Abstract
Background
Surgical care in the operating room (OR) contributes one-third of the greenhouse gas (GHG) emissions in healthcare. The European Association of Endoscopic Surgery (EAES) and the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) initiated a joint Task Force to promote sustainability within minimally invasive gastrointestinal surgery.
Methods
A scoping review was conducted by searching MEDLINE via Ovid, Embase via Elsevier, Cochrane Central Register of Controlled Trials, and Scopus on August 25th, 2023 to identify articles reporting on the impact of gastrointestinal surgical care on the environment. The objectives were to establish the terminology, outcome measures, and scope associated with sustainable surgical practice. Quantitative data were summarized using descriptive statistics.
Results
We screened 22,439 articles to identify 85 articles relevant to anesthesia, general surgical practice, and gastrointestinal surgery. There were 58/85 (68.2%) cohort studies and 12/85 (14.1%) Life Cycle Assessment (LCA) studies. The most commonly measured outcomes were kilograms of carbon dioxide equivalents (kg CO2eq), cost of resource consumption in US dollars or euros, surgical waste in kg, water consumption in liters, and energy consumption in kilowatt-hours. Surgical waste production and the use of anesthetic gases were among the largest contributors to the climate impact of surgical practice. Educational initiatives to educate surgical staff on the climate impact of surgery, recycling programs, and strategies to restrict the use of noxious anesthetic gases had the highest impact in reducing the carbon footprint of surgical care. Establishing green teams with multidisciplinary champions is an effective strategy to initiate a sustainability program in gastrointestinal surgery.
Conclusion
This review establishes standard terminology and outcome measures used to define the environmental footprint of surgical practices. Impactful initiatives to achieve sustainability in surgical practice will require education and multidisciplinary collaborations among key stakeholders including surgeons, researchers, operating room staff, hospital managers, industry partners, and policymakers.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00464-024-11141-x.
Keywords: Sustainability, Minimally invasive surgery, Climate change, Greenhouse gas emissions, Recycling, Surgical waste
Climate change is recognized as the greatest public health threat of the twenty-first century [1]. Climate change is associated with an increase in infectious diseases, respiratory, neurological and cardiovascular complications, as well as mortality [2]. It has also been reported to adversely affect mental health, pregnancy, nutrition [2]. Healthcare is the second-leading contributor to waste in the United States [3], and is responsible for 10% of the nation’s greenhouse gas (GHG) emissions [4]. Surgery is responsible for up to one-third of waste in healthcare [5]. Surgical care in Canada, the United Kingdom, and the United States emits 9.7 million tons of carbon dioxide equivalents (CO2eq) per year, with the equivalent climate impact of 2 million motor vehicles [6]. Operating rooms (OR) are the most resource-intensive area of the hospital due to the use of consumables, anesthetic gases, sterilization processes, and significantly high energy requirements [7, 8]. Gastrointestinal surgery produces the third-highest output of solid waste per case relative to other specialties [5]. The rapid adoption of minimally invasive surgery (MIS) has accelerated the reliance on single use equipment, waste production, and energy consumption. The clinical benefits of MIS must be weighed against its relative contribution to the OR carbon footprint [5, 9].
Hospitals and health sector companies are systematically decarbonizing the healthcare supply chains in line with the US & European Union’s pledge to cut GHG emissions in half by 2030[10, 11] Although initiatives targeted at reducing carbon emissions in the operating room are anticipated to be among the most impactful within healthcare, organizational leadership in such efforts has been slow and disjointed [12, 13]. Healthcare organizations have had limited success in engaging perioperative leadership. One obstacle to developing sustainable surgical practices is a lack of knowledge among perioperative teams about the relative contribution of operative elements to the carbon footprint [7, 14]. The limited understanding among healthcare providers, lack of standardized protocols, and absence of evidence-based guidelines, has limited efforts to implement green initiatives, especially due to the uncertainty of overall impact of the carbon footprint.
The EAES (European Association of Endoscopic Surgery) and SAGES (Society of American Gastrointestinal and Endoscopic Surgeons) created a Sustainable Surgical Practices (SSP) Joint Task Force in response to this global environmental challenge (https://eaes.eu/sustainability-in-surgical-practice/; SUSTAINABILITY IN SURGICAL PRACTICE—SAGES). The aim is to develop actionable recommendations to inform members of the best practices in mitigating climate risk in surgical practice, specifically in MIS. The SSP Task Force embarked on a scoping review of all relevant publications on the topic of sustainability measures, practice, and initiatives in the field of gastrointestinal surgery.
Materials and methods
The EAES and SAGES conducted a scoping review in alignment with methodological guidance from the JBI Scoping Review Methodology Group [15]. We followed the reporting standards for the Preferred Reporting Items for Systematic Review and Meta-Analysis Extension for Scoping Reviews (PRISMA-ScR) according to our protocol (supplementary appendix 1) [16]. The review aimed to address the following research questions:
What is the fundamental, core terminology in sustainability research relevant for surgeons and researchers?
Are there evidence-based outcome measures used in sustainability research?
What is the scope of sustainability relevant to gastrointestinal surgical practice?
What is the climate impact of surgical practice, including:
All general surgical procedures performed in the operating room.
Anesthesia practice (e.g., choice of anesthetic).
Any practices in the operating room that may impact the environment.
What evidence exists to support the practical implementation of green surgery initiatives to achieve sustainable surgical practice?
Literature search & inclusion criteria
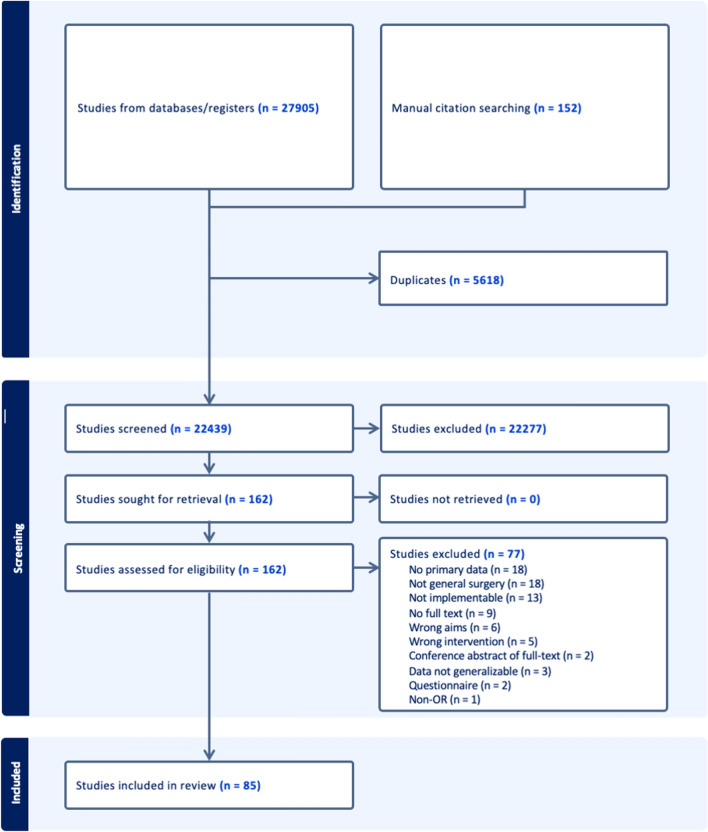
A comprehensive search strategy was developed with the help of an academic health sciences librarian with expertise in scoping reviews (Fig. 1). MEDLINE via Ovid, Embase via Elsevier, Cochrane Central Register of Controlled Trials, and Scopus were queried from inception to August 25th, 2023 to identify key articles of interest (Table 1). Backward and forward manual citation searching were conducted on all included articles to identify additional articles of interest. Search syntax is available in supplementary appendix 2.
Fig. 1.
Literature search overview
Table 1.
Inclusion & exclusion criteria
| Inclusion criteria | Exclusion criteria | |
|---|---|---|
| Design |
RCTs, prospective studies, observational studies Life-cycle assessments Conference proceedings |
*Non-primary literature Systematic reviews (SR), meta-analyses (MA) Standards of practice Case reports, questionnaires, narrative reviews, commentaries, editorials, letter to the editor, opinion articles |
| Population |
Studies assessing topics of sustainability in: 1Gastrointestinal surgical practice Adult and pediatric surgery 2General practice in the operating room |
Animal studies Veterinary studies Studies assessing sustainability topics notrelated to 1gastrointestinal surgical practice Studies assessing endoscopic 3procedures Studies assessing infrared-guided procedures or interventions |
| Aims |
Studies assessing the 4climate impact of gastrointestinal surgical practice Studies assessing practically implementable 5interventions or initiatives to promote sustainable surgical practice |
Studies assessing basic science topics (non-clinical) Studies assessing interventions or initiatives in surgery with novel, innovative technology, or equipment Studies evaluating clinical outcomes of interventions or initiatives in surgery |
| Studies evaluating cost of interventions or initiatives in surgery | Studies describing global surgery initiatives | |
| Studies assessing telehealth or telemedicine |
1Gastrointestinal surgery defined as below:
All procedures performed in the operating room such as laparoscopic cholecystectomy, totally extraperitoneal hernia repair (TEP).
Includes open and minimally invasive (laparoscopic & robotic) surgery
2General practice in the operating room:
Anesthesia practice (e.g., choice of anesthetic)
Air treatment practices
Any practices in the operating room that may impact the environment
3Endoscopic procedures: colonoscopy, esophagogastroduodenoscopy, laryngoscopy, cystoscopy, etc.
4Climate impact:
Climate change (CO2eq)
Study selection & data extraction
Records identified by the systematic literature search were uploaded to Covidence for the screening phase. A review team was led by a review coordinator with experience in systematic and scoping review methodology. Literature screening was performed in two rounds; first by title and abstract and second by full-text. Each article was screened by a minimum of two reviewers. Prior to the first round of screening, a pilot screening round was conducted with a sample of 25 abstracts. After abstracts were screened independently, the review team met to calibrate reviewer selections. Next, the first round of screening by title and abstract was conducted using the inclusion criteria outlined in Table 1. Prior to entering the second round of screening, pilot screening was completed using five full-text articles. An additional meeting was held to calibrate reviewer selections. Finally, the second round of full-text screening was conducted. Throughout both rounds of screening, reviewers met to resolve discrepancies and when necessary, a senior author was available to reconcile disagreements.
Included articles from both rounds of screening entered data extraction. Data extraction from included studies was conducted independently, while each article was extracted by two team members. In cases of discrepancies, resolution was achieved through consensus. For any unresolved discrepancies, a senior author with content expertise was consulted to achieve resolution.
Data analysis
Quantitative data were summarized using descriptive statistics. Baseline characteristics of included articles were summarized using counts and percentages, including practice setting, study design, the reporting of educational/behavior change programs, and the use of core outcome measures applied in included studies for analysis. Descriptive analysis was supported by graphical representations in diagrammatic form when applicable. A narrative summary was developed to accompany the findings.
Scope of sustainability in surgical practice
Studies available in the literature spanned all three scopes delineated in the Greenhouse Gas (GHG) Protocol (https://ghgprotocol.org/) [17, 18]. Measurements of the environmental impact of costly and environmentally harmful anesthetic gases and the multiple interventions to reduce anesthetic gas emissions fall under Scope 1. Initiatives to decrease energy consumption in the OR, whether by implementing occupancy-based LED lighting, anesthetic gas scavenging, or Heating, Ventilation, & Air Conditioning (HVAC) systems, fall under Scope 2 of the GHG Protocol. Additionally, studies focusing on waste reduction and the carbon footprint of the supply chain would be categorized into Scope 3. Water consumption, which is not captured by the GHG Protocol, is equally an important scope in the climate impact of surgical care. Studies were classified according to study design as cohort studies, randomized controlled trials (RCTs), computational studies, correspondence articles with primary data, and LCA studies.
Concepts, terminology, and definitions
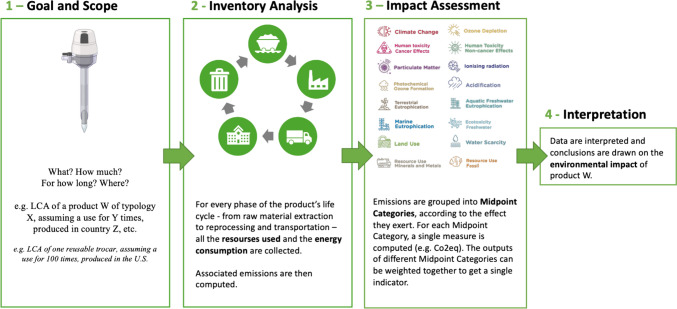
Key concepts, terminology, and definitions applied in the assessment and measurement of sustainability in surgical practice are summarized in Table 2. LCA is defined as a systematic approach to evaluate and quantify the environmental impacts associated with a product, process, or service, examining every stage in its life cycle. LCAs are widely recognized as the benchmark for measuring environmental impact [19]. ISO 14040 and 14,044 are international standards which provide an important framework for LCAs. Unique outcomes can be measured in LCAs including terrestrial, freshwater, and marine ecotoxicity, human carcinogenic toxicity, land use, ionizing radiation, and marine eutrophication (Fig. 2) [20].
Table 2.
Glossary of core terminology for sustainability in gastrointestinal surgical practice
| Terms | Definitions |
|---|---|
| Principles | |
| Circular economy | A model of economy that involves activities that are restorative or regenerative by design and aims for the elimination of waste through the superior design of materials, products, and systems |
| Climate change | Shifts in weather and climate patterns that occur over long periods of time, acknowledging that the current warming temperature is caused primarily by human activity |
| Decarbonize | The act of reducing the amount of GHG emissions associated with a process or product, with the goal of being net neutral |
| Green | A colloquial term to refer to initiatives, products or practices that have environmental benefits such as reduced use of environmental resources |
| Greenhouse gas (GHG) | A gas (primarily CO2 but including CH4, N2O, and others) that absorbs, traps, and re-emits heat and radiant energy back into the earth's atmosphere |
| Planetary health | An emerging concept that prioritizes solutions that simultaneously benefit human health and advance environmental sustainability |
| Sustainability | Meeting the needs of the present without compromising the ability of future generations to meet their own (UN Brundtland Commission) |
| Study Designs | |
| Life Cycle Assessment (LCA) | Life cycle assessments are a rigorous methodology for studying the environmental impact of a product or process. LCAs consider both the upstream and disposal of products to capture all inputs and outputs. Outcomes measured LCAs include a comprehensive range of outcome measures. While time intensive, these are the gold standard for sustainability studies |
| Outcome Measures | |
| Carbon dioxide equivalents (CO2eq) | A measure of the carbon dioxide required to generate a corresponding amount of climate impact, which allows for comparison. It is an outcome measure used to compare the emissions from various greenhouse gases based on their global-warming potential (GWP), by converting amounts of other gases to the equivalent amount of CO2 with the same global warming potential. CO2eq are expressed as unit of mass. The International System of Units (SI) unit of mass is the kilogram (consider that multiples—as tons—often applies) |
| Cost | An economic measure of resource consumption most commonly in euros, US dollars, or some other currency |
| Ecosystem quality (PDF*m2*year or species.year) | A measure of the effect on biodiversity caused by climate change, marine acidification, land use, toxic substances (freshwater ecotoxicity), substances that cause terrestrial and aquatic acidification, freshwater and marine eutrophication. It can be expressed as potentially disappeared fraction (PDF)* of species over a certain area over a certain time (PDF.m2.yr) or as species over year (species.yr).[104] |
| Energy (kWh, MJ) | A measure of the amount of energy used to deliver surgical care. The International System of Units (SI) unit of energy is the joule (megajoules—MJ—typically applies), while the non-SI unit is the energy delivered by one kilowatt of power for one hour (kWh) |
| Human health (DALY/person/year) | A measure of the impact of climate change on human health in disability-adjusted-life-years (DALY). One DALY represents the loss of the equivalent of one year of full health. The unit commonly used to express Human Health is the number of DALYs per person per year (DALY/person/yr).[105] |
| Waste (kg) | A measure of the amount of waste generated to deliver surgical care, typically express as a mass. Less commonly reported in L |
| Water (L) | A measure of the amount of water used to deliver surgical care, typically expressed as a volume. Less commonly reported as m3 or kg |
Fig. 2.
Overview of life-cycle assessment
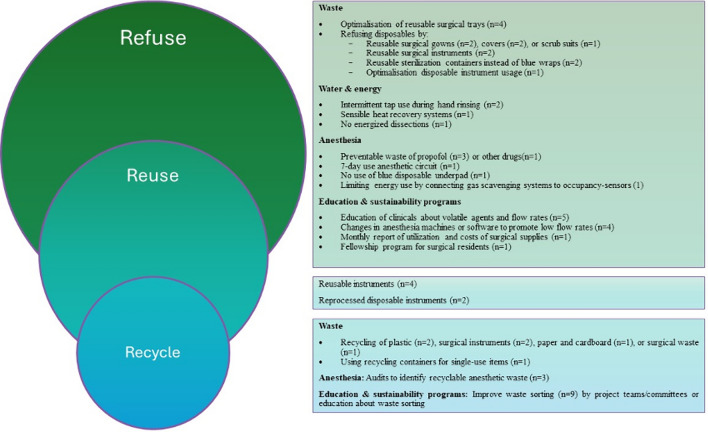
Another key concept with a strong framework in sustainability research is the 10R model of the circular economy. [21] This approach prioritizes strategies based on their potential to minimize emissions. These strategies are ranked by their effectiveness and include the need to refuse, reduce, rethink, reuse, repair, refurbish, remanufacture, repurpose, recycle, and recover (Fig. 3) [21]. By adopting these practices, organizations can transition toward a more sustainable and circular approach to design and production. The goal is to minimize waste, conserve resources, and create products that contribute positively to the environment and society. We used the 10R model to organize and present the findings of the scoping review.
Fig. 3.

10R model of circular economy
Results
A total of 22,439 articles were screened to yield 85 relevant papers (Fig. 1). Studies were conducted in the settings of anesthesia (n = 30/85, 35.3%), general surgical practice (n = 35/85, 41.2%), and gastrointestinal surgery (n = 21/85, 24.7%). There were 51/85 (60.0%) prospective studies, 7/85 (8.2%) retrospective studies, 9/85 (10.6%) correspondence articles, and 12/85 (14.1%) LCA studies (Table 3). No studies applied the 10R model. With respect to scope, there were 17/85 (20.0%) articles related to Scope 1 (anesthetic gas), 4/85 (4.7%) articles to Scope 2 (energy), 53/85 (62.4%) to Scope 3 (waste), and 4/85 (4.7%) articles to water consumption (Table 3).
Table 3.
Characteristics of studies evaluating sustainability in the operating room for gastrointestinal surgery, general surgical practice, and anesthesia
| Author | Country | Study design | Single vs multisite | Aim | Scope | Surgical procedure |
|---|---|---|---|---|---|---|
| Gastrointestinal surgery | ||||||
| Adler, 2005 | Germany | Case study | NR | Reusable vs disposable | 3* | Laparoscopic cholecystectomy |
| Agarwal, 2010 | India | Prospective | Single | Energy | 2 | Laparoscopic cholecystectomy |
| Billings, 2017 | USA | Prospective | – | Waste—impact | 3 | Elective colectomy |
| Bischofberger, 2023 | Switzerland | Prospective | Single | Anastomotic leaks | 3 | – |
| Blankush, 2021 | USA | LCA | – | Open vs robotic | 3 | Ventral hernia repair |
| Boag, 2022 | UK | Prospective | Multisite | Leaner equipment | 3 | Laparoscopic appendectomy |
| Boberg, 2022 | Sweden | LCA | – | Reusable vs disposable | 3 | Laparoscopic cholecystectomy |
| Brady, 2017 | USA | Prospective/Retrospective | – | Reusable vs disposable | 3 | Laparoscopic colectomy |
| Caycedo-Marulanda, 2020 | Canada | Correspondence with primary data | Multisite | Anesthetic gas | 1 | taTME |
| Colak, 2004 | Turkey | RCT | – | Reusable vs disposable | 3 | Laparoscopic cholecystectomy |
| Dettenkofer, 1999 | Germany | LCA | – | – | Waste | 3 | – |
| Ford, 2022 | UK | Prospective | Single | Leaner equipment | 3 | Laparoscopic appendectomy |
| Gough, 2022 | UK | Prospective | Leaner equipment | 3 | Laparoscopic cholecystectomy | |
| Graham, 2019 | USA | Retrospective | – | Waste—impact | 3 | Laparoscopic appendectomy |
| Labib, 2023 | UK | Prospective | Multisite | Leaner equipment | 3 | Laparoscopic appendectomy |
| Park, 2021 | USA | Prospective | – | Education—surgeon report card | 3 | Multiple |
| Petterwood, 2009 | Australia | Prospective | – | Water | - | – |
| Rizan, 2022 | UK | LCA | Single | Reusable vs disposable | 3 | Laparoscopic cholecystectomy |
| Robb, 2022 | UK | Prospective | – | Anesthetic gas | 1 | Inguinal hernia repair |
| Sullivan, 2023 | USA | Prospective | – | Waste—impact | 3 | Multiple pediatric |
| Vacharathit, 2021 | USA | Correspondence | ||||
| With primary data | – | Education—Fellowship program | 1,2,3 | – | ||
| General surgical practice | ||||||
| Burguburu, 2022 | France | LCA | Multisite | Reusable vs disposable | 3 | – |
| Cannings, 2022 | UK | Correspondence | ||||
| With primary data | Water—scrubbing | - | Multiple | |||
| Chasseigne, 2018 | France | Prospective | Multisite | Waste—impact | 3 | Multiple |
| Conrardy, 2010 | USA | Correspondence | ||||
| With primary data | Single | Reusable vs disposable | 3 | Multiple | ||
| Cunningham, 2023 | USA | Retrospective/ Prospective | Single | Leaner equipment | 3 | Multiple |
| Friedericy, 2022 | The Netherlands | LCA | Multisite | Waste—recycling | 3 | – |
| Gilliam, 2008 | UK | Correspondence | ||||
| With primary data | Single | MIS | 3 | Multiple laparoscopic general surgery | ||
| Ibbotson, 2013 | Germany | LCA | Single | Reusable vs disposable | 3 | – |
| Jehle, 2008 | UK | Retrospective/Prospective | Single | Water—scrubbing | – | Multiple |
| MacNeill, 2017 | Canada/USA/UK | LCA | Multisite | Waste—impact | 3 | Multiple |
| Martin, 2022 | France | Correspondence | ||||
| With primary data | Multisite | Waste- recycling | 3 | Multiple | ||
| Martin, 2017 | United States | Prospective | Single | Waste—recycling | 3 | Multiple |
| McKendrick, 2017 | United Kingdom | Prospective | Single | Waste—recycling | 3 | Multiple |
| Moreno, 2019 | Spain | Computational | Single | Waste—impact | 2 | – |
| Ramos, 2023 | Denmark | Prospective | Single | Energy—air recycling | 3 | Multiple |
| Rizan, 2022 | UK | Retrospective | Single | Reusable vs disposable | 3 | Multiple |
| Rouvire, 2022 | France | LCA | Multisite | Waste—recycling/disposal | 3 | Multiple |
| Sadler, 2017 | UK | Prospective | Single | Waste—impact | 3 | Multiple |
| Singleton, 2019 | UK | Prospective | Single | Reusable vs disposable | 3 | – |
| Sinha, 2023 | UK | Correspondence | ||||
| With primary data | Single | Waste—recycling | 3 | Simple skin excision | ||
| Somner, 2008 | UK | Prospective | Single | Waste—impact | 3 | – |
| Tieszen, 1992 | USA | Retrospective | – | Water—scrubbing | – | Multiple |
| Van Straten, 2021 | Netherlands | Prospective | Multisite | Waste—recycling | 3 | – |
| Vozzola, 2020 | USA | LCA | Single | Reusable vs disposable | 3 | – |
| Wormer, 2013 | USA | Prospective | Multisite | Reusable vs disposable | 3 | – |
| Wyssusek, 2016 | Australia | Prospective | Single | Waste—impact, recycling | 3 | – |
| Wyssusek, 2020 | Australia | Prospective | Single | Waste—impact, recycling | 3 | – |
| Amariglio, 2021 | Italy | Prospective | Single | Waste—impact | 3 | Multiple |
| Dohmen, 2023 | Germany | Prospective | Single | Waste—impact | 3 | Multiple |
| Mhlaba, 2015 | USA | Prospective | Single | Reusable vs disposable | 3 | Multiple |
| Nast, 2019 | USA | Prospective | Single | Reusable vs disposable | 3 | Multiple urology |
| Power, 2012 | USA | Retrospective | Single | Leaner equipment | 3 | Multiple |
| Rizan, 2022 | UK | LCA | Single | MIS | 3 | – |
| Rizan, 2023 | UK | Prospective | Multisite | Reusable vs disposable | 3 | Multiple |
| Anesthesia | ||||||
| Alexander, 2018 | Canada | Correspondence | ||||
| With primary data | Multisite | Anesthetic gas | 1 | – | ||
| Atcheson, 2016 | USA | Prospective | Single | Anesthetic gas | 1 | Multiple |
| Baloi, 2018 | UK | Prospective | Multisite | Waste—impact | 3 | Multiple |
| Benness, 2021 | Australia | Prospective | Single | Anesthetic gas | 1 | Multiple |
| Boyle, 2018 | UK | Prospective | Multisite | Anesthetic gas | 1 | Multiple |
| Carter, 2019 | UK | Prospective | Single | Anesthetic gas | 1 | – |
| Caycedo-Marulanda, 2022 | Canada | Correspondence with primary data | Single | Anesthetic gas | 1 | – |
| Chambrin, 2023 | France | Retrospective | Single | Anesthetic gas | 1 | Multiple |
| Connolly, 2019 | Australia | Prospective | Single | Waste—recycling | 3 | Multiple |
| Davies, 2023 | Australia | Prospective | Multisite | Waste—impact, recycling | 3 | Multiple |
| Fraifeld, 2021 | USA | Prospective | Single | Waste– impact, recycling | 3 | Multiple |
| Glenski, 2020 | USA | Prospective | Multisite | Anesthetic gas | 1 | Multiple pediatric |
| Hansen, 2023 | USA | Prospective | Single | Anesthetic gas | 1 | Multiple pediatric |
| Hickman, 2021 | UK | Prospective | Multisite | Energy | 2 | Multiple |
| Hubbard, 2017 | USA | Prospective | Single | Anesthetic gas | 1 | Multiple |
| Ito, 2021 | UK | Prospective | Single | Anesthetic gas | 1 | Multiple |
| Kaniyil, 2017 | India | Prospective | Single | Waste—impact | 3 | Multiple |
| Langbein, 1999 | Germany | Laboratory | Single | Waste—impact | 3 | – |
| Livingston, 2019 | Scotland | Prospective | Single | Waste—recycling | 3 | Multiple |
| Mankes, 2012 | USA | Prospective | Single | Waste—impact | 3 | Multiple |
| McGain, 2009 | Australia | Prospective | Single | Waste—impact | 3 | Multiple |
| McGain, 2010 | Australia | LCA | Single | Waste—impact | 3 | Multiple |
| McGain, 2014 | Australia | Prospective | Single | Waste—impact | 3 | Multiple |
| Nesaratnam, 2018 | UK | Prospective | Single | Waste—impact | 3 | Multiple |
| Pierce, 2014 | UK | Prospective | Single | Energy | 2 | Multiple |
| Ryan, 2010 | US | Laboratory | Single | Anesthetic gas | 1 | – |
| Sherman, 2012 | USA | LCA | Single | Anesthetic gas | 1 | – |
| Sulbaek Andersen, 2010 | USA | Prospective | Single | Anesthetic gas | 1 | Multiple |
| Wyssusek, 2022 | Australia | Retrospective | Single | Anesthetic gas | 1 | Multiple |
| Zuegge, 2019 | USA | Retrospective | Single | Anesthetic gas | 1 | Multiple |
*Three Scopes defined in the GHG Protocol (https://ghgprotocol.org/) [17, 18]
Scope 1: Measurements of the environmental impact of costly and environmentally harmful anesthetic gases and the multiple interventions to reduce anesthetic gas emissions
Scope 2: Initiatives to decrease energy consumption in the OR, whether by implementing occupancy-based LED lighting, anesthetic gas scavenging, or HVAC systems
Scope 3: Additionally, studies focusing on waste reduction and the carbon footprint of the supply chain
Outcome measures
Outcomes evaluated in the included studies demonstrated substantial heterogeneity. The most commonly studied outcome measure was CO2eq in 39/85 (45.9%) studies, with most studies measuring kilograms (kg) CO2eq. The cost of resource consumption was the second most commonly studied outcome across 32/85 (37.6%) studies in US dollars, euros, or some other form of currency. Surgical waste was measured in 28/85 (32.9%) studies and were typically reported in units of mass (kg) or volume in liters (L). Water consumption was evaluated in 11/85 (12.9%) articles in liters (L) or less commonly in kg. Energy consumption was assessed in 7/85 (8.2%) studies in kilowatt-hours (kWh), or less commonly in megajoules (MJ). The impact on human health was measured in disability-adjusted life-years (DALYs) in 3/85 (3.5%) articles, and ecosystem damage (PDFm2/yr) in 2/85 (2.4%) studies. Key outcomes studied in LCAs include the climate change impact (kg of CO2eq), ecosystem damage (PDFm2yr),
Climate impact
Surgical care exerts up to 5,187,936 kg of CO2eq annually from one academic institution, alone [6]. Some contributors to climate impact are undesired, but to some extent uncontrollable. For example, anastomotic leaks are associated with an average climate, water and waste impact per patient of 1303kgCO2eq, 1803m3 of water and 123 kg waste, respectively, including diagnosis, inpatient stay in addition to treatment and monitoring [22]. Thus, it is helpful to focus on contributors to climate change that are within the control of surgical teams. Studies included in this review did not apply the 10R framework, but their findings can be re-conceptualized using portions of this framework including refuse, reuse, and recycle (Fig. 4).
Fig. 4.
Study findings aligned with the 10R model
Refuse
Waste: It is estimated that $368 of waste is generated per case across general surgical procedures due to unnecessary equipment use of sutures, staplers reload, and other items [23]. This amounts to a total preventable annual cost of $18,410 across 50 common general surgery cases [23]. Chasseigne et al. reported that wasted supplies represent 20.1% of the total cost allocated to surgical supplies [24]. For common procedures such as appendectomy, it is estimated that 75% of equipment-related consumables could be reduced [25]. Up to 59% of surgical instrument trays may be unused, leading to unnecessary water and energy uses for sterilization. [26]
Water, Energy, & MIS: There is interest in the use of alcohol-based scrubs to mitigate water use. Canning and colleagues showed that 1,606,692L of water would be saved with alcohol-based rather than soap and water-based scrubbing, equating to 2.2 tons of carbon saved annually [27]. Similarly, Jehle et al. showed that over 15,500 procedures performed in a 1-year period, 931,938L of water would be saved with alcohol-based agents [28].
Anesthesia: Anesthetic gases have been known to significantly impact the environment since 1999.[29] Desflurane exerts the greatest impact on global warming compared to isoflurane or sevoflurane [30], even after accounting for resource extraction and manufacturing of anesthetic drugs, transport to health care facilities, clinical use, and disposal or emission to the environment [31]. Caycedo-Marulanda and colleagues showed a lower impact on CO2eq with sevoflurane (8.4 kg) compared to desflurane (408.6 kg) for transanal total mesorectal excision (taTME) surgery [32]. Given the higher costs and environmental impact of desflurane, some hospitals have chosen to stop using this agent altogether. Caycedo-Marulanda et al. found that when their facility implemented a desflurane-free strategy in their operating rooms there was a significant reduction in CO2eq [33]. Hansen et al. combined the removal of desflurane from the formulary with avoiding nitrous oxide, decreasing flow rates, and applying educational initiatives. These practices reduced GHG emissions by 87% and CO2eq from volatile anesthetics > 50% [34].
Rethink
Waste: Considering alternative approaches to surgical care can mitigate the impact of surgery on the environment. It has been shown that the use of clips for appendectomies produces 10.2 g of waste per case compared to 975.1 g per case with staplers, resulting in equivalent efficacy and cost savings of $286.33 per case in 2019 [35]. Additionally, sterilization processes may be modified with the use of rigid sterilization containers to reduce the carbon footprint by 85% compared to disposable blue wraps, with an ecological advantage after 98 of 5,000 use cycles. Moreover, rigid sterilization container use resulted in 84.5% less environmental impact in terms of eco-costs, with an ecological advantage already occurring after 67 out of 5000 use cycles [36].
MIS: In addition to waste, MIS exerts additional impact on the overall surgical footprint. Blankush et al. performed a LCA that demonstrated that robotic approaches consume 143% more energy than open approaches for ventral hernia repair, equating to an additional 1.4 barrel of oil equivalents per procedure, resulting in 144% (609 kg CO2eq) more GHG emissions. Robotic ventral hernia repair resulted in 18% more solid waste per case; with downstream environmental impact causing an incremental loss of 1.9 × 10–3 DALYs per case [37]. In laparoscopic surgery, Gillam reported that climate impact from CO2 use alone in 2006 was minimal [38]. However, Power et al. reviewed over two million laparoscopic cases performed in the USA in 2009, showing that laparoscopic procedures produced 355,924 tons of CO2/year when accounting for the transportation, capture, and compression of CO2. [39] Notably, length of stay was not captured in these studies, and it has been established that MIS reduces the length of stay, the rate of complications, and healthcare costs compared to open surgery [40]. The impact of these factors on the climate impact of MIS has yet to be elucidated.
Anesthesia: Robb et al. reported a saving of 10.2 kgCO2e/case by using local anesthetic instead of general anesthesia for inguinal hernias [41]. Ensuring appropriate triage of the urgency of cases may also ameliorate the impact of surgical care, as an analysis of four anesthetic gases showed that the highest CO2kg/hr was recorded for emergency (17.6), followed by elective cases (7.7) due to excessive gas flow rates [42].
Reduce
Waste: Many initiatives aimed to reduce surgical waste. Boag et al. downsized laparoscopic appendectomy instrument trays from 119 to 49 items, saving 7.48kgCO2eq and £25.1 per procedure [43]. Leaning appendectomy trays to reduce consumables can save a net £34,423- £219,452 and 512kgCO2eq -3.02 tons CO2eq per year over a predicted seven-year life span of instruments [25, 44]. Despite an investment needed to lean equipment trays, the investment of £19,731 was recuperated within six months [25]. Elsewhere, Cunningham and colleagues removed 46 items across 113 pediatric procedures which, saved $27,503 in surgical equipment acquisition costs and prevented > 6,000 tons of waste annually [45]. Similarly, authors reduced instruments trays for orchiopexy and inguinal hernia repairs from 57 to 35 instruments, which saved $3,489.42 annually [46].
In contrast, Sinha and colleagues analyzed the waste generated by full drape coverage, fully gowned and gloved surgeon versus a pragmatic draping policy with single fenestrated drape and only sterile gloves, for minor surgeries as simple skin incisions. The full approach produced 596 g of plastic waste per patient (£14.62 per patient) while pragmatic draping policy in 120 g of plastic waste per patient (£8.53/ per patient) [47].
Water & Energy: With respect to mitigating the use of water, Petterwood et al. compared two scrub techniques: continuous tap flow versus intermittent tap use during hand rinsing. The latter resulted in a 71% water savings (15.5L reduced to 4.5L) [48]. Similarly, Somner and colleagues reported that having the tap on for only one as opposed to two minutes reduced the use of water by 5.7L per surgical scrub [49].
Mitigating the use of energy can also improve the climate impact of surgery. Authors have shown that installing a sensible heat recovery system in the operating room recirculates 50% of the airflow in the theater, reducing energy demands by 44.3%, equating to 49, 261.9 kWh/year, saving €7,389.29 annually [50]. Conversely, Agarwal et al. reported a reduction from 57 to 39 L CO2 per laparoscopic cholecystectomy without energized dissection [51].
Anesthesia: In addition to anesthetic gases, other medications used in anesthesia are costly, resource intensive to produce, and contribute to environmental contamination. Atcheson et al. looked at the preventable anesthetic waste in 543 separate surgical cases and found that the estimated yearly cost of preventable anesthetic drug waste was $185,250 [52]. Studies by Baloi and Butt, Kaniyil et al., and Mankes found that the highest volume of drug waste is propofol [53–55]. This finding led to a change in formulary at one hospital with 50 mL and 100 mL bottles of propofol exchanged for 20 mL bottles, with a resultant decrease in propofol waste from 29 mL/day/bin to 3 mL/day/bin [55].
McGain et al. (2014) evaluated the difference in microbial contamination with different frequency of anesthetic circuit changes in the setting of single use airway filters. They found that there was no difference in proportion of circuit contamination if changed every 24 h (57/105), 48 h (43/100) or 7 days (46/100). This resulted in $4,846 savings per year (for 6 ORs) as well as decreased sterilizer loads saving 2760 kWH per year and 48,000 L of water [56]. Furthermore, Pierce et al. attempted to mitigate energy use by using meters of outlets for machines and in-use energy estimates for the anesthetic gas scavenging system. The total energy use per day for anesthesia was 28kWH per theater, with the majority (18kWH) of this energy coming from the anesthetic gas scavenging system [57]. Hickman et al. found that 14 of 29 anesthetic gas scavenging systems were on inappropriately, generating 26,980kWH of unnecessary energy use. By connecting the scavenging system to existing occupancy-sensors used for the HVAC system, they reduced the time the system was running when the operating room was unoccupied, preventing the generation of 14.3 tons of CO2 across the 29 OR system in a single year [58].
Education/Sustainability Programs: Initiatives to educate surgical staff on the climate impact of surgery have been implemented. Park et al. applied a monthly surgeon report card detailing the utilization and cost of disposable and reusable surgical supplies on cost and waste reduction for pediatric laparoscopic procedures, showcasing a reduction of 43% of costs (from $631 to $235 median supply cost per case). This also reduced the use of disposable trocars by 56% and of disposable harmonics and staplers by 33% [59]. Vacharathit et al. reported the 5-year results of a fellowship program for surgical residents in healthcare sustainability, primarily focused on greening the OR which resulted in 116,865 gallons of water saved per year with education on water waste, scrub-less surgical solutions and motion activated faucets; 1 million pounds of plastics diverted from landfill, regulated medical waste reduced by 26 tons per month with waste segregation education and additional recycling sorting assistance; and $53,075 savings and reduction in 717 metric tons of CO2 equivalents per year with automated lighting linked to OR occupancy [60].
Zuegge et al. educated anesthesia providers on volatile agent choices and flow rates, decreasing emissions by 64% (in terms of CO2eq). This was driven by decreased use of desflurane, with associated cost savings of $25,000/month [61]. Benness et al. designed a series of educational interventions to decrease use of desflurane, which accounted for 80% of the volatile carbon footprint in their department. Their education interventions resulted in a 58% reduction in the use of desflurane over the course of 9 months, which equated to > $46,000 in cost savings and avoidance of 360 ton CO2eq [62]. Wyssusek et al. implemented several educational interventions regarding inhaled anesthetics and reduced combined sevoflurane and desflurane usage costs and emissions by 58.33% and 87.88%, respectively, over the 6 years following implementation [63]. Furthermore, Davies et al. provided education on anesthetic gas selection to an Australasian network focused on sustainable anesthesia practices through an initiative titled Operation Clean Up. This reduced the volume of desflurane used from 1.85L/100 cases to 0.97L/100 cases, with use still reduced from baseline a year later (1.42L/100 cases) [64].
Education initiatives were also coupled with changes in anesthesia machines or incorporating software to promote low flow rates. Alexander and colleagues looked at the environmental impact of volatile anesthetics after implementation of modern, low-flow anesthetic machines that regulate expired end tidal gas concentrations and adjust flow rates. From 2012 to 2016, they found a difference in CO2eq of 8.9 million kg, representing a 66% reduction in GHG emissions and a total volume of volatile anesthetic use from 1703L to 1173L [65]. Similarly, Boyle et al. purchased machines with a lower gas flow rate and educated staff on environmental harm from volatile anesthetics, particularly desflurane. They noted a total volatile spend of €30,943 which equated to a 52% cost saving as well as an 81% reduction in CO2eq from 394,126 to 74,004 kg [66]. Carter et al. sought to implement the use of low flow anesthesia and encourage the use of cheaper and environmentally conscious gases like isoflurane. They reported a 25% decrease in total expenditure of volatile agents despite an increase in operating room activity [67]. Glenski and Levine implemented low-flow software on anesthesia machines and education initiatives, achieving 20% decrease in sevoflurane use per month [68].
Reuse
Waste: The use of reusable rather than disposable instruments has been well-studied. Gough and colleagues evaluated surgical instrument waste in laparoscopic cholecystectomy, finding that reusable scissors, clip appliers, and ports would save 10.7 kg CO2eq per case compared to single-use versions [69]. Similarly, Adler et al. compared waste production from disposable trocars, scissors, and Veress cannula to reusable instruments in laparoscopic cholecystectomy. Single-use instruments generated 1.16 kg household waste, 0.56 kg cardboard waste, and 1.47 kg plastic waste per case [70]. Boberg’s LCA showed a median difference of 446 kg CO2eq, 79 potentially disappeared fraction of species in the same area per year (PDF*m2*year), 2.4 × 10–4 DALYs, and 5160 MJ resource consumption with disposable relative to reusable trocars per laparoscopic cholecystectomy [71]. Similarly, Rizan et al. found environmental superiority of reusable instruments in laparoscopic cholecystectomy [72]. Elsewhere, authors have reported a 56% reduction in expenditure on laparoscopic cholecystectomy using reprocessed trocars, dissectors, curved scissors, jaws, graspers, hooks, and clips [73], as reprocessed devices have not been found to have an increased defect rate compared to original equipment manufacturer devices [74].
Burguburu's LCA identified significant environmental benefits for reusable rather than disposable scrubs, with a 31% lower carbon footprint over a four-year usage period [75]. Reusable surgical gowns offer substantial reductions in natural resource energy consumption (64%), GHG emissions (66%), water usage (83%), and solid waste (84%), assuming a 60-cycle reuse potential [76]. Additionally, reusable surgical basins, gowns, and covers reduced medical waste by 65% in two U.S. medical centers, achieving cost savings of $12.600–$14.000 per hospital [77]. Dettenkofer's comparative analysis between disposable (pulp/PE) and mixed (cotton/synthetic) surgical drapes demonstrated a 5.4 kg lower CO2eq, 87.1 MJ lower resource consumption, 72 g lower waste production, and 696 kg lower water consumption associated with the utilization of disposable drapes [78].
Rizan et al. compared carbon and financial costs associated with different modeled scenarios for decontamination and packaging of surgical instruments. Instruments were wrapped individually in flexible pouches, or prepared as surgical sets housed in single-use tray wraps or reusable rigid containers. This resulted in a carbon footprint of 77gCO2eq (€1.05) per instrument housed in aluminum containers, 66gCO2eq (€1.07) per instrument in tray wrap, and 189gCO2eq (€7.35) per individually wrapped instrument. Additionally, incineration of waste increased the carbon footprint of single-use packaging by 33–55%, while this was reduced by up to 10% with appropriate recycling [79]. Other instruments such as the LigaSure have been reprocessed to reduce costs by 55.5% in laparoscopic colectomy [80]. Scissors have been studied, as repairing 17-cm straight Mayo reusable scissors after 40 uses rather than replacing them decreases CO2eq emissions by 19% per use and reduces costs from £1.43 to £0.97 [20]. Ibbotson's LCA found that disposable stainless-steel scissors have a 40% higher CO2eq impact than plastic versions and a 94% higher impact than reusable stainless-steel scissors, advocating for a 44% cost reduction with reusable options [81]. McGain et al. performed a LCA and found that disposable drug trays in anesthesia cost twice as much, produced 15% more CO2 and consumed three times the amount of water compared to reusable trays [82].
Recycle
Waste: Amariglio et al. examined elective surgical cases at their institution over one year and identified that 57% of waste was inappropriately discarded, and that 71% of this waste could have been recycled [83]. McKendrick et al. audited the introduction of recycling of paper and cardboard in the theater preparation room and anesthetic room in 20 cases, diverting 54 kg of recycled bags and saving 25 kg CO2.[84] Conversely, Wyssusek and colleagues measured the volume of plastic accumulated across 22 ORs, estimating an annual saving of 1,700 kg of recyclable plastic [85].
Efforts have been made to mitigate surgical waste in the OR. In 1992, Tieszen and colleagues surmised that reusable linen products and recycling methods could reduce the weight of surgical waste by 73% [86]. One initiative aimed to reduce plastic waste and recycle theater equipment such as oxygen masks and tubing, advertised the recycling program, and created a dedicated PVC disposal pathway for staff porters over three months. This improved the weight of plastic recycling from operating rooms by 300% [87]. Elsewhere, Martin and colleagues used a systematic approach to improve waste sorting over two weeks, decreasing the weight of solid waste and regulated medical waste by 12% and 59% per OR per day, respectively [88]. Subsequently, Martin et al. used a multi-prong approach to improve waste sorting in the OR and decrease subsequent CO2eq emissions over one year. This consisted of educating staff on the importance of sorting infectious versus non-infectious waste, identifying reusable waste, and reorganizing operating rooms to facilitate waste sorting [89].
Sadler et al. introduced reusable metal recycling containers for single-use metal items, collecting 0.14 tons of metal over six weeks, which extrapolated to an annual collection of 1.18 tons [90]. Van Straten et al. examined waste from discarded reusable and disposable stainless-steel instruments in operating rooms across three hospitals by segregating repairable instruments. A total of 1.380 kg of instrument waste was collected, with 237 kg suitable for refurbishment, resulting in cost savings of €38.868 [91, 92]. Dohmen et al. recycled 239 kg of commonly used disposable surgical instruments over six months instead of incinerating them, achieving a reduction of 545 kg CO2eq [92]. Rouviere’s LCA targeted sterile medical devices in the OR through 13 actions: seven concerned waste reduction, five focused on waste sorting, and one addressed eco-responsible purchasing of equipment. This reduced 203 tons CO2eq emissions and saved 552 m3 of water [93].
Anesthesia: McGain et al. conducted a waste audit of OR waste in six operating theaters for five days and found that 66/90 kg of anesthetic waste was non-infectious, and that 58% of this was recyclable [94]. This is higher than a waste audit conducted by Nesaratnam et al. over 1 month with 20 full OR days or 121 cases. Their team found a total of 413 kg of anesthetic waste, of which 136 kg (33%) was recyclable while 277 kg was infectious and or nonrecyclable [95]. Connolly et al. also conducted a waste audit, but with the focus of quantifying volume of glass. Since glass can be recycled, this offers a way to reduce sharps waste which are not recycled into new materials and is more expensive ($0.95/kg sharps vs $0.33/kg glass). Over a one-week period, they found 15.8 kg of glass was able to be recycled [96].
Livingston et al. piloted recycling in several operating rooms by using different bags before patients entered the room and the possibility of contamination occurred. Over one week, this diverted 505.5 kg of waste from the landfill, translating to 25 tons per year. Other researchers have instead focused on reducing infectious regulated medical waste—a more costly and more energy intensive waste stream than general trash [97]. Fraifeld et al. provided education on waste separation in the OR, clarifying which items need to be disposed of via regulated medical waste containers. This decreased the volume of regulated medical waste from 0.33 kg/case to 0.09 kg/case, with a cost savings of $28,392 for their 35 operating rooms over the course of a year [98]. Hubbard et al. discarded anesthetic waste in standard waste bins before patient entry in the operating room, yielding a potential annual reduction of 13,800 kg of regulated medical waste and a cost savings of $2200 in their institution [99].
Education/sustainability programs: There is a growing trend toward implementing team-based strategies to improve quality and sustainability in surgical practice. Wyssusek et al. used a systematic approach to improve waste sorting in the operating room by educating the OR staff and forming a project team with key stakeholders including nursing, anesthesia, OR assistants, directors, and supervisors of perioperative services. The staff was educated regularly, advertisements for appropriate waste sorting were made, waste management change champions were identified to support clinicians in daily practice, and waste segregation and waste recycling programs were implemented over several years. This reduced 60% of unnecessary waste costs, reduced clinical OR waste by 82%, and reduced total OR waste by more than 50% [100]. Wormer and colleagues formed a Green Operating Room Committee including members from corporate leadership, nursing, anesthesia, and OR staff. Their multi-pronged initiative diverted 6.5 tons of medical waste. Recycling all single-use devices reduce annual solid waste by 5,833.2 kg, implementing reusable gel pads rather than disposable OR foam padding saved greater than $50,000 annually, turning off all anesthesia equipment and OR lights when not in use saved $33,000 and 234.3 metric tons of CO2 emissions annually, and finally, they showed that converting to alcohol-based scrub would save 2.7 million L of water annually [101].
Discussion
This scoping review was conducted by the EAES/SAGES joint SSP Taskforce in an effort to establish standard sustainability terminology, consolidate evidence-based outcome measures, define the scope of sustainable action in gastrointestinal surgical practice and assess the impact of prior sustainability initiatives.
We noted significant heterogeneity in study design and outcome measures across included studies. Most studies were prospective cohort studies while a minority were LCA studies. Yet, LCA studies are the gold standard in sustainability research [102]. While LCA studies provide the most comprehensive review of the overall environmental footprint, they are time and resource-intensive which limits wider use [19]. It may be more feasible to measure climate impact using non-LCA studies with a select but important group of outcomes including resource utilization such as the consumption of energy or water associated with a particular product, process, or service; or via economic analysis of the cost associated with implementing a sustainable initiative or solution (Fig. 5). Non-LCA studies evaluating climate impact or resource use may apply the 10R model of circular economy which provides a structured and practical framework for classifying and measuring the environmental impact of sustainable interventions. The 10R model was endorsed by our SSP Taskforce as a reporting framework for evaluating sustainable initiatives in surgical practice.
Fig. 5.
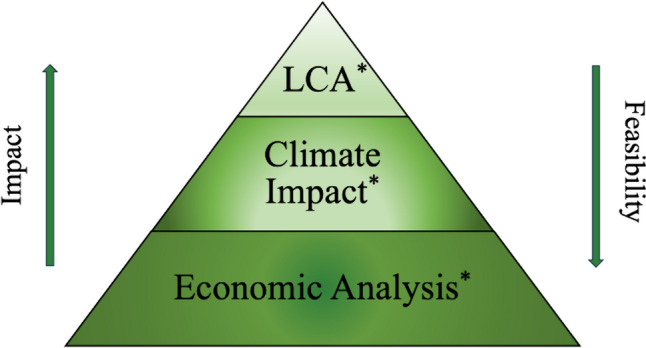
Hierarchy of evidence for sustainability research in surgery
Surgical waste production was identified as a major contributor to the environmental footprint of surgical practice. Implementation of a recycling program and education of staff members across operating rooms were among the most impactful interventions in reducing the carbon footprint from surgical practices. The use of leaner equipment kits and reusable surgical instruments also substantially reduced climate impact and associated OR costs. Simple and low-cost initiatives reduce water consumption, including the judicious use of water while scrubbing or the use of alcohol-based scrubs. Importantly, mitigating the use of anesthetic gases, particularly desflurane, also had among the greatest reported improvement in carbon footprint. These represent key areas for institutions to target in their effort to implement sustainability measures in the OR, particularly in gastrointestinal surgery. The importance of establishing a green team with local institutional and division champions was identified as an essential step in supporting the long-term success of a sustainability program [100, 103].
This scoping review has limitations. The broad heterogeneity in study populations, methodology, outcome measures, and data reporting precluded any quantitative synthesis of the comparative effectiveness of interventions on surgical climate impact. Additionally, sustainability expertise from other disciplines such as environmental science and civil engineering were not captured, though these were outside the scope of this review. Some articles are likely not captured despite the comprehensive search applied, due to the variability in aims, methodology, and outcome measures employed across surgical sustainability research. Studies may not have been captured outside of the English, French, German, or Dutch language. Finally, the complex interplay between outcome measures and the permitted degree of flexibility or tailoring of the interventions may limit their evaluation; for instance, the climate impact of equipment used in MIS must be balanced against the indirect positive impact from reduced complications and shorter length of stay. Still, the evidence for sustainability in surgical practice demonstrates the necessity of education, collaboration, and action among the stakeholders in surgical practice.
Conclusion
This scoping review established standard terminology, outcome measures, and scope across surgical sustainability studies while identifying the most impactful initiatives to reduce the climate impact of surgical practice. The use of standard terminology and SSP outcome measures, will facilitate the interpretation and aggregation of data on the environmental impact of surgical care. Multidisciplinary perioperative team education and collaborations will be required to deploy effective and sustainable initiatives with meaningful impact on reducing the environmental footprint of surgical practice.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The authors would like to acknowledge the contribution of SAGES and EAES members for their contribution in the design and planning of this joint initiative.
Funding
This initiative received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Declarations
Disclosures
Patricia Sylla is a consultant for Ethicon, Safeheal, Tissium, and Stryker. Nader Francis has consulted for Medtronic, Olympus, Applied Medical, Pharmacosmos and Fisher & Paykel Healthcare. Robert Lim is a consultant for Up-to-date. Shaneeta Johnson is a consultant for Baxter and Intuitive Surgical. Yewande Alimi is a consultant for Medtronic. Sheetal Nijihawan is a consultant for Smart SurgN. Benjamin Miller has research funding from the American Hernia Society. Drs. Bright Huo, M.M.M. Eussen, Stefania Marconi, Wendelyn M. Oslock, Nana Marfo, Oleksii Potapov, Ricardo J. Bello, Jonathan Vandeberg, Ryan P. Hall, Adnan Alseidi, Manuel Sanchez-Casalongue, Andrea Pietrabissa, Alberto Arezzo, Maximos Frountzas, Vittoria Bellatot, Paul Barach, Miran Rems, Sheetal Nijihhawan, Tejas S. Sathe, Benjamin Miller, Sarah Samreen, Jimmy Chung, and N.D. Bouvy have no conflicts of interest to disclose.
Ethical approval
Not applicable.
Patient consent
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Costello A, Abbas M, Allen A, Ball S, Bell S, Bellamy R, Friel S, Groce N, Johnson A, Kett M, Lee M, Levy C, Maslin M, McCoy D, McGuire B, Montgomery H, Napier D, Pagel C, Patel J, de Oliveira JAP, Redclift N, Rees H, Rogger D, Scott J, Stephenson J, Twigg J, Wolff J, Patterson C (2009) Managing the health effects of climate change. Lancet and University College London Institute for Global Health Commission. The Lancet 373:1693–1733 [DOI] [PubMed] [Google Scholar]
- 2.Rocque RJ, Beaudoin C, Ndjaboue R, Cameron L, Poirier-Bergeron L, Poulin-Rheault RA, Fallon C, Tricco AC, Witteman HO (2021) Health effects of climate change: an overview of systematic reviews. BMJ Open. 10.1136/bmjopen-2020-046333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kwakye G, Brat GA, Makary MA (2011) Green Surgical Practices for Health Care [DOI] [PubMed]
- 4.Eckelman MJ, Sherman J (2016) Environmental impacts of the US health care system and effects on public health. PLoS ONE. 10.1371/journal.pone.0157014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shoham MA, Baker NM, Peterson ME, Fox P (2022) The environmental impact of surgery: a systematic review. Surgery (United States) 172:897–905. 10.1016/j.surg.2022.04.010 [DOI] [PubMed] [Google Scholar]
- 6.MacNeill AJ, Lillywhite R, Brown CJ (2017) The impact of surgery on global climate: a carbon footprinting study of operating theatres in three health systems. Lancet Planet Health 1:e360–e367. 10.1016/S2542-5196(17)30162-6 [DOI] [PubMed] [Google Scholar]
- 7.Adisa A, Bahrami-Hessari M, Bhangu A, George C, Ghosh D, Glasbey J, Haque P, Ingabire JCA, Kamarajah SK, Kudrna L, Ledda V, Li E, Lillywhite R, Mittal R, Nepogodiev D, Ntirenganya F, Picciochi M, Simões JFF, Booth L, Elliot R, Kennerton AS, Pettigrove KL, Pinney L, Richard H, Tottman R, Wheatstone P, Wolfenden JWD, Smith A, Sayed AE, Goswami AG, Malik A, Mclean AL, Hassan A, Nazimi AJ, Aladna A, Abdelgawad A, Saed A, Abdelmageed A, Ghannam A, Mahmoud A, Alvi A, Ismail A, Adesunkanmi A, Ebrahim A, Al-Mallah A, Alqallaf A, Durrani A, Gabr A, Kirfi AM, Altaf A, Almutairi A, Sabbagh AJ, Ajiya A, Haddud A, Alnsour AAM, Singh A, Mittal A, Semple A, Adeniran A, Negussie A, Oladimeji A, Muhammad AB, Yassin A, Gungor A, Tarsitano A, Soibiharry A, Dyas A, Frankel A, Peckham-Cooper A, Truss A, Issaka A, Ads AM, Aderogba AA, Adeyeye A, Ademuyiwa A, Sleem A, Papa A, Cordova A, Appiah-Kubi A, Meead A, Nacion AJD, Michael A, Forneris AA, Duro A, Gonzalez AR, Altouny A, Ghazal A, Khalifa A, Ozair A, Quzli A, Haddad A, Othman AF, Yahaya AS, Elsherbiny A, Nazer A, Tarek A, Abu-Zaid A, Al-Nusairi A, Azab A, Elagili A, Elkazaz A, Kedwany A, Nuhu AM, Sakr A, Shehta A, Shirazi A, Mohamed AMI, Sherif AE, Awad AK, Abbas AM, Abdelrahman AS, Ammar AS, Azzam AY, Ciftci AB, Dural AC, Sanli AN, Rahy-Martín AC, Tantri AR, Khan A, Al-Touny A, Tariq A, Gmati A, Costas-Chavarri A, Auerkari A, Landaluce-Olavarria A, Puri A, Radhakrishnan A, Ubom AE, Pradhan A, Turna A, Adepiti A, Kuriyama A, Kassam A-F, Hassouneh A, El-Hussuna A, Habeebullah A, Ads AM, Mousli A, Biloslavo A, Hoang A, Kirk A, Santini A, Melero AV, Calvache AJN, Baduell A, Chan A, Abrate A, Balduzzi A, Sánchez AC, Navarrete-Peón A, Porcu A, Brolese A, Barranquero AG, Saibene AM, Adam AA, Vagge A, Maquilón AJ, Leon-Andrino A, Sekulić A, Trifunovski A, Mako A, Bedada AG, Broglia A, Coppola A, Giani A, Grandi A, Iacomino A, Moro A, D’amico A, Malagnino A, Tang A, Doyle A, Alfieri A, Haynes A, Wilkins A, Baldwin A, Heriot A, Laird A, Lazarides A, O’connor A, Trulson A, Rokohl AC, Caziuc A, Triantafyllou A, Anesi A, Nikova A, Andrianakis A, Charalabopoulos A, Tsolakidis A, Chirca A, Arnaud AP, Narvaez-Rojas AR, Kavalakat A, Spina A, Recordare A, Annicchiarico A, Conti A, Mohammed AD, Kocataş A, Almhimid A, Arnaout A, Fahmy A, Mangi A, Modabber A, Ulas AB, Mohamedahmed AYY, Frontali A, Moynihan A, Yunus A, Ahmad A, Kent AJ, Khamees A, Ugwu AO, Turan A, Mohammed AAK, Navarro-Barrios A, Yebes A, De Sousa ÁFL, Moreno A, Sethi A, Dawson AC, Othman AAA, Kaur A, Wolde A, Antonelli A, Scifo A, Alhamad A, Davis A, Alderazi A, Harky A, Mohammed-Durosinlorun A, Seguya A, Okhakhu A, Chamakhi A, Sebai A, Souadka A, Asla A, Agrawal A, Persad A, Gupta A, Elgazar A, Kulkarni A, Coates A, Bellés AC, Hadzibegovic AD, Jotic A, Kowark A, Martins A, Pineda AM, Peral A, Gollarte AS, Senent-Boza A, Camarena AIA, Castaño-Leon AM, Bravo AMM, Moro AMG, Musina A-M, Tapia-Herrero A-M, Kothari A, Gupta A, Raja A, Aljaiuossi A, Taha A, Majbar AM, Prodromidou A, Kanatas A, Gupte A, Zakaria AD, Balla A, Barberis A, Bondurri A, Bottari A, Costantino A, Figus A, Lauretta A, Mingoli A, Romanzi A, Sagnotta A, Scacchi A, Picchetto A, Valadez AEC, Luzzi A-P, Älgå A, Fontalis A, Hecker A, Demetriades AK, Serban A-M, Văcărașu AB, Cokan A, Isaza-Restrepo A, Beamish A, Schache A, Stevenson A, Yiu A, Cockbain AJ, Litvin A, Abad-Motos A, Becerra A, Ramos ÁC, Chiaradia A, Dell A, Romano A, Pascale A, Marra AA, Dimas A, Kolias A, Cerovac A, Koneru A, Tidjane A, Agbeko AE, Bajaj A, Gosain A, Allan A, Carreras-Castañer A, D’amore A, Dare A, Maffioli A, Palepa A, Paspala A, Konney A, Gatta AN Della, Ezanno A-C, Yiallourou A, Kinnair A, Rayner A, Scafa AK, Bowan AB, Veglia A, Russo A, Maniaci A, Castaldi A, Gil-Moreno A, Maffuz-Aziz A, Meola A, Nenna A, Ferrer AP, Bonilla AR, Ramos-De La Medina A, Infante AR, Santoro A, Laganà AS, Bateman A, Michael ALR, Abozid A, Seidu AS, Lowery A, Tantraworasin A, Rasheed A, Picciariello A, Isik A, Saif A, Anjum A, Ioannidis A, Abeldaño A, Hussain A, Nathan A, Bedzhanyan A, Perfecto A, De Virgilio A, Galvan A, Sablotzki A, Böttcher A, Pellacani A, Gatti A, Ibrahimli A, Menon A, Sahni A, Mwenda AS, Choudhry A, Jayawardane A, Gupta A, Ramasamy A, Mitul AR, Bawa A, Nugur A, Rammohan A, Sachdeva A, Mehraj A, Yildirim A, Alqaseer A, Radwan A, Sallam A, Syllaios A, Tampakis A, Alwael A, Samara A, Eroglu A, Rahman A, Ulkucu A, Zaránd A, Dulskas A, Tawiah A, Zani A, Vas A, Lukosiute-Urboniene A, Adamu A, Aujayeb A, Malik AA, İplikçi A, Mahmud A, Cil AP, Makanjuola A, Akwaisah A, Galandarova A, Saracoglu A, Regan A, Barlas AM, Alhassan BA Bin, Mostafa B, Hamida B Ben, Torun BC, Abdullah B, Balagobi B, Banky B, Singh B, Alegbeleye B, Yigit B, Hajjaj BN, Burgos-Blasco B, Seeliger B, Alayande B, Alhazmi B, Enodien B, Torre B, Pérez BG, Tamayo BV, De Andrés-Asenjo B, Quintana-Villamandos B, Girgin B, Barmayehvar B, Beisenov B, Creavin B, Dunne B, Marson B, Waterson B, Martin B, Zucker B, Wong BNX, Ozmen BB, Hammond B, Mbwele B, Núñez B, Dhondt B, Gafsi B, Mcleish B, Lieske B, Tailor B, La Pira B, Picardi B, Zampogna B, Casagranda B, Festa BM, Panda B, Kirmani B, Sulaiman B, Gurung B, Zacharia B, Bette B, Ayana B, Nikolovska B, Vilaró BC, De Vega Sánchez B, Hameed BZ, Diaconescu B, Kovacevic B, Bumber B, Sakakushev B, Tadic B, Malek B, Alrayes B, Thomas B, Gális B, Gallagher B, Knowles B, Cunningham B, Daley B, Mishra B, Ashford B, Pirozzi BM, Berselli B, Martinez-Leo B, Sensi B, Nardo B, Celik B, Giray B, Abud B, Almiqlash B, Pramesh CS, Taskiran C, De Campos Prado CA, Cipolla C, Kumar C, English C, Riccetti C, Vanni C, Brasset C, Downey C, Duffy C, Chwat C, Cutmore C, Sars C, Ratto C, Pacilio CA, De La Infiesta García C, Moreno CG, Magalhães C, Prada C, Zapata CS, Senni C, Flumignan CDQ, Martinez-Perez C, Duarte CL, Garcia CSR, Anderson C, Hing C, Cullinane C, Cina C, Zabkiewicz C, Sohrabi C, Guldogan CE, Ciubotaru C, Desai C, Raut C, Demetriou C, Handford C, Okpani C, Paranjape C, Koh C, Khatri C, Parmar C, Mok CW, Caricato C, Marafante C, Echieh CP, Tan CY, Ong CS, Conso C, Jardinez C, Konrads C, Warner C, Makwe CC, Henein C, Fleming C, Roland CL, Maurus C, Nitschke C, Mittermair C, Mallmann C, Andro C, Harmston C, Kuppler C, Lotz C, Nahm C, Rowe C, Ryalino C, Wallis C, Millward CP, Anthoulakis C, Apostolou C, Chouliaras C, Kalfountzos C, Kaselas C, Vosinakis C, Okereke C, Chean CS, Barlow C, Tatar C, Clancy C, Forde C, Sharpin C, Mccarthy C, Nestor C, Warden C, Ávila CC, Massaguer C, Fang CEH, Martins CP, Guerci C, Mauriello C, Holzmeister C, Miller C, Weber C, Wiesinger CG, Kenington C, Noel C, Sue-Chue-Lam C, Adumah C, Neary C, Sen C, Fitzgerald C, Ezeme C, Nastos C, Mesina C, Bombardini C, Torregrosa C, Valdespino CP, Don CP, Wickramasinghe D, Milanesi D, Armijos D, Asiimwe D, Beswick D, Clerc D, Cox D, Doherty D, Martínez DF, Lechuga DG, Gero D, Gil-Sala D, Lindegger D, Reim D, Shaerf D, Shmukler D, Branzan D, Filipescu D, Rega D, Bernardi D, Bissacco D, Fusario D, Morezzi D, Sabella D, Zimak DM, Vinci D, Sale D, Khan DZ, Thereska D, Andreotti D, Tartaglia D, Abdulai DR, Mukherjee D, Verdi D, Idowu D, John D, Johnson D, Moro-Valdezate D, Naumann D, Omar D, Proud D, Roberts D, Guzmán DS, Watson D, Bergkvist DJ, Lumenta DB, Ferrari D, Rizzo D, Degarege D, Castillo DFC, Douglas D, Wright D, Nanjiani D, Bratus D, Altun D, Sievers D, Vaysburg D, Katechia D, Ghosh D, Azize DA, Rodrigues D, Pachajoa DAP, Hayne D, Mutter D, Raimondo D, Eskinazi D, Sasia D, Corallino D, Muduly D, Grewal D, Hadzhiev D, Peristeri D, Pournaras D, Raptis DA, Angelou D, Haidopoulos D, Magouliotis D, Moris D, Schizas D, Symeonidis D, Tsironis D, Korkolis D, Tatsis D, Thekkinkattil D, Bulian DR, Pandey D, Vatansever D, Parker D, Wiedemann D, Borselle D, Pedini D, Schweitzer D, Venskutonis D, Otokwala J, Adamu KM, Pk P, Garod M, Ellafi AAD, Zivkovic D, Jelovac D, Wijeysundera D, Mcpherson D, Ryan É, Ugwu E, Baidoo EI, Shaddad E, Memişoğlu E, Naranjo EPL, Brodkin E, Segalini E, Viglietta E, Hendriks E, Bonci E-A, Sá-Marta E, Ortega EN, Gomez EG-L, Joviliano EE, Clune E, Horwell E, Mains E, Vasarhelyi E, Caruana EJ, Nevins EJ, Yenli EMT-A, Baili E, Lostoridis E, Morgan E, Shiban E, Latif E, Tampaki EC, Ezenwa E, Irune E, Borg E, Eisa E, Gialamas E, Parvez E, Theophilidou E, Toma EA, Arnaoutoglou E, Samadov E, Kantor E, Ulman EA, Colak E, Cassinotti E, Bannone E, Sarjanoja E, Yates E, Vincent E, Lun EWY, Cerovac E, Dif ES, Alkhalifa E, Daketsey E, Fayad EA, Sheikh E, Pontecorvi E, Cammarata E, La Corte E, Rausa E, Odai ED, Guasch E, Cano-Trigueros E, Uldry E, Ros EP, Matthews E, Donmez EE, Giorgakis E, Kapetanakis E, Stamatakis E, Bua E, Schneck E, Nachelleh EA, Ofori EO, Akin E, Gönüllü E, Kirkan EF, Çelik E, Wong E, Capozzi E, Pinotti E, Colás-Ruiz E, González E, Fekaj E, Ohazurike E, Kebede E, Erginöz E, Duran EES, Scott E, Aytac E, Albanese E, Castro EJ, Albayadi E, Kriem E, Siddig E, Otify E, El Tayeb EEABH, Hong EH, Saguil E, Belzile E, Tuyishime E, Panieri E, Martínez EG, Myriokefalitaki E, Wong EG, Samara E, Agbeno EK, Drozdov E, Tokidis E, Shah FA, Barra F, Carbone F, Ferreli F, Marino F, Martinelli F, D’acapito F, Masciello F, Bàmbina F, Issa F, Salameh F-T, Kethy F, Mahmood F, Gareb F, Idrees F, Karimian F, Ashraf F, Haji F, Inayat F, Begum F, Nabil F, Rosa F, Haider F, Parray F, Calculli F, Ferracci F, Saraceno F, Coppola F, Coccolini F, Fusini F, Migliorelli F, Pecoraro F, Alconchel F, Coimbra FJF, Trivik-Barrientos F, Naegele F, Almarshad F, Agresta F, Fleming F, Mendoza-Moreno F, Brzeszczyński F, Carannante F, Wu F, Aljanadi F, Hayati F, Campo F, Sorbi F, Milana F, Takeda FR, Shekleton F, Gessler F, Recker F, Grama F, Cherbanyk F, Faponle F, Angelis F, Calabretto F, Gaino F, Toia F, Bianco F, Bussu F, Cammarata F, Castagnini F, Colombo F, Ferrara F, Fleres F, Guerrera F, Litta F, Mongelli F, Pata F, Roscio F, Mulita F, Ardura F, Tejero-Pintor FJ, Calvo FJR, Escobedo FJB, Camacho FJB, Odicino F, Schmitt F, Bloemers F, Hölzle F, Gyamfi FE, Messner F, Koh F, Cáceres F, Smolle-Juettner F-M, Herman F, Ayeni F, Djedovic G, De Oliveira GP, Rodrigues G, Wagner G, Bellio G, Giarratano G, Capolupo GT, Budd G, Marom G, Poillucci G, Thiruchandran G, Nicholson G, Groot G, Hoey G, Bass GA, Sachdev G, Agarwal G, Aggarwal G, Cormio G, Mazzarella G, Perrone G, Osterhoff G, Singer G, Dejeu G, Fowler G, Garas G, Gradinariu G, Theodoropoulos G, Tzimas G, Babis G, Wong GKC, Cross GW V, Micha G, Chrysovitsiotis G, Koukoulis G, Peros G, Tsoulfas G, Kapetanios G, Karagiannidis G, Verras G-I, Ekwen G, Perrotta G, Petruzzi G, Bertelli G, Calini G, Fiacchini G, Pirola GM, Dolci G, Mendiola G, Baiocchi GL, Palini GM, Prucher GM, D’andrea G, Maggiore G, Cassese G, Franceschini G, Pellino G, Saponaro G, Pattacini GC, Pantuso G, Iannella G, Bonsaana GB, Lever G, Brachini G, Giraudo G, Lisi G, Russo GI, Aprea G, Pascale G, Tomasicchio G, Sandri GBL, Armatura G, Turri G, Zaccaria G, Barugola G, Lantone G, Gasparini G, Iacob G, Sozzi G, Zancana G, Mercante G, Bianco G, Brisinda G, Consorti G, Currò G, Giannaccare G, Palomba G, Pascarella G, Rotunno G, Spriano G, Vizzielli G, Cucinella G, Sica G, Campisi G, Baiocchi G, Guerra GR, Pacheco GMF, Atis G, Augustin G, Šantak G, Chauhan GS, Branagan G, Harris G, Stewart GD, Padmore G, Kocher GJ, Di Franco G, De Jesus Labrador Hernandez G, Christodoulidis G, Neal-Smith G, Yim G, Piozzi GN, Claret G, Yanowsky-Reyes G, Dhaity GD, Cakmak GK, Mohamed G, Kucuk GO, Ancans G, Banipal GS, De Bacco Marangon G, Laporte G, Martinez-Mier G, Recinos G, V GMM, Benshetrit G, Vijgen G, Pickett G, Rodriguez HA, Shiwani H, Derilo H, Awad H, El Assaad H, Raji HO, Hardgrave H, Karakullukcu HK, Abdussalam HO, Mustafa H, Parwaiz H, Khan H, Arbab H, Naga H, Salem H, Ulgur HS, Perez-Chrzanowska H, Greenlee H, Javanmard-Emamghissi H, Lederhuber H, Osman H, Adamou H, Majid HJ, Van Goor H, Spiers HVM, Manesh HF, Mushtaq H, Aljaaly H, Hasan H Ben, Ahmed HTA, Martinez-Said H, Aguado HJ, Consani H, Chaplin H, Mohan H, Van Vliet H, Lohse HAS, Shah H, Claireaux H, Lule H, Juara H, Abozied H, Bayo HL, Alibrahim H, Kroon HM, Ulman H, Khan H, Yonekura H, Abou-Taleb H, Wong HYF, Carpenter H, Majd HS, Zenha H, Mayer HF, Elghadban H, Abdou H, Elfeki H, Yusefi H, Gomez-Fernandez H, Horsfall HL, Meleiro H, Sungurtekin H, Junior HFL, Moloo H, Bayhan H, Şevi̇k H, Embarek H, Hamid HKS, Pradeep IHDS, Donkin I, Ateca IV, Jafarov I, Salisu I, Abdalaal I, Garzali IU, Sall I, Adebara I, Aghadi I, Ugwu I, Zapardiel I, Reis I, Nwafor I, Fakhradiyev I, Surya IU, Robo I, Njokanma I, Iannone I, Khan I, Correia I, Königsrainer I, Seiwerth I, Linero IB, Kadiri I, Florian I-A, Tzima I, Akrida I, Baloyiannis I, Gerogiannis I, Katsaros I, Tsakiridis I, Valioulis I, Negoi I, Yadev I, De Haro Jorge I, Vázquez IO, Dajti I, Russo IS, Afzal I, Wasserman I, Chukwu I, Gracia I, Oliver IM, Hughes I, Mondi I, Ncogoza I, Bsisu I, Rashid I, Balasubramanian I, Omar I, Dominguez-Rosado I, Smati I, Vokshi I, Al-Badawi IA, Saleh IA, Pilkington I, Kirac I, Trostchansky I, Gawron IM, Trebol J, Martellucci J, Andreuccetti J, Abou-Khalil J, Shah J, Manickavasagam J, De Alarcón JR, Mihanovic J, O’riordan J, Archer J, Ashcroft J, Blair J, Hamill J, Munthali J, Park J, Parry J, Ryan J, Tomlinson J, Wheeler J, Wilkins J, Balogun JA, Hodgetts JM, Vatish J, Žatecký J, Dziakova J, Martin J, Beatty JW, Stijns J, Faiz J, Ripollés-Melchor J, Mata J, Vásquez JAG, Mitra JK, Tuech JJ, Mvukiyehe JP, Fallah J-M, Díaz JT, Vishnoi JR, Van Den Eynde J, Rickard J, Rolinger J, Kaplowitz J, Meyer J, Reid J, Rossaak J, Smelt J, Thomas JJ, Reyes JAS, Davies J, Luc J, Alonso JAM, Hajiioannou J, Querney J, Van Acker J, Pu JJ, Cama J, Simoes J, Cozens J, Barbosa-Breda J, Ribeiro J, De Haro J, Nigh J, Bowen J, Pollok JM, Strotmann JJ, Doerner J, Edwards J, Green J, Massoud J, Mcgrath J, Squiers J, Street J, Windsor J, Santoshi JA, Meara JG, Abebrese JT, Reilly J-J, Zabaleta J, Phillips J, Herron J, Horsnell J, Dawson J, Sheen J, Kauppila JH, Konsten J, Raurich-Leandro J, Romera JS, Nuñez J, Gass J-M, Blanco J, Calvache JA, Iturralde JLF, Daddino JL, Hermosa JMG, Guillen JRO, Beristain-Hernandez J-L, Sole-Sedeno JM, Vives JMM, Attwood J, Furey J, Hadaya J, Mckay J, Meilak J, Natale J, Shalhoub J, Jung J, Arthur J, Kealey J, Wright J, Moreau J, Miskovic J, Juloski J, Bauset JCC, Segura-Sampedro JJ, Cisneros JRT, Gomez-Rosado J-C, Arneja J, Heider J, Fernández JD, Plata-Bello J, Villanueva J, Olaogun J, Hing JX, Košir JA, Daruwalla J, Yeung J, Wormald J, Seyi-Olajide J, Rani J, Wong KY, Hristova K, Kajal K, Algarni K, Theivendran K, Futaba K, Elsayem K, Kapur K, Bailey K, El-Boghdadly K, Ataya K, Lacorbiniere K, Shah K, Tellez KSM, Szyluk K, Rangasamy K, Iyengar K, Szabómihályová K, Atkinson K, Camargo-Parra K, Galliard K, Dickson K, Singh K, Qader K, Hasan K, Spellar K, Feeney K, Ajenifuja K, Oh KE, Okunade K, Adanu K, Bateman K, Saracoglu K, Ho KW, Enwerem K, Mishra K, Verhoeff K, Bensoltane K, Larabi K, Hamdan KH, Nadi K, Fozo K, Abdelwahab K, Al-Sayaghi K, Dajani K, Algahtany K, Abdel-Galil K, Ahmed K, Bajunaid K, Bhatti K, Sofi K, Abdulsalam K, Tamoos K, Dzhumabaev K, Samo KA, Purich K, Madhvani K, Qin KR, Underwood K, Senanayake KJ, Augestad KM, Sigamoney K, Apostolou K, Bouchagier K, Bouliaris K, Bramis K, Gousias K, Lasithiotakis K, Paraskevopoulos K, Perivoliotis K, Roditis K, Stamatis K, Stroumpoulis K, Paraskevas KI, Govindarajan KK, Šimko K, Olson KA, Khobragade K, Seah KM, Kishore K, Ayad K, Papavasiliou K, Angelou K, Paniagua LC, Czako L, Ching LVK, Rai L, Gupta L, Ismail L, Mbodi L, Dasanayake L, Schröder L, Baiyewu LA, Fortuna L, Fernandez LG, Vivancos LG, Jack L, Keçi L, Lavalle L, Leonard L, Shelmerdine L, Vaassen L, Hasan L, Lazarou L, Tzelves L, Matos L, Siragusa L, Licari L, Lima LS, Solaini L, Lichman L, Moral LT, Cabeza L, Kaplan L, Valeanu L, Kaman L, Karout L, Pieteris L, Chan L, Grüßer L, Zamora L, Catarzi L, Rampersad L, Anyanwu L-J, Cheung LK, Rodríguez LV, Andreani L, Cobianchi L, Petagna L, Howse L, Gonzalez LE, Bains L, Vohra L, Ansaloni L, Bertolaccini L, Ferrario L, Orecchia L, Tirloni L, Zanin L, Morelli L, Scaravilli L, Locatello LG, García LD, Vida L, Carbone L, Heindl LM, Bonavina L, Conti L, Marano L, Verre L, Conte LE, Boccalatte L, Tellez LG-S, Loureiro L, Sánchez-Guillén L, Tallon-Aguilar L, Nakano L, Alvarez-Lozada LA, Gonzalez LAS, Flórez LJG, Capitan-Morales L-C, Kowalski LP, Widmer LW, Harper L, Render L, Wheldon L, Abdur-Rahman L, Doğan L, Prusty L, Katsiaras L, Gourbault L, Siddiqui MT, Saleh M, Karthigeyan M, Rodriguez M, Chowdhury M, Nagappa M, Sultania M, Bashir M, Alam M, Elshahawy MAM, Elfiky M, Loubani M, Marei M, Mewafy M, Alali M, Nassar MA, Alobied M, Bilfaqirah M, Ahmad M, Rius M, Manangi M, Dornseifer MD, Tripathi M, S M, Sokolov M, Pigeolet M, Alonso MD, Losada M, Carretero MM, Tousidonis M, Cotovio MD, Wijeyaratne M, Boira MA, Franza M, Albdour M, Alkhatieb M, Déserts MD Des, Niewiera M, Vallve-Bernal M, Kavanagh MM, Migliore M, Calabrò M, Martino M Di, Reicher M, Baia M, Caricato M, Clementi M, De Zuanni M, Fiore M, Giacometti M, Inama M, Maestri M, Materazzo M, Sparavigna M, Pascale MM, Nemeth M, Serra M, Fahim MMF, Soucheiron MC, Papadoliopoulou M, Wittmann M, Sotiropoulou M, García-Conde M, Ranucci MC, Amo MDA Del, Boedo MJM, Velázquez MJM, Pissaridou MK, Petersen ML, Sacras ML, Modolo MM, Caubet MM, Di Nuzzo MM, Ntalouka MP, Menna MP, Aguilera-Arevalo M-L, Rela M, Capuano M, Hollyman M, Olivos M, Sacdalan MD, Raphael M-C, Takkenberg M, Bortul M, Cabrera M, Castaño M, D’oria M, Giuffrida M, Laborde MM, Rodriguez-Lopez M, Trejo-Avila M, Papa MV, Ghobrial M, Kryzauskas M, Anwer M, Cheetham M, Davies M, Higgins M, Siboe M, Tarle M, Velten M, Wurm M, Süleyman M, Bauer M, O’dwyer M, Caretto M, De La Rosa-Estadella M, Fragoso M, Serra ML, Merayo M, Golet MR, Martínez-Sánchez MI, Domingo MMA, Gosselink M, Batstone M, Reichert M, Salö M, Soljic M, Zambon M, Angeles MA, Abdulkhaleq M, Abdelkarim M, Alsefri M, Iwasaki M, Shiota M, Veroux M, Molina-Corbacho M, Frasson M, Serenari M, De Pastena M, Desio M, Risaliti M, Rottoli M, Bence M, Chan M, Watson M, Wiles M, Boisson M, Berselli M, Capobianco M, Di Bartolomeo M, Fehervari M, Pacilli M, Romano M, Zizzo M, Domanin M, Montuori M, Podda M, Zago M, Dzogbefia M, Frountzas M, Thaw MH, Al-Juaifari M, Gharat M, Mohamed M, Hannan MJ, Venketeswaran M, Chisthi M, Dessalegn M, Kaplan M, Çakıcı MÇ, Ulutaş ME, Hassan M, Elsadek M, Mengesha MG, Gómez ME, Elbadawy MA, Pitcher M, Tanal M, Tokocin M, Ergenç M, Çelik MN, Bareka M, Pekcici MR, Cappuccio M, Dasa M, Dewan M, El Boghdady M, Ezeanochie M, Greenhalgh M, Jenkinson M, Kelly M, Spartalis M, Zyskowski M, Racine M, De Cillia M, Chu MJJ, Mallmann MR, Zhu MZL, Klimovskij M, Vailas M, Kisielewski M, Adamina M, Campanelli M, Carvello M, Ammendola M, Manigrasso M, Scopelliti M, White M, Collins ML, Chevallay M, Borges MF, Mayo-Yáñez M, Melo MR, Ruiz-Marín M, Eiras MAF, Cunha MF, Pertea M, Slavchev M, Davidescu M, Prieto M, Agapov M, Gahwagi M, Prats MC, Rudic M, Verbic MS, Kostusiak M, Stoleriu MG, Lucas MA, Barone M, Ahmad M, Alemu MAA, Fatima M, Ida M, Sahu M, Muhaisen M, Salem M, Emara MM, Oludara M, Sotudeh M, Kassab MB, Abdelkhalek M, Alsori M, Anwar M, El-Kassas M, Elbahnasawy M, Eldabaa M, Rabie M, Hassanin MA, Thaha MA, Ali MSM, Alhamid M, Almoshantaf MB, Keramati MR, Bafaquh M, Abuzaid M, Al-Shehari M, Alharthi M, Alkahlan M, Alwash M, Alyousef M, Amir M, Basendowah M, Deputy M, Jibreel M, Alam MS, Alsharif M, Issahalq MD, Omer MEA, Abubakar MK, Draman MR, Elnour MAE, Eltayeb M, Castillo MN, Jawad M, Raut M, Ghalleb M, Katsura M, Lebe M, Abbas M, Abdelrahman M, Shalaby M, Farhan-Alanie M, Farooq M, Musadaq M, Arshad M, Anjum MA, Usman M, Chaudhary MA, Raza MA, Karim MFSA, Chaudhary MH, Janjua MH, Khokhar MI, Malik MIK, Pirzada MT, Younis MU, Elhadi M, Suer MS, Ergenç M, Binnawara M, Emmanuel M, Abbasi M, Naimzada MD, Kulimbet M, Kusunoki M, Eugene M, Chauhan M, Shokor MA, Aljiffry M, Kalın M, Kurawa M, Dincer MB, Tolani MA, Soytas M, Yakubu M, Usman MI, Aremu M, Paranyak M, Talat N, Kausar N, Dudi-Venkata N, Bazzi N, Hasan N Ben, Van Wyk NN, Shaban N, Almgla N, Kandevani NY, Alzerwi N, Alvarez N, Motas N, Rincón NAR, Blencowe N, Simon N, Aghtarafi N, Ghuman NK, Sharma N, Wijekoon N, Kumar N, Hassan N, Onyemaechi N, Prijović N, Özçay N, Goel N, Segaren N, Sharma N, Kalyva N, Palacios NM, Alonso NFP, Onyeagwara N, Petrucciani N, Daddi N, Lightfoot N, Power N, Segaren N, Starr N, Dreger NM, Cillara N, Colucci N, Eardley N, Tartaglia N, Zanini N, Bacalbasa N, Campuzano N, Mouawad N, Federico NSP, Tamini N, Mariani NM, Beasley N, Adu-Aryee NA, Burlov N, Dimitrokallis N, Gouvas N, Machairas N, Memos N, Thomakos N, Tsakiridis N, Schizas N, Börner N, Theochari N, Al-Saadi N, Glass N, Horesh N, R NE, Gahlot N, Ismail N, Aljirdabi N, Maria NUH, Trabulsi N, Akeel N, Borges N, Moda N, Redondo NV, Nyarko OO, Ginghina O, Enciu O, Okere O, Ekwunife OH, Quadri O, Ogundoyin O, Tucker O, Mateo-Sierra O, Azzis O, Ojewuyi O, Habeeb O, Idowu O, Elebute O, Agboola O, Ladipo-Ajayi O, Oyinloye O, Adebola O, Ekor O, Ogundoyin O, Salamanca O, Vergara-Fernandez O, Wafi O, Aladawi O, Bahassan OM, Tammo Ö, Ozkan OF, Williams OM, Salami O, Akinajo O, Sakhov O, Gallo O, Sole OM, Milella O, Alser O, Bettar O Al, Alomar O, Osman OS, Aisuodionoe-Shadrach O, Basnayake O, Bozbiyik O, Hodges O, Ojo O, Yanık Ö, Mutlu ÖPZ, Kazan O, Calavia P, García PR, Urriza PV, Lopez PR, Christidis P, Dorovinis P, Kokoropoulos P, Mourmouris P, Papatheodorou P, Garg PK, Patel P, Vassiliu P, Campennì P, De Nardi P, Bernante P, Ubiali P, Baroffio P, Pizzini P, Sapienza P, Myrelid P, Chatzikomnitsa P, Tsiantoula P, Gada P, Avella P, Cianci P, Romero P, Méndez PS, Pazmiño PAF, Coughlin P, Kirchweger P, Pessaux P, Maguire PJ, Petrone P, Cullis P, Köglberger P, Marriott P, Nankivell P, Santos-Costa P, Martins PN, Panahi P, Botelho P, Teixeira P, Escobar P, Vázquez PJG, Gribnev P, Nolte P, Agbonrofo P, Bobak P, Choong P, Elbe P, Hutchinson P, Labib P, Paal P, Pockney P, Reemst P, Szatmary P, Vaughan-Shaw PG, Alexander P, Pucher P, Stather P, Foessleitner P, Winnand P, Zehnder P, Kruse P, Matos PAW, Lapolla P, Cicerchia PM, Solli P, Di Lascio P, Zarif P, Champagne P-O, Anoldo P, Bertoglio P, Fransvea P, Familiari P, Lombardi PM, Stogowski PT, Bruzzaniti P, Tripathi P, D’sa P, Salunke P, Shah PA, Punjabi PPP, Christodoulou P, Hamdan Q, Tawalbeh R, Gadelkareem R, Awad R, Callcut R, Clegg R, Choron R, Payne R, Gefen R, Costea R, Drasovean R, Mirica RM, Ravindra R, Fajardo RT, Nunes RL, Aspide R, Lombardi R, Vidya R, Elboraei R, Saaid R, Ghodke R, Gupta R, Sharma RD, Lunevicius R, Kalayarasan R, Mohan R, Singh R, Sivaprakasam R, Seenivasagam RK, Rajendram R, Radulescu RB, Goicea R, Seshadri RA, Sarı R, Nataraja R, Aslam R, Abdelemam R, Shrestha R, Bharathan R, Pellini R, Guevara R, Agarwal R, Vissapragada R, Alharmi RA, Sayyed R, Browning R, Critchley R, Mallick R, Alarabi R, Beron RI, Függer R, Othman R, Saad R, Amores RR, Colombari RC, Radivojević RC, Patrone R, Novysedlák R, Huatuco RMP, Baertschiger R, Liang R, Luckwell R, Escrevente R, Rezende RF, Cruz RP, Lenzi R, Rosati R, Donovan R, Egan R, Morris R, Page R, Seglenieks R, Unsworth R, Wilkin R, Skipworth RJ, Davies RJ, Bezirci R, Talwar R, Azami R, Bohmer R, Crichton R, Fruscio R, Hooker R, Jach R, Parker R, Pillerstorff R, Sinnerton R, Stabler R, O’connell RM, Ragozzino R, Tutino R, Angelico R, Cammarata R, Colasanti R, Macchiavello R, Peltrini R, Pirrello R, Vaschetti R, Pires RE, Papalia R, Arrangoiz R, Hompes R, Mittal R, Salah R, Pinto R, Flumignan R, Callan R, Cuthbert R, Dennis R, Scaramuzzo R, Macías RM, Sánchez R, Ogu R, Ramely R, Sgarzani R, Ramli R, Hillier R, Thumbadoo R, Ooi R, Abdus-Salam R, Masri R, Hodgson R, Mathew R, Wade R, D’archi S, Khan S, Ngaserin S, Kale S, Hassan S, Merghani S, Benamar S, Muhammad S, Badran S, Elsahli S, Heta S, Hammouche S, Baeesa S, Paiella S, Eldeen STEHT, Arkani S, Mittal S, Hirji S, Tebha S, Emile S, Dbouk S, Bandyopadhyay SK, Muhammad S, Olori S, Asirifi SA, Hailu S, Ling S, Newman S, Ross S, Wanjara S, Kumar S, Seneviratne S, Tamburello S, Suarez SB, Ingallinella S, Irshaidat S, Konswa S, Mambrilla S, Nasser S, Parini S, Pitoni S, Ornaghi S, Rodrigues SC, Abdelmohsen S, Aitken S, Tian S, Badiani S, Ahmad S, Swed S, Muthu S, Lakpriya S, Alzahrani S, Mikalauskas S, Lasrado S, Satoskar S, Bawa S, Altiner S, Garcia S, Stevens S, Demir S, Ken-Amoah S, Tranca S, Ziemann S, Awad S, Atici SD, Subramaniam S, Erel S, Jiang S, Efetov S, Efremov S, Katorkin S, Valladares SC, Contreras SM, Meriç S, Zenger S, Safi S, Leventoğlu S, Elsalhawy S, Shaikh S, Sheik S, Islam S, Shamim S, Waqar SH, Ahmad S, Farid S, Seraj SS, Sundarraju S, Karandikar S, Sambhwani S, Chopra S, Chowdhury S, Laura S, Ahmed S, Wason S, Tan SJH, Fraser S, Williams S, Ghozy S, Abdelmawgoud S, Shehata S, Sharma S, Ahmed S, Al-Touny SA, Ramzanali S, Nah SA, Jansen S, Rajan S, Dindyal S, Amin S, Ahmad S, Shoukrie SIM, Karar S, Patkar S, Abdulsalam S, Lin S, Hegde S, Fiorelli S, Quaresima S, Redondo SV, Palmisano S, Ruggiero S, Balogun S, Cais S, Cole S, Federer S, Le Roux S, Ippoliti S, Meneghini S, Viola S, Manfredelli S, Novello S, Gananadha S, Mesli SN, Kale S, Tani SI, Malik S, Anastasiadou S, Boligo S, Esposito S, Valanci S, Xenaki S, Pejkova S, Bandyopadhyay S, Trungu S, Basu S, Alkhatib S, Pérez-Bertólez S, Flores SL, Donoghue S, Lunca S, Orsoo S, Potamianos S, Devarakonda S, Suresh S, Croghan SM, Turi S, Capella S, Lucchini S, Magnone S, Salizzoni S, Scabini S, Scaringi S, Cioffi SPB, Seyfried S, Degener S, Potten S, Taha-Mehlitz S, Ali S, Angamuthu S, Mcaleer S, Knight SR, White S, Mantziari S, Kykalos S, Goh SK, Chowdhury SP, Ibrahim S, Elzwai S, Bansal S, Tripathy S, Amrayev S, Anwar SL, Banerjee S, Thakar S, Saeed S, Venkatappa SK, Das S, Techapongsatorn S, Dube SK, Lee S, González-Suárez S, Henriques S, Konjevoda S, Gisbertz S, Bravo SL, Mannan S, Bukhari SI, Zafar SN, Batista S, Chin SL, Arif T, Lawal TA, Aktokmakyan TV, Osborn T, Szakmany T, Sztipits T, Triantafyllou T, Valadez TAC, Singh T, Khaliq T, Patel T, Fadalla T, Jichi T, Sammour T, Al-Shaiji T, Naggs T, Barišić T, Nikolouzakis T, Bisgin T, Perra T, Uprak TK, Dagklis T, Liakakos T, Sidiropoulos T, Adjeso TJK, Dölker T, Oung T, Aherne T, Diehl T, Pinkney T, Raymond T, Rhomberg T, Schmitz-Rixen T, Madhuri TK, Lohmann TK, Yeoh T, Zaimis T, Bright T, Vilz TO, Glowka TR, Board T, Hardcastle T, Cohnert T, Mahečić TT, William TG, Klatte T, Abbott T, Watcyn-Jones T, Mendes T, Kulis T, Sečan T, Campagnaro T, Frisoni T, Simoncini T, Violante T, Safranovs TJ, Risteski T, Pang T, Akinyemi T, Yotsov T, Laeke T, Kochiyama T, Sholadoye TT, Alekberli T, Ezomike U, Giustizieri U, Grossi U, Köksoy ÜC, Bork U, Kisser U, Ronellenfitsch U, Saeed U, Bracale U, Jayarajah U, Rauf UHA, Bumbasirevic U, Ferrer UMJ, Ahmed U, Bello UM, Jogiat U, Sadia U, Galandarov V, Narayanan V, Calu V, Bianchi V, Ciniero V, Tonini V, Silvestri V, Vijay V, Dewan V, Lohsiriwat V, Thuduvage V, Mousafeiris V, Dragisic V, Sasireka V, Santric V, Kusuma VRM, Kolli VS, Alonso V, De Simone V, Picotti V, Martínez VM, Panduro-Correa V, Kakotkin V, Angulo VP, Turrado-Rodriguez V, Krishnamoorthy V, Ban VS, Shah V, Maiola V, Giordano V, La Vaccara V, Lizzi V, Papagni V, Schiavone V, Satchithanantham V, Garcia-Virto V, Jimenez V, Kumar V, Shelat V, Bhat V, Sodhai V, Graziadei V, Kutuzov V, Stoyanov V, Oktseloglou V, Flis V, Elhassan WAF, Yang W, Soon WC, Tashkandi W, Al-Khyatt W, Mabood W, Bijou W, Wijenayake W, D W, Krawczyk W, Atkins W, Bolton W, White W, Ceelen W, Vagena X, Gozal Y, Baba YI, Subramani Y, Jansen Y, Mittal Y, Kara Y, Zwain Y, Noureldin Y, Alawneh Y, Aydin Y, Lam YH, Tang Y, Lim Y, Dean Y, Tanas Y, Su Y-X, Fujimoto Y, Altinel Y, Frolova Y, Oshodi Y, Fadel ZT, Zahid Z, Elahi Z, Djama Z, Zaheen Z, Jawad Z, Demetrashvili Z, Gebremeskel Z, Gudisa Z, Alyami Z, Garoufalia Z, Li Z, Zimak Z, Radin Z, Balogh ZJ (2023) Reducing the environmental impact of surgery on a global scale: systematic review and co-prioritization with healthcare workers in 132 countries. British Journal of Surgery 110:804–817. 10.1093/bjs/znad092
- 8.Thiel CL, Eckelman M, Guido R, Huddleston M, Landis AE, Sherman J, Shrake SO, Copley-Woods N, Bilec MM (2015) Environmental impacts of surgical procedures: life cycle assessment of hysterectomy in the United States. Environ Sci Technol 49:1779–1786. 10.1021/es504719g [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Papadopoulou A, Kumar NS, Vanhoestenberghe A, Francis NK (2022) Environmental sustainability in robotic and laparoscopic surgery: Systematic review. Br J Surg 109:921–932 [DOI] [PubMed] [Google Scholar]
- 10.Bistline J, Abhyankar N, Blanford G, Clarke L, Fakhry R, Mcjeonn H, Reily J, Roney C, Wison T, Yuan M, Zhao A (1979) Zhao A (2022) Actions for reducing US emissions at least 50% by 2030. Science 376:922–924 [DOI] [PubMed] [Google Scholar]
- 11.Jäger-Waldau A, Kougias I, Taylor N, Thiel C (2020) How photovoltaics can contribute to GHG emission reductions of 55% in the EU by 2030. Renew Sustain Energy Rev 126:89 [Google Scholar]
- 12.Pradere B, Mallet R, de La Taille A, Bladou F, Prunet D, Beurrier S, Bardet F, Game X, Fournier G, Lechevallier E, Meria P, Matillon X, Polguer T, Abid N, De Graeve B, Kassab D, Mejean A, Misrai V, Pinar U (2023) Climate-smart actions in the operating theatre for improving sustainability practices: a systematic review. Eur Urol 83:331–342 [DOI] [PubMed] [Google Scholar]
- 13.Harris H, Bhutta MF, Rizan C (2021) A survey of UK and Irish surgeons’ attitudes, behaviours and barriers to change for environmental sustainability. Ann R Coll Surg Engl 103:725–729. 10.1308/rcsann.2021.0271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Garoufalia Z, Cunha M, Dudi-Venkata NN, An Y, Bellato V, Gallardo C, Zaffaroni G, Christensen P, Kenington C, Aytac E, Brady RRW, Pellino G (2022) The European society of coloproctology collecting opinions on sustainable surgery study. Dis Colon Rectum 65:1297–1300 [DOI] [PubMed] [Google Scholar]
- 15.Peters MDJ, Marnie C, Tricco AC, Pollock D, Munn Z, Alexander L, McInerney P, Godfrey CM, Khalil H (2020) Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth 18:2119–2126 [DOI] [PubMed] [Google Scholar]
- 16.Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks L, Hempel S, Akl EA, Chang C, McGowan J, Stewart L, Hartling L, Aldcroft A, Wilson MG, Garritty C, Lewin S, Godfrey CM, MacDonald MT, Langlois EV, Soares-Weiser K, Moriarty J, Clifford T, Tunçalp Ö, Straus SE (2018) PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann Intern Med 169:467–473 [DOI] [PubMed] [Google Scholar]
- 17.Gonzalez-Pizarro P, Brazzi L, Koch S, Trinks A, Muret J, Sperna Weiland N, Jovanovic G, Cortegiani A, Fernandes TD, Kranke P, Malisiova A, McConnell P, Misquita L, Romero CS, Bilotta F, De Robertis E, Buhre W (2024) European Society of Anaesthesiology and Intensive Care consensus document on sustainability. Eur J Anaesthesiol 41:260–277. 10.1097/EJA.0000000000001942 [DOI] [PubMed] [Google Scholar]
- 18.Ranganathan J, Corbier L, Schmitz S, Oren K, Dawson B, Spannagle M, Bp MM, Boileau P, Canada E, Frederick R, Vanderborght B, Thomson HF, Kitamura K, Woo CM, Naseem &, Kpmg P, Miner R, Pricewaterhousecoopers LS, Koch J, Bhattacharjee S, Cummis C, Eaton R, Gillenwater M, Pricewaterhousecoopers MM, Acosta R, Camobreco V (2004) The Greenhouse Gas Protocol A Corporate Accounting and Reporting Standard
- 19.Curran M (2014) Strengths and Limitations of Life Cycle Assessment. In: Background and Future Prospects in Life Cycle Assessments. pp 189–206
- 20.Rizan C, Brophy T, Lillywhite R, Reed M, Bhutta MF (2022) Life cycle assessment and life cycle cost of repairing surgical scissors. Int J Life Cycle Assess 27:780–795. 10.1007/s11367-022-02064-7 [Google Scholar]
- 21.Reike D, Vermeulen W, Witjes S (2022) Conceptualization of Circular Economy 3.0: Synthesizing the 10R Hierarchy of Value Retention Options. In: Towards a Circular Economy. pp 47–70
- 22.Bischofberger S, Adshead F, Moore K, Kocaman M, Casali G, Tong C, Roy S, Collins M, Brunner W (2023) Assessing the environmental impact of an anastomotic leak care pathway. Surg Open Sci 14:81–86. 10.1016/j.sopen.2023.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Billings J, Ovsepyan G, Wend J, Zaghiyan K, Tang J, Fleshner P (2017) Surgical instrument waste in elective colorectal surgery: a prospective. Intervent Study Gastroenterol 152:S1213 [Google Scholar]
- 24.Chasseigne V, Leguelinel-Blache G, Nguyen TL, de Tayrac R, Prudhomme M, Kinowski JM, Costa P (2018) Assessing the costs of disposable and reusable supplies wasted during surgeries. Int J Surg 53:18–23. 10.1016/j.ijsu.2018.02.004 [DOI] [PubMed] [Google Scholar]
- 25.Ford B, Labib P, Kanwar A, Sanders G, Douie W, Winfield M (2022) Reducing single-use surgical instruments during laparoscopic appendicectomy: using sustainable quality improvement as a catalyst to encourage wider behavioural change in a surgical department. BJS 109:1 [Google Scholar]
- 26.Mhlaba JM, Stockert EW, Coronel M, Langerman AJ (2015) Surgical instrumentation: the true cost of instrument trays and a potential strategy for optimization. J Hosp Adm 4:82. 10.5430/jha.v4n6p82 [Google Scholar]
- 27.Cannings E, Kenington C, Cox K (2022) Calculating the carbon footprint of surgical scrubbing. Br J Surg 109:v3 [Google Scholar]
- 28.Jehle K, Jarrett N, Matthews S (2008) Clean and green: saving water in the operating theatre. Ann R Coll Surg Engl 90:22–24. 10.1308/003588408X242277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Langbein T, Sonntag H, Trapp D, Hoffmann A, Malms W, Röth E-P, Mörs V, Zellner R (1999) Laboratory Investigations Volatile anaesthetics and the atmosphere: atmospheric lifetimes and atmospheric effects of halothane, enflurane, isoflurane, desflurane and sevoflurane [DOI] [PubMed]
- 30.Ryan SM, Nielsen CJ (2010) Global warming potential of inhaled anesthetics: application to clinical use. Anesth Analg 111:92–98. 10.1213/ANE.0b013e3181e058d7 [DOI] [PubMed] [Google Scholar]
- 31.Sherman J, Le C, Lamers V, Eckelman M (2012) Life cycle greenhouse gas emissions of anesthetic drugs. Anesth Analg 114:1086–1090. 10.1213/ANE.0b013e31824f6940 [DOI] [PubMed] [Google Scholar]
- 32.Caycedo-Marulanda A, Caswell J, Mathur S (2020) Comparing the environmental impact of anesthetic gases during transanal total mesorectal excision surgery at a tertiary healthcare centre. Can J Anesth 67:607–608 [DOI] [PubMed] [Google Scholar]
- 33.Caycedo-Marulanda A, Mathur S (2022) Suggested strategies to reduce the carbon footprint of anesthetic gases in the operating room. Can J Anesth 69:269–270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hansen EE, Chiem JL, Righter-Foss K, Zha Y, Cockrell HC, Greenberg SLM, Low DK, Martin LD (2023) Project spruce: saving our planet by reducing carbon emissions, a pediatric anesthesia sustainability quality improvement initiative. Anesth Analg 137:98–107. 10.1213/ANE.0000000000006421 [DOI] [PubMed] [Google Scholar]
- 35.Graham CW, Komidar L, Perger L (2019) Comparison of polymeric clips and endoscopic staplers for laparoscopic appendectomy. J Laparoendosc Adv Surg Tech 29:240–242. 10.1089/lap.2018.0173 [DOI] [PubMed] [Google Scholar]
- 36.Friedericy HJ, van Egmond CW, Vogtländer JG, van der Eijk AC, Jansen FW (2022) Reducing the environmental impact of sterilization packaging for surgical instruments in the operating room: a comparative life cycle assessment of disposable versus reusable systems. Sustainability. 10.3390/su14010430 [Google Scholar]
- 37.Blankush JM, Gardiner A, Tiwari V, Jordan M, Baroud H, Koester D, Adams D, Broucek JR (2021) Comparative environmental effects and disability-adjusted life-year impacts of robotic and open ventral hernia repair. Surg Endosc 35:1–10333170335 [Google Scholar]
- 38.Gilliam AD, Davidson B, Guest J (2008) The carbon footprint of laparoscopic surgery: should we offset? Surg Endosc Other Interv Tech 22:573. 10.1007/s00464-007-9722-x [DOI] [PubMed] [Google Scholar]
- 39.Power NE, Silberstein JL, Ghoneim TP, Guillonneau B, Touijer KA (2012) Environmental impact of minimally invasive surgery in the United States: an estimate of the carbon dioxide footprint. J Endourol 26:1639–1644. 10.1089/end.2012.0298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Xu T, Hutfless SM, Cooper MA, Zhou M, Massie AB, Makary MA (2015) Hospital cost implications of increased use of minimally invasive surgery. JAMA Surg 150:489–490 [DOI] [PubMed] [Google Scholar]
- 41.Robb H, Gan J, Winter-Beatty J, Dryden S, Ortega P, Purkayastha S (2022) Back to the future: does increasing the proportion of local anaesthetic inguinal hernia repairs help achieve a #NetZeroNHS? Br J Surg 109:v76 [Google Scholar]
- 42.Ito Y, Damm E, Daley H, Takacs R, Mittal R (2021) Environmental impact of anaesthetic gases at a tertiary hospital: a comparison of subspecialties and analysis of anaesthetic choices. Anaesthesia 76:11–116. 10.1111/anae.15521 [Google Scholar]
- 43.Boag K, Ho T, Quyn A, Peckham-Cooper A (2022) A sustainable appendicectomy. BJS 109:75 [Google Scholar]
- 44.Labib P, Ford B, Winfield M, Douie W, Kanwar A, Sanders G (2023) Revising a laparoscopic appendicectomy set to reduce reliance on disposable surgical instruments: supporting the transition to sustainable surgical practice. Ann R Coll Surgeons Engl. 10.1308/rcsann.2023.0015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cunningham AJ, Krakauer K, Schofield C, Kenron D, Krishnaswami S (2023) Reducing disposable surgical items: decreasing environmental impact and costs at a children’s hospital, a pilot study. J Surg Res 288:309–314. 10.1016/j.jss.2023.02.035 [DOI] [PubMed] [Google Scholar]
- 46.Nast K, Swords KA (2019) Decreasing operating room costs via reduction of surgical instruments. J Pediatr Urol 15:153.e1-153.e6. 10.1016/j.jpurol.2019.01.013 [DOI] [PubMed] [Google Scholar]
- 47.Sinha V, Zolfaghari Y, Vijayan R (2023) The great cover up: Environmental toll of excessive surgical draping in minimally invasive surgery. J Plast Reconstr Aesthet Surg 82:209–210. 10.1016/j.bjps.2023.04.058 [DOI] [PubMed] [Google Scholar]
- 48.Petterwood J, Shridhar V (2009) Water conservation in surgery: a comparison of two surgical scrub techniques demonstrating the amount of water saved using a “taps on/taps off” technique. Aust J Rural Health 17:214–217. 10.1111/j.1440-1584.2009.01074.x [DOI] [PubMed] [Google Scholar]
- 49.Somner JEA, Stone N, Koukkoulli A, Scott KM, Field AR, Zygmunt J (2008) Surgical scrubbing: can we clean up our carbon footprints by washing our hands? J Hosp Infect 70:212–215. 10.1016/j.jhin.2008.06.004 [DOI] [PubMed] [Google Scholar]
- 50.Sánchez-Barroso Moreno G, García-Sanz Calcedo J, González AG, Salgado DR (2019) Sustainable solutions for thermal energy saving in hospital operating theatres. In: E3S Web of Conferences. EDP Sciences
- 51.Agarwal BB, Agarwal KA, Sahu T, Mahajan KC (2010) Carbon footprint of laparoscopic cholecystectomy performed with or without energized dissection: a case controlled study
- 52.Atcheson CLH, Spivack J, Williams R, Bryson EO (2016) Preventable drug waste among anesthesia providers: opportunities for efficiency. J Clin Anesth 30:24–32. 10.1016/j.jclinane.2015.12.005 [DOI] [PubMed] [Google Scholar]
- 53.Baloi A, Butt A (2018) Audit of drug wastage in operation theatres at Louth Group of Hospitals. Royal College of Surgeons in Ireland. Anaesthesia 73:12–116. 10.1111/anae.14448 [Google Scholar]
- 54.Kaniyil S, Krishnadas A, Parathody A, Ramadas K (2017) Financial implications of intravenous anesthetic drug wastage in operation room. Anesth Essays Res 11:304. 10.4103/0259-1162.186596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mankes RF (2012) Propofol wastage in anesthesia. Anesth Analg 114:1091–1092. 10.1213/ANE.0b013e31824ea491 [DOI] [PubMed] [Google Scholar]
- 56.McGain F, Algie CM, O’Toole J, Lim TF, Mohebbi M, Story DA, Leder K (2014) The microbiological and sustainability effects of washing anaesthesia breathing circuits less frequently. Anaesthesia 69:337–342. 10.1111/anae.12563 [DOI] [PubMed] [Google Scholar]
- 57.Pierce JMT, Parker B (2014) Article in Health estate journal: journal of the Institute of Hospital Engineering
- 58.Hickman J, Shinde S (2021) On and off: the importance of the anaesthetic gas scavenging system. Anaesthesia 76:11–116. 10.1111/anae.15521 [Google Scholar]
- 59.Park KY, Russell JI, Wilke NP, Marka NA, Nichol PF (2021) Reducing cost and waste in pediatric laparoscopic procedures. J Pediatr Surg 56:66–70. 10.1016/j.jpedsurg.2020.09.052 [DOI] [PubMed] [Google Scholar]
- 60.Vacharathit V, Walsh RM, Utech J, Asfaw SH (2022) Action in healthcare sustainability is a surgical imperative: this is a novel way to do it. J Surg Educ 79:275–278. 10.1016/j.jsurg.2021.09.002 [DOI] [PubMed] [Google Scholar]
- 61.Zuegge KL, Bunsen SK, Volz LM, Stromich AK, Ward RC, King AR, Sobeck SA, Wood RE, Schliewe BE, Steiner RP, Rusy DA (2019) Provider education and vaporizer labeling lead to reduced anesthetic agent purchasing with cost savings and reduced greenhouse gas emissions. Anesth Analg 128:E97–E99. 10.1213/ANE.0000000000003771 [DOI] [PubMed] [Google Scholar]
- 62.Benness M, Doanne M (2021) Anaesthetists are primed to leap into action on climate change. Anaesth Intensive Care 49:1–16. 10.1177/0310057X211055028 [DOI] [PubMed] [Google Scholar]
- 63.Wyssusek K, Chan KL, Eames G, Whately Y (2022) Greenhouse gas reduction in anaesthesia practice: a departmental environmental strategy. BMJ Open Qual. 10.1136/bmjoq-2022-001867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Davies JF, Seglenieks R, Cameron R, Kuruvilla NA, Grove EM, Shrivathsa A, Grobler S (2023) Operation clean up: A model for eco-leadership and sustainability implementation. Anaesth Intensive Care 51:88–95. 10.1177/0310057X221102469 [DOI] [PubMed] [Google Scholar]
- 65.Alexander R, Poznikoff A, Malherbe S (2018) Greenhouse gases: the choice of volatile anesthetic does matter. Can J Anesth 65:221–222 [DOI] [PubMed] [Google Scholar]
- 66.Boyle A, Coleman A, Barker K, Baraclough D (2018) A grassroots approach to the greenhouse effect: implementing recent guidance from the AAGBI and RCoA. Anaesthesia 73:12–116. 10.1111/anae.14448 [Google Scholar]
- 67.Carter LA, Oyewole M, Bates E, Sherratt K (2019) Promoting low-flow anaesthesia and volatile anaesthetic agent choice. BMJ Open Qual. 10.1136/bmjoq-2018-000479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Glenski TA, Levine L (2020) The implementation of low-flow anesthesia at a tertiary pediatric center: A quality improvement initiative. Paediatr Anaesth 30:1139–1145. 10.1111/pan.13994 [DOI] [PubMed] [Google Scholar]
- 69.Gough V, Strunzova A, Curry H (2022) Laparoscopic Cholecystectomy-can we make it both Greener and cheaper? BJS 109:19–20 [Google Scholar]
- 70.Adler S, Scherrer M, Rückauer KD, Daschner FD (2005) Comparison of economic and environmental impacts between disposable and reusable instruments used for laparoscopic cholecystectomy. Surg Endosc Other Interv Tech 19:268–272. 10.1007/s00464-003-9232-4 [DOI] [PubMed] [Google Scholar]
- 71.Boberg L, Singh J, Montgomery A, Bentzer P (2022) Environmental impact of single-use, reusable, and mixed trocar systems used for laparoscopic cholecystectomies. PLoS ONE. 10.1371/journal.pone.0271601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Rizan C, Bhutta MF (2022) Environmental impact and life cycle financial cost of hybrid (reusable/single-use) instruments versus single-use equivalents in laparoscopic cholecystectomy. Surg Endosc 36:4067–4078. 10.1007/s00464-021-08728-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Colak T, Ersoz G, Akca T, Kanik A, Aydin S (2004) Efficacy and safety of reuse of disposable laparoscopic instruments in laparoscopic cholecystectomy: a prospective randomized study. Surg Endosc Other Interv Tech 18:727–731. 10.1007/s00464-004-8112-x [DOI] [PubMed] [Google Scholar]
- 74.Loftus TJ (2015) A comparison of the defect rate between original equipment manufacturer and reprocessed single-use bipolar and ultrasound diathermy devices. J Med Devices Trans ASME 10(1115/1):4030858 [Google Scholar]
- 75.Burguburu A, Tanné C, Bosc K, Laplaud J, Roth M, Czyrnek-Delêtre M (2022) Comparative life cycle assessment of reusable and disposable scrub suits used in hospital operating rooms. Cleaner Environ Syst. 10.1016/j.cesys.2021.100068 [Google Scholar]
- 76.Vozzola E, Overcash M, Griffing E (2020) An environmental analysis of reusable and disposable surgical gowns. AORN J 111:315–325. 10.1002/aorn.12885 [DOI] [PubMed] [Google Scholar]
- 77.Conrardy J, Hillanbrand M, Myers S, Nussbaum GF (2010) Reducing medical waste. AORN J 91:711–721. 10.1016/j.aorn.2009.12.029 [DOI] [PubMed] [Google Scholar]
- 78.Dettenkofer M, Grießhammer R, Scherrer M, Daschner F (1999) Life-cycle assessment of single-use versus reusable surgical drapes (cellulose/polyethylene ± mixed cotton system). Surgeon 70:485–491 [DOI] [PubMed] [Google Scholar]
- 79.Rizan C, Lillywhite R, Reed M, Bhutta MF (2022) Minimising carbon and financial costs of steam sterilisation and packaging of reusable surgical instruments. Br J Surg 109:200–210. 10.1093/bjs/znab406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Brady JT, Bhakta A, Steele SR, Trunzo JA, Senagore AJ, Holmgren K, Schillero A, Champagne BJ (2017) Reprocessed bipolar energy for laparoscopic colectomy: Is it worth it? Am J Surg 214:59–62. 10.1016/j.amjsurg.2017.02.012 [DOI] [PubMed] [Google Scholar]
- 81.Ibbotson S, Dettmer T, Kara S, Herrmann C (2013) Eco-efficiency of disposable and reusable surgical instruments: a scissors case. Int J Life Cycle Assess 18:1137–1148. 10.1007/s11367-013-0547-7 [Google Scholar]
- 82.McGain F, McAlister S, McGavin A, Story D (2010) Reusable vs single-use dRug tRays. Anesthesia Intensive Care 38:583–544 [DOI] [PubMed] [Google Scholar]
- 83.Amariglio A, Depaoli D (2021) Waste management in an Italian Hospital’s operating theatres: an observational study. Am J Infect Control 49:184–187. 10.1016/j.ajic.2020.07.013 [DOI] [PubMed] [Google Scholar]
- 84.McKendrick 2017 Pragmatic recycling of paper and cardboard in the operating theatre- an audit [DOI] [PubMed]
- 85.Wyssusek K, Keys M, Laycock B, Avudainayagam A, Pun K, Hansrajh S, van Zundert A (2020) The volume of recyclable polyethylene terephthalate plastic in operating rooms: a one-month prospective audit. Am J Surg 220:853–855 [DOI] [PubMed] [Google Scholar]
- 86.Tieszen ME, Gruenberg JC A Quantitative, qualitative, and critical assessment of surgical waste surgeons venture through the trash can [PubMed]
- 87.Singleton J, Paterson S, Davis A, Karmali A (2019) Introducing PVC recycling to theatres: the challenges faced. Anaesthesia 74:10–101. 10.1111/anae.14812 [Google Scholar]
- 88.Martin DM, David Yanez CN, Treggiari MM (2017) An initiative to optimize waste streams in the operating room: RECycling in the Operating Room (RECOR) Project, AANA Journal, April 2017 [PubMed]
- 89.Martin C, Labaste F, Assad A, Minville V, Vardon-Bounes F (2022) Implementation of a more sustainable waste management policy in the operating room. Anesthesiology 137:748–749. 10.1097/ALN.0000000000004350 [DOI] [PubMed] [Google Scholar]
- 90.Sadler A, Wilde P, Raju P, Rodney G (2017) A trial of metal recycling in healthcare waste management. Anaesthesia 72:10–88. 10.1111/anae.14060 [Google Scholar]
- 91.van Straten B, Dankelman J, van der Eijk A, Horeman T (2021) A Circular Healthcare Economy; a feasibility study to reduce surgical stainless steel waste. Sustain Prod Consum 27:169–175. 10.1016/j.spc.2020.10.030 [Google Scholar]
- 92.Dohmen J, Lessau M, Schmitz M, Kalff JC (2023) Recycling of disposable surgical instruments - is it worth it? Zentralblatt fur Chirurgie - Zeitschrift fur Allgemeine, Viszeral- und Gefasschirurgie 148:329–336. 10.1055/a-2122-7519 [DOI] [PubMed] [Google Scholar]
- 93.Rouvière N, Chkair S, Auger F, Alovisetti C, Bernard MJ, Cuvillon P, Kinowski JM, Leguelinel-Blache G, Chasseigne V (2022) Ecoresponsible actions in operating rooms: a health ecological and economic evaluation. Int J Surgery. 10.1016/j.ijsu.2022.106637 [DOI] [PubMed] [Google Scholar]
- 94.McGain F (2009) An audit of potentially recyclable waste from anaesthetic practice. Anaesthesia Intens Care 37:820–823 [DOI] [PubMed] [Google Scholar]
- 95.Nesaratnam A, Jani K, Cleaver S (2018) Sustainability in anaesthesia: a service evaluation of theatre waste recycling. Anaesthesia 73:9–79. 10.1111/anae.14192 [Google Scholar]
- 96.Connolly M, Smith N (2019) A Novel method of recycling in wollongong operating theatres. Anaesth Intensive Care 47:1–29. 10.1177/0310057x19846066 [Google Scholar]
- 97.Livingston A, Warnock G, Morrison A (2019) Waste segregation initiative in a district general hospital. Anaesthesiae 74:10–101. 10.1111/anae.14812 [Google Scholar]
- 98.Fraifeld A, Rice AN, Stamper MJ, Muckler VC (2021) Intraoperative waste segregation initiative among anesthesia personnel to contain disposal costs. Waste Manage 122:124–131. 10.1016/j.wasman.2021.01.006 [DOI] [PubMed] [Google Scholar]
- 99.Hubbard RM, Hayanga JA, Quinlan JJ, Soltez AK, Hayanga HK (2017) Optimizing anesthesia-related waste disposal in the operating room: a brief report. Anesth Analg 125:1289–1291. 10.1213/ANE.0000000000001932 [DOI] [PubMed] [Google Scholar]
- 100.Wyssusek KH, Foong WM, Steel C, Gillespie BM (2016) The gold in garbage: implementing a waste segregation and recycling initiative. AORN J 103:316.e1-316.e8. 10.1016/j.aorn.2016.01.014 [DOI] [PubMed] [Google Scholar]
- 101.Wormer BA, Augenstein VA, Carpenter CL, Burton P V, Yokeley WT, Prabhu AS, Harris B, Norton S, Klima DA, Lincourt AE, Todd Heniford B The green operating room: simple changes to reduce cost and our carbon footprint [PubMed]
- 102.Lanzoni L, Whatford L, Atzori AS, Chincarini M, Giammarco M, Fusaro I, Vignola G (2023) Review: the challenge to integrate animal welfare indicators into the life cycle assessment. Animal 17:8 [DOI] [PubMed] [Google Scholar]
- 103.Moore D, Johnson S, Synott K, Lynch T, Ryan K, Reilly S, Boccato L, Viani L, Bracken T, Julius B, Conlon E, Stanistreet D (2024) Sustainability Principles and Practice in Surgery
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.