Abstract
Aim:
This article reports on the development of patient resources for the IMPlementing IMProved Asthma self-management as RouTine (IMP2ART) programme that aimed to encourage patients to attend asthma reviews (invitation letters), encourage patients to enquire about asthma action plans (posters), and equip patients with the knowledge to manage their asthma (information website).
Background:
To improve supported asthma self-management in UK primary care, the IMP2ART programme developed a whole-systems approach (patient resources, professional education, and organisational strategies).
Methods:
Linked to behaviour change theory, we developed a range of patient resources for primary care general practices (an information website, invitation letters to invite patients for asthma reviews, and posters to encourage asthma action plan ownership). We elicited qualitative feedback on the resources from people living with asthma in the UK (n = 17). In addition, we conducted an online survey with volunteers in the UK-wide REgister for Asthma researCH (REACH) database to identify where they source asthma information, whether their information needs are met, and what information would be useful (n = 95).
Findings:
Following feedback gathered from the interviews and the online survey, we refined our patient resources for the IMP2ART programme. Refinements included highlighting the seriousness of asthma, enhancing trustworthiness, and including social support resources. We also made necessary colour and formatting changes to the resources. In addition, the patient resources were updated following the COVID-19 pandemic. The multi-stage development process enabled us to refine and optimise the patient resources. The IMP2ART strategy is now being tested in a UK-wide cluster RCT (ref: ISRCTN15448074).
Keywords: asthma, asthma education, patient education, patient resources
Introduction
There are approximately 5.4 million people living with asthma across the United Kingdom (UK) (Asthma UK, 2020) resulting in around 6.3 million primary care consultations and 100 000 hospital admissions per year (Mukherjee et al., 2016). A recent meta-review found that supported asthma self-management can reduce hospitalisations, accident and emergency attendances, and unscheduled care consultations (Pinnock et al., 2017). Further, supported self-management can improve markers of asthma control and quality of life across a range of demographic, cultural, and healthcare settings (Pinnock et al., 2017). Core components of supported asthma self-management include a personalised asthma action plan, regular clinical review, and appropriate patient education (Hodkinson et al., 2020).
Despite strong evidence of its benefits (Pinnock et al., 2017), and recommendations in national and international asthma guidelines (BTS/SIGN, 2019; Global Initiative for Asthma, 2022), supported asthma self-management is poorly implemented. For example, only half of respondents (52%) to a survey conducted by Asthma UK owned an asthma action plan (Asthma UK, 2020), whilst in our review of clinical records only 6% of people with asthma had a record of being provided with an action plan (Newby et al., 2017). Further, according to the annual Asthma UK survey (Asthma UK, 2020), almost 30% of respondents had not attended an annual asthma review in which basic asthma care can be provided and supported self-management discussed.
To promote asthma self-management and support action plan implementation, understanding the needs of people with asthma is pivotal. A recent systematic review exploring barriers and facilitators of effective asthma self-management identified that patients expressed a need for information, especially about asthma control, triggers, and medication (Miles et al., 2017). These findings were relatively universal including among those with low health literacy and those from ethnic minorities, who actively sought information often from lay sources (Miles et al., 2017). Similarly, a survey from Australia on information needs of those with asthma showed that a third of respondents had outstanding information needs (Kong et al., 2013) on similar topics.
In response to the poor implementation of supported asthma self-management in UK primary care, the IMPlementing IMProved Asthma self-management as RouTine (IMP2ART) programme was developed (McClatchey et al., 2023). IMP2ART aims to develop and evaluate a whole-systems implementation strategy comprising of resources for patients (e.g. information for patients, invitation letters showing the importance of asthma reviews, promotional materials that highlight the importance of asthma action plans), professional training, and organisational resources. This paper reports on the design and development of theoretically informed patient resources that can be used in primary care general practices to help provide information, encourage attendance at annual reviews, and encourage action plan ownership for those living with asthma.
Methods
The IMP2ART patient resources were developed between late-2018 and late-2020 (see Figure 1) in line with O’Cathain et al.’s (2019) guidance on how to develop complex interventions to improve health and healthcare. The IMP2ART team developed resources with our Asthma UK Centre for Applied Research (AUKCAR) Patient and Public Involvement (PPI) group (‘PPI colleagues’), and our Professional Advisory Group (‘Professional colleagues’), which consisted of general practitioners (GPs) and nurses from the Primary Care Respiratory Society (PCRS). Table 1 maps the development of the patient resources to the guidance.
Figure 1.
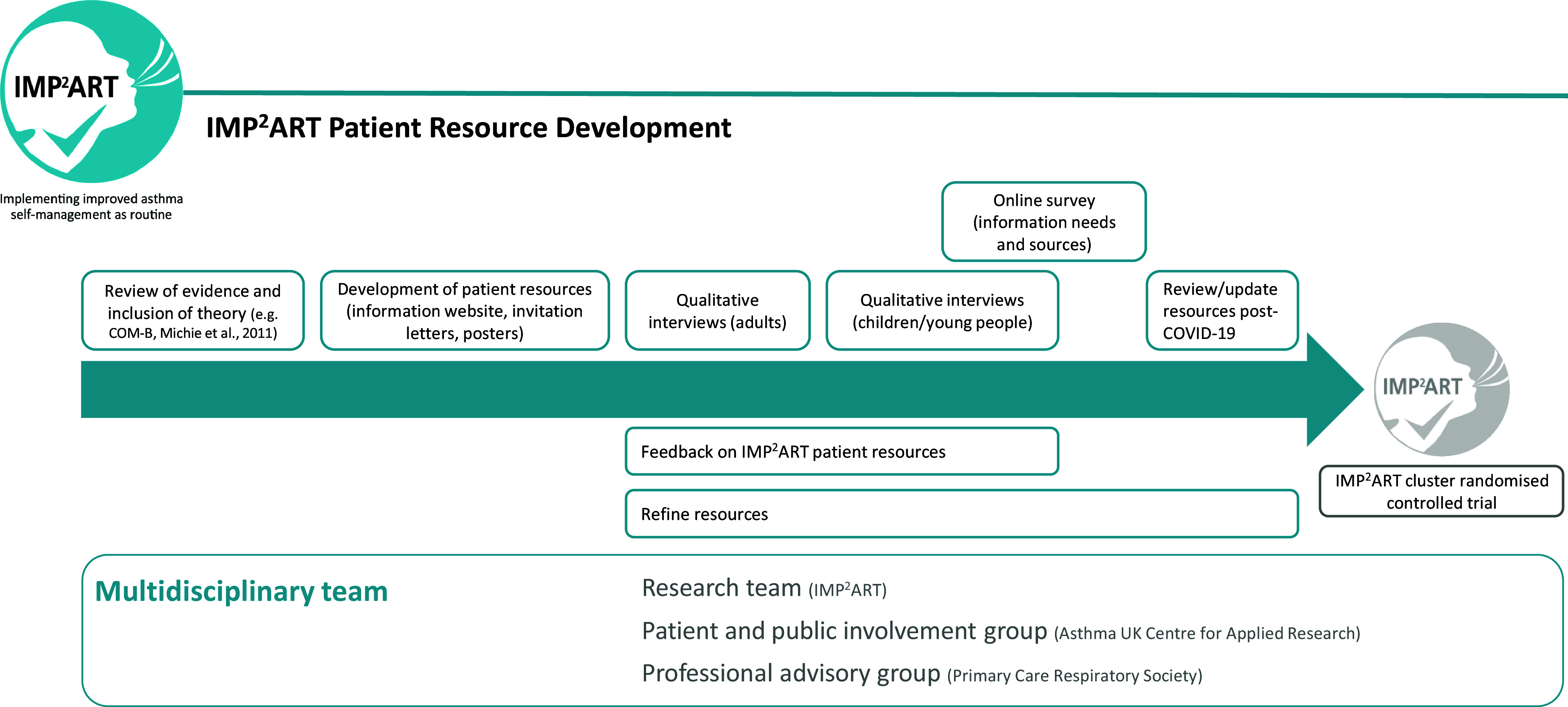
Development phases of the IMP2ART patient resources.
Table 1.
Framework of actions for intervention (patient resources) development (O’Cathain et al., 2019)
| Action | Application to the development of patient resources within the IMP2ART programme |
|---|---|
| Plan the development process |
|
| Involve stakeholders, including those who will deliver, use and benefit from the intervention |
|
| Bring together a team and establish decision-making processes |
|
| Review published research evidence |
|
| Draw on existing theories |
|
| Articulate programme theory |
|
| Undertake primary data collection |
|
| Understand context |
|
| Pay attention to future implementation of the intervention in the real world |
|
| Design and refine the intervention |
|
| End the development phase |
|
Design of the IMP2ART patient resources
Prior research (Miles et al., 2017; Morrow et al., 2017; Daines et al., 2020) has highlighted that patients want more information about managing their asthma, and that encouraging patients to attend for routine asthma reviews can be challenging. Considering this with the low uptake of asthma action plans (Asthma UK, 2020), and with the advice of the patient and professional colleagues, three resources were conceived: a patient information website, invitation letters for general practices to invite patients for asthma reviews, and posters to encourage asthma action plan ownership. To develop the resources, we utilised behaviour change techniques (the active component of an intervention designed to change behaviour) from the Behavior Change Technique Taxonomy (Michie et al., 2013). The three resources are outlined below.
Patient information website
For the patient information website, we aimed to find existing relevant online asthma information from trusted asthma sources (e.g. the charities Asthma UK and the British Lung Foundation (now merged as Asthma and Lung UK), the European Lung Foundation, My Lungs my Life, and the NHS) and house all the information topics on one site with links to the original sources. The information included a variety of topics that covered, for example: general asthma information (e.g. what is asthma); annual asthma reviews; triggers; living with asthma (e.g. exercise, sleep, travel etc.); asthma attacks; coping with asthma and emotions; children and young people; asthma management (e.g. asthma action plans – where we considered various languages, literacy, and age groups); and inhaler technique videos.
Invitation letters
The IMP2ART team designed three invitation letter templates that general practices could tailor and send to patients to: 1) invite patients for their annual review, 2) remind patients about missed review appointments, 3) invite patients to a review following unscheduled care. Invitation letters were designed to include behaviour change techniques identified from the Behavior Change Technique Taxonomy (Michie et al., 2013) including ‘information about health consequences’, for example, that asthma is a variable condition and self-management can reduce symptoms and the risk of an asthma attack, and a ‘social comparison’, for example, that one in three people in the UK have an asthma action plan.
Posters for use in primary care practices
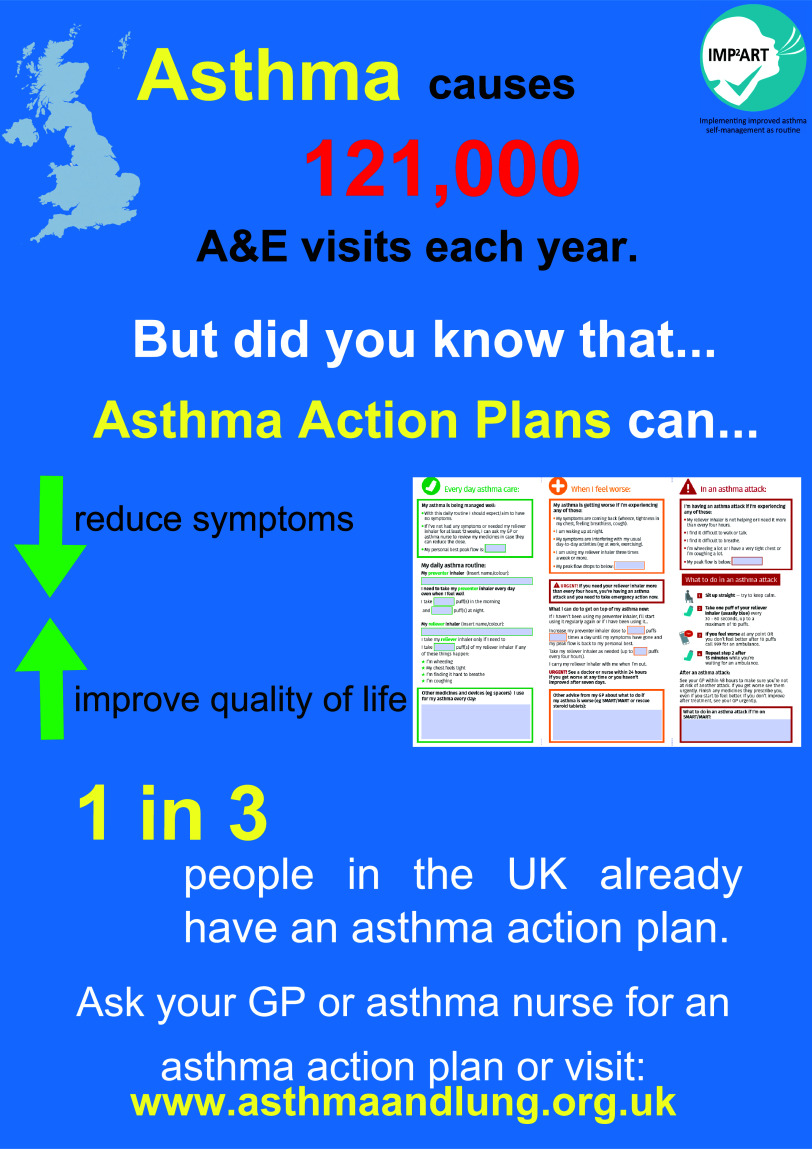
We designed two posters for use in general practices to encourage and prompt conversations around asthma action plan ownership, one for noticeboards and a digital version for display screens. Both poster types contained the same text content. Posters were also designed in line with behaviour change techniques (Michie et al., 2013), and included ‘information about health consequences’, for example, that asthma causes 6.3 million GP consultations per year, and a ‘social comparison’ for example that one in three people in the UK have an asthma action plan.
Two rounds of feedback and refining the patient resources
We conducted semi-structured qualitative interviews with adults in the UK living with asthma (in February–March 2019) to obtain initial feedback on the prototype IMP2ART resources. Participants were purposively recruited from six demographically diverse general practices (e.g. patient list size, socioeconomic status). Eligible patients included those over 18 years old with ‘active asthma’ (defined as having a coded diagnosis and received pharmacological treatment within the previous year (NHS Confederation, 2003)), with the capacity to provide informed consent and take part in the interview. GPs could exclude participants in the event of substantial comorbidity (e.g. dementia), illness, or residential care.
Prototype versions of the resources were sent to participants in a pdf format. The website pdf listed the source of the online information (e.g. Asthma UK) and was broken down into topic areas (e.g. triggers) with subheadings (e.g. pollen). The topic guide asked participants what thoughts they had on the resources, and what feedback they had (if any). Following giving participants information about the study and obtaining informed consent, interviews were conducted via telephone and were carried out by KM (a health psychologist) and KS (a medical student) and lasted 20 to 40 min. Participants were unknown to the researchers.
Following refinements of the resources based on recommendations from round one interviews, we realised that many of the resources were directed at children and therefore conducted a second round of semi-structured qualitative interviews and focus groups with children and young people. They were purposively recruited via a general practice and the SPEAK Asthma network (a group enabling children and young people living with asthma to get involved in research at the Asthma UK Centre for Applied Research). Eligible patients included those 6–16 years old with ‘active asthma’ and having the capacity to provide informed consent or take part in the interview. Interviews and focus groups were conducted face-to-face by KM between July and September 2019 after informed consent was obtained, and lasted between 15 and 35 min in duration. Interviews from both phases were audio-recorded, transcribed verbatim, and analysed using Framework Analysis (Ritchie & Spencer, 1994) supported by NVivo 11.
Sense-checking resources for the patient website (quantitative survey)
We conducted an online survey, to ensure we captured well-used information sources for the website and included information where gaps where identified. The survey included both open and closed questions that were designed in line with the Practical Reviews in Self-Management Support (PRISMS) taxonomy (Pearce et al., 2016). The survey questions included demographic information; perception of asthma symptoms; where information about asthma is sourced (e.g. from healthcare professionals, websites); whether information needs are met; and what information would be useful for patients. Survey participants were recruited using the REgister for Asthma researCH (REACH) recruitment database. REACH was a secure database that people living with asthma (aged 16 years and over) in the UK were able to register their information, in order to be informed about research studies. Participants signed up to the database were emailed information about the survey and instructions on how to participate (if they were over 16 years old with ‘active asthma’). Following obtaining informed consent, data were collected between August and September 2019. Survey data were anonymised and analysed using descriptive statistics in SPSS version 24.
Results
Feedback on the patient resources (qualitative interviews with adults)
A total of ten participants completed interviews (seven female; age range 38–75 years, all located in Scotland), one of whom also provided feedback on the resources via email, and a further two individuals provided feedback on the resources via email alone. Three themes were identified and are described below.
Patient information website
Almost all participants had positive perceptions of the prototype website, finding the content clear, concise, and educational. Participants generally agreed that the website was comprehensive, as there was useful information across a wide range of topics which covered various demographics (e.g. children and adults).
‘The “for kids” one I thought was extremely good, I really liked that… It’s making it child-friendly, which I thought was a really nice thing’. (Participant 5, female)
Some participants viewed the website as a good source to learn more about their condition and even gained new knowledge.
“I didn’t realise that – I don’t drink a lot – but I didn’t realise until I read this that alcohol can affect your asthma…” (Participant 8, male)
Trustworthiness was discussed as key to patient information. The NHS website was regarded as an especially reliable source, being the primary online resource for some participants. Participants voiced that they trust sources recommended by their healthcare professional (e.g. GP, pharmacist).
“The NHS website I think is very good to check up on ailments and things, and the information they give, I trust that quite a lot. I think there are some websites and things that are a bit… not trustworthy.” (Participant 3, female)
In terms of recommendations for the website, a participant suggested to include an opening description for the website, and one participant suggested the inclusion of social support networks for people with asthma, as it was something she found valuable when managing her condition.
Invitation letters
Information included in the letters was viewed positively by participants in terms of simplicity, clarity, and the amount of detail covering everything patients would need to know before attending a review appointment.
“It’s not long-winded, it’s reasonably short, to-the-point, and it’s clear and easy to understand.” (Participant 6, female)
The significance of letters in asthma care was recognised, as participants appreciated receiving such letters particularly after experiencing an asthma attack.
“I would be quite pleased that somebody was following up on the attack and making sure that I was having the right treatment and doing the proper things to help prevent having another one.” (Participant 8, male)
Most participants found the IMP2ART invitation letters similar to the letters they already receive from their practices, although more detailed and with the explicit mention of action plans. In contrast, a few interviewees mentioned the level of detail in the letters was ‘too wordy’ and ‘dense’. Furthermore, all participants agreed that both annual review and post-asthma attack letters would have a positive effect on attendance. Some interviewees suggested that the letters should emphasise the importance of reviews by highlighting (in a sensitive manner) the negative health consequences of not attending reviews.
“…say that this review is to help you get over your asthma attacks, to miss out on this review may involve you suffering more. Without being bullyish.” (Participant 8, male)
Participants offered a variety of suggestions for emphasising the necessity of having a post-attack review, such as adding colour, boldness, and making the important information larger and more strongly worded.
Posters for use in primary care practices
Participants indicated that the information on both the noticeboard and digital poster was clear and easily comprehensible, some attributing this to the simple language.
“It’s in very straightforward English, it’s not oodles and oodles of information, and it’s nice short concise sentences.” (Participant 1, female)
Views varied on visual aspects of posters such as layout, graphics, colour, text size, and blank space. Some of the participants thought that the noticeboard poster was eye-catching due to its colour and brightness while others thought that it was cramped and too busy. Some interviewees, however, described the digital posters which had less imagery as ‘dull’, and not as eye-catching as the noticeboard posters but conversely thought they were more effective in presenting the information as they had more free space around the text. They believed that digital posters would be noticed more because people nowadays pay more attention to electronic screens. Participants agreed that the posters would have some degree of success in encouraging patients to enquire about or use action plans. They assumed that the information on the benefits of action plans (e.g. reducing symptoms, improving quality of life) would spark interest in asthma patients.
“…it’s suggesting it [an action plan] can reduce the symptoms and increase your quality of life then obviously you would be interested, wouldn’t you?” (Participant 10, male)
Other participants, through recalling their own experiences of sitting in waiting rooms, stated that unwell patients may be unlikely to pay attention to any posters.
“I think people in that situation… I know from when I was at [a hospital for treatment], that you’re so focused on your own thing, it’s not the point that you’re maybe ready to absorb information like that, the visual cues.” (Participant 9, female)
The majority of suggestions about the poster centred around its design, such as removing images to make the noticeboard poster less busy and replacing them with asthma-related information (e.g. a helpline number). Further, participants suggested stronger wording to emphasise the importance of asthma action plans.
“It says “asthma causes 6.3 million GP consultations a year” but it’s not saying that, you know, asthma is dangerous…what it’s not saying here is that actually, you know, an action plan could actually save your life.” (Participant 5, female)
Refinements to the patient resources following the qualitative interviews with adults
Following the qualitative exploration, we designed the next version of the patient information website with University of Edinburgh website developers. The IMP2ART team and PPI colleagues agreed on visual options for the website (including both desktop and mobile versions). We included a clear descriptor on the homepage detailing the purpose of the website and that the site had been designed by a team of researchers and patients at the Asthma UK Centre for Applied Research. This descriptor was designed to enhance trustworthiness (which was highlighted by participants in the interviews as being an important factor), and we also added the university logo to the website footer. Through feedback from the PPI group, accessibility was considered, for example, images descriptions were added where necessary and embedded videos included subtitles.
For the invitation letters, we made minor formatting changes, including making some content bold to highlight the importance of the review, and added a sentence that asked patients to bring their asthma action plan to their review. We did not respond to some suggestions, for example, to add colour, as we learnt from qualitative data collection that general practices rarely use colour printing (Morrow et al., 2017). We refined the posters to ensure that the images were clear. We also changed the opening statement from ‘Asthma causes 6.3 million GP consultations a year’ to ‘Asthma causes 121 000 A&E visits each year’. This was based on feedback to highlight the seriousness of asthma.
Feedback on the refined patient resources (qualitative interviews with children and young people)
A total of seven children and young people (five female; age range 11–15 years, located in both England and Scotland) participated in interviews or focus groups, and we found that participants were positive about the patient information website (although they rarely utilised the internet for information about asthma). One focus group participant mentioned that the colours and icons of the website looked “very NHS-ey” which another participant agreed and said it “associates it with…the healthcare system… it associates you into thinking it’s a good reliable website”. The participants did not have any feedback about the invitation letters, and although most were positive about the posters it was recommended to make the colours stand out more.
Refinements to the patient resources following the qualitative interviews with children and young people
We made minor changes to some of the colours on the poster to stand out. Figure 2 displays the finalised version of the noticeboard poster.
Figure 2.
Finalised version of the noticeboard poster for use in general practices to encourage asthma action plan ownership.
Sense-checking resources for the patient website (online survey)
Of the total 151 eligible participants invited to participate, 95 completed the online survey (62.9% response rate). Participant characteristics can be found in Table 2.
Table 2.
Online survey participant characteristics
| Participant characteristics | n | % | |
|---|---|---|---|
| Age group (years) | 16–25 | 20 | 21.1 |
| 26–35 | 15 | 15.8 | |
| 36–45 | 21 | 22.1 | |
| 46–55 | 13 | 13.7 | |
| 56–65 | 18 | 18.9 | |
| 65 and over | 8 | 8.4 | |
| Gender | Male | 29 | 30.5 |
| Female | 65 | 68.4 | |
| Non-binary | 1 | 1.1 | |
| Duration of asthma diagnosis | Less than a year | 2 | 2.1 |
| 1–10 years | 15 | 15.8 | |
| More than 10 years | 78 | 82.1 | |
| Perceived asthma severity | Very mild | 6 | 6.3 |
| Mild | 24 | 25.3 | |
| Moderate | 40 | 42.1 | |
| Severe | 19 | 20 | |
| Very severe | 6 | 6.3 | |
Fewer than half of the respondents had an asthma action plan (n = 45; 47.4%), and of those, 82% received the action plan from a healthcare professional. Most respondents had a regular asthma review at their general practice (n = 75; 78.9%), mostly with a nurse (n = 68; 90.7%), though GPs (n = 6; 8.0%) and pharmacists (n = 1; 1.3%) also conducted reviews.
Information provision
Fewer than half of the respondents felt that all or a lot of their asthma information needs were met (n = 44; 46.3%), and only half (n = 51; 53.7%) felt there was adequate information available from their general practice explaining asthma and how to manage it. Over half of the sample (n = 53; 55.8%) had not received any resources to help with asthma management skills (e.g. information about inhaler technique). Further, social support was recommended by a healthcare professional to only 2.1% of participants (n = 2).
Information sources and usage
Most participants (n = 72; 75.8%) would contact their general practice if they had any questions about their asthma. Other information sources included websites (n = 58; 61.1%) (mostly Asthma UK (n = 31), and the NHS (n = 22)); the Asthma UK helpline (n = 25; 26.3%); pharmacists (n = 24; 25.3%); the emergency department (n = 10; 10.5%); and the NHS 24 helpline (n = 8; 8.4%). Most respondents had not used resources to encourage them to take medication for their asthma (n = 78; 82.1%). Less than a third of respondents used resources to monitor asthma symptoms (n = 29; 30.5%), and of those, 62.1% used mobile applications, and 34.5% used a diary to monitor symptoms. Most of the sample did not use any resources to help them to prepare for consultations with their healthcare provider about their asthma (n = 79; 83.2%). Further, most of the sample did not use any information to support the day-to-day management of their lifestyle (n = 68; 71.6%).
Information recommendations
Those who felt that there was not adequate information available to them from their general practice were asked what information would be helpful. The most requested information included asthma leaflets (n = 6), advice on asthma treatment (e.g. inhalers, how to use them, and side effects) (n = 6), provision of an action plan (n = 6), information on how asthma happens and diagnoses information (n = 3), information about severe asthma (n = 4), and support groups available (n = 2). Respondents also suggested there should be posters about asthma in general practices (n = 3), and further information available online (n = 2) including ‘a repository of information available online to patients’.
In an optional open response question, respondents were able to describe the information about asthma that they most needed. Treatment and medication information (including how to use inhalers) (n = 28) and information about asthma management including how to manage symptoms and when to call for help (n = 29) were the most stated needs. Additionally, a number of respondents wanted further information on asthma triggers (n = 4) information about asthma generally, for example, why it happens, how it affects the body, and the long-term prognosis (n = 3) and day-to-day living with asthma, for example, employment, sleep, and travel (n = 5).
Refinements to the patient resources following the online survey
The survey supported our rationale to provide various resources for patients, for example, an information website and posters about asthma. In terms of website content, the survey ensured that we included suggested topics and relevant sources of information for those living with asthma in the UK. For example, we added a dedicated social support section, which is linked to various trusted asthma relevant social support forums (e.g. Asthma UK and British Lung Foundation).
Refinements following the COVID-19 pandemic
During the COVID pandemic, we reviewed our IMP2ART patient resources. We conducted a rapid review of COVID-19 information for those living with asthma (McClatchey et al., 2021) and added a section on the patient information website for COVID-19 and asthma. We also collaborated with PPI and professional colleagues to create additional videos for the website on topics including: ‘Patient’s tips for managing your asthma’; ‘Get the best from your asthma review’; and ‘Working together with patients’.
Additionally, we changed the wording of the invitation letters to reflect that appointments may be conducted remotely, and we added an image on the letter to reflect a remote appointment (a smartphone and computer screen).
A dynamic and iterative process
The process of developing the finalised IMP2ART patient resources followed key principles of intervention development, that it is dynamic, iterative, creative, and open to change (O’Cathain et al., 2019). We have continued to identify new content for the information website as it became available throughout the development process – for example, reflecting the topic of climate change and metered dose inhalers.
Discussion and conclusion
We developed a suite of resources for patients (information website, invitation letters, and posters) that general practices in the implementation arm of the IMP2ART cluster-RCT could use to support asthma self-management. We followed a systematic approach to intervention development (O’Cathain et al., 2019), and the resources were initially developed in line with behaviour change theory and adapted according to feedback from those currently living with asthma. Further, this paper adds to the available knowledge on the self-management educational needs of asthma patents in the UK.
Prior research and the current online survey exploration shows that asthma information needs are often not met (Kong et al., 2013; Miles et al., 2017), and the IMP2ART patient website aims to address this gap. The IMP2ART patient website was adapted during its development to ensure trustworthiness following the qualitative feedback we received. This may have a positive effect on trust and credibility, as a review exploring web-based health information found that the authority of the owner can positively impact trust and credibility (Sbaffi & Rowley, 2017). By ensuring that the information aligned with UK guidelines (BTS/SIGN, 2019; NICE, 2021), we reduced the risk of patients receiving conflicting advice.
Both the patient website and the invitation letters highlight the importance of asthma reviews, which may improve on the current figures of non-attendance at asthma reviews (approximately 30% (Asthma UK, 2020)). Further, there are suboptimal levels of asthma action plan ownership in the UK (Newby et al., 2017; Asthma UK, 2020), and the patient information website, the invitation letters, and the posters for use in primary care practices may encourage asthma action plan ownership. With regard to the posters, following the qualitative interviews, we made refinements to the posters to highlight the seriousness of asthma. Recent qualitative work with those living with asthma in the UK has found that perceptions about how serious asthma can be are variable, and that seriousness may not be apparent until an admission to hospital or the experience of a severe attack (Apps et al., 2019). By highlighting the seriousness of asthma, as suggested by our participants currently living with asthma, this may encourage asthma self-management.
Strengths and limitations
A major strength of the work was following guidance on how to develop complex interventions to improve health and healthcare (O’Cathain et al., 2019) and the use of a mixed-method design to elicit feedback from participants (e.g. interviews with both adults and children/young people, and a survey). An additional strength was directly involving those currently living with asthma in the UK, who will be receiving support from their primary care provider. Although we only interviewed ten adults and seven children, we also had input from 95 respondents to the survey and interpretation and advice was provided by the PPI colleagues (n = 4). Further, healthcare professionals were not interviewed or surveyed as part of patient resource development, although the IMP2ART team includes healthcare professionals, and the Professional Advisory Group who contributed to the design and development of the resources is made up of GPs, nurses and pharmacists currently working in primary care.
A further strength is that the iterative methodology allowed for adaptation, for example, adding information to the website about the pandemic and updating all the resources to consider remote consulting. This adaptability has continued as we have added new resources to reflect topical issues such as the switch to dry powder devices in response to zero carbon initiatives. In the future, a change in resources may be needed if UK guidelines change to recommend ‘as required’ combination inhalers.
Practice implications
The IMP2ART strategy (incorporating the patient resources, as well as professional training and organisational resources) is now being tested in a UK-wide cluster RCT (ref: ISRCTN15448074), evaluating implementation (action plan ownership) and health outcomes (unscheduled care). We will track patient information website usage during the trial using Google Analytics, and the process evaluation (Sheringham et al., 2024) will include qualitative discussions with general practice teams that will explore invitation letter and poster usage. It is anticipated that the IMP2ART-developed patient resources will encourage patients to attend their annual asthma reviews (invitation letters); encourage patients to enquire about asthma plan ownership at their general practice (posters); and equip patients with the knowledge to successfully manage their asthma (information website).
Conclusions
We conclude that a multi-stage development process, following guidance on how to develop complex interventions to improve health and healthcare (O’Cathain et al., 2019), contributed to the design and development of the patient resources. Theoretical considerations, multidisciplinary team discussions, and the advice of PPI and professional colleagues, informed the initial development; and mixed-method feedback enabled refinement.
Acknowledgements
We acknowledge all members of the IMP2ART group for their contributions including Brian McKinstry, Aziz Sheikh (University of Edinburgh); Sandra Eldridge, Chris Griffiths, Chris Newby (Queen Mary University of London); Steven Julious (University of Sheffield); Deborah Fitzsimmons (University of Swansea); Ann-Louise Caress (University of Huddersfield). Dr Susan Morrow was Programme Manager during early stages of this work; Emily Healy and Lesley Gardner provided invaluable administrative support.
We are grateful to members of the IMP2ART Primary Care Respiratory Society Professional Advisory Group, coordinated by Dr Steve Holmes, and to the IMP2ART Patient and Public Involvement Group, co-ordinated by Dr Tracy Jackson. We thank the primary care general practices that participated in this study. We acknowledge the helpful advice of the Independent Programme Steering Committee chaired by Professor Robbie Foy.
Funding statement
This work was supported by the National Institute for Health and Care Research (NIHR) Programme Grants for Applied Research (RP-PG-1016-20008). The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care.
Competing interests
The authors declare that there are no conflicts of interest.
Ethics standards
The study was undertaken in 2018–2020 with ethics approval from West Midlands – Black Country Research Ethics Committee (REC ref: 18/WM/0300), NHS governance approvals from Health Research Authority (ref: IRAS 249302), and the Usher Research Ethics Group (UREG) at the University of Edinburgh. The trial sponsor was the Academic and Clinical Central Office for Research and Development (ACCORD), The University of Edinburgh and NHS Lothian Health Board.
References
- Apps LD, Chantrell S, Majd S, Eglinton E, Singh SJ, Murphy AC, Bradding P, Green RH, Hudson N and Evans RA (2019) Patient perceptions of living with severe asthma: challenges to effective management. The Journal of Allergy and Clinical Immunology: In Practice 7, 2613–2621. [DOI] [PubMed] [Google Scholar]
- Asthma UK (2020) Annual Asthma Survey 2020. Retrieved 28 February 2023 from https://www.asthma.org.uk/65fe870b/contentassets/927811d182034c45bebeb56824a023bf/aas-2020_2a-1.pdf
- British Thoracic Society, Research Unit of the Royal College of Physicians of London, King’s Fund Centre and National Asthma Campaign (1990) Guidelines for management of asthma in adults: I-chronic persistent asthma. BMJ 301, 651–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- British Thoracic Society/Scottish Intercollegiate Guideline Network (2019) British guideline on the management of asthma. Retrieved 23 January 2023 from https://www.brit-thoracic.org.uk/document-library/guidelines/asthma/btssign-guideline-for-the-management-of-asthma-2019
- Daines L, Morrow S, Wiener-Ogilvie S, Scott C, Steed L, Taylor SJ and Pinnock H (2020) Understanding how patients establish strategies for living with asthma: a qualitative study in UK primary care as part of IMP2ART. British Journal of General Practice 70, e303–e311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Global Initiative for Asthma (2022) Global strategy for asthma management and prevention. Retrieved 7 November 2022 from www.ginasthma.org
- Hodkinson A, Bower P, Grigoroglou C, Zghebi SS, Pinnock H, Kontopantelis E and Panagioti M (2020) Self-management interventions to reduce healthcare utilisation and improve quality of life among patients with asthma: a systematic review and network meta-analysis. BMJ 370, m2521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong ML, Armour C, LeMay K and Smith L (2013) Information needs of people with asthma. International Journal of Pharmacy Practice 22, 178–185. [DOI] [PubMed] [Google Scholar]
- McClatchey K, Hammersley V, Steed L, Sheringham J, Marsh V, Barat A, Delaney B, Hamborg T, Fitzsimmons DF, Holmes S and Jackson T (2023) IMPlementing IMProved Asthma self-management as RouTine (IMP2ART) in primary care: study protocol for a cluster randomised controlled implementation trial. Trials 24, 252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClatchey K, Jackson T, Delaney B, Morgan N, Pinnock H and Chan AH (2021) COVID-19 information for people living with asthma: a rapid review of publicly available information. The Journal of Allergy and Clinical Immunology: In Practice 9, 2070–2072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michie S, van Stralen MM and West R (2011) The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implementation Science 6, 42. doi: 10.1186/1748-5908-6-42. PMID: 21513547; PMCID: PMC3096582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, Eccles MP, Cane J and Wood CE (2013) The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Annals of Behavioral Medicine 46, 81–95. 10.1007/s12160-013-9486-6 [DOI] [PubMed] [Google Scholar]
- Miles C, Arden-Close E, Thomas M, Bruton A, Yardley L, Hankins M and Kirby SE (2017) Barriers and facilitators of effective self-management in asthma: systematic review and thematic synthesis of patient and healthcare professional views. NPJ Primary Care Respiratory Medicine 27, 57. 10.1038/s41533-017-0056-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrow S, Daines L, Wiener-Ogilvie S, Steed L, McKee L, Caress AL, Taylor SJC and Pinnock H (2017) Exploring the perspectives of clinical professionals and support staff on implementing supported self-management for asthma in UK general practice: an IMP2ART qualitative study. NPJ Primary Care Respiratory Medicine 27, 45. doi: 10.1038/s41533-017-0041-y. PMID: 28720751; PMCID: PMC5515882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukherjee M, Stoddart A, Gupta RP, Nwaru BI, Farr A, Heaven M, Fitzsimmons D, Bandyopadhyay A, Aftab C, Simpson CR, Lyons RA, Fischbacher C, Dibben C, Shields MD, Phillips CJ, Strachan DP, Davies GW, McKinstry B and Sheikh A (2016) The epidemiology, healthcare and societal burden and costs of asthma in the UK and its member nations: analyses of standalone and linked national databases. BMC Medicine 14, 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newby C, Wright N, Eldridge S, Morrow S, Vince-Lawer E, Appiagyei F, Hjelmbjerg T, Skinner D, Price D, Taylor SJ and Pinnock H (2017) Estimating exacerbation rates from routine UK primary care data: an exploratory validation from the IMP2ART programme. European Respiratory Journal 50(suppl 61), PA1603. doi: 10.1183/1393003.congress-2017.PA1603 [DOI] [Google Scholar]
- NHS Confederation (2003) British Medical Association new GMS contract 2003: investing in general practice. London.
- NICE guideline [NG80] (2021) Asthma: diagnosis, monitoring and chronic asthma management. Retrieved 7 November 2022 from https://www.nice.org.uk/guidance/ng80
- O’Cathain A, Croot L, Duncan E, Rousseau N, Sworn K, Turner KM, Yardley L and Hoddinott P (2019) Guidance on how to develop complex interventions to improve health and healthcare. BMJ open 9, e029954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearce G, Parke HL, Pinnock H, Epiphaniou E, Bourne CL, Sheikh A and Taylor SJ (2016) The PRISMS taxonomy of self-management support: derivation of a novel taxonomy and initial testing of its utility. Journal of Health Services Research & Policy 21, 73–82. [DOI] [PubMed] [Google Scholar]
- Pinnock H, Parke HL, Panagioti M, Daines L, Pearce G, Epiphaniou E, Bower P, Sheikh A, Griffiths CJ and Taylor SJ (2017) Systematic meta-review of supported self-management for asthma: a healthcare perspective. BMC Medicine 15, 1–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritchie J and Spencer L (1994) Qualitative data analysis for applied policy research. In Bryman A and Burgess R, editors, Analyzing Qualitative Data. London: Routledge, 173–194. 10.4324/9780203413081_chapter_9 [DOI] [Google Scholar]
- Royal College of Physicians (2014) Why asthma still kills: the National Review of Asthma Deaths (NRAD) confidential enquiry report. London, RCP. https://www.rcplondon.ac.uk/projects/outputs/why-asthma-still-kills
- Sbaffi L and Rowley J (2017) Trust and credibility in web-based health information: a review and agenda for future research. Journal of Medical Internet Research 19, e218. doi: 10.2196/jmir.7579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheringham J, Steed L, McClatchey K, Delaney B, Barat A, Hammersley V, Marsh V, Fulop NJ, Taylor SJ and Pinnock H (2024) Understanding the processes underpinning IMPlementing IMProved Asthma self-management as RouTine (IMP2ART) in primary care: study protocol for a process evaluation within a cluster randomised controlled implementation trial. Trials 25, 1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steed L, Sheringham J, McClatchey K, Hammersley V, Marsh V, Morgan N, Jackson T, Holmes S, Taylor SJC and Pinnock H (2023) IMP2ART: development of a multi-level programme theory integrating the COM-B model and the iPARIHS framework, to enhance implementation of supported self-management of asthma in primary care. Implementation Science Communications 4, 136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor SJC, Pinnock H, Epiphaniou E, Pearce G and Parke H (2014) A rapid synthesis of the evidence on interventions supporting self-management for people with long-term conditions. (PRISMS Practical Systematic Review of Self-Management Support for long-term conditions). Health Services and Delivery Research 2, 54. [PubMed] [Google Scholar]