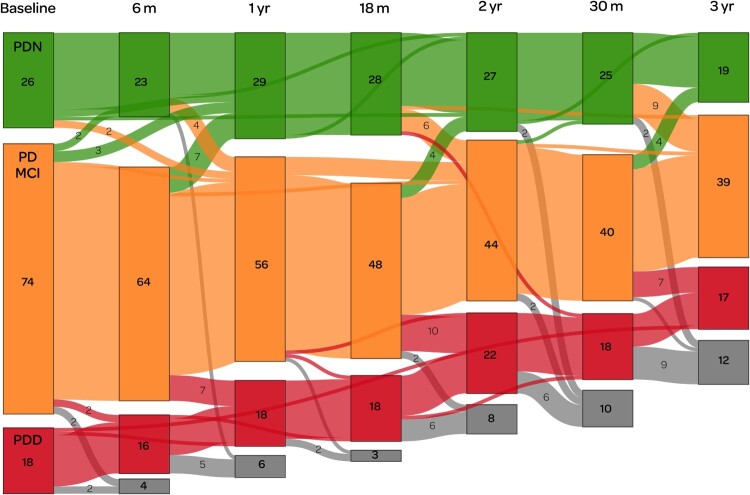
Figure 4.
Depiction of a sub-study in which we used positron emission tomography (PET) imaging to measure cerebral amyloid in Parkinson’s (Melzer et al. 2019). This illustrates the complexity of longitudinal research in patients who can change (not always unidirectionally) between diagnostic categories, who do not always attend all scheduled sessions, and who are also at substantial risk of dropping out due to mortality and morbidity. We began with a sub-sample enriched to over-represent PD-MCI (74 participants at baseline, shown in orange), with smaller reference groups of PDN (green, n = 26) and PDD (red, n = 18). Coloured boxes show the number of participants within each category at (ideally) 6-monthly assessment intervals over a three year period. Grey boxes indicate those who were lost to follow-up at each assessment, due to death or other factors. Numbers in a lighter-weight font indicate transitions between different categories. Only one person appeared to transition directly (between assessments at 18 and 30 months) from PDN to PDD: otherwise, all conversions to dementia were detected via the intermediate stage of PD-MCI. Some PD-MCI participants, meanwhile, reverted to being classified as PDN, indicating the inherent difficulty in determining the boundary between the two states. Although the number of people with PDD appears to have been relatively constant throughout the study, only one person who entered the study with PDD actually survived to completion: the remainder developed dementia during the study. Figure available under an open CC-BY licence (MacAskill 2021b).