes if they have a high fibrinogen to albumin ratio (FAR), syntax score II, neutrophil–lymphocyte ratio (NLR), platelet-lymphocyte ratio (PLR), monocyte-to-lymphocyte ratio, high-sensitive C-reactive protein (hsCRP), and low HALP (hemoglobin, albumin, lymphocyte, and platelet) levels below 3.72 [11, 17–21]. Additionally, lifestyle education was also found to be a reliable and independent predictor of worse outcomes [19]. These biomarkers can be easily detected using non-invasive and innovative techniques. However, these biomarkers are not applicable in our setup.
The mortality rate for individuals with ACS has decreased due to the widespread use of revascularization through percutaneous coronary intervention (PCI) and pharmaceutical therapy [22]. In patients with ST-elevation myocardial infarction (STEMI) or non-ST-elevation myocardial infarction (NSTEMI), the American College of Cardiology/American Heart Association (ACC/AHA) recommends aspirin, statins, P2Y12 inhibitors, beta-blockers, and angiotensin-converting enzyme inhibitors (ACEI) or angiotensin receptor blockers (ARB), often referred to as optimal medical therapy (OMT), in patients with STEMI or NSTEMI. The early versions of the ESC guidelines contain a Class I, Level A recommendation for aspirin, P2Y12 inhibitors, and statins in all ACS patients unless contraindicated [23, 24].
Existing evidence showed that OMT prescription at discharge was associated with significantly lower clinical outcomes in patients with ACS [25–30]. However, several reports have shown large gaps between the recommended and prescribed dose and regimen of secondary prevention medications in a patient with ACS after hospital discharge [27, 31–36]. Different studies in Ethiopia determined in-hospital mortality of ACS; however, there are no studies done to assess the use of OMT at discharge and its association with mortality and MACE. Therefore, the study aims to assess OMT, clinical outcome, and its predictors among ACS patients after discharge with secondary prevention medications.
Methods
Study setting and design
The study was conducted at the University of Gondar Comprehensive and Specialized Hospital (UOGCSH). It is found in central Gondar administrative district. The hospital is found 176 km away from the regional city of Bahir Dar and 750 km from the capital city of Ethiopia, Addis Ababa. This is a teaching hospital serving approximately 5–7 million people throughout most of Amhara State and neighboring regions. Gondar town includes 24 kebeles and has Weyina Dega climatic conditions [37]. According to the 2007 Ethiopian census report, the population of Gondar town in 2021 is estimated to be 378,000 [38].
Teaching hospitals is vital to the delivery of community services, research, and education. The facility offers a variety of fields of study, including psychiatry, internal medicine, surgery, gynecology, pediatrics, and HIV care, in addition to more than 500 inpatient beds and outpatient clinics. The study was conducted from January 2018 to February 2023, and the data was collected from May to August 2023. Retrospective cohort study design was employed among ACS patients.
Inclusion and exclusion criteria’s
Inclusion criteria
Adult patients of an age greater than 18 who were admitted to the hospital with a diagnosis of ACS based on the Third Universal Definition of Myocardial Infarction [39]. Moreover, these individuals were discharged with secondary prevention medication between January 31, 2018, and February 1, 2023.
Exclusion criteria
Patients refused to receive secondary prevention medications; missing time variables, no prescribing information, those who were transferred in, those without at least one follow-up, and those who developed re-infarction, CHF, and stroke at the start of the study were excluded from the study.
Sample size determination and sampling technique
Sample size determination
The sample size was calculated by using the single population proportion formula by considering the following: 5% for two-tailed type-I error (Zα/2 = 1.96), 95% confidence interval (CI), assumed the magnitude of all-cause mortality is 50% since none of the study was done in Ethiopia.
where n is the required sample size, Za/2 is the confidence level, p is assumed proportions of all-cause mortality, q is 1-p, and d is the margin of error, n = 384. By taking d = 0.05, p = 0.5, and Zα/2 = 1.96. Then we added 10% contingency by considering the possible missed and lost data.
Sampling technique
A retrospective cohort review of patients with a documented ACS event presenting between January 31, 2018 and February 1, 2023 was conducted, using data from UOGCSH. According to UOGCSH Health Management Information System registries, a total of 1200 ACS patients were treated from January 31, 2018 to February 1, 2023. A systematic random sampling technique was employed to select the study participants (K = 1200/422 = 2.84 ~ 3), then select every 3rd unit. The first patient medical chart was selected by lottery method. The next patient's medical chart was taken if the medical chart was not available and did not meet the inclusion criteria. Then, patient chart was retrieved from chart rooms using the medical registration numbers of each of the patients.
Outcome measurements
Clinical outcomes in this study include all-cause mortality and MACE (heart failure, stroke, and re-infarction). The event of interest was death/MACEs, and the time to death/MACEs was calculated at the time between the dates of discharge and the date of death/MACEs.
Operational definitions
Optimal medical therapy (OMT) was defined as the treatment with a minimum of four drug regimens, which consist of DAPT (aspirin and P2Y12 inhibitors), statins, and beta-blockers.
If comorbidities like hypertension and diabetes are present, OMT is defined as the use of five medications, including ACEIs or ARBs, in addition to the above medications according to ACC/AHA recommendations without contraindication [24, 40, 41], and was defined as reporting taking ≥ 75% of the indicated medications at discharge, which was used as a cut-off point to say OMT [36].
The definition of statin intensity will be based on the ACC/AHA guideline on the management of blood cholesterol [33]. Atorvastatin at 40 or 80 mg daily and rosuvastatin at 20 or 40 mg daily were defined as high-intensity statins, and the other statins were classified as a low-to-moderate intensity statins [23, 27, 42, 43].
Clinical outcome: In this study, defined as:
➢ All-cause mortality and MACEs reported by caregivers and/or health care professionals.
Major adverse cardiovascular events (MACEs): MACE in this study includes re-infarction, stroke, and heart failure [27, 44].
Event: Death from ACS was an event of interest.
Time to death: The time to death was calculated at the time between the dates of discharge and the date of death.
Data collection procedures and data quality control technique
A questionnaire form was created using Kobo Toolbox to collect data on the medical records of patients and, if necessary, by phone calls on ACS patients admitted from January 31, 2018, to February 1, 2023, that was adapted from a tool developed by previous studies [25–27, 29, 45, 46], which contains four sections. The first section is regarding socio-demographic characteristics; the second section is for the assessment of ACS; the third section is regarding patient-related characteristics; and the fourth section is regarding treatment-related characteristics.
Patients were selected from the Health Management Information System (HMIS) registration book for accessing the card numbers of ACS patients admitted from January 31, 2018, to February 1, 2023. Then the medical registration numbers were listed, and the list was reentered and checked for duplications by using Microsoft Office Excel 2013 in order to get an independent observation. Their medical charts were searched using this number from the card room. Then, patients’ charts were retrieved and collected from the record and documentation office. A pre-test was done on 5% of the total sample size (21 medical charts) to assess the completeness of the patient charts before the actual data collection time. Data collectors were trained for one day about the objective of the study, the technique of data extraction, and ethical considerations. The principal investigator carried out the supervision. Regular check-ups for the completeness and consistency of the data were done on a daily basis.
Data processing and analysis
The data were exported to Excel and Statistical Package for Social Science (SPSS) version 26 statistical analysis from Kobo toolbox. Then the repeated data were cleaned in Excel before being exported to SPSS. Descriptive analysis (frequency, percentage, mean, and standard deviation) was calculated and presented in tables. A chi-square test was performed to assess the differences in proportions. A binary logistic regression model was employed to identify candidate variables for further analysis. Variables with P-value ≤ 0.25 in the binary logistic regression model were further entered into multivariable logistic regression analysis to identify factors associated with OMT. Assumption of multi-collinearity was met as variance inflation factor is < 10 and tolerance > 0.1 for all variables. The outcomes of logistic regression stated that the selected model was a good logistic regression model fit, since the Hosemer-Lemeshow goodness of fit p-value is greater than 0.05 (OMT; P = 0.13), then fails to reject the null hypothesis, and it is stated that the logistic model is a good fit for the data set. Assumptions like outliers were checked before running the analysis, and the data values had no outliers (cooks distance test 0.071, which was between 0 and 1).
An all-cause mortality estimate was displayed by using Kaplan–Meier curves. Multivariate Cox proportional hazard models and log-rank tests were conducted to estimate adjusted hazard ratios (aHR) if there are significant changes in clinical outcome between different sets of predictor variables, and 95% confidence intervals were used to evaluate statistical significance [47]. All candidate variables would be from the patients’ baseline characteristics. Variables with a p-value less than 0.05 were declared to be associated with clinical outcomes. During the retrospective follow-up period, any recordings that were lost or where an individual did not experience the event of interest by the end of the follow-up were considered censored. For time-to-all-cause mortality, the proportional hazards assumption was checked using the Schoenfeld residuals test (global test, P-value = 0.8297), complementary log–log plots, graphical parallel assumption test, and Cox-Snell residual was used to test model goodness of fit. Age, dose of medications, and Killip class were among the potential confounding factors that were taken into account by multivariate analysis and stratification in our primary analyses.
Ethical consideration and consent to participate
An official permission letter was obtained from the University of Gondar's specialized referral hospital administrative office, and ethical clearance was obtained from the School of Pharmacy's Ethical Review Committee and the University of Gondar Institutional Review Board (IRB) with the approval number of SOPS/276/2023. Permission to access the medical charts of patients was obtained from the UOGCSH clinical directorate. Participants provided informed consent, both written and verbal, stating their desire to participate in the study after being informed of its aim. Confidentiality was ensured through no patient’s name and identifier was taken; rather, codes were used as identifiers. Information regarding patients was used for the study purpose only.
Result
Socio-demographic characteristics of acute coronary syndrome patients
A total of 422 ACS patient charts were included in the study. The mean ages of patients were 61.56 ± 9.686 years, with a range of 34–84 years, and 54.7% of the patients were men. Of the total study subjects, 57.6% were getting health insurance coverage, and 44.3% were urban residents (Table 1).
Table 1.
Socio-demographic characteristics of acute coronary syndrome patients in UOGCSH from January 31, 2018 to February 1, 2023 (n = 422)
| Variables | Category | Frequency n (%) |
|---|---|---|
| Sex | Male | 231 (54.7) |
| Female | 191 (45.3) | |
| Age (years) | ≤ 55 | 134 (31.8) |
| 56–64 | 139 (32.9) | |
| ≥ 65 | 149 (35.3) | |
| Residency | Rural | 235 (55.7) |
| Urban | 187(44.3) | |
| Health insurance coverage | Yes | 243 (57.6) |
| No | 179 (42.4) |
Symptoms on admission, clinical characteristics, killip class, and comorbidities of acute coronary syndrome patients
The frequently recorded patients’ symptoms on admission were chest pain alone (50.5%), followed by chest pain and nausea and vomiting (24.6%). Out of 422 patients with evidence of Killip class, 32.2% of them had Killip class II and 28.2% had Killip class III. Hypertension was the most prominent comorbidity in ACS patients (43.1%), followed by diabetes (28.4%). The mean length of hospital stay was 9.07 ± 3.86 days, with a minimum of two days and a maximum of 20 days.
Of the total study subjects, 15.9% had elevated systolic blood pressure in the range of 130–139 mmHg, and 24.6% of patients had elevated diastolic blood pressure in the range of 80–89 mmHg (Table 2).
Table 2.
Symptoms on admission, clinical characteristics, Killip class and risk factors of acute coronary syndrome patients in UOGCSH from January 31, 2018 to February 1, 2023 (n = 422)
| Variables | Category | Frequency n(%) |
|---|---|---|
| Symptom on admission | Chest pain | 213 (50.5) |
| Chest pain and NV | 104(24.6) | |
| Chest pain and SOB | 90 (21.3) | |
| SOB | 2 (0.5) | |
| othersa | 13 (3.1) | |
| Length of hospitalization (days) | < 7 | 178 (42.2) |
| 7–14 | 200 (47.4) | |
| ≥ 15 | 44 (10.4) | |
| SBP (mmHg) | < 90 | 2 (0.5) |
| 90–119 | 281 (66.6) | |
| 120–129 | 38 (9) | |
| 130–139 | 67 (15.9) | |
| ≥ 140 | 34 (8.1) | |
| DBP (mmHg) | < 60 | 181 (42.9) |
| 60–79 | 127 (30.1) | |
| 80–89 | 104 (24.6) | |
| ≥ 90 | 10 (2.4) | |
| HR (beat/min) | < 60 | 10 (2.4) |
| 60–100 | 397 (94.1) | |
| > 100 | 15 (3.6) | |
| Smoking status | Yes | 26 (6.2) |
| No | 396 (93.8) | |
| Killip class | Class I | 50 (11.85) |
| Class II | 136 (32.2) | |
| Class III | 119 (28.2) | |
| Class IV | 117 (27.73) | |
| Cardiac catheterization | Yes | 12 (2.8) |
| No | 410 (97.2) | |
| Comorbidities | Hypertension | 182 (43.1) |
| Diabetes mellitus | 120 (28.4) | |
| Dyslipidaemia | 93 (22.0) | |
| Cardiogenic shock | 73 (17.2) | |
| Chronic kidney disease | 49 (11.6) | |
| Obesity | 13 (3.1) | |
| Atrial fibrillation | 36 (8.5) | |
| Family history of CAD | 44 (10.5) | |
| Othersb | 22 (5.2) |
CAD Coronary artery disease, SOB Shortness of breath, NV Nausea and vomiting, SBP Systolic blood pressure, DBP Diastolic blood pressure, mmHg Millimeters of mercury, HR Heart rate
Othersa: easy fatigability, palpitation, abdominal pain and syncope
Othersb: Anemia, Pneumonia, Thyroid disease, HIV, and Seizure
Profile of laboratory findings and diagnostic investigations of acute coronary syndrome patients
In the case of laboratory and diagnostic investigations, as can be seen from the data in Table 3, from recorded investigations, about one-fifth (20%) had elevated low-density lipoprotein. Total cholesterol was higher than normal value in 11.9% of the patients. About 35.6% had lower-than-normal values of high-density lipoprotein and 12.5% had elevated triglyceride levels.
Table 3.
Profile of laboratory findings and diagnostic investigations of acute coronary syndrome patients in UOGCSH from January 31, 2018 to February 1, 2023(n = 422)
| Variable | Category (mg/dl) | Frequency n (%) |
|---|---|---|
| Total cholesterol | < 200 | 141 (88.1) |
| ≥ 200 | 19 (11.9) | |
| Triglyceride | < 150 | 140 (87.5) |
| ≥ 150 | 20 (12.5) | |
| HDL | < 40 | 26 (35.6) |
| ≥ 40 | 47 (64.4) | |
| LDL | < 100 | 124 (80) |
| ≥ 100 | 31 (20) | |
| Laboratory value | Mean ± SD | Reference range |
| Serum creatinine | 0.95 ± 0.17 | 0.65–1.2 mg/dl |
| Troponin level | 0.48 ± 0.13 | 0–0.04 ng/dl |
HDL High density lipo-proteins, LDL Low density lipo-proteins
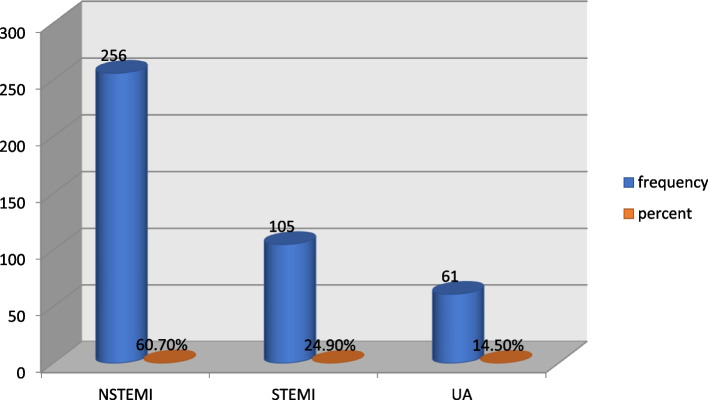
Regarding the class of diagnosis, 256 (60.7%), 105 (24.9%), and 61 (14.5%) were classified under NSTEMI, STEMI, and UA, respectively (Fig. 1).
Fig. 1.
Class diagnosis for acute coronary syndrome patients in UOGCSH from January 31, 2018 to February 1, 2023(n = 422)
Medication given at discharge
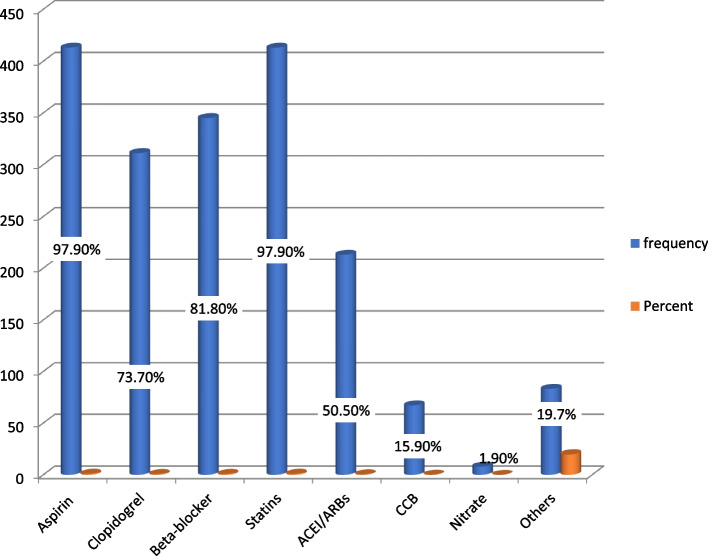
Regarding discharge medications, most of the patients (413, 97.9%) had been prescribed aspirin and statins. About 345 (81.8%) patients were discharged with beta-blockers, and clopidogrel was prescribed on 311 (73.7%). ACEIs/ARBs and calcium channel blockers were documented in 213 (50.5%) and 67 (15.9%) patients, respectively (Fig. 2).
Fig. 2.
Discharge medications of acute coronary syndrome patients admitted from January 31, 2018 to February 1, 2023(n = 422)
Optimal medical therapy (OMT) and clinical outcomes
A total of 250 (59.2%) patients were discharged with all indicated drugs (OMT), 95% CI: (54.4–64.0%). Concerning clinical outcomes, from the total of 422 patients who were admitted during the five years, 70 (16.6%) patients died with a 95% CI of 13.2–20.5%. Moreover, 130 (30.8%) patients had experienced MACEs with a 95% CI of 26.4–35.5%; from this, 14.2%, 11.4%, and 6.8% were stroke, CHF, and myocardial re-infarction, respectively (Table 4).
Table 4.
Optimal medical therapy and clinical outcomes in patient with acute coronary syndrome admitted from January 31, 2018 to February 1, 2023(n=422)
| Outcomes | On OMT | Frequency n (%) | 95% CI (%) | |||
|---|---|---|---|---|---|---|
| Yes | No | |||||
| Death | Yes | 24 | 46 | 70 (16.6) | 13.2-20.5 | |
| No | 226 | 126 | ||||
| MACE |
Yes No |
17 233 |
113 59 |
130(30.8) | 26.4-35.5 | |
| Stroke |
Yes No |
7 243 |
53 119 |
60 (14.2) | 2.90-14.7 | |
| CHF |
Yes No |
5 245 |
45 127 |
50 (11.4) | 3.60-18.5 | |
| Re-infarction |
Yes No |
5 245 |
17 155 |
22 (5.2) | 4.90-35.5 | |
MACEs Major adverse cardiovascular events, CHF Congestive heart failure; and OMT Optimal medical therapy
Factors associated with optimal medical therapy
Among variables tested for association in bivariable analysis, age, sex, residence, health insurance coverage, smoking status, diabetes, cardiogenic shock, family history of coronary artery disease (CAD), atrial fibrillations (AF), and chronic kidney disease (CKD) were variables with a P-value ≤ 0.25 and candidates for multivariable analysis. Patients with age greater than or equal to sixty-five were 0.488 times less likely to obtain OMT as compared to patients with age less than or equal to fifty-five [AOR = 0.488, 95% CI (0.261–0.912), P value = 0.025]. Male patients with acute coronary syndrome were 1.919 times more likely to be discharged with OMT as compared to female patients [AOR = 1.919, 95% CI (1.125–3.273), P value = 0.017].
Regarding comorbidities, acute coronary syndrome (ACS) patients with cardiogenic shock were 0.552 times less likely to be discharged with OMT as compared to patients without cardiogenic shock [AOR = 0.552, 95% CI (0.306–0.996), P value = 0.049]. ACS patients with AF were 0.187 times less likely to be discharged with OMT as compared to patients without AF [AOR = 0.187, 95% CI (0.081–0.433), P value = 0.001]. Moreover, ACS patients with CKD were 0.257 times less likely to be discharged with OMT as compared to patients without CKD [AOR = 0.257, 95% CI (0.123–0.537), P value = 0.001] (Table 5).
Table 5.
Multivariable logistic regression analysis of factors associated with optimal medical therapy at discharge in patient with acute coronary syndrome admitted from January 31, 2018 to February 1, 2023(n = 422)
| Variables | Category | OMT (N) | COR (95% CI) | AOR (95% CI) | P-value | |
|---|---|---|---|---|---|---|
| Yes | No | |||||
| Age | ≤ 55 | 89 | 34 | 1 | 1 | |
| 56–64 | 91 | 42 | 0.828(0.483–1.418) | 1.00(0.554–1.806) | 0.999 | |
| ≥ 65 | 70 | 96 | 0.279(0.169–0.46) | 0.488(0.261–0.912) | 0.025* | |
| Sex | Male | 164 | 67 | 2.989(1.998–4.470) | 1.919(1.125–3.273) | 0.017* |
| Female | 86 | 105 | 1 | 1 | ||
| Residence | Rural | 149 | 86 | 1 | 1 | |
| Urban | 101 | 86 | 0.678(0.458–1.008) | 1.294(0.801–2.090) | 0.292 | |
| Health insurance coverage | Yes | 162 | 81 | 2.068(1.392–4.718) | 1.456(0.918–2.307) | 0.110 |
| No | 88 | 91 | 1 | 1 | ||
| Smoking status | Yes | 19 | 7 | 1.939(0.797–4.718) | 0.906(0.344–2.385) | 0.841 |
| No | 231 | 165 | 1 | 1 | ||
| Comorbidities | ||||||
| Diabetes | Yes | 64 | 56 | 0.713(0.465–1.092) | 0.782(0.482–1.267) | 0.318 |
| No | 186 | 116 | 1 | 1 | ||
| Cardiogenic shock | Yes | 27 | 46 | 0.332(0.197–0.559) | 0.552(0.306–0.996) | 0.049* |
| No | 223 | 126 | 1 | 1 | ||
| Family history of CAD | Yes | 21 | 23 | 0.597(0.319–1.116) | 0.933(0.45–1.937) | 0.853 |
| No | 228 | 149 | 1 | 1 | ||
| AF | Yes | 10 | 26 | 0.234(0.110–0.499) | 0.187(0.081–0.433) | 0.001* |
| No | 240 | 146 | 1 | 1 | ||
| CKD | Yes | 13 | 36 | 0.207(0.106–0.404) | 0.257(0123–0.537) | 0.001* |
| No | 237 | 136 | 1 | 1 | ||
CKD Chronic kidney disease, CAD Coronary artery disease, AF Atrial fibrillation, COR Crude odds ratio, AOR Adjusted odds ratio
Predictors of all-cause mortality in patients with ACS
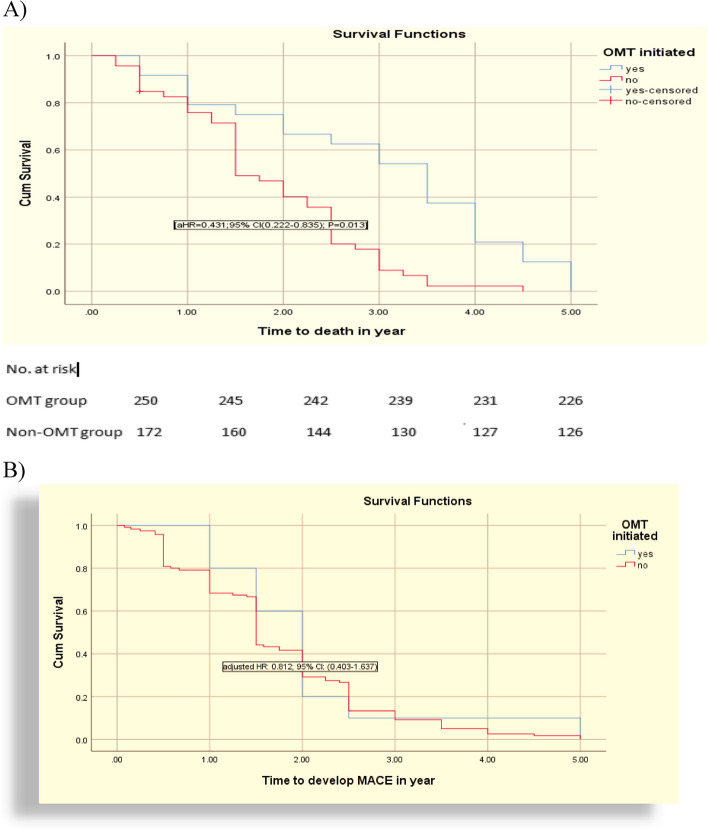
Multivariate Cox's proportional hazard model was applied to determine the relationship between different covariates at discharge on 5-year all-cause mortality. In the analysis, only one variable was found to be an independent predictor of all-cause mortality in patients with ACS. Overall, OMT prescription at discharge was associated with a reduction in 5-year mortality (AHR = 0.431; 95%CI: 0.222–0.835; P = 0.013) and no significant difference in MACE (AHR = 0.812; 95%CI: 0.403–1.637) (Table 6).
Table 6.
Multivariable cox-regression analysis of covariates associated with the predicted all-cause mortality of ACS patients in UOGCSH admitted from January 31, 2018 to February 1, 2023(n = 422)
| Variables | Category | Death | CHR (95%CI) | AHR (95%CI) | P-value | |
|---|---|---|---|---|---|---|
| Yes | No | |||||
| Killip class | Class I | 3 | 47 | 1 | 1 | |
| Class II | 11 | 125 | 0.763(0.204–2.848) | 0.836(0.149–4.687) | 0.838 | |
| Class III | 11 | 108 | 1.055(0.293–3.796) | 0.537(0.09–3.207) | 0.495 | |
| Class IV | 45 | 72 | 1.197(0.370–3.872) | 1.067(0.222–5.140) | 0.936 | |
| Diagnosis | STEMI | 47 | 63 | 1.564(0.842–2.004) | 2.075(0.743–5.793) | 0.164 |
| NSTEMI | 10 | 231 | 1.667(0.727–3.823) | 1.664(0.541–5.122) | 0.375 | |
| UA | 13 | 58 | 1 | 1 | ||
| Hypertension | Yes | 42 | 140 | 0.717(0.438–1.173) | 0.707(0.397–1.259) | 0.239 |
| No | 28 | 212 | 1 | 1 | ||
| Cardiogenic shock | Yes | 55 | 18 | 1.236(0.696–2.195) | 0.978(0.357–2.682) | 0.966 |
| No | 15 | 334 | 1 | 1 | ||
| Cardiac catheterization | Yes | 8 | 6 | 1.996(0.936–4.256) | 1.354(0.583–3.144) | 0.481 |
| No | 62 | 346 | 1 | 1 | ||
| Dose of statin | 40–80 | 20 | 312 | 0.555(0.326–0.944) | 0.667(0.324–1.371) | 0.270 |
| < 40 | 50 | 40 | 1 | 1 | ||
| OMT initiated | Yes | 24 | 226 | 0.362(0.205–0.638) | 0.431(0.222–0.835) | 0.013* |
| No | 46 | 126 | 1 | 1 | ||
| Length of hospitalization (day) | < 7 | 9 | 138 | 1 | 1 | |
| 7–14 | 12 | 183 | 1.212(0.510–2.882) | 2.564(0.748–8.794) | 0.134 | |
| ≥ 15 | 49 | 32 | 1.528(0.746–3.131) | 1.321(0.605–2.887) | 0.485 | |
CHR Crude hazard ratio, CI Confidence interval, AHR Adjusted hazard ratio
*Significant
Survival estimate for time to death by life table
Totally, 422 adult ACS patients were followed for a five-year period, with the cumulative probability of survival at year one, at year two, and at year three being 0.8429 ± 0.0435 (95% CI; 0.7342, 0.9097), 0.5571 ± 0.0594 (95% CI; 0.4335, 0.6641), and 0.3286 ± 0.0561 (95% CI; 0.2223, 0.4388), respectively (Table 7).
Table 7.
life table showing the probability of survival among ACS patients in UOGCSH admitted from January 31, 2018 to February 1, 2023(n = 422)
| Years | Patient at risk | Number of deaths | Censored | Cumulative survival | SD. error | [95% CI] |
|---|---|---|---|---|---|---|
| 1 | 422 | 17 | 55 | 0.8429 | 0.0435 | 0.7342 0.9097 |
| 2 | 350 | 19 | 89 | 0.5571 | 0.0594 | 0.4335 0.6641 |
| 3 | 242 | 17 | 64 | 0.3286 | 0.0561 | 0.2223 0.4388 |
| 4 | 161 | 11 | 146 | 0.1429 | 0.0418 | 0.0733 0.2348 |
| 5 | 4 | 6 | 4 | 0.0429 | 0.0242 | 0.0114 0.1090 |
SD Standard deviation, CI Confidence interval
Survival estimate for time to death by Kaplan–Meier graph
In this study, a total of 70 (16.6%) ACS patients died during a 5-year period, and most patients died in the second and third years of life. The mean survival time was 3 ± 0.302 years with CI (2.407–3.593) in the OMT group and 1.861 ± 0.147 years with CI (1.572–2.150) in the non-OMT group. The median survival time of the OMT group was 3.5 ± 0.395 with CI (2.725–4.275) and 1.5 ± 0.179 with CI (1.149–1.851) in the non-OMT group. The time to all-cause mortality and time to MACE were also determined using the Kaplan–Meier survival estimate, and the fulfillment of the hazard assumptions was confirmed using the log–log plot (Fig. 3).
Fig. 3.
Kaplan Meier curve of (A) 5-year survival, and (B) major adverse cardiac events (MACE) between OMT and non-OMT group
Lastly, a Schoenfeld residual test (also known as the global test) was used to verify the hazard proportional assumption. As a result, the assumption was satisfied, and the global test's p-value, or Schoenfeld residual test, was 0.8297.
Discussion
To our knowledge, this is the first study to determine optimal medical therapy (OMT) prescription, clinical outcome, and associated factors among acute coronary syndrome (ACS) patients in Ethiopia. Based on this, we found that only 59.2% of patients received OMT at discharge. Age ≥ 65, atrial fibrillation, chronic kidney diseases, and cardiogenic shock were negative independent predictors of optimal medical therapy. On the other hand, male sex was independently associated with the use of optimal medical therapy.
In this study, the rate of OMT prescription was found to be 59.2% (95% CI = 54.4%, 64.0%). This finding was consistent with previous studies done in France (57.4%) [26, 29, 48]. But it was higher than those studies done in Sudan (45.2%), Thailand (42.6%), the Netherlands (43.2%, 43.7%), Iraq (53.5%), China (15.1%, 36%, 36.2%, 39.8%), and India (46%), respectively [25, 27, 30, 35, 46, 49–53]. This might be due to different reasons; first, in these studies, the definition of OMT is the use of five medications: aspirin, clopidogrel/P2Y12 inhibitors, beta-blockers, statins, and ACEIs/ARBs. Second, investigators from other low- and middle-income countries have also evaluated the use of optimal medical therapy in their registries. For example, the use of optimal medical therapy at discharge, defined by the concurrent use of aspirin, β-blockers, statin, and ACE-I/ARBs, was evaluated in the Clinical Pathways for ACS in China registries [54]. However, use of clopidogrel given its class I recommendation for all patients [33], which is not the case with ACE-I/ARBs, which requires concomitant heart failure, left ventricular systolic dysfunction, diabetes mellitus, or hypertension for a class I indication [24, 33]. The rate of OMT prescription in this study was lower than those studies done in Korea (63.2%, 75.71%), the Netherlands (69.1%), and Australia (65%), respectively [55–58]. The possible reason might be in OMT prescription at discharge in ACS patients among different studies: is local context, study time point, the severity of diagnosis, health coverage, and medication availability [27, 49, 53]. This suboptimal use of OMT leads to mortality and morbidity, as well as increased healthcare costs regarding hospital admission.
The current findings showed that elderly patients were less likely discharged with OMT than younger patients. This finding was in accord with studies done in Canada [29, 59], Korea [48], and the southern US [60]. This might be due to elderly patients exhibiting higher rates of comorbidities and having higher rates of adverse events [55, 59, 60]. Statins were found to be equally effective in lowering the risk of cardiovascular death, ACS, stroke, or coronary revascularization in patients 75 years of age or older, according to a recent meta-analysis [61]. The findings were also consistent across statin trials. Even with very low low-density lipoprotein levels, statins have no effect on patient-reported cognition [62], according to the most recent data, despite post-market studies raising concerns about cognitive damage, particularly in the aging population. However, recent emerging evidence showed no difference in efficacy and safety outcomes in relation to age [63–65]. Moreover, the existing evidence recommends OMT for all patients without considering age differences. Therefore, OMT should be considered for elderly patients with ACS with the exception of contraindications [23, 33, 40, 42, 66].
Regarding sex, our study indicated that male patients were more likely to be discharged with OMT than female patients. This outcome is consistent with research conducted in Australia [67–69], West China (17), Italy (54), Thailand [27], the Netherlands [67, 70], and Malaysia [71, 72]. Since females with ACS were less likely to present with chest pain and diaphoresis but more likely to present with shoulder pain or gastrointestinal symptoms. This could be explained by the fact that female patients are frequently older and more complex with multiple baseline adverse comorbidities [67–70, 73, 74]. Furthermore, females had higher rates of baseline renal dysfunction, which contributed to the lower rates of ACEI/ARB prescriptions. As a result, the advantages of OMT may be underestimated [70–72]. Despite the long-term benefits of ACEI/ARBs being well established, many physicians are still hesitant to prescribe them to patients with renal dysfunction. In addition, the lower rate of dual antiplatelet therapy (DAPT) prescriptions among females in this study is due to a fear of bleeding complications. However, studies have demonstrated there is no sex difference in major bleeding risk at 12 months with DAPT [67, 75].
This study found that CKD patients had a lower likelihood of receiving an OMT during discharge. The study findings concurred with research from Thailand and Canada [29]. This could be because using ACEI/ARBs increases the risk of side effects and may require precautions against hyperkalemia or acute renal injury [27]. Patients with chronic kidney disease (CKD) should typically have a renal function test in order to alter their dosage, as most secondary preventive drugs have different effects on the kidney. Nonetheless, this study brought to light concerning issues with ACEI/ARB usage in ACS patients. Only 50.5% of the study participants were discharged with an ACEI or ARBs; most of them had hypertension or diabetes. Moreover, even though statin use has been shown to lower mortality in patients with or at risk for ACS, patients with CKD who have ACS are less likely to receive this treatment [76–78]. Data from the National Registry of Myocardial Infarction 4 indicate that statin administration within the first 24 h of hospitalization for acute myocardial infarction significantly lowers the rate of early complications and in-hospital mortality, in addition to the long-term benefits of statin therapy in ACS patients [79]. In fact, statins seem to mitigate the effects of inflammation, endothelial dysfunction, and coagulation problems, which are all linked to acute myocardial infarction [80]. There is uncertainty regarding the causes of this under-use of OMT in ACS patients with CKD. Potential explanations include worry about harmful side effects and additional deterioration of renal function. Moreover, there is more co-morbidity in CKD patients, which increases their contraindications to these medications.
Our study revealed that patients with atrial fibrillation (AF) were less likely to be discharged with OMT as compared to patients without AF. This result is consistent with studies done in Thailand [27] and Serbia [81]. Compared to patients without AF, those with AF had a lower likelihood of receiving beta-blockers, according to the GISSI-3 data [82]. In this study, digoxin and antiarrhythmic medications were used more frequently to treat AF patients. Another investigation revealed that patients with AF who had never been diagnosed before had a lower chance of receiving clopidogrel [83]. AHA/ACC and ESC guidelines recommend the use of triple therapy for patients with atrial fibrillation, consisting of DAPT and warfarin or a non-vitamin K anticoagulant (NOAC) or dual therapy (P2Y12 inhibitors plus warfarin or NOACs) to prevent stroke in patients who are more likely to experience thromboembolism-related problems [41, 81, 84, 85]. However, double therapy may be used in place of DAPT, which has an impact on the percentage of DAPT prescriptions in this study.
Our study also suggested that patients who experienced cardiogenic shock had a lower likelihood of being discharged with OMT. The finding was similar to the study done in six Middle Eastern countries [32]. The possible reason might be due to the presence of patients who are comparatively contraindicated. These patients may have started off hemodynamically unstable but later improved and became candidates for starting B-blockers. Therefore, the commencement of beta-blockers, which may have begun at a low dose and increased based on the patient's state, was overlooked for these individuals when their hemodynamic stability and progress were seen. Another possible cause is a disruption in the medicine delivery [10]. Additionally, because this study was retrospective, there was a risk that the number of real contraindications may not have been recorded in the patient files, lowering the actual secondary prevention.
In terms of clinical outcomes, over a 5-year period, approximately 16.6%, 95% CI (13.2%, 20.5%), of ACS patients died, and 30.8%, 95% CI (26.4–35.5%), had MACE, which included 11.4% of CHF cases, 14.2% of stroke cases, and 5.2% of re-infarction cases. Overall, OMT prescription at discharge was associated with a reduction in 5-year mortality (AHR = 0.431; 95%CI: 0.222–0.835; P = 0.013).
Regarding to all-cause mortality, our finding is in accord with studies done in Israel (15.8%) [86], Netherlands (16.7%) [87], and Australia (16.8%) [88]. The results were higher than studies done in China (6.8%) [35], and Japan (7.1%, 6.3%) [89, 90]. On one hand, it might be due to sample size variation; in this study, only 422 patients were included, whereas the sample size in China, Australia, and Japan was larger. The other possible reasons might be due to the non-availability of thrombolytic drugs, non-adherence to the recommended guidelines, lifestyle issues, non-availability of CABG (coronary artery bypass graft), PCI (percutaneous coronary interventions) procedures, and P2Y12 inhibitors (ticagrelor, prasugrel) in the study area, which could all be the possible reasons.
Overall, our study revealed that patients who were discharged from the hospital with an optimal medical therapy (OMT) regimen consisting of four medications—aspirin, clopidogrel/P2y12 inhibitors, beta-blockers, statins, or the use of ACEI/ARBs on the top of the above medications if the patient had comorbidities like diabetes or hypertension—had a lower all-cause mortality rate. The present findings align with previous studies that have demonstrated improved outcomes for patients receiving OMT at the time of discharge [25, 26, 29, 35, 36, 48, 91, 92]. Optimal medical therapy (OMT) had been associated with lower MACE, according to a study conducted in Italy [92]. However, in this study, there was no statistically significant difference in MACE between the OMT and non-OMT groups. This study supports the use of OMT with all four drugs in combinations, as OMT was associated with a 56.9% reduced risk of all-cause mortality in patients with ACS.
Study strength and limitations
It is important to emphasize this study's advantages. This is the first study that assessed secondary prevention medication after ACS for a five-year period in Ethiopia. Because the research is based on actual data, it offers a reliable representation of the therapeutic advantages of OMT regimens. The assessment of the causal link between OMT prescriptions and therapeutic benefit on mortality yielded reliable findings with strong statistical power.
This study has some limitations. Due to the retrospective nature of the study design, it was not possible to capture important data from the patient charts, such as contraindications and pertinent laboratory values. Second, the study was conducted at a single center, which may limit its external validity and scientific rigor in justifying broad practice modifications. It is unclear if the patients took the prescribed drugs, as many had multiple comorbidities and were taking various medications that are associated with poor adherence. However, a retrospective analysis found no significant difference in medication adherence rates at 3 months and 1 year after discharge for patients with acute myocardial infarction [93].
Conclusion
This study found that the use of optimal medical therapy (OMT) in patients discharged with acute coronary syndrome (ACS) was associated with a decrease in overall mortality. However, the utilization of OMT remains suboptimal, with only 59.2% of patients being discharged with this treatment. The research also revealed that patients aged 65 years and older, those with chronic kidney disease (CKD), atrial fibrillation (AF), and cardiogenic shock were less likely to receive OMT at discharge. On the other hand, male ACS patients were more likely to receive OMT. Therefore, it is crucial for healthcare providers to actively work towards optimizing the use of OMT at discharge, especially in the early stages of the illness.
Acknowledgements
The University of Gondar, School of Pharmacy, Department of Clinical Pharmacy, and every employee of the medical ward are acknowledged by the authors for their assistance in this research.
Authors’ contributions
GWG assisted with project management and conceptualization of the study. TTA, AFB, YAW, GTG, and SSA contributed to the study designs, supervision and clinical concepts. Finally, MEM, SF, and ADG contributed to the document writing. All authors participated in the data analysis and interpretation, as well as the final document production, review, and editing. GWG is the guarantor.
Funding
This research received no specific grant from any funding agency in the public commercial or not-for-profit sectors.
Availability of data and materials
Information is accessible upon justifiable request. The corresponding author can provide all pertinent information upon reasonable request, including the data and materials supporting the study's findings.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
An official permission letter was obtained from the University of Gondar's specialized referral hospital administrative office, and ethical clearance was obtained from the School of Pharmacy's Ethical Review Committee and the University of Gondar Institutional Review Board (IRB) with the approval number of SOPS/276/2023. Permission to access the medical charts of patients were obtained from UOGCSH clinical directorate. Participants provided informed consent, both written and verbal, stating their desire to participate in the study after being informed of its aim. Confidentiality was ensured through no patient’s name and identifier was taken; rather, codes were used as identifiers. Information regarding patients was used for the study purpose only.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Cheema KM, et al. Long-term trends in the epidemiology of cardiovascular diseases in the UK: insights from the British Heart Foundation statistical compendium. Cardiovasc Res. 2022;118(10):2267–80. [DOI] [PubMed] [Google Scholar]
- 2.Angaw DA, et al. The prevalence of cardiovascular disease in Ethiopia: a systematic review and meta-analysis of institutional and community-based studies. BMC Cardiovasc Disord. 2021;21(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boden WE, et al. Contemporary approach to the diagnosis and management of non–ST-Segment elevation acute coronary syndromes. Prog Cardiovasc Dis. 2008;50(5):311–51. [DOI] [PubMed] [Google Scholar]
- 4.Hodzic E, et al. Seasonal incidence of acute coronary syndrome and its features. Mater soc-med. 2018;30(1):10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bhatt DL, Lopes RD, Harrington RA. Diagnosis and treatment of acute coronary syndromes: a review. JAMA. 2022;327(7):662–75. [DOI] [PubMed] [Google Scholar]
- 6.Adem F, et al. In-hospital mortality from acute coronary syndrome in Africa: a systematic review and meta-analysis. SAGE Open Med. 2023;11:20503121221143650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Timmis A, et al. European society of cardiology: cardiovascular disease statistics 2021. Eur Heart J. 2022;43(8):716–99. [DOI] [PubMed] [Google Scholar]
- 8.Angaw DA, et al. The prevalence of cardiovascular disease in Ethiopia: a systematic review and meta-analysis of institutional and community-based studies. BMC Cardiovasc Disord. 2021;21:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bogale K, et al. Treatment outcomes of patients with acute coronary syndrome admitted to Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia. Clin Med Insights: Cardiol. 2019;13:1179546819839417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Desta DM, et al. Treatment outcome of acute coronary syndrome patients admitted to Ayder Comprehensive Specialized Hospital, Mekelle, Ethiopia; a retrospective cross-sectional study. PLoS ONE. 2020;15(2): e0228953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hou X-G, et al. The fibrinogen-to-albumin ratio is associated with poor prognosis in patients with coronary artery disease: findings from a large cohort. J Cardiovasc Transl Res. 2023;16(5):1177–83. [DOI] [PubMed] [Google Scholar]
- 12.Wang X, et al. Predictive impact of fibrinogen-to-albumin ratio (FAR) for left ventricular dysfunction in acute coronary syndrome: a cross-sectional study. Eur J Med Res. 2023;28(1):68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hoogeveen RM, et al. Monocyte and haematopoietic progenitor reprogramming as common mechanism underlying chronic inflammatory and cardiovascular diseases. Eur Heart J. 2018;39(38):3521–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Escárcega RO, et al. Inflammation and atherosclerosis: cardiovascular evaluation in patients with autoimmune diseases. Autoimmun Rev. 2018;17(7):703–8. [DOI] [PubMed] [Google Scholar]
- 15.Larsen JB, Hvas AM. Fibrin clot properties in coronary artery disease: new determinants and prognostic markers. Pol Arch Intern Med. 2021;131(11):16113. [DOI] [PubMed] [Google Scholar]
- 16.Zhu Y, et al. Association between fibrinogen/albumin ratio and severity of coronary artery calcification in patients with chronic kidney disease: a retrospective study. PeerJ. 2022;10: e13550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Adukauskienė D, et al. Clinical relevance of high sensitivity C-reactive protein in cardiology. Medicina. 2016;52(1):1–10. [DOI] [PubMed] [Google Scholar]
- 18.Karadeniz F, Karadeniz Y, Altuntaş E. Systemic immune-inflammation index, and neutrophil to-lymphocyte and platelet-to-lymphocyte ratios can predict clinical outcomes in patients with acute coronary syndrome. Cardiovasc J Afr. 2023;34:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Karakayali ZB, Seven A, Karakayali M. The effect of education on hospitalization and quality of life in patients with heart failure. In: Anatolian journal of cardiology. Fahrettin Kerim Gokay Caddesi. No: 200/AD: 2 Cemenzar: KARE PUBL Goztepe Mah; 2022. [Google Scholar]
- 20.Karakayali M, et al. The prognostic value of HALP score in predicting in-hospital mortality in patients with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention. Coron Artery Dis. 2023;34(7):483–8. [DOI] [PubMed] [Google Scholar]
- 21.Rencuzogullari I, et al. Value of syntax score II for predicting in-hospital and long-term survival in octogenarians with ST-segment elevation myocardial infarction: a comparison of six different risk scores. Arch Gerontol Geriatr. 2019;83:37–43. [DOI] [PubMed] [Google Scholar]
- 22.Szummer K, et al. Improved outcomes in patients with ST-elevation myocardial infarction during the last 20 years are related to implementation of evidence-based treatments: experiences from the SWEDEHEART registry 1995–2014. Eur Heart J. 2017;38(41):3056–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ibanez B, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119–77. [DOI] [PubMed] [Google Scholar]
- 24.Damman P, et al. 2015 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: comments from the Dutch ACS working group. Neth Hear J. 2017;25(3):181–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hoedemaker NP, et al. Trends in optimal medical therapy prescription and mortality after admission for acute coronary syndrome: a 9-year experience in a real-world setting. Eur Heart J-Cardiovasc Pharmacotherapy. 2018;4(2):102–10. [DOI] [PubMed] [Google Scholar]
- 26.Tomasevic D, et al. Effect of optimal medical therapy at discharge in patients with reperfused ST-segment elevation myocardial infarction on 1-year mortality (from the Regional RESCUe Registry). Am J Cardiol. 2018;121(4):403–9. [DOI] [PubMed] [Google Scholar]
- 27.Wongsalap Y, et al. Trends in optimal medical therapy at discharge and clinical outcomes in patients with acute coronary syndrome in Thailand. J Cardiol. 2021;77(6):669–76. [DOI] [PubMed] [Google Scholar]
- 28.Wongwai N, Kanjanasilp J. Outcomes of secondary prevention medications in patients with non–ST-elevation acute coronary syndrome after hospital discharge at 1 year follow-up. Northeast Thailand: Mahasarakham University; 2022.
- 29.Yan AT, et al. Optimal medical therapy at discharge in patients with acute coronary syndromes: temporal changes, characteristics, and 1-year outcome. Am Heart J. 2007;154(6):1108–15. [DOI] [PubMed] [Google Scholar]
- 30.Zhang J, et al. Current trends in optimal medical therapy after PCI and its influence on clinical outcomes in China. BMC Cardiovasc Disord. 2021;21(1):258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ahmed KO, et al. Optimal medical therapy for secondary prevention of acute coronary syndrome: a retrospective study from a tertiary hospital in Sudan. Ther Clin Risk Manag. 2022;18:391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Al-Zakwani I, et al. Medication use pattern and predictors of optimal therapy at discharge in 8176 patients with acute coronary syndrome from 6 Middle Eastern countries: data from the gulf registry of acute coronary events. Angiology. 2011;62(6):447–54. [DOI] [PubMed] [Google Scholar]
- 33.Amsterdam EA, et al. 2014 AHA/ACC guideline for the management of patients with non–ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. J Am Coll Cardiol. 2014;64(24):e139–228. [DOI] [PubMed] [Google Scholar]
- 34.Byeon HJ, Yang Y-M, Choi EJ. Optimal medical therapy for secondary prevention after an acute coronary syndrome: 18-month follow-up results at a tertiary teaching hospital in South Korea. Ther Clin Risk Manag. 2016;12:167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chen S-J, et al. The impact of optimal medical therapy at discharge on mortality in patients with coronary artery disease. J Geriatr Cardiol: JGC. 2017;14(2):100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chow CK, et al. Secondary prevention therapies in acute coronary syndrome and relation to outcomes: observational study. Heart Asia. 2019;11(1):e011122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Aynalem M, Adane T, Getawa S. Magnitude of coagulation abnormalities and associated factors among patients with heart diseases at the University of Gondar Comprehensive Specialized Hospital. Vasc Health Risk Manag. 2022;Volume 18:617–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chekol YM, et al. Development and validation of a risk prediction model to estimate the risk of stroke among hypertensive patients in University of Gondar comprehensive specialized hospital, Gondar, 2012 to 2022. Degener Neurol Neuromuscul Dis. 2023;13(2023):89–110. [DOI] [PMC free article] [PubMed]
- 39.Guidelines, E.C.f.P, et al. Third universal definition of myocardial infarction. J Am Coll Cardiol. 2012;60(16):1581–98. [DOI] [PubMed] [Google Scholar]
- 40.Collet J-P, et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: the task force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2021;42(14):1289–367. [DOI] [PubMed] [Google Scholar]
- 41.January CT, et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines and the heart rhythm society in collaboration with the society of thoracic surgeons. Circulation. 2019;140(2):e125–51. [DOI] [PubMed] [Google Scholar]
- 42.O’gara PT, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. J Am Coll Cardiol. 2013;61(4):e78–140. [DOI] [PubMed] [Google Scholar]
- 43.Spencer FA, et al. Association of statin therapy with outcomes of acute coronary syndromes: the GRACE study. Ann Intern Med. 2004;140(11):857–66. [DOI] [PubMed] [Google Scholar]
- 44.Bosco E, et al. Major adverse cardiovascular event definitions used in observational analysis of administrative databases: a systematic review. BMC Med Res Methodol. 2021;21(1):1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bedetti G, et al. Comparison of prognostic value of echocardiacgraphic risk score with the Thrombolysis in Myocardial Infarction (TIMI) and Global Registry in Acute Coronary Events (GRACE) risk scores in acute coronary syndrome. Am J Cardiol. 2010;106(12):1709–16. [DOI] [PubMed] [Google Scholar]
- 46.Nassr OA, Forsyth P, and Johnson CF, Evaluation of discharge prescriptions for secondary prevention in patients with acute coronary syndromes in Iraq. Pharmacy Practice (Granada). 2019;17(1):1372. [DOI] [PMC free article] [PubMed]
- 47.Spruance SL, et al. Hazard ratio in clinical trials. Antimicrob Agents Chemother. 2004;48(8):2787–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lee JH, et al. Suboptimal use of evidence-based medical therapy in patients with acute myocardial infarction from the Korea Acute Myocardial Infarction Registry: prescription rate, predictors, and prognostic value. Am Heart J. 2010;159(6):1012–9. [DOI] [PubMed] [Google Scholar]
- 49.Ahmed KO, et al. Optimal medical therapy for secondary prevention of acute coronary syndrome: a retrospective study from a Tertiary Hospital in Sudan. Therapeut Clin Risk Manag. 2022;Volume 18:391–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.He X, et al. Impact of optimal medical therapy at discharge on one-year direct medical costs in patients with acute coronary syndromes: a retrospective, observational database analysis in China. Clin Therapeutics. 2019;41(3):456–65 e2. [DOI] [PubMed] [Google Scholar]
- 51.Hao J-Y, et al. Clinical prognosis of optimal medical therapy after percutaneous coronary intervention in patients with coronary heart disease. Chin Med J. 2021;134(16):2003–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Huffman MD, et al. Optimal in-hospital and discharge medical therapy in acute coronary syndromes in Kerala: results from the Kerala acute coronary syndrome registry. Circ: Cardiovasc Qual Outcomes. 2013;6(4):436–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hoedemaker NP, et al. Optimal medical therapy prescription in patients with acute coronary syndrome in the Netherlands: a multicenter pilot registry. Am J Cardiovasc Drugs. 2021;21:219–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bi Y, et al. Evidence-based medication use among Chinese patients with acute coronary syndromes at the time of hospital discharge and 1 year after hospitalization: results from the Clinical Pathways for Acute Coronary Syndromes in China (CPACS) study. Am Heart J. 2009;157(3):509–16 e1. [DOI] [PubMed] [Google Scholar]
- 55.Lee JH, et al. Contemporary trends of optimal evidence-based medical therapy at discharge for patients surviving acute myocardial infarction from the Korea Acute Myocardial Infarction Registry. Clin Cardiol. 2015;38(6):350–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Byeon HJ, Yang YM, Choi EJ. Optimal medical therapy for secondary prevention after an acute coronary syndrome: 18-month follow-up results at a tertiary teaching hospital in South Korea. Ther Clin Risk Manage. 2016;12:167–75. [DOI] [PMC free article] [PubMed]
- 57.Tra J, et al. Adherence to guidelines for the prescription of secondary prevention medication at hospital discharge after acute coronary syndrome: a multicentre study. Neth Hear J. 2015;23:214–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Redfern J, et al. Prescription of secondary prevention medications, lifestyle advice, and referral to rehabilitation among acute coronary syndrome inpatients: results from a large prospective audit in Australia and New Zealand. Heart. 2014;100(16):1281–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yan RT, et al. Age-related differences in the management and outcome of patients with acute coronary syndromes. Am Heart J. 2006;151(2):352–9. [DOI] [PubMed] [Google Scholar]
- 60.Fox AN, et al. Optimal medical therapy prescribing patterns and disparities identified in patients with acute coronary syndromes at an academic medical center in an area with high coronary heart disease-related mortality. Am J Cardiovasc Drugs. 2019;19:185–93. [DOI] [PubMed] [Google Scholar]
- 61.Damluji A, et al. Management of acute coronary syndrome in the older adult population: a scientific statement from the american heart association. Circulation. 2023;147:e32–62. 10.1161/CIR.1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gencer B, et al. Cognition after lowering LDL-cholesterol with evolocumab. J Am Coll Cardiol. 2020;75(18):2283–93. [DOI] [PubMed] [Google Scholar]
- 63.Olsson AG, et al. Effects of high-dose atorvastatin in patients≥ 65 years of age with acute coronary syndrome (from the myocardial ischemia reduction with aggressive cholesterol lowering [MIRACL] study). Am J Cardiol. 2007;99(5):632–5. [DOI] [PubMed] [Google Scholar]
- 64.Armitage J, et al. Efficacy and safety of statin therapy in older people: a meta-analysis of individual participant data from 28 randomised controlled trials. Lancet. 2019;393(10170):407–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Miettinen TA, et al. Cholesterol-lowering therapy in women and elderly patients with myocardial infarction or angina pectoris: findings from the Scandinavian Simvastatin Survival Study (4S). Circulation. 1997;96(12):4211–8. [DOI] [PubMed] [Google Scholar]
- 66.Nakamura T, et al. Optimal medical therapy after percutaneous coronary intervention in very elderly patients with coronary artery disease. Int J Cardiol Cardiovasc Risk Prev. 2023;16: 200162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Dagan M, et al. Sex disparity in secondary prevention pharmacotherapy and clinical outcomes following acute coronary syndrome. Eur Heart J-Qual Care Clin Outcomes. 2022;8(4):420–8. [DOI] [PubMed] [Google Scholar]
- 68.Haider A, et al. Sex and gender in cardiovascular medicine: presentation and outcomes of acute coronary syndrome. Eur Heart J. 2020;41(13):1328–36. [DOI] [PubMed] [Google Scholar]
- 69.Hay M, et al. Sex differences in optimal medical therapy following myocardial infarction according to left ventricular ejection fraction. Eur J Prev Cardiol. 2020;27(19):2348–50. [DOI] [PubMed] [Google Scholar]
- 70.van Oosterhout RE, et al. Sex differences in symptom presentation in acute coronary syndromes: a systematic review and meta-analysis. J Am Heart Assoc. 2020;9(9): e014733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lu HT, et al. Sex differences in acute coronary syndrome in a multiethnic Asian population: Results of the Malaysian National Cardiovascular Disease database—Acute Coronary Syndrome (NCVD-ACS) registry. Glob Heart. 2014;9(4):381–90. [DOI] [PubMed] [Google Scholar]
- 72.Lee CY, et al. Sex and gender differences in presentation, treatment and outcomes in acute coronary syndrome, a 10 year study from a multi-ethnic Asian population: The Malaysian National Cardiovascular Disease Database—Acute Coronary Syndrome (NCVD-ACS) registry. PLoS ONE. 2021;16(2): e0246474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Cirillo P, et al. Gender-related differences in antiplatelet therapy and impact on 1-year clinical outcome in patients presenting with ACS: the START ANTIPLATELET registry. Angiology. 2019;70(3):257–63. [DOI] [PubMed] [Google Scholar]
- 74.Dagan M, et al. Gender disparity in secondary prevention medication and outcomes following percutaneous coronary intervention for acute coronary syndrome. Heart Lung Circ. 2019;28:S400–1. [Google Scholar]
- 75.Madonis SM, Skelding KA, Roberts M. Management of acute coronary syndromes: special considerations in women. Heart. 2017;103(20):1638. [DOI] [PubMed] [Google Scholar]
- 76.Santopinto J, et al. Creatinine clearance and adverse hospital outcomes in patients with acute coronary syndromes: findings from the global registry of acute coronary events (GRACE). Heart. 2003;89(9):1003–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Anavekar NS, et al. Relation between renal dysfunction and cardiovascular outcomes after myocardial infarction. N Engl J Med. 2004;351(13):1285–95. [DOI] [PubMed] [Google Scholar]
- 78.Wison S, et al. Renal function and risk stratification in acute coronary syndromes. Am J Cardiol. 2003;91(9):1051–4. [DOI] [PubMed] [Google Scholar]
- 79.Fonarow GC, et al. Effect of statin use within the first 24 hours of admission for acute myocardial infarction on early morbidity and mortality. Am J Cardiol. 2005;96(5):611–6. [DOI] [PubMed] [Google Scholar]
- 80.Ray KK, Cannon CP. Early time to benefit with intensive statin treatment: could it be the pleiotropic effects? Am J Cardiol. 2005;96(5):54–60. [DOI] [PubMed] [Google Scholar]
- 81.Potpara TS, et al. Management of acute coronary syndrome in patients with non-valvular atrial fibrillation: results of the European Heart Rhythm Association Survey. Europace. 2014;16(2):293–8. [DOI] [PubMed] [Google Scholar]
- 82.Pizzetti F, et al. Incidence and prognostic significance of atrial fibrillation in acute myocardial infarction: the GISSI-3 data. Heart. 2001;86(5): 527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lau DH, et al. Prognostic impact of types of atrial fibrillation in acute coronary syndromes. Am J Cardiol. 2009;104(10):1317–23. [DOI] [PubMed] [Google Scholar]
- 84.Kirchhof P, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Kardiologia Polska (Polish Heart Journal). 2016;74(12):1359–469. [DOI] [PubMed] [Google Scholar]
- 85.Lingel JM, Srivastava MC, Gupta A. Management of coronary artery disease and acute coronary syndrome in the chronic kidney disease population—a review of the current literature. Hemodial Int. 2017;21(4):472–82. [DOI] [PubMed] [Google Scholar]
- 86.Hammer Y, et al. Guideline-recommended therapies and clinical outcomes according to the risk for recurrent cardiovascular events after an acute coronary syndrome. J Am Heart Assoc. 2018;7(18): e009885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Aarts BR, et al. Long-term clinical outcomes in patients with non-ST-segment elevation acute coronary syndrome and ST-segment elevation myocardial infarction with thrombolysis in myocardial infarction 0 flow. IJC Heart Vasc. 2023;48: 101254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Yudi MB, et al. Prognostic significance of suboptimal secondary prevention pharmacotherapy after acute coronary syndromes. Intern Med J. 2021;51(3):366–74. [DOI] [PubMed] [Google Scholar]
- 89.Sawano M, et al. One-year outcome after percutaneous coronary intervention for acute coronary syndrome-an analysis of 20,042 patients from a Japanese Nationwide Registry-. Circ J. 2021;85(10):1756–67. [DOI] [PubMed] [Google Scholar]
- 90.Daida H, et al. Management and two-year long-term clinical outcome of acute coronary syndrome in Japan-Prevention of AtherothrombotiC Incidents Following Ischemic Coronary Attack (PACIFIC) Registry–. Circ J. 2013;77(4):934–43. [DOI] [PubMed] [Google Scholar]
- 91.Lee JH, et al. Contemporary trends of optimal evidence-based medical therapy at discharge for patients surviving acute myocardial infarction from Korea acute myocardial infarction registry. Am Heart Assoc. 2013;38(6):350–6. [DOI] [PMC free article] [PubMed]
- 92.Cirillo P, et al. Optimal medical therapy on top of dual-antiplatelet therapy: 1-year clinical outcome in patients with acute coronary syndrome: the START antiplatelet registry. Angiology. 2020;71(3):235–41. [DOI] [PubMed] [Google Scholar]
- 93.Faridi KF, et al. Timing of first postdischarge follow-up and medication adherence after acute myocardial infarction. JAMA Cardiology. 2016;1(2):147–55. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Information is accessible upon justifiable request. The corresponding author can provide all pertinent information upon reasonable request, including the data and materials supporting the study's findings.
No datasets were generated or analysed during the current study.