Abstract
Background
Factors affecting time to lung cancer care may occur at multiple levels of influence. Mixed-methods reviews provide an approach for collectively synthesizing both quantitative and qualitative data. Prior reviews on timeliness of lung cancer care have included only either quantitative or qualitative data, been agnostic of the multilevel nature of influencing factors, or focused on a single factor such as gender or socioeconomic inequalities.
Objective
We aimed to update the literature on systematic reviews and identify multilevel factors associated with delays in lung cancer screening, diagnosis, and treatment.
Design
The proposed systematic review will be conducted in accordance with the Joanna Briggs Institute (JBI) Manual for Evidence Synthesis specific for mixed methods systematic reviews. Reporting will be consistent with PRISMA guidelines.
Methods
Medline (PubMed), CINAHL, and SCOPUS will be searched using validated search terms for lung cancer and factors, health disparities and time/delay. Eligible studies will include original articles with quantitative, qualitative, or mixed-methods designs that investigate health disparities in, risk factors for, or barriers to timely screening, confirmatory diagnosis, or treatment among patients with lung cancer or those at risk for lung cancer. Title, abstract, and full-text screening, study quality assessment, and data extraction will be conducted by two reviewers. A convergent integrated approach with thematic synthesis will be applied to synthesize the extracted and generated analytical themes.
Discussion
Findings from this review will inform the design of an intervention to address delays in lung cancer screening for high-risk persons, diagnosis of suspected lung cancer, and treatment of confirmed cases.
Introduction
Lung cancer is the second most common cancer in both men and women and the leading cause of cancer mortality in the US [1, 2]. Five-year survival for patients with lung cancer is 25% ranging from 7% to 63% for late-stage vs early stage diagnoses [3]. Only 16% of lung cancers are diagnosed early [4], and the wait time to initiation of appropriate treatment following from initial suspicion of lung cancer may be long [5–14]. Delayed treatment, particularly treatment with curative intent, has also been shown to be associated with poor survival [5, 7, 15–19]. Delays occur at multiple stages along the lung cancer care pathway that cumulatively prevent the timely receipt of lifesaving treatment. Intervals of delay include cues to screening, diagnostic work-up following a positive screen, and time taken to initiate treatment. These delays are potentially preventable and can be targets for intervention to improve lung cancer outcomes.
Factors affecting time to lung cancer care occur at multiple, expanding spheres of influence, ranging from the micro or individual level to the macro or societal level. According to Taplin’s ecological framework, the levels of influence occur at the individual, family/social support, provider/team, organization/practice setting, and environment which are identified as levels of contextual influence that affect behaviors along the cancer care continuum [20, 21]. These multilevel factors could potentially interact, increasing their influence on timeliness of receiving care. For example, in the US, non-Hispanic Blacks and Hispanics are more likely than non-Hispanic Whites to live below the poverty line [22], and the interaction of race/ethnicity and poverty status has implications for access to and timeliness of receiving cancer care [23, 24]. Furthering the example, racial/ethnic minorities, particularly Blacks, have been shown to exhibit some mistrust of the health system. The interaction of race/ethnicity and medical mistrust, at the health system level, can also lead to delays in receiving cancer care by affecting the quality of communication between providers and their patients with lung cancer [25]. Such interaction among factors requires multilevel interventions (MLIs) to address both proximal determinants of the problem at their various levels of influence and achieve distal outcomes.
Although prior reviews have been conducted on the timeliness of receiving lung cancer care, these had some limitations. In a systematic review by Cassim et al. of qualitative studies on barriers to early diagnosis of lung cancer, identified barriers were classified into disease, patient, and healthcare and system factors [26]. A different review of quantitative studies identified individual (age, comorbidity, and atypical symptoms at presentation in a hospital setting) and health system factors (treatment intent, type of physician at initial referral, number of diagnostic tests, and number of facilities involved) [27]. Other reviews on timeliness of receiving lung cancer care have been either agnostic of the multilevel nature of influencing factors [27–30] or focused on a single factor such as gender [31] or socioeconomic inequalities [32]. They also included studies from different countries and were restricted to only qualitative or quantitative studies, which have implications both for the contextualization of findings across different geographic areas and also for the breadth of synthesized evidence across study designs.
Mixed-methods systematic reviews provide an approach for collectively synthesizing both quantitative and qualitative data. Considering that previous systematic reviews were limited to either only quantitative or qualitative data and/or had an international scope, a mixed-methods systematic review on multilevel factors affecting the timeliness of receiving lung cancer care in the US will provide a timely and comprehensive update. A comprehensive understanding of the contextual factors that influence the timeliness of lung cancer care at the various levels of influence will inform the design of MLIs to reduce time to receipt of care along the care continuum. Such interventions will ultimately improve outcomes for patients with lung cancer.
Objectives
The objective of this systematic review is to identify multilevel factors associated with delays experienced by patients along the lung cancer care continuum from screening to diagnosis and treatment in the US. To achieve this, we propose to address the following aims:
To identify the multilevel factors associated with delays in lung cancer screening in the US
To identify the multilevel factors associated with delays in lung cancer diagnosis in the US
To identify the multilevel factors associated with delays in lung cancer treatment in the US
Materials and methods
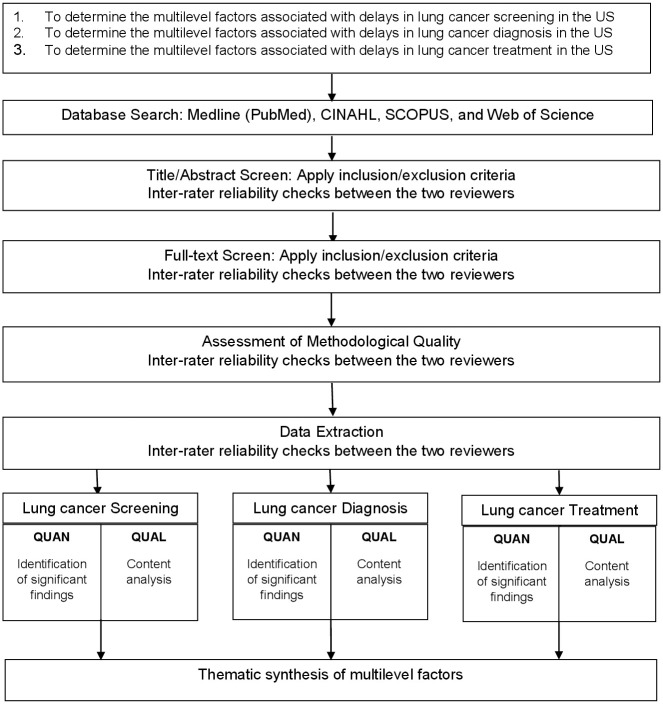
The proposed systematic review will be conducted in accordance with the Joanna Briggs Institute (JBI) Manual for Evidence Synthesis specific for mixed methods systematic reviews (Fig 1) [33]. Reporting will be conform to the Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA) guidelines [34]. The protocol for the proposed study is registered with PROSPERO (CRD42022346097).
Fig 1. Mixed-method systematic review design flow chart.
QUAN = Quantitative data; QUAL = Qualitative data.
Outcomes
Our outcome of interest is delay in receipt of lung cancer care and includes: 1) delay in screening for lung cancer; 2) delay in diagnosis of lung cancer; and 3) delay in receipt of lung cancer treatment. Delay is defined based on the time intervals between two points along the cancer care continuum or wait times to receive care and could include non-receipt, refusal or failure to follow-up on provider recommendation for care.
Informational sources and search strategy
The following databases will be searched from inception for published studies in the literature–Medline (PubMed), CINAHL, and SCOPUS–using validated search terms lung cancer [35] and terms specific for factors [36], health disparities [37] and time/delay [27, 32, 38, 39] adapted from prior reviews for the four databases (Table 1) [40].
Table 1. MEDLINE (PubMed) search strategy.
| S/N | Search Terms |
|---|---|
| 1 | ((Lung neoplasms[mh:noexp] OR bronchial neoplasms[mh] or pancoast syndrome[mh] or lung cancer*[tw]) AND humans[sb]) OR (NSCLC[ti] OR SCLC[ti] OR (pancoast[ti] AND (syndrome[ti] OR tumor*[ti] OR tumour*[ti])) OR ((lung*[ti] OR pulmonary[ti] OR bronchus[ti] OR bronchogenic[ti] OR bronchial[ti] OR bronchoalveolar[ti] OR bronchioalveolar[ti] OR bronchioloalveolar[ti]) AND (cancer*[ti] OR carcinoma*[ti] OR adenocarcinoma*[ti] OR malignan*[ti] OR metastas*[ti] OR tumor*[ti] OR tumour*[ti] OR neoplasm*[ti])) NOT medline[sb]) NOT (meta analysis[pt] OR meta analysis[tiab] OR meta analysis[mh] OR review[pt] OR search*[tiab])AND English[la] |
| 2 | Healthcare Disparities/ OR Health Equity/ OR Health Status Disparities/ OR Culturally Competent Care/ OR Social Determinants of Health/ OR Sociology, Medical/ |
| 3 | (disadvantaged[tiab] OR discriminat*[tiab] OR disparat*[tiab] OR disparit*[tiab] OR disproportion*[tiab] OR inequal*[tiab] OR inequit*[tiab] OR unequal[tiab] OR underserved[tiab] OR under-served[tiab] OR (cultural* adj compet*[tiab]) OR (social* adj determin*[tiab])) OR (difference[ti] OR different[ti]) |
| 4 | predict*[ti] OR barrier*[ti] OR challeng*[ti] OR factor[ti] OR factors[ti] OR determine*[ti] OR relationship*[ti] |
| 5 | time factors[MeSH] OR waiting lists[MeSH] OR delay[tw] OR Timeliness[tw] OR Time[tw] OR prognosis[MeSH] |
| 6 | delay*[tiab] OR interval*[tiab] OR time*[tiab] OR pathway*[tiab] OR route*[tiab] OR wait*[tiab] OR timeline[tiab] OR timeliness[tiab] OR timeframe[tiab] OR period[tiab] OR periods[tiab] OR latency[tiab] OR late[tiab] OR lateness[tiab] |
| 7 | #2 OR #3 OR #4 |
| 8 | #5 OR #6 |
| 9 | #1 AND #7 AND #8 |
Eligibility criteria
Eligible studies will be original articles with quantitative, qualitative, or mixed-methods designs that investigate health disparities in, risk factors for, or barriers to timely screening, confirmatory diagnosis, or treatment among patients with lung cancer or those at risk for lung cancer. Studies that investigate factors associated with whether or not patients receive lung cancer care will also be included as non-receipt of care is also indicative of delays along the cancer care continuum. To contextualize synthesized findings within the environment in which the factors affecting lung cancer care are experienced, included studies will be restricted to primary studies conducted in the US with full-text articles published in English. Letters to the editor, editorials, and commentaries will be excluded. The identified study titles and abstracts will be screened against the selection criteria by two independent reviewers for relevance. Selected studies will be retrieved in full and undergo full-text screening by two independent reviewers based on inclusion criteria. Reasons for excluded studies will be documented. Disagreements will be resolved through discussion. In the event that consensus is not reached, input will be sought from a third reviewer to resolve the discrepancy.
Quality assessment
Methodological quality will be assessed by two independent reviewers using the NIH Quality Assessment Tool for quantitative studies [41] and the Consolidated Criteria for Reporting Qualitative Research checklist for qualitative studies [42]. Disagreements will be resolved through discussion. The NIH Quality Assessment Tool is a collection of tools developed by the National Heart, Lung, and Blood Institute and assesses the internal validity of a study. This tool(s) offers the advantage of assessing multiple studies based on different quantitative research designs including intervention studies, observational cohort and cross-sectional studies, case-control studies, pre-post studies with no control group, and case series studies. Consistent with guidelines from the NIH Quality Assessment Tool, the overall quality rating will be based on the totality of flaws identified.
Evidence synthesis
Data extraction
Qualitative and quantitative data will be extracted from the full-text of the included studies using JBI data extraction tool adapted for a spreadsheet (S1 File). Article related data will be extracted including study-reference (authors’ names, publication year) and context (setting in which study is conducted). Study type and methodology will be extracted, along with participant data: age, gender, LGBTQ+ status, race, ethnicity, socioeconomic status, disability status, rurality, Appalachian status, and number. Phenomena of interest include health disparities (for studies that identify disparate groups that experience delays to lung cancer care), risk factors (for studies that identify predictors of delays in receiving lung cancer care), and barriers (for studies that identify reasons for delays to lung cancer care). Time to lung cancer screening, diagnosis, and treatment as well as risk factors/barriers identified will also be noted. In addition, consistent with the JBI SUMARI tool, qualitative studies will include themes supported by illustrations, along with level of credibility [33]. Disagreements will be resolved through discussion.
Data transformation
Results from quantitative data will be transformed into ‘qualitized data’ [43]. This will involve transformation of quantitative data into textual descriptions using narrative synthesis to describe factors with significant findings (p < 0.05) along with the relevant numerical data. Thus, this qualitized data will be integrated with qualitative data for the overall systematic review.
Data synthesis and integration
JBI discusses a number of possibilities for the management of mixed methods data in order to be able to validate or triangulate qualitative and quantitative findings [33]. Because our approach captures and analyzes data at the same time, and the qualitative and quantitative data will be used to answer the same questions about delays in care, we will utilize a convergent [44] integrated [45] approach for mixed methods systematic reviews. As noted by JBI methodology for mixed methods systematic reviews, we will combine the qualitized data with the qualitative data for analysis so that all extracted data are in qualitative form. The combined extracted data will be synthesized using thematic synthesis [46]. The thematic synthesis will be conducted by two reviewers. Any disagreements will be reconciled by discussion.
First, free codes will be generated based on verbatim findings from the qualitative studies and qualitized data from the quantitative studies. The free codes would then be grouped hierarchically to develop descriptive themes. Analytical themes that answer the research question on factors associated with lung cancer care would then be generated. The analytical themes will be categorized based on Taplin’s ecological framework for improving cancer care quality and outcomes– 1) individual, 2) family/social support, 3) provider/team, 4) organization/practice setting, and 5) environment [21]. Results will be presented by textual discussion of the analytical themes as well as the graphical presentation of the ecological framework.
Discussion
This systematic review will provide a comprehensive synthesis of the evidence on factors that contribute to delays in receiving health services along the lung cancer care continuum. Our multi-level approach will not only explore important individual factors, but it will also examine the impact of the interaction of different factors, and these factors may interact at a single or multi-level. Our theoretical framework promises to shed light on the sometimes confusing array of factors identified in individual studies and collect them to help to be comprehensive and perhaps disambiguate the contribution of single and multiple factors. This ecological framework can also help situate the issue of health disparities in lung cancer outcomes within a broader context of social and environmental factors which may contribute to diagnostic and treatment delays.
Utilization of a mixed method approach allows for the identification of these factors as well as the context in which the factors might influence timeliness of care. By including both qualitative and quantitative data, we will be able to triangulate and provide a more convincing picture of the association of different factors, such as medical mistrust, stigma, and access, to our lung cancer outcomes of interest: delays which affect the morbidity and mortality of diverse populations in the US. Ultimately, findings from this review will inform the design of an MLI to address delays in lung cancer screening for high-risk persons, diagnosis of suspected lung cancer, and treatment of confirmed cases. It will also inform cancer care providers and managers seeking to make quality improvement in the process of care.
Dissemination of information
Findings will be disseminated at a cancer-focused research meeting with at least one peer-reviewed publication in a health journal.
Supporting information
(DOC)
(XLSX)
Data Availability
No datasets was generated or analysed during the preparation of the protocol.
Funding Statement
Funding for this work was provided to Sabina Nduaguba as a subgrant from the National Cancer Institute (NCI) Geographic Management of Cancer Health Disparities Program (GMaP, http://gmapr1.com/). The grant number is: P30 CA177558-10S1. GMaP played no role in the study design, decision to publish, or preparation of the manuscript.
References
- 1.GBD 2019 Cancer Collaborators. Cancer Incidence, Mortality, Years of Life Lost, Years Lived with Disability, and Disability-Adjusted Life Years for 29 Cancer Groups from 2010 to 2019: A Systematic Analysis of Cancer Burden Globally, Nationally, and by Socio-Demographic Index for the Global Burden of Disease Study 2019. JAMA Oncology. doi: 10.1001/jamaoncol.2021.6987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72(1):7–33. doi: 10.3322/caac.21708 [DOI] [PubMed] [Google Scholar]
- 3.Howlader N, Noone AM, Krapcho M, Miller D, Brest A, Yu M, et al. SEER Cancer Statistics Review, 1975–2017. Bethesda, MD: National Cancer Institute; 2020. [Google Scholar]
- 4.American Lung Association. Lung Cancer Fact Sheet 2022. https://www.lung.org/lung-health-diseases/lung-disease-lookup/lung-cancer/resource-library/lung-cancer-fact-sheet. Accessed August 11, 2024.
- 5.Heiden BT, Eaton DB Jr., Engelhardt KE, Chang SH, Yan Y, Patel MR, et al. Analysis of Delayed Surgical Treatment and Oncologic Outcomes in Clinical Stage I Non-Small Cell Lung Cancer. JAMA Netw Open. 2021;4(5):e2111613. doi: 10.1001/jamanetworkopen.2021.11613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alsamarai S, Yao X, Cain HC, Chang BW, Chao HH, Connery DM, et al. The effect of a lung cancer care coordination program on timeliness of care. Clin Lung Cancer. 2013;14(5):527–34. doi: 10.1016/j.cllc.2013.04.004 [DOI] [PubMed] [Google Scholar]
- 7.Haque N, Raza A, McGoey R, Boulmay B, Diethelm L, Kantrow S. Small cell lung cancer: time to diagnosis and treatment. South Med J. 2012;105(8):418–23. doi: 10.1097/SMJ.0b013e3182601198 [DOI] [PubMed] [Google Scholar]
- 8.Hunnibell LS, Rose MG, Connery DM, Grens CE, Hampel JM, Rosa M, et al. Using nurse navigation to improve timeliness of lung cancer care at a veterans hospital. Clin J Oncol Nurs. 2012;16(1):29–36. doi: 10.1188/12.CJON.29-36 [DOI] [PubMed] [Google Scholar]
- 9.Gould MK, Ghaus SJ, Olsson JK, Schultz EM. Timeliness of care in veterans with non-small cell lung cancer. Chest. 2008;133(5):1167–73. doi: 10.1378/chest.07-2654 [DOI] [PubMed] [Google Scholar]
- 10.Yorio JT, Xie Y, Yan J, Gerber DE. Lung cancer diagnostic and treatment intervals in the United States: a health care disparity? J Thorac Oncol. 2009;4(11):1322–30. doi: 10.1097/JTO.0b013e3181bbb130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Albano D, Bilfinger T, Feraca M, Kuperberg S, Nemesure B. A Multidisciplinary Lung Cancer Program: Does It Reduce Delay Between Diagnosis and Treatment? Lung. 2020;198(6):967–72. doi: 10.1007/s00408-020-00404-8 [DOI] [PubMed] [Google Scholar]
- 12.Vidaver RM, Shershneva MB, Hetzel SJ, Holden TR, Campbell TC. Typical Time to Treatment of Patients With Lung Cancer in a Multisite, US-Based Study. J Oncol Pract. 2016;12(6):e643–53. doi: 10.1200/JOP.2015.009605 [DOI] [PubMed] [Google Scholar]
- 13.Phillips WW, Copeland J, Hofferberth SC, Armitage JR, Fox S, Kruithoff M, et al. Lung Cancer Strategist Program: A novel care delivery model to improve timeliness of diagnosis and treatment in high-risk patients. Healthc (Amst). 2021;9(3):100563. doi: 10.1016/j.hjdsi.2021.100563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maiga AW, Deppen SA, Pinkerman R, Callaway-Lane C, Massion PP, Dittus RS, et al. Timeliness of Care and Lung Cancer Tumor-Stage Progression: How Long Can We Wait? Ann Thorac Surg. 2017;104(6):1791–7. doi: 10.1016/j.athoracsur.2017.06.051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stokstad T, Sørhaug S, Amundsen T, Grønberg BH. Associations Between Time to Treatment Start and Survival in Patients With Lung Cancer. In Vivo. 2021;35(3):1595–603. doi: 10.21873/invivo.12416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gomez DR, Liao KP, Swisher SG, Blumenschein GR, Erasmus JJ Jr., Buchholz TA, et al. Time to treatment as a quality metric in lung cancer: Staging studies, time to treatment, and patient survival. Radiother Oncol. 2015;115(2):257–63. doi: 10.1016/j.radonc.2015.04.010 [DOI] [PubMed] [Google Scholar]
- 17.Mayne NR, Elser HC, Darling AJ, Raman V, Liou DZ, Colson YL, et al. Estimating the Impact of Extended Delay to Surgery for Stage I Non-small-cell Lung Cancer on Survival. Ann Surg. 2021;273(5):850–7. doi: 10.1097/SLA.0000000000004811 [DOI] [PubMed] [Google Scholar]
- 18.Wai ES, Mackinnon M, Hooker R, Moccia P, Perry KR, Truong PT. Wait times in diagnostic evaluation and treatment for patients with stage III non-small cell lung cancer in British Columbia. Am J Clin Oncol. 2012;35(4):373–7. doi: 10.1097/COC.0b013e3182143cce [DOI] [PubMed] [Google Scholar]
- 19.Cushman TR, Jones B, Akhavan D, Rusthoven CG, Verma V, Salgia R, et al. The Effects of Time to Treatment Initiation for Patients With Non-small-cell Lung Cancer in the United States. Clin Lung Cancer. 2021;22(1):e84–e97. doi: 10.1016/j.cllc.2020.09.004 [DOI] [PubMed] [Google Scholar]
- 20.Taplin SH, Rodgers AB. Toward improving the quality of cancer care: addressing the interfaces of primary and oncology-related subspecialty care. J Natl Cancer Inst Monogr. 2010;2010(40):3–10. doi: 10.1093/jncimonographs/lgq006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Taplin SH, Anhang Price R, Edwards HM, Foster MK, Breslau ES, Chollette V, et al. Introduction: Understanding and influencing multilevel factors across the cancer care continuum. J Natl Cancer Inst Monogr. 2012;2012(44):2–10. doi: 10.1093/jncimonographs/lgs008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.United States Census Bureau. Income and Poverty in the United States: 2020. 2021. https://www.census.gov/library/publications/2021/demo/p60-273.html.
- 23.Ortiz SE, Segel JE, Tran LM. Health Savings Plans and Disparities in Access to Care by Race and Ethnicity. Am J Prev Med. 2021;61(2):e81–e92. doi: 10.1016/j.amepre.2021.02.020 [DOI] [PubMed] [Google Scholar]
- 24.Leslie TF, Frankenfeld CL, Menon N. Disparities in colorectal cancer time-to-treatment and survival time associated with racial and economic residential segregation surrounding the diagnostic hospital, Georgia 2010–2015. Cancer Epidemiol. 2022;81:102267. doi: 10.1016/j.canep.2022.102267 [DOI] [PubMed] [Google Scholar]
- 25.Cuevas AG, O’Brien K, Saha S. African American experiences in healthcare: "I always feel like I’m getting skipped over". Health Psychol. 2016;35(9):987–95. doi: 10.1037/hea0000368 [DOI] [PubMed] [Google Scholar]
- 26.Cassim S, Chepulis L, Keenan R, Kidd J, Firth M, Lawrenson R. Patient and carer perceived barriers to early presentation and diagnosis of lung cancer: a systematic review. BMC Cancer. 2019;19(1):25. doi: 10.1186/s12885-018-5169-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Olsson JK, Schultz EM, Gould MK. Timeliness of care in patients with lung cancer: a systematic review. Thorax. 2009;64(9):749–56. doi: 10.1136/thx.2008.109330 [DOI] [PubMed] [Google Scholar]
- 28.Doubeni CA, Gabler NB, Wheeler CM, McCarthy AM, Castle PE, Halm EA, et al. Timely follow-up of positive cancer screening results: A systematic review and recommendations from the PROSPR Consortium. CA Cancer J Clin. 2018;68(3):199–216. doi: 10.3322/caac.21452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jacobsen MM, Silverstein SC, Quinn M, Waterston LB, Thomas CA, Benneyan JC, et al. Timeliness of access to lung cancer diagnosis and treatment: A scoping literature review. Lung Cancer. 2017;112:156–64. doi: 10.1016/j.lungcan.2017.08.011 [DOI] [PubMed] [Google Scholar]
- 30.Malalasekera A, Blinman PL, Dhillon HM, Stefanic NA, Grimison P, Jain A, et al. Times to Diagnosis and Treatment of Lung Cancer in New South Wales, Australia: A Multicenter, Medicare Data Linkage Study. J Oncol Pract. 2018;14(10):e621–e30. doi: 10.1200/JOP.18.00125 [DOI] [PubMed] [Google Scholar]
- 31.Rana RH, Alam F, Alam K, Gow J. Gender-specific differences in care-seeking behaviour among lung cancer patients: a systematic review. J Cancer Res Clin Oncol. 2020;146(5):1169–96. doi: 10.1007/s00432-020-03197-8 [DOI] [PubMed] [Google Scholar]
- 32.Forrest LF, Sowden S, Rubin G, White M, Adams J. Socio-economic inequalities in stage at diagnosis, and in time intervals on the lung cancer pathway from first symptom to treatment: systematic review and meta-analysis. Thorax. 2017;72(5):430–6. doi: 10.1136/thoraxjnl-2016-209013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lizarondo L, Stern C, Carrier J, Godfrey C, Rieger K, Salmond S, et al. Chapter 8: Mixed methods systematic reviews. JBI Manual for Evidence Synthesis 2020. [DOI] [PubMed] [Google Scholar]
- 34.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.CareSearch. Lung Cancer PubMed Searches. 2021. https://www.caresearch.com.au/tabid/6874/Default.aspx. Accessed August 11, 2024.
- 36.Gellad WF, Grenard JL, Marcum ZA. A systematic review of barriers to medication adherence in the elderly: looking beyond cost and regimen complexity. Am J Geriatr Pharmacother. 2011;9(1):11–23. doi: 10.1016/j.amjopharm.2011.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mackey K, Ayers CK, Kondo KK, Saha S, Advani SM, Young S, et al. Racial and Ethnic Disparities in COVID-19-Related Infections, Hospitalizations, and Deaths: A Systematic Review. Ann Intern Med. 2021;174(3):362–73. doi: 10.7326/M20-6306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhang J, IJ MJ, Oberoi J, Karnchanachari N, Bergin RJ, Franchini F, et al. Time to diagnosis and treatment of lung cancer: A systematic overview of risk factors, interventions and impact on patient outcomes. Lung Cancer. 2022;166:27–39. doi: 10.1016/j.lungcan.2022.01.015 [DOI] [PubMed] [Google Scholar]
- 39.Malalasekera A, Nahm S, Blinman PL, Kao SC, Dhillon HM, Vardy JL. How long is too long? A scoping review of health system delays in lung cancer. Eur Respir Rev. 2018;27(149). doi: 10.1183/16000617.0045-2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Institute for Evidence-Based Healthcare. Systematic Review Accelerator. 2022. https://sr-accelerator.com/#/polyglot. Accessed August 11, 2024.
- 41.National Institutes of Health. Study Quality Assessment Tools. 2021. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools. Accessed August 11, 2024.
- 42.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57. doi: 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- 43.Onwuegbuzie AJ, Leech NL. Qualitizing Data. The Routledge Reviewer’s Guide to Mixed Methods Analysis2021.
- 44.Hong QN, Pluye P, Bujold M, Wassef M. Convergent and sequential synthesis designs: implications for conducting and reporting systematic reviews of qualitative and quantitative evidence. Syst Rev. 2017;6(1):61. doi: 10.1186/s13643-017-0454-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sandelowski M, Voils CI, Barroso J. Defining and Designing Mixed Research Synthesis Studies. Res Sch. 2006;13(1):29. [PMC free article] [PubMed] [Google Scholar]
- 46.Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8:45. doi: 10.1186/1471-2288-8-45 [DOI] [PMC free article] [PubMed] [Google Scholar]