Abstract
Background:
We quantify the mortality burden and economic loss attributable to nonoptimal temperatures for cold and heat in the Central and South American countries in the Multi-City Multi-Country (MCC) Collaborative Research Network.
Methods:
We collected data for 66 locations from 13 countries in Central and South America to estimate location-specific temperature–mortality associations using time-series regression with distributed lag nonlinear models. We calculated the attributable deaths for cold and heat as the 2.5th and 97.5th temperature percentiles, above and below the minimum mortality temperature, and used the value of a life year to estimate the economic loss of delayed deaths.
Results:
The mortality impact of cold varied widely by country, from 9.64% in Uruguay to 0.22% in Costa Rica. The heat-attributable fraction for mortality ranged from 1.41% in Paraguay to 0.01% in Ecuador. Locations in arid and temperate climatic zones showed higher cold-related mortality (5.10% and 5.29%, respectively) than those in tropical climates (1.71%). Arid and temperate climatic zones saw lower heat-attributable fractions (0.69% and 0.58%) than arid climatic zones (0.92%). Exposure to cold led to an annual economic loss of $0.6 million in Costa Rica to $472.2 million in Argentina. In comparison, heat resulted in economic losses of $0.05 million in Ecuador to $90.6 million in Brazil.
Conclusion:
Most of the mortality burden for Central and South American countries is caused by cold compared to heat, generating annual economic losses of $2.1 billion and $290.7 million, respectively. Public health policies and adaptation measures in the region should account for the health effects associated with nonoptimal temperatures.
Keywords: Nonoptimal temperatures, Mortality burden, Economic loss, Time series, Distributed lag nonlinear models, Multicountry, Central and South America
What this study adds:
This study provides evidence of the health burden and economic losses attributable to heat and cold in Central and South American countries, covering various climates and populations. Most of the mortality burden for Central and South American countries is caused by cold compared to heat. The results showed geographical and climatic variations, indicating a significantly higher impact of nonoptimal temperatures in countries of the Southern Cone and locations with temperate climates. These findings offer direct evidence to guide policymakers in developing public health policies for mitigation and adaptation to the region’s health effects and economic impacts of nonoptimal temperatures.
Introduction
Epidemiological studies have already provided significant evidence for the association between ambient temperature and mortality.1–5 However, most of the evidence for the temperature–mortality association comes from studies conducted in high-income countries.6 Climate change is currently a global concern, affecting vulnerable populations in low- and middle-income countries, including those in the Central and South American region. Moreover, the region is one of the most urbanized among developing countries,7 which may increase the impact of nonoptimum temperatures on the growing population.
Several studies examined the temperature–mortality association in the Central and South American countries. Multicity studies have been conducted nationwide in Brazil8 and Mexico,9 both reported effects of low and high temperatures on the risk of cardiovascular mortality and nonexternal and cause-specific mortality in the elderly, respectively. Bell et al10 also reported that elevated temperatures are associated with an increased risk of cardiovascular and respiratory mortality in a study conducted in three major South American cities (Sao Paulo, Santiago, and Mexico City). Moreover, a larger multicity study across Latin American cities reported that a substantial proportion of deaths is attributable to nonoptimal ambient temperatures, with the impact being much strongest for cold than for heat.11
Although previous studies have reported estimates of the attributable burden as an absolute or relative excess of deaths, exposure to nonoptimal temperatures also burdens the economy. However, the costs of health hazards have mainly been quantified economically in high-income countries,12–14 and evidence of the economic loss attributable to nonoptimal temperatures from middle and low-income countries, including Central and South American countries, is still unknown. Moreover, the Central and South American regions comprise a wide range of climatic conditions, from tropical rainforests to arid deserts, each presenting unique temperature-related health challenges. However, the health impact of nonoptimal temperatures according to the climatic zones in the region has not yet been addressed.
In this study, we aim to quantify the total mortality burden and economic losses attributable to the short-term associations of nonoptimal ambient temperatures and determine the relative contributions from cold and heat in the Central and South American countries within the Multi-City Multi-Country (MCC) Collaborative Research Network (http://mccstudy.lshtm.ac.uk/).
Methods
Data
We collected time-series daily data from 66 locations in 13 countries, Argentina (three cities, 2005–2015), Brazil (18 cities, 1997–2011), Chile (four cities, 2004–2014), Colombia (five cities, 1998–2013), Costa Rica (one city, 2000–2017), Ecuador (two cities, 2014–2018), Guatemala (one city, 2009–2016), Mexico (10 metropolitan areas, 1998–2014), Panama (one city, 2013–2016), Paraguay (one city, 2004–2016), Peru (18 regions, 2008–2014), Puerto Rico (one city, 2009–2016), and Uruguay (one city, 2012–2016), and three overseas territories of France (French Guiana, Guadalupe, and Martinique, 2005–2015). The data included observed daily mortality for all causes or nonexternal causes (International Classification of Diseases 9th Revision: 0-799, and 10th Revision: A00-R99) and daily mean temperature for each location.5 Additional details on data collection are provided in Appendix A; http://links.lww.com/EE/A300.
Statistical analysis
We followed the same two-stage procedure in a previous MCC study.2 In the first stage, distributed lag nonlinear models in quasi-Poisson regression were separately applied to each location. These models included a natural cubic B-spline of time with eight degrees of freedom per year to control long-term trends and seasonality, indicator variables of weekdays, and the cross-basis for daily mean temperature. The exposure–response curve in the cross-basis was modeled with a quadratic B-spline with internal knots placed at the 10th, 75th, and 90th centiles of location temperature distribution. The lag–exposure curve was defined with a natural cubic spline with three internal knots equally spaced in the log scale. In addition, the lag period was extended to 21 to capture the long delay in the effects of cold. Sensitivity analyses have thoroughly tested these modeling choices in previous studies, showing that the results were not dependent on modeling assumptions.2,3
In the second stage, location-specific estimates were pooled to represent the overall exposure–response relationship by cumulating risks during the lag period by country and climatic zone. A random-effects multilevel meta-analytical model was applied, including the average temperature and temperature range as meta-predictors and accounting for variations in risk nested across locations, countries, and climatic zones.15 We used this fitted meta-analytical model to derive the best linear unbiased predictions of the overall temperature–response association in each location. The best linear unbiased predictions can borrow information from the pooled associations within the same hierarchical level, thus providing more accurate estimates than the first-stage estimates in locations with small daily mortality counts or short time series.
The minimum mortality temperature (MMT) and the attributable deaths were derived from the best linear unbiased predictions of the overall cumulative exposure–response association in each location and country. The total attributable number of deaths caused by nonoptimum temperatures is given by the sum of the contributions from all the days of the series. Its ratio with the total number of deaths provides the total attributable fraction (AF).16 We calculated the components attributable to cold and heat, including extremely cold and hot temperatures, defined using cutoff values at the 2.5th and 97.5th temperature percentiles, above and below the MMT. Empirical confidence intervals (eCIs) for AFs were calculated using Monte Carlo simulations.16 The choice of these temperature percentiles was made to ensure comparability with a previous MCC study,2 during which data from South and Central American countries, except Brazil, was not available. Moreover, these percentiles have also been extensively used by others to define cold and heat effects.17–20
Economic assessment
Although it is common to use Value of a Statistical Life (VSL) to quantify the benefit of delaying a death, Armstrong et al4 provided strong evidence that most deaths associated in daily analyses with cold and heat are displaced by at least 1 year. Consequently, we used the Value of a Life Year (VOLY) in US dollars ($) to estimate the economic impact of the mortality burden attributable to cold and heat assuming a 1-year displacement. This can be considered as a conservative estimate of the economic impact of the mortality burden attributable to cold and heat. However, due to the lack of VSL and VOLY values related to nonoptimal temperature and to ensure comparability between countries, we relied on international income-adjusted estimates of the VSL21 to calculate country-specific VOLY values (Appendix B; http://links.lww.com/EE/A300). The economic assessment of cold and heat losses is the product of the number of delayed deaths and VOLY values averaged over the study period and population covered for each country and climatic zone.
Results
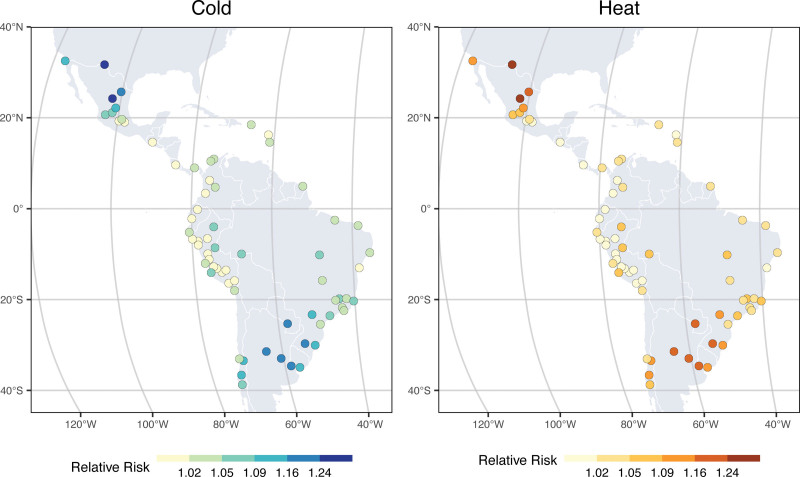
Table 1 shows the descriptive statistics from each country and climatic zone. The data included almost 10 million deaths in the countries included in the analysis. The country-specific annual average temperature ranged from 17.9 ºC in Peru to 28.1 ºC in Panama and from 19.0 ºC in locations with a temperate climate to 25.8 ºC in those in tropical climate. The temperature–mortality relationships were mostly J- or V-shaped, although some locations showed a plateau in the exposure–response curve with a large confidence interval for the MMT, suggesting adaptation to a wider range of moderate temperatures. Moreover, most of the locations in tropical climates showed almost flat exposure–response curves, basically not showing any association (Figure S1; http://links.lww.com/EE/A300). We observed the highest cold-related mortality risk over locations in Mexico and the Southern Cone (Argentina, Paraguay, and Uruguay). Although the mortality risk for heat risks was substantially lower than for cold, the highest heat-related mortality risks were also found in some locations in Mexico and Argentina (Figure 1).
Table 1.
Summary of the locations, study periods, number of deaths, and temperature distributions for the countries included in the study
| Locations | Study perioda | Total deaths | Temperature (°C); mean (range) | |
|---|---|---|---|---|
| Country | ||||
| Argentina | 3 | 2005–2015 | 686,333 | 18.2 (0.4 to 33.9) |
| Brazil | 18 | 1997–2018 | 3,895,158 | 23.4 (3.2 to 35.1) |
| Chile | 4 | 2004–2014 | 325,462 | 13.7 (−1.7 to 27.5) |
| Colombia | 5 | 1998–2013 | 956,539 | 23.4 (10.5 to 31.1) |
| Costa Rica | 1 | 2000–2017 | 31,117 | 22.7 (18.3 to 27.5) |
| Ecuador | 2 | 2014–2018 | 112,264 | 20.9 (10.1 to 30.2) |
| Guatemala | 1 | 2009–2016 | 62,715 | 19.4 (11.8 to 26.5) |
| Mexico | 10 | 1998–2014 | 2,980,086 | 18.8 (0.4 to 35.3) |
| Overseas France | 3 | 2000–2015 | 53,300 | 26.9 (21.8 to 30.4) |
| Panama | 1 | 2013–2016 | 11,457 | 28.1 (23.4 to 31.6) |
| Paraguay | 1 | 2004–2019 | 48,037 | 23.3 (5.6 to 35.1) |
| Peru | 18 | 2008–2014 | 633,137 | 17.9 (−0.2 to 30.7) |
| Puerto Rico | 1 | 2009–2016 | 26,564 | 26.8 (19.7 to 31.1) |
| Uruguay | 1 | 2012–2016 | 153,554 | 18.6 (5.6 to 33.5) |
| Climatic zoneb | ||||
| Tropical | 23 | 1,890,881 | 25.8 (11.8 to 35.1) | |
| Arid | 13 | 1,107,450 | 19.7 (0.4 to 35.3) | |
| Temperate | 30 | 6,734,992 | 19.0 (−1.7 to 35.1) | |
The study period may vary according to data available from each location including the climatic zone.
Three cities with polar climate were not considered.
Figure 1.
Location-specific relative risk of all-cause mortality due to cold and heat.
At the country level, the minimum mortality temperature percentiles (MMTPs) ranged from the 36th percentile in Costa Rica to the 98th in Ecuador (Table 2). The AFs for cold varied substantially between countries, with the highest in Uruguay (9.64%) and the lowest in Costa Rica (0.22%). The AFs for heat were more homogeneously distributed, between the highest in Paraguay (1.41%) and the lowest in Ecuador (0.01%). Although some estimates were uncertain, the results seemed more likely to be caused by the small number of locations in some countries than by a different pattern. By climatic zones, the MMTPs ranged from the 44th percentile in tropical climates to the 80th percentile in arid and temperate climates. Moreover, we observed a similar pattern in arid and temperate climates, showing a higher mortality impact for cold (5.10% and 5.29%, respectively) than for heat (0.69% and 0.59%). However, in tropical climates, the mortality impact of cold was much reduced (1.71%), while for heat, it was slightly higher than in the other climatic zones (0.92%). Location-specific relative risk and AF estimates are reported in Table S1; http://links.lww.com/EE/A300.
Table 2.
All-cause mortality attributable to cold and heat by country and climatic zone
| MMTP (%) | Cold AF (%) (95% eCI) |
Heat AF (%) (95% eCI) |
|
|---|---|---|---|
| Country | |||
| Argentina | 79 | 8.95 (7.16, 10.56) | 1.26 (0.97, 1.54) |
| Brazil | 64 | 3.04 (2.57, 3.49) | 0.78 (0.54, 1.01) |
| Chile | 83 | 7.60 (5.22, 10.01) | 0.66 (0.21, 1.05) |
| Colombia | 39 | 5.24 (1.72, 8.35) | 0.49 (0.08, 0.91) |
| Costa Rica | 36 | 0.22 (−1.24, 1.55) | 0.39 (−1.27, 2.05) |
| Ecuador | 98 | 4.33 (−1.23, 9.48) | 0.01 (−0.09, 0.08) |
| Guatemala | 86 | 2.60 (−0.55, 5.63) | 0.12 (−0.17, 0.39) |
| Mexico | 76 | 5.00 (3.90, 6.17) | 0.45 (0.26, 0.65) |
| Overseas France | 39 | 1.05 (−0.25, 2.23) | 0.98 (−0.06, 1.98) |
| Panama | 38 | 0.77 (−1.13, 2.42) | 1.37 (−0.70, 3.19) |
| Paraguay | 77 | 6.92 (4.10, 9.44) | 1.41 (0.77, 1.99) |
| Peru | 96 | 3.58 (1.95, 4.93) | 0.19 (−0.05, 0.42) |
| Puerto Rico | 43 | 1.71 (−0.13, 3.46) | 1.22 (−0.47, 3.00) |
| Uruguay | 76 | 9.64 (7.12, 12.26) | 1.07 (0.61, 1.50) |
| Climatic zonea | |||
| Tropical | 44 | 1.71 (1.15, 2.27) | 0.92 (0.55, 1.28) |
| Arid | 80 | 5.10 (3.94, 6.18) | 0.69 (0.49, 0.88) |
| Temperate | 80 | 5.29 (4.61, 5.94) | 0.58 (0.45, 0.71) |
Three cities with polar climate were not considered.
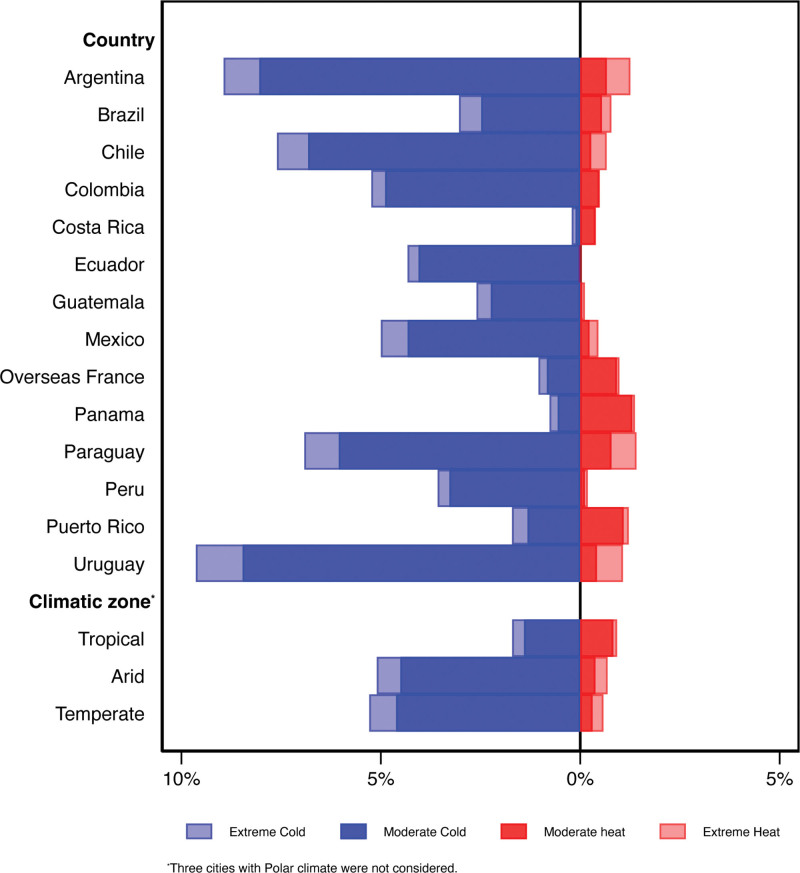
We separated the AFs into components related to moderate and extreme temperatures, as the ranges between the MMT and below and above the cutoff values for cold and heat, respectively. In all countries, most of the mortality risk attributable to temperature was related to moderate cold, while extreme temperatures (either cold or heat) were only responsible for a small fraction (Figure 2). However, extremely cold temperatures had a higher impact on mortality than extreme heat in most countries, but in Panama, Puerto Rico, and the overseas French territories, extremely cold temperatures had a higher impact. By climatic zones, arid and temperate climates show a similar pattern, with higher impact due to cold than heat. Conversely, in tropical climates, the impact due to cold was substantially reduced, while heat impact was higher than in arid and temperate climates.
Figure 2.
Fraction of all-cause mortality attributable to moderate and extreme cold and heat.
The annual economic losses from all-cause deaths related to cold temperatures surpassed those attributed to heat in most countries, except Costa Rica and Panama (Table 3). For cold-related losses, economic estimates ranged from $0.3 million in Costa Rica to $472.2 million in Argentina, whereas for heat-related losses varied between $0.05 million in Ecuador and $90.6 million in Brazil. Moreover, the annual economic loss per 100,000 inhabitants due to cold was significantly higher in the Southern Cone (e.g., $18.7 million in Uruguay, and $2.5 million in Chile and Argentina), while for the other countries ranged between $0.1 to $1.1 million. For heat, the economic loss per 100,000 inhabitants ranged between $0.01 and $0.8 million, being much higher in Uruguay ($2.1 million). Additionally, the annual economic loss associated with cold in temperate climates was nearly 10 times greater than in tropical and arid climates. Conversely, heat-related economic losses were three to seven times smaller in arid climates than in tropical and temperate climates.
Table 3.
Economic loss (in million US dollars, $) due to all-cause deaths associated with cold and heat
| Total attributable deaths | Annual economic loss | Annual economic loss per 100,000 inhabitants | |||||
|---|---|---|---|---|---|---|---|
| VOLY | Cold | Heat | Cold | Heat | Cold | Heat | |
| Country | |||||||
| Argentina | 85.08 | 61,075 | 8,586 | 472.4 | 66.4 | 2.4 | 0.3 |
| Brazil | 68.31 | 113,528 | 29,170 | 352.5 | 90.6 | 0.8 | 0.2 |
| Chile | 94.59 | 23,128 | 2,018 | 198.9 | 17.4 | 2.5 | 0.2 |
| Colombia | 48.52 | 47,826 | 4,465 | 145.0 | 13.5 | 0.9 | 0.1 |
| Costa Rica | 68.30 | 67 | 121 | 0.3 | 0.5 | 0.1 | 0.1 |
| Ecuador | 39.55 | 4,624 | 6 | 36.6 | 0.05 | 0.8 | 0.01 |
| Guatemala | 23.28 | 1,608 | 72 | 4.7 | 0.2 | 0.4 | 0.02 |
| Mexico | 63.79 | 122,141 | 11,109 | 458.3 | 41.7 | 1.1 | 0.1 |
| Overseas France | 288.52 | 557 | 521 | 10.0 | 9.4 | 0.9 | 0.8 |
| Panama | 77.89 | 80 | 142 | 1.6 | 2.8 | 0.3 | 0.6 |
| Paraguay | 28.20 | 3,297 | 672 | 5.8 | 1.2 | 1.1 | 0.2 |
| Peru | 40.62 | 15,141 | 986 | 87.9 | 5.7 | 0.5 | 0.03 |
| Puerto Rico | 140.17 | 438 | 312 | 7.7 | 5.5 | 0.4 | 0.3 |
| Uruguay | 110.41 | 14,626 | 1,626 | 323.0 | 35.9 | 18.8 | 2.1 |
| Climatic zonea | |||||||
| Tropical | 32,608 | 17,639 | 134.5 | 69.4 | 0.5 | 0.2 | |
| Arid | 38,812 | 5,220 | 170.8 | 21.4 | 0.7 | 0.1 | |
| Temperate | 336,716 | 37,132 | 1,799.3 | 200.5 | 1.7 | 0.2 | |
Economic loss calculated from country-specific VOLY for cities in each climatic zone. Three cities with polar climate were not considered.
Discussion
This study provides evidence for the health burden and economic loss attributable to heat and cold in Central and South American countries covering various climates and populations. Most of the mortality burden in the region was caused by cold days compared with warmer days, generating a considerable annual total economic loss of $2.1 billion associated with cold and $290.7 million associated with heat.
The impact of temperature on daily mortality in Central and South America has been reported in several studies.8–11 A recent multicity study conducted in Latin America reported similar findings to those we found in our study, showing a substantially higher proportion of deaths attributable to cold (5.19%) than to heat (0.66%).11 Although our study did not include cities from all Central and South American countries, we included cities with cold-humid winters and hot-dry summers, like those from Chile and Argentina, and cities with cold-dry winters and hot-humid summers, like those from Central America (Mexico, Costa Rica, Guatemala, Panama, and Ecuador) and a few from the Caribbean (Puerto Rico, Guadalupe, Martinique). Our results by climatic zones showed a higher mortality impact from cold temperatures in arid and temperate regions than in tropical zones. The tropical climate may offer some protection against the health impacts of cold due to more homogeneously distributed temperatures and higher humidity levels. Conversely, we found a slightly higher impact from heat in locations in tropical climates, probably due to their higher temperatures compared to those in arid and temperate climatic zones.
A key strength of our study is the estimation of economic loss due to the nonoptimum temperature in the region. The Central and South American regions are in an asymmetrical position since their contribution to total greenhouse gas emissions is quite limited. Yet, it is highly vulnerable to the effects of climate change.22 An impact that, according to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change (IPCC), will aggravate economic and social inequalities in the region.23 A recent global study on projections of temperature-related excess mortality predicts a steep rise in heat-related excess mortality that, under extreme scenarios of global warming, is not offset by a decrease in cold-related deaths. The net impact is projected to be stronger in warmer areas of the Americas, particularly in locations with tropical climates, and notably high in arid or equatorial regions.24
In our study, we included the largest cities with populations of more than five million, including Sao Paulo and Rio de Janeiro (Brazil), Mexico City (Mexico), Buenos Aires (Argentina), Lima (Peru), Bogota (Colombia), and Santiago (Chile), cities in countries with the highest gross domestic product per capita (Uruguay, Panamá, Chile, and Argentina), and cities in countries with lowest gross domestic product per capita (Guatemala, Ecuador, and Paraguay y Peru). The annual economic loss due to nonoptimum temperatures in these countries was estimated as $2.4 billion per year, with a substantial proportion attributed to cold. In addition, our results showed some geographical variation across countries, more particularly for cold, with the highest economic loss per 100,000 inhabitants notably higher in countries located in the Southern Cone (i.e., Uruguay, Chile, and Argentina). Although direct comparison with economic loss in other locations is difficult, several studies also reported a considerable economic loss due to nonoptimum temperatures in several locations. For example, in the United States, the economic losses from heat-related deaths were estimated at $4.2 million and $5.1 billion in Michigan13 and California,12 respectively. A study in Australia reported an economic burden of $6.2 billion annually due to reduced labor productivity due to heat stress.25 In France, the economic impact of selected health effects of heat waves amounts to €25.5 billion, mainly in mortality.14 More recently, a study conducted in Wuhan, China, estimated the induced economic losses were around $22 billion.26 Moreover, Helo Sarmiento et al27 have already indicated that most research results highlight the high costs of the health effects of climate change in South America.
However, some limitations should be acknowledged. First, our results for some of the countries/climatic zones may not be representative, as not all the cities were included. Furthermore, most locations were urban areas; therefore, the results may not be generalizable to less urban locations. Furthermore, we did not conduct the assessment by age, sex, ethnicity, or specific causes due to the lack of data. Thus, we could not explore the vulnerability. However, previous studies in the region have already reported that the health impacts of nonoptimal temperatures are strongest among older adults,10,11 although vulnerability by sex and education may vary between city.10 Finally, further research is needed to expand our estimations, especially concerning economic losses, to other locations in the region, such as rural areas. This will enable a better understanding of the impact of climate change on both health and the economy within the region.
In conclusion, our results provide significant evidence and contribute to addressing the research gap on the health burden and economic losses associated with nonoptimal temperatures in Central and South America.28,29 Therefore, it is essential to develop public health policies for mitigation and adaptation plans, providing detailed information to guide policymakers in implementing practical actions within the region to address the health effects of nonoptimal temperatures in the current climate change scenario.30
Conflicts of interest statement
A.T. was supported by the JSPS KAKENHI Grant Number 24K13527. The other authors declare that they have no conflicts of interest with regard to the content of this report.
Supplementary Material
Footnotes
Published online 10 October 2024
Data have been collected within the MCC (Multi-Country Multi-City) Collaborative Research Network (https://mccstudy.lshtm.ac.uk/) under a data-sharing agreement and cannot be made publicly available. Researchers can refer to MCC participants listed as coauthors for information on accessing the data for each country.
Supplemental digital content is available through direct URL citations in the HTML and PDF versions of this article (www.environepidem.com).
References
- 1.Anderson BG, Bell ML. Weather-related mortality: how heat, cold, and heat waves affect mortality in the United States. Epidemiology. 2009;20:205–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gasparrini A, Guo Y, Hashizume M, et al. Mortality risk attributable to high and low ambient temperature: a multicountry observational study. Lancet. 2015;386:369–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guo Y, Gasparrini A, Armstrong B, et al. Global variation in the effects of ambient temperature on mortality: a systematic evaluation. Epidemiology. 2014;25:781–789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Armstrong B, Bell ML, de Sousa Zanotti Stagliorio Coelho M, et al. Longer-term impact of high and low temperature on mortality: an international study to clarify length of mortality displacement. Environ Health Perspect. 2017;125:107009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sera F, Armstrong B, Tobias A, et al. How urban characteristics affect vulnerability to heat and cold: a multi-country analysis. Int J Epidemiol. 2019;48:1101–1112. [DOI] [PubMed] [Google Scholar]
- 6.Green H, Bailey J, Schwarz L, Vanos J, Ebi K, Benmarhnia T. Impact of heat on mortality and morbidity in low and middle income countries: a review of the epidemiological evidence and considerations for future research. Environ Res. 2019;171:80–91. [DOI] [PubMed] [Google Scholar]
- 7.Division UP. Population 2030: Demographic Challenges and Opportunities for Sustainable Development Planning. 2015. [Google Scholar]
- 8.Silveira IH, Oliveira BFA, Cortes TR, Junger WL. The effect of ambient temperature on cardiovascular mortality in 27 Brazilian cities. Sci Total Environ. 2019;691:996–1004. [DOI] [PubMed] [Google Scholar]
- 9.Hurtado-Diaz M, Cruz JC, Texcalac-Sangrador JL, et al. Short-term effects of ambient temperature on non-external and cardiovascular mortality among older adults of metropolitan areas of Mexico. Int J Biometeorol. 2019;63:1641–1650. [DOI] [PubMed] [Google Scholar]
- 10.Bell ML, O’Neill MS, Ranjit N, Borja-Aburto VH, Cifuentes LA, Gouveia NC. Vulnerability to heat-related mortality in Latin America: a case-crossover study in Sao Paulo, Brazil, Santiago, Chile and Mexico City, Mexico. Int J Epidemiol. 2008;37:796–804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kephart JL, Sanchez BN, Moore J, et al. City-level impact of extreme temperatures and mortality in Latin America. Nat Med. 2022;28:1700–1705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Knowlton K, Rotkin-Ellman M, Geballe L, Max W, Solomon GM. Six climate change-related events in the United States accounted for about $14 billion in lost lives and health costs. Health Aff (Millwood). 2011;30:2167–2176. [DOI] [PubMed] [Google Scholar]
- 13.Gronlund CJ, Cameron L, Shea C, O’Neill MS. Assessing the magnitude and uncertainties of the burden of selected diseases attributable to extreme heat and extreme precipitation under a climate change scenario in Michigan for the period 2041-2070. Environ Health. 2019;18:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Adelaide L, Chanel O, Pascal M. Health effects from heat waves in France: an economic evaluation. Eur J Health Econ. 2022;23:119–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sera F, Armstrong B, Blangiardo M, Gasparrini A. An extended mixed-effects framework for meta-analysis. Stat Med. 2019;38:5429–5444. [DOI] [PubMed] [Google Scholar]
- 16.Gasparrini A, Leone M. Attributable risk from distributed lag models. BMC Med Res Methodol. 2014;14:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tian Z, Li S, Zhang J, Guo Y. The characteristic of heat wave effects on coronary heart disease mortality in Beijing, China: a time series study. PLoS One. 2013;8:e77321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lin SY, Ng CFS, Kim Y, et al. Ambient temperature and nervous system diseases-related mortality in Japan from 2010 to 2019: a time-stratified case-crossover analysis. Sci Total Environ. 2023;867:161464. [DOI] [PubMed] [Google Scholar]
- 19.Li H, Yao Y, Duan Y, et al. Years of life lost and mortality risk attributable to non-optimum temperature in Shenzhen: a time-series study. J Expo Sci Environ Epidemiol. 2021;31:187–196. [DOI] [PubMed] [Google Scholar]
- 20.Demoury C, De Troeyer K, Berete F, et al. Association between temperature and natural mortality in Belgium: effect modification by individual characteristics and residential environment. Sci Total Environ. 2022;851:158336. [DOI] [PubMed] [Google Scholar]
- 21.Viscusi WK, Masterman CJ. Income elasticities and global values of a statistical life. J Benefit Cost Anal. 2017;8:226–250. [Google Scholar]
- 22.Yglesias-Gonzalez M, Palmeiro-Silva Y, Sergeeva M, et al. ; Red de Clima y Salud de América Latina y el Caribe. Code red for health response in Latin America and the Caribbean: enhancing peoples’ health through climate action. Lancet Reg Health Am. 2022;11:100248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.IPCC. Climate Change 2023: Synthesis Report. Contribution of Working Groups I, II and III to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change. 2023. [Google Scholar]
- 24.Gasparrini A, Guo Y, Sera F, et al. Projections of temperature-related excess mortality under climate change scenarios. Lancet Planet Health. 2017;1:e360–e367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zander KK, Botzen WJW, Oppermann E, Kjellstrom T, Garnett ST. Heat stress causes substantial labour productivity loss in Australia. Nat Clim Change. 2015;5:647–651. [Google Scholar]
- 26.Chen S, Zhao J, Lee SB, Kim SW. Estimation of relative risk of mortality and economic burden attributable to high temperature in Wuhan, China. Front Public Health. 2022;10:839204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Helo Sarmiento J, Melo O, Ortiz-Alvarado L, Pantoja Vallejos C, Reyes-Mandujano IF. Economic impacts associated with the health effects of climate change in South America: a scoping review. Lancet Reg Health Am. 2023;26:100606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Palmeiro-Silva YK, Lescano AG, Flores EC, et al. Identifying gaps on health impacts, exposures, and vulnerabilities to climate change on human health and wellbeing in South America: a scoping review. Lancet Reg Health Am. 2023;26:100580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fernandez-Guzman D, Lavarello R, Yglesias-Gonzalez M, Hartinger SM, Rojas-Rueda D. A scoping review of the health co-benefits of climate mitigation strategies in South America. Lancet Reg Health Am. 2023;26:100602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Paz-Soldan VA, Valcarcel A, Canal-Solis K, et al. A critical analysis of national plans for climate adaptation for health in South America. Lancet Reg Health Am. 2023;26:100604. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.