Abstract
Background
Helicopter Emergency Medical Services (HEMS) in the United Kingdom (UK) deliver enhanced care to high-acuity, critically ill and injured patients. To enable patients to meet the HEMS team who treated them, many services within the UK have developed or are in the process of developing a Patient and Family Aftercare Service (PFAS). This study aims to evaluate whether the introduction of PFAS mitigates anxiety associated with patient aftercare visits.
Methods
A service evaluation of anxiety in HEMS team members before and after patient aftercare visits were conducted. The study was carried out between 1 September 2023, and 31 October 2023, and patient visits were undertaken between March 2022 and July 2023. An electronic survey was distributed to the respondents who provided informed consent for participation. The survey comprised the validated generalised anxiety disorder anxiety scale (GAD-7) and five additional contextualised statements developed through the wider PFAS. Anonymised data were collected using REDCap, a secure electronic database and was analysed in R programming. Free-text comments were reported by content analysis, placed into themes, and discussed with a narrative to complement the quantitative analysis.
Results
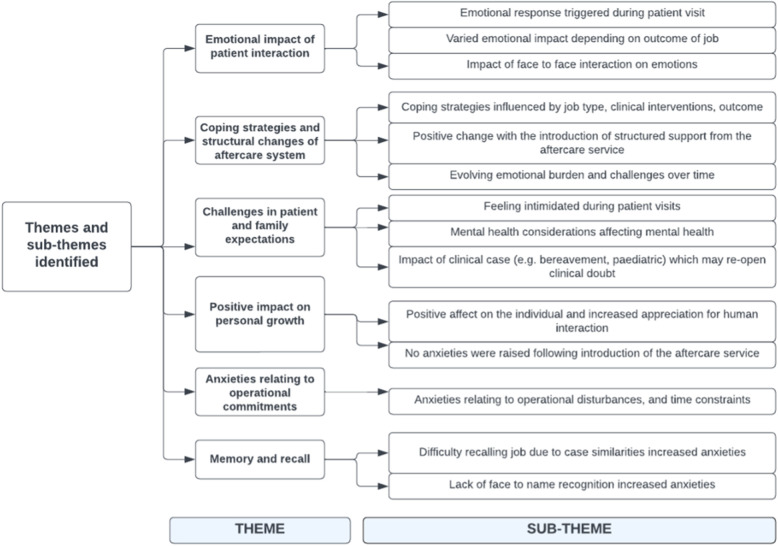
Of the 33 recipients, 25 completed the questionnaire. Between the pre- and post-aftercare visits, a statistically significant difference was found between scores for GAD-7 (0.004, p < 0.05) and contextualised statements (0.001, p < 0.05). In addition, six broad themes were identified through content analysis. These include the emotional impact of patient interaction, coping strategies and structural changes in the aftercare system, challenges in patient and family expectations, anxieties relating to operational commitments, memory and recall of the incident, and a positive impact on personal growth.
Conclusion
Anxiety related to patient aftercare visits was reduced when measured before and after the patient visits. Following this service evaluation, we can hypothesise that within pre-hospital care, PFAS plays an important structural role. Future research should focus on affirming the correct tool to measure anxiety in multi-disciplinary teams and prospectively evaluating these methods collaboratively across multiple pre-hospital services.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12913-024-11720-7.
Keywords: Trauma, Pre-hospital, Helicopter emergency medical services, Patient and family aftercare service, Anxiety
Background
The restructuring of trauma services in the United Kingdom (UK) has resulted in the formation of regional trauma networks [1]. The main goal of these networks is to improve the organisation of care and integrate rehabilitation services for injured patients. These networks are centered around major trauma centers (MTCs) and trauma units (TUs) which provide continuous, multidisciplinary, and consultant-led care for seriously injured patients. Although this hub-and-spoke model is highly efficient, it often necessitates transporting patients over longer distances, which can have a detrimental impact on local rehabilitation services and the patient’s family support [2, 3]. Patient and family aftercare services (PFAS) are a new endeavour in the pre-hospital sector that aim to provide a holistic service integral to the patient’s journey from their core primary retrieval to the hospital and subsequent rehabilitation [4, 5].
Comprehensive and effective aftercare services for patients and their families cannot be overstated in modern healthcare [5, 6]. As medical advancements continue to extend and enhance individuals’ lives, the focus on post-treatment support is pivotal [3]. The PFAS objectives align within a coordinated trauma system. One key objective of patient aftercare services is to provide ongoing support services to patients and their families (including bereaved families) [2, 5] which commonly requires facilitated base visits. Often, a patient may have no recollection of the incident, and they are keen to bridge the gap between an incident and their road to recovery [5, 6]. Patient visits are multi-professional, and often include HEMS clinicians, dispatchers, or pilots. Prior to the implementation of the PFAS, these visits were largely reactive in nature and structure, which may have increased stress and anxiety [7].
Anxiety, although a normal human emotion, can become excessive, pervasive, and ultimately assume pathological significance [8]. Anxiety may affect instrumental activities of daily living, and the negative spiral of these circumstances may cause personal and professional aspects of life to decline [8]. Pre-hospital emergency medicine often leads to high-pressure environments and it is widely acknowledged that pre-hospital clinicians are regularly exposed to stress and anxiety in the operational environment [9–11]. Studies have indicated that all grades and types of clinicians may experience poor well-being, stress, burnout and poor mental health [6, 10, 12, 13] which has been confirmed by specific biomarkers [14]. On the inception of the PFAS, it was key to establish the emotional impact on crew members of reuniting the HEMS teams with former patients. Furthermore, patterns of work-related stress can affect anxiety and burnout [11], such as in remote operational working [15, 16]. Studies report that the opportunity to forge team positivity and increase empathy towards patients through one-to-one care, as well as the chance to be reunited with former patients, can facilitate improved job satisfaction [17, 18]. However, this has not been studied since the introduction of PFAS.
Our study aimed to report the anxiety levels experienced by HEMS teams in the context of patient and family aftercare visits. We hypothesised that the introduction of PFAS affects the level of anxiety experienced by HEMS crew members during a patient and family aftercare visit. By comparing the reported anxiety levels both before and after patient and family aftercare visits, the study sought to discern the impact of PFAS on HEMS teams and explore the structural processes that may mitigate or exacerbate this anxiety.
Methods
Study design
A cross-sectional survey design was employed. Participants were eligible if they were employed by Air Ambulance Charity Kent Surrey Sussex in a role as a Dispatcher, Paramedic, Doctor, or Pilot, and had participated in a patient and family aftercare visit. Participants were recruited from a recorded log held within the PFAS management team. The research questionnaire (Supplementary File 1) was designed based on the first initial meeting of the former patient. Any subsequent meetings with the same patients were not included in the study. The study period for inclusion was patient visits between 1 May 2022, and 31 July 2023, with a clinical incident in the preceding year. The study was completed between 1 September 2023, and 31 October 2023. A purposive sampling method was adopted and respondents were selected only if they fulfilled the eligibility criteria [19].
Study setting
Air Ambulance Charity Kent Surrey Sussex (KSS) is a HEMS covering three counties in southeast England, with a resident population of 4.5 million. Two doctor/paramedic teams respond in either a helicopter or rapid response car from an operational base. Doctors have a minimum of five years postgraduate experience, including a minimum of six months of hospital emergency anaesthesia training. Paramedics undergo further specialist training, including theoretical modules for pre-hospital emergency anaesthesia. All crew undergo an intense training period prior to independent practice, including structured medical education, simulation training and operational supervision by pre-hospital care consultants and senior paramedics. Within the operation clinicians are in constant communication with other non-clinical facing roles, such as the dispatchers and pilots.
Implementation of the PFAS in May 2022 was a pivotal component of the five-year strategic objectives at KSS. Key organisational structures were developed alongside a staffing model through stakeholder engagement to deliver a governed aftercare service. Stakeholders included associated Major Trauma Systems within the region, Senior Leaders within the local ground Emergency Medical Service (EMS) and the Trustee board at KSS. Importantly a consultation was held with patients and families from within the region. The model is staffed with a Patient and Aftercare Manager and Patient and Aftercare Lead, with wider support through the organisational Senior Leadership Team. The PFAS at KSS is funded by income generated by the Charity. Ultimately, the service aims to play a role in supporting patients’ recovery and rehabilitation from traumatic incidents or acute medical illness. One key objective is to facilitate patient and family aftercare visits (including bereaved families) which may include multi-professional team members. Patient visits were conducted in a room specifically designed for PFAS aftercare. They are decorated with soft furnishings and interiors to promote a calming atmosphere in a confidential setting. The visit is primarily hosted by the aftercare team (SP/ST).
Study population
Individuals were eligible for participation if they fulfilled the following criteria: employed at KSS, professionals trained as either a Pilot, Doctor, Paramedic or Dispatcher (whether in permanent or part-time employment), and attended a visit planned by the HEMS PFAS with a former patient, accompanied by family, or without. The exclusion criteria pertained to those employed at KSS and invited to attend a visit but were not part of the team that treated the patient. The decision to include non-clinical professions align with objectives outlined by the Health Services Safety Investigations Body (HSSIB) [20]. Non-clinical roles provide essential support functions to clinicians delivering pre-hospital interventions often with exposure to patient care at the point of injury. Aligned dispatch, aviation operations and clinical medicine is essential for streamlined patient safety and patient care at KSS, therefore the inclusion of these roles was deemed relevant within a system-focused organisation [20].
Research question and objectives
Does the introduction of PFAS affect the level of perceived anxiety felt by HEMS during a patient and family aftercare visit, and explore factors which may mitigate or exacerbate anxiety both pre- and post- patient visit.
Questionnaire design
The self-completed, closed-question questionnaire was distributed using the Research Electronic Data Capture (REDCap) software hosted at KSS. The questionnaire was retrospectively delivered over two time points and anxiety levels scored both before and after meeting former patients and their families. The chosen questionnaire comprised the GAD-7, and this was adopted in combination with contextualised statements. Questions pertaining to the professional background and demographics of the respondent were also included.
REDCap is a secure, web-based software platform designed to support data capture for research studies, providing an intuitive interface for validated data capture; audit trails for tracking data manipulation and export procedures; automated export procedures for seamless data downloads to common statistical packages, and procedures for data integration and interoperability with external sources [21]. Following data collection anonymised data was downloaded into Excel (Version 16.79.1). The data were cleaned, coded, and pre-processed for analysis.
Generalised anxiety disorder anxiety scale and contextualised statements
The GAD-7 (Table 1) is recommended by National Institute of Clinical Excellence (NICE; Clinical Knowledge Summaries, 2022) and has become a popular tool in research and clinical settings because of its brevity and ease of administration [8, 22]. The tool asks your feeling of anxiety of the previous two weeks [22]. Developed in 1971 by a Stanley Rachman and his colleagues it is a popular tool used worldwide [8]. The tool itself is a self-reporting questionnaire asking 7 questions, with 4 points, scoring 0–3, and resulting scores range from 0 to 21 [8, 22]. The GAD-7 is validated by NICE, and is a brief and easily administered self-report tool, this brevity and its wide usage in research and clinical settings made it a practical and usable tool for the pre-hospital setting [8, 23].
Table 1.
GAD-7 constructs
| Over the last two weeks how often have you been bothered by the following problems* | Not at all | Several days | More than half the days | Nearly every day |
|---|---|---|---|---|
| Feeling nervous, anxious or on edge | 0 | 1 | 2 | 3 |
| Not being able to stop or control worrying | 0 | 1 | 2 | 3 |
| Worrying too much about different things | 0 | 1 | 2 | 3 |
| Trouble relaxing | 0 | 1 | 2 | 3 |
| Being so restless that it is hard to sit still | 0 | 1 | 2 | 3 |
| Becoming easily annoyed or irritable | 0 | 1 | 2 | 3 |
| Feeling afraid as if something awful might happen | 0 | 1 | 2 | 3 |
| The following cut offs correlate with level of anxiety severity: | ||||
| Score 0–4 | Minimal anxiety | |||
| Score 5–9 | Mild anxiety | |||
| Score 10–14 | Moderate anxiety | |||
| Score 15 or greater | Severe anxiety | |||
In addition to the GAD-7, following a structured literature review pertaining to patient and family aftercare services across healthcare sectors (Supplementary File 2) the researchers devised five questions that were contextually specific to the aftercare setting. Although unvalidated, through previous experience it was believed that these may enable a better analysis of the anxiety levels associated with patient visits. At that time the PFAS team had (within an 18-month period) facilitated over 60 visits with HEMS teams and former patients, and the statements were drawn from the expert consensus of the wider PFAS (SP/ST/LC). Contextualised statements comprised Statement A: Meeting the patient and/or their family, Statement B: Comprehension of the patient’s injury burden, Statement C: Uncertainties surrounding the process of the patient visit, Statement D: If you consider yourself to hold moral trauma, has the idea of a patient visit increased the burden of your own moral trauma, Statement E: Meeting patient’s expectations, and Statement F: Other, which allowed free text descriptive comments. The statements were measured on a Visual Analogue Scale (VAS) with a scale from to 0–10.
Statistical analysis
Normality and distribution tests were performed on pre-processed data to determine the appropriate statistical tests. K-S tests and normality plots were used. Each GAD-7 construct was scored out of 3, with 7 constructs allowing for a total of 21. The NICE Guidance (NICE General Anxiety Disorder, 2023) with a composite score was calculated for both the pre- and post-visit questionnaires. Tests for differences (e.g., Chi-squared or Wilcoxon Ranked Sum, depending on data distribution) between reports of anxiety both pre- and post-visit were calculated. Categorical variables were calculated and reported as frequencies and percentages, whereas quantitative variables were reported as means and standard deviations. Categorical variables were tested using the chi-square test or t-test. Statistical significance was set at p ≤ 0.05. Data was cleaned and structured in Microsoft Excel. Statistical analysis was performed in R (R: A language and environment for statistical computing, Vienna, Austria) statistical programming language (version 4.2.1).
The study design incorporated free text responses. The responses were analysed qualitatively using content analysis [26], a common technique used in qualitative research, where relevant comments were separated into categories and sub-categories from free-text answers [26]. Content analysis aimed to (1) identify and understand themes, patterns, and relationships within the data, (2) explore how the data could inform theoretical claims made in research studies, and (3) quantify qualitative data [27]. Themes and subthemes were visualised using a modified Braun and Clarke approach (2006). Due to the nature of the study question, study setting, and pre-study engagement, it was not anticipated that there would be high quantities of missing data; however, missing data was reported as appropriate.
Results
Study population demographics and characteristics
From the organisation 33 participants were deemed eligible to meet the study inclusion criteria. The questionnaire was distributed to all 33 individuals and was completed by 25 respondents (76% response rate). Fifteen respondents were male (60%) and 10 were female (40%). The highest proportion of respondents were paramedics (11/25, 44%), dispatchers (5/25, 20%), doctors (7/25, 28%), and pilots (2/25, 8%). Of those eligible, the response rates for paramedics were 11/12 (92%), dispatchers 5/5 (100%), doctors 7/14 (50%) and pilots 2/2 (100%).
Analysis of the GAD-7 constructs
The total mean pre- and post-visit scores for the GAD-7 decreased from 8.2 before the aftercare visit to 7.2 after the visit. Table 2 presents the individual constructs. All showed a decrease in pre- and post-scores. The construct ‘Feeling nervous, anxious, or on edge’ showed the largest reduction from pre [28] to post [25] aftercare visits. One respondent scored > 15 (severe anxiety) and was signposted effectively.
Table 2.
GAD-7 scores for pre- and post-groups highlighting the scores for each construct (n = 25)
| GAD-7 constructs | Range of possible scores | Time point | Total score * | Median score for construct |
|---|---|---|---|---|
| Feeling nervous, anxious or on edge | 0–3 | Pre | 34 | 1 |
| Post | 25 | 1 | ||
| Not being able to stop or control worrying | 0–3 | Pre | 27 | 1 |
| Post | 25 | 0 | ||
| Worrying too much about things | 0–3 | Pre | 28 | 1 |
| Post | 27 | 0.92 | ||
| Trouble relaxing | 0–3 | Pre | 33 | 1.2 |
| Post | 27 | 0.92 | ||
| Being so restless that it is hard to sit still | 0–3 | Pre | 26 | 0.96 |
| Post | 26 | 0.96 | ||
| Becoming easily annoyed or irritable | 0–3 | Pre | 31 | 1.16 |
| Post | 28 | 1.04 | ||
| Feeling afraid as if something awful might happen | 0–3 | Pre | 26 | 0.96 |
| Post | 22 | 1 |
GAD-7 Generalised Anxiety Disorder-7, SD Standard Deviation. *All respondents
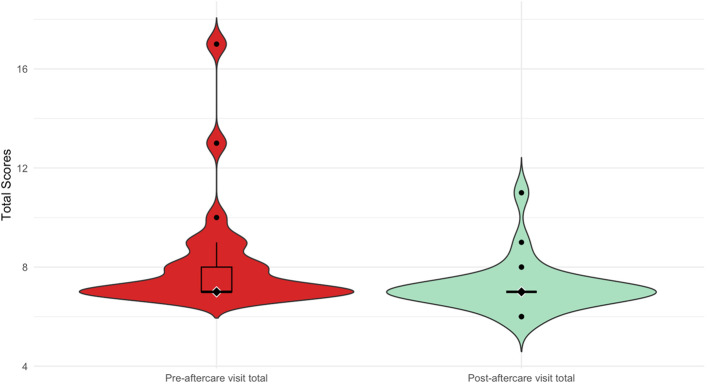
A Wilcoxon signed-rank test was performed because of the non-normal data distribution between the two related groups. The test statistic was 0.000 with a standard error of 13.973. The standardised test statistic was − 3.256. The obtained p-value of 0.004 suggests a rejection of the null hypothesis at a significance level of 0.05 in favour of the alternative hypothesis. This suggests a significant difference between the mean pre and post GAD-7 scores (Fig. 1).
Fig. 1.
Violin plot showing the distribution and difference between mean total GAD-7 scores before and after the aftercare visit. Violin plot showing the difference between the total median GAD-7 scores in the pre- and post-aftercare visits. A violin plot visualizes the data distribution and probability density. The width of the ‘violin’ at different levels indicates the frequency of data points, with wider sections representing a higher density. The internal black dot marks the median, whereas the black bar indicates the interquartile range
Analysis of contextualised statements
Each of the five contextualised statements was coded and the scores totalled for each contextualised statement, with a possible score between 0 and 10. The maximum score for all contextualised statements was between 0 and 50. The totals were then calculated for both pre- and post-aftercare visits for all the respondents. The total score for the post-aftercare visit (273) was lower than the pre-aftercare visit score (410) for the sample (Table 3). Statement E (“Meeting Patient Expectation”) saw the largest reduction from a score of 111 to 69 (62% reduction). Figure 2 highlights the difference between the mean scores for pre- and post-aftercare visits for the contextualised statements.
Table 3.
Contextualised statements pre and post scores (n = 25) for total sample
| Contextualised statement domain (anxiety regarding) | Range of possible score | Time point | Sample total score | Mean |
|---|---|---|---|---|
| Meeting the patient/ and or their family | 0–10 | Pre | 95 | 3.8 |
| Post | 55 | 2.2 | ||
| Comprehension of the patient’s ongoing injury burden | 0–10 | Pre | 84 | 3.3 |
| Post | 69 | 2.7 | ||
| Uncertainties surrounding the process of the patient visit | 0–10 | Pre | 68 | 2.7 |
| Post | 41 | 1.6 | ||
| If you consider yourself to be the subject of moral trauma, has the idea of a patient visit increased the personal burden of this moral trauma | 0–10 | Pre | 52 | 2 |
| Post | 39 | 1.5 | ||
| Meeting patient expectations | 0–10 | Pre | 111 | 4.4 |
| Post | 69 | 2.7 |
Contextualised statements for both pre- and post-scores were calculated for the total study sample
Fig. 2.
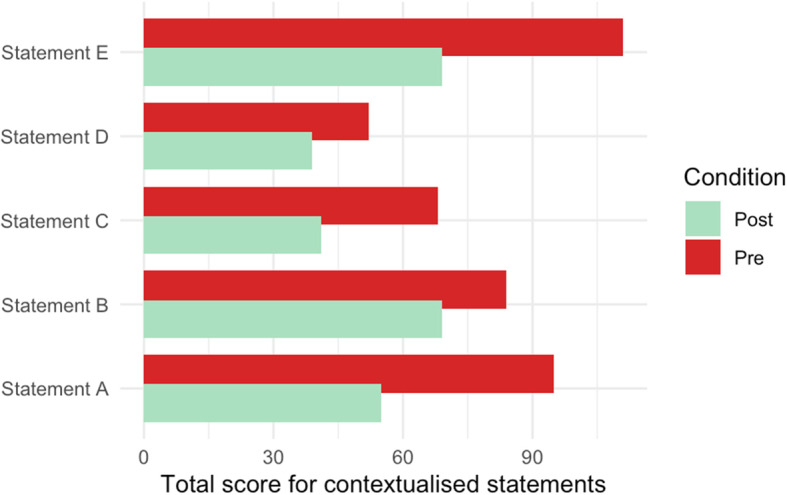
Paired bar graph comparing pre- and post-aftercare scores for each contextualised statement. Statement A: Meeting the patient and/or their family, Statement B: Comprehension of the patient’s ongoing injury burden, Statement C: Uncertainties surrounding the process of the patient visit, Statement D: If you consider yourself to be the subject of moral trauma, has the idea of a patient visit increased the personal burden of this moral trauma, Statement E: Meeting patient expectations
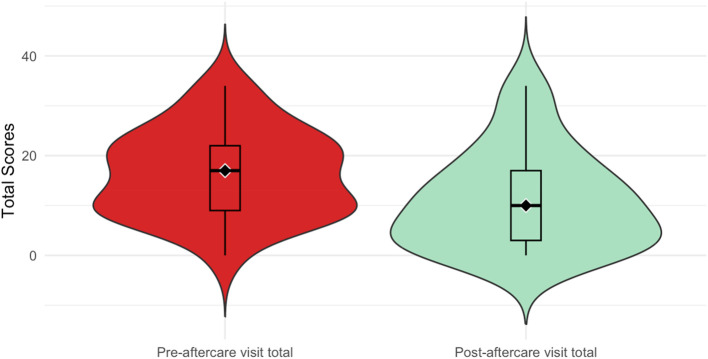
A paired t-test was performed to test the difference between pre- and post-scores for contextualised statements. The t-statistic was found to be t = 3.542 with df = 24 degrees of freedom, resulting in a p-value < 0.001. Given the small p-value, we reject the null hypothesis, indicating that the true mean difference between the pre- and post-event total scores is not equal to 0. The 95% confidence interval for the true mean difference ranged from 2.28 to 8.67, providing a plausible range for the population mean difference. This interval did not include zero, further supporting the rejection of the null hypothesis (Fig. 3).
Fig. 3.
Violin plot showing the distribution and difference between the mean total contextualised statement scores for pre- and post-aftercare visits. Violin plot for pre- and post-aftercare visit total scores for contextualised statements. A violin plot visualizes the data distribution and probability density. The width of the ‘violin’ at different levels indicates the frequency of data points, with wider sections representing a higher density. The internal black dot marks the median, whereas the black bar indicates the interquartile range
Content analysis of the free text responses
Content analysis was performed with free-text sections in both the pre- and post-aftercare visit questionnaires. Two questions allowed free-text comments in the pre- and post-questionnaires. The following themes were derived using content analysis, as previously described. Each theme and sub-theme were reported using a content analysis approach. Where appropriate, verbatim statements were shown to illustrate the themes identified. The identified broad themes are graphically represented in Fig. 4.
Fig. 4.
Broad themes and subthemes identified through content analysis. Thematic analysis using a modified Braun and Clarke approach was used to identify the main themes and subthemes from pre- and post-aftercare visits following the introduction of the PFAS
Memory and recall challenges
Within the theme of memory and recall challenges, two prominent sub-themes emerged: difficulty remembering patients due to the volume of similar jobs and lack of face-to-name recognition.
Several respondents indicated that their anxiety stemmed from difficulties in recalling and remembering specific patients and their circumstances during encounters with the HEMS team. The high volume of similar cases contributed to this challenge, making it difficult for staff to maintain clear recollections of individual patients. Additionally, the absence of face-to-name recognition exacerbated feelings of anxiety. This issue was clearly articulated by one respondent, who noted, “not remembering the patient as we attend so many jobs that are similar and not having a face for the name” (ID 10). This highlights the significant impact of these memory and recognition challenges on the respondents’ overall anxiety levels.
Emotional impact of the patient interaction
This theme explores the emotional impact experienced by respondents during patient interactions, with a particular focus on face-to-face encounters. Three sub-themes emerged: emotional responses triggered during patient visits, the impact of face-to-face interaction on emotions, and varied emotional responses depending on the job outcome.
Respondents reported that each patient interaction, especially those involving direct face-to-face contact, had a notable emotional effect. The outcome of these interactions—whether positive or negative—was also perceived to influence the level of anxiety experienced by the respondents. For instance, one respondent described feeling distressed during patient visits, noting, “I find that maybe 10 or 15 minutes into the visit, when the patient describes their experiences/injuries/recovery quite upsetting in certain situations. I think being face to face with the patient and/or their family to be quite triggering as you feed off their emotions” (ID 14). This statement underscores the significant emotional burden that can arise from direct patient interactions and the varying emotional responses based on the outcomes of these encounters.
Coping strategies and changes over time
This theme delves into the respondents’ perspectives on coping strategies, the evolving emotional burden, and the impact of structured support from the aftercare team. It encompasses three sub-themes: coping strategies influenced by job type, clinical interventions, and outcomes; the evolving emotional burden and challenges over time; and positive change facilitated by the introduction of structured support.
Respondents noted that their coping strategies were significantly influenced by the nature of the job, the clinical interventions required, and the overall outcomes. When the outcomes were positive, such as successful patient recoveries with minimal clinical intervention, respondents experienced relatively lower levels of anxiety and concern. In contrast, jobs resulting in death or severe disability posed greater emotional challenges. One respondent articulated this variation in emotional response, stating, “Answers to the above questions vary depending on the job type, clinical interventions, and overall outcome. In cases where the outcome is positive for the patient, there is often minimal anxiety/concern. Where there has been a death or severe disability because of the job, they are more difficult to deal with. With this job, the outcome was positive, and the patient hadn’t required any specific clinical interventions from us; however, in other circumstances, this can be more challenging and more of an emotional burden” (ID 10).
Additionally, the introduction of structured support from the aftercare team was seen as a positive development, providing essential support that helped mitigate emotional burdens and enhance coping mechanisms over time.
Challenges in patient and family engagement
This theme addresses the emotional and psychological effects of family visits on respondents, highlighting three sub-themes: feeling intimidated during family visits, mental health considerations affecting engagement, and the impact of contextual factors such as bereavement or paediatric cases that may exacerbate clinical doubt.
Respondents reported feeling intimidated during interactions with families and, in some cases, patients who sought detailed information about their injuries and the broader implications on their daily lives and families. This sense of intimidation could be associated with a cumulative impact on mental health, which could influence performance in subsequent jobs. One respondent shared a profound experience, noting, “On more than one occasion I have felt intimidated by families and in some cases patients when they wanted to probe more about their injuries and the implications these have had for them on their daily life and how they have affected their families. There did come a point where I no longer wanted to engage in family visits as I felt it was increasingly detrimental to my mental health and affecting my ability to emotionally manage some of the more traumatic jobs we go to” (ID 6). This statement illustrates how the pressures of family interactions and the mental health challenges associated with them can impact the ability to effectively manage and engage in future patient visits, particularly in emotionally charged contexts.
Anxieties relating to the context of visit during operational hours
This sub-theme addresses the anxiety experienced by respondents concerning operational aspects, including disturbances and time constraints during aftercare visits.
Respondents noted that insufficient time to thoroughly address and close out aftercare visits could lead to unresolved emotions being carried over into subsequent tasks. This unresolved ‘emotional baggage’ was reported to contribute to heightened anxiety. As one respondent described, “Anxiety around being operational and being disturbed at difficult times or not being able to spend the necessary time with the patient and/or family” (ID 22). Another respondent added that the emotional intensity of interactions with patients or their families could be overwhelming, particularly when they were required to move on to new tasks immediately. They noted, “Level of emotion expressed by patient/family can sometimes be overwhelming and can be difficult to process if immediately sent out on job” (ID 3).
These insights highlight the challenges of managing emotional responses in the context of operational demands and time pressures, emphasising the need for adequate time and support to process and address feelings arising from patient interactions.
Positive impact on personal growth
This theme explores the positive effects of patient aftercare visits on personal growth, focusing on increased appreciation for human interactions and the absence of anxiety in some cases.
Respondents reported that, in certain instances, patient aftercare visits had a notably positive impact on their personal development. These visits were associated with an enhanced appreciation for human interactions, fostering a greater sense of connection and empathy. One respondent reflected on this positive experience, stating, “Had a positive effect on me and made me appreciate the human interaction more (in a good way), did not raise any anxieties” (ID 17). This indicates that, rather than contributing to anxiety, these interactions were perceived as beneficial and enriching, highlighting the potential for such experiences to support personal growth and emotional resilience.
Discussion
A statistically significant reduction in anxiety was noted among respondents between pre- and post-patient aftercare visits. Regarding the GAD-7, there was a significant difference between the median pre (8.2) and median post (7.2) aftercare visit scores (p < 0.05) with the score remaining in the same anxiety bracket as mild anxiety (4–9 score) overall. Contextualised statements also showed a significant reduction in total score (p < 0.05). In combination with free-text comments, the results highlight the structural importance of PFAS-facilitated patient aftercare visits.
For the contextualised statements, the greatest reduction was seen in the statement ‘Meeting Patient Expectations.’ Patient visits are facilitated by someone with clinical and organisational knowledge that is broader than that of the individual undergoing the patient visit. This may prove to be a protective feature [17] in effectively reducing and improving healthcare professionals’ ability to manage their emotional and cognitive responses. Similarly, the reduction in scores for the personal burden of moral trauma was notable, which highlights that feelings of moral distress among healthcare professionals were alleviated. Another large reduction was seen around ‘Uncertainties surrounding the patient visit,’ as this appeared to increase anxiety in respondents. These results underscore the importance of targeted interventions and structures to support healthcare professionals in managing the complex emotional landscape of patient care after the incident [6].
Themes identified in the free-text responses revealed that the experience of anxiety varied and was dependent on factors such as the severity of injuries, emotional distress witnessed, or perceived operational pressures during the visit. A noteworthy observation was the impact of a supportive structure on re-engaging individuals who had previously refrained from participating in patient aftercare visits. The challenges highlighted included the perception of ‘operational pressure’ i.e. if the individual was on clinical duty whilst the visit was undertaken, as supported by other research [6]. Respondents highlighted that extra anxiety and stress were induced by trying to recall all the facts from the visit, and this was compounded if there was perceived time pressure. Therefore, we can infer that the PFAS promotes an objective and factual account of the incident, and within confidential restraints, this is supportive of those within patient aftercare visits [18]. Certain visits can induce anxiety, especially if conducted immediately after an incident [6], and so the timing and frequency of aftercare visits are important [5]. It also highlights the importance of trauma risk management in pre-hospital services. Trauma Risk Management (TRiM) is a structured approach designed to provide trauma-focused peer support for individuals who have encountered or been exposed to traumatic events [29].
Dasan et al. (2015) suggest that structured visits may reduce negative emotions connecting to subsequent cases, as there is a greater understanding of the impact on patients, especially if the outcome was positive [17]. Participants have previously expressed that they believe the role of Patient and Family Liaison Personnel (PFLP) significantly benefits patients, their families, HEMS clinicians, and related charities [5]. This perception aligns with existing studies on the positive impact of liaison nursing roles in intensive care and general medical practice settings [5, 6]. Research conducted by Norwegian Helicopter Emergency Physicians suggests that patient visits can positively impact job satisfaction among clinicians. Reid (2020) studied pre-hospital stressors in this context and reported high levels of job satisfaction among the physicians. Reid et al. (2020) further documented that the opportunity to forge team positivity and increase empathy towards patients through one-to-one care, as well as the chance to be reunited with former patients, can facilitate improved job satisfaction. Similarly, Burnett et al. (2023) found that resilience training in hospitals could also have a positive effect [30]. Dasan et al. (2015) highlighted that a key difference between compassion fatigue and satisfaction among consultants working in hospitals and intensive care units was the degree of varied work, team positivity, and patient empathy, which can lead to increased job satisfaction. In an intensive care setting, there was an “overjoyed” feeling when a former patient returned to visit, although this was tempered by visits from those bereaved [17].
Vicarious trauma is evident particularly within the pre-hospital environment, which may explain the largest reductions in anxiety shown in those remote from the scene. Rauvola et al. (2019) highlight that call takers who hear or read job details may experience a large degree of vicarious trauma [7]. Rauvola et al. (2019) conducted a qualitative review that differentiated between vicarious trauma, compassion fatigue, and secondary traumatic stress [7, 31]. Secondary traumatic stress occurs when the caregiver, whose client is experiencing a traumatic event, exhibits symptoms of post-traumatic stress disorder [32]. Gender, age, education, and occupational role differences may influence the manifestation of secondary traumatic stress [12], a phenomenon reported in both civilian and military settings [32]. Willis et al. (2020) suggested that ambulance call-takers are at risk of cumulative and vicarious trauma [33], and a small study by Powell (2022) highlighted that positive feedback from supportive peers can enhance their well-being [16]. Similarly, quality of life in the workplace and coping skills are crucial factors in promoting positive clinical performance of all healthcare professionals [28, 34, 35]. Armour and Ross (2017) found that pilot well-being is heavily influenced by operational pressure rather than combat-related issues [15]. Although this study focused on drone pilots, there are similarities to the experiences and work patterns of HEMS pilots, who are also exposed to traumatic events.
The questionnaire was anonymous; however, participants’ familiarity with the researcher may have introduced a Hawthorne effect [36], as it led to a dual role [37]. This may potentially influence participants’ behaviour when completing the questionnaire and is an ongoing debate in practice-based healthcare settings such as counselling due to ethical considerations [37]. However, this role allows researchers to produce effective and contextual research findings [38]. The method used to capture the data was a strength of the study and enabled the collection of an anonymised dataset in a secure and timely manner [39]. In combination with this quantitative approach, the inclusion of qualitative free-text responses allowed a contextual understanding of the scores reported. This also provides tangible objectives for service improvement within PFAS. Future research may benefit from a mixed-methods qualitative approach, as this would allow for more detailed exploration of an individual’s perception. Researchers may consider individual focus groups or interview-based methodologies [40] from a grounded theory methodology to inductively generate theory using qualitative data [41]. Further, this methodology would enable researchers to further explore described feelings of ‘intimidation’ and ‘overwhelming emotions’ stated in the free text responses. Future study would also enable the service to strengthen PFAS, whilst ensuring clinicians are not exposed to additional stressors and create anxiety through the process itself.
Limitations
The methodological approach has limitations similar to other retrospective studies [38]. The GAD-7 (Generalised Anxiety Disorder-7) measures generalised anxiety rather than short-term situational anxiety. Consequently, it may not fully capture the immediate or transient anxiety experienced in specific, situational contexts such as during patient interactions [22, 42]. This limitation suggests that whilst the GAD-7 provides valuable insights into overall anxiety levels, it may not completely reflect the nuanced, context-specific emotional responses identified in the study. One aspect of this literature review explored other psychological inventory, or tools used to measure stress and anxiety. The State and Trait Anxiety Inventory (STAI) consists of 40 self-reported items on a 4-point Likert scale, originally developed by the psychologist Charles Spielberger in 1970, and revised in 1983. The STAI measures two types of anxiety. Firstly, it measures the ‘state’ of your perceived anxiety at a given moment. Second, it measures the ‘trait’ of anxiety in day-to-day living. The higher the scores the higher the associated anxiety. Despite its perceived utility for ‘state’ anxiety it was felt that an inventory of 40 items may lead to incompletion and reduce the response rate. Despite the above limitations of the chosen GAD-7 it was felt that the structured literature search in combination with exert opinion amongst stakeholders, although unvalidated, were deemed less likely to be affected by extrinsic confounding or temporal factors affecting participants general anxiety state at the time the questionnaire was administered.
In addition, the retrospective nature of the study raises concerns about the accuracy of participants’ recollections over time [43], such as the potential for recall bias [43]. Respondents were asked to recall their perspective on their level of anxiety on two occasions after the visit, and literature suggests that responses may have been either heightened or reduced depending on the individual’s ability to recall the event [43]. These studies indicate that anxiety and depression are linked to both explicit and implicit memory biases, which are defined as the tendency to preferentially recall emotionally negative information at the conscious and subconscious levels, respectively [44]. This would have led to increased anxiety scores in the pre- and post-test and is important to recognise as a methodological limitation in the study design. In addition, contextualised statements were drawn from an unvalidated expert consensus. Future collaborative recommendations and consensus on the use of these statements should be prospectively undertaken [29, 45].
Conclusion
Following this service evaluation, we can hypothesise that aftercare services play a structurally important role within the aftercare setting. Future research should focus on affirming the correct tool to measure anxiety and prospectively evaluate these methods across collaborative pre-hospital services. Considering the responsibility of these services to mitigate the effects of potential traumatic experiences for employees during patient visits and in the context of patient and family aftercare services, it is essential to explore whether anxiety levels in individuals can be reduced before and after patient aftercare visits.
Supplementary Information
Supplementary Material 1. Pre- and post-patient aftercare visit questionnaires.
Supplementary Material 2. Structured literature review undertaken to inform the Contextualised Statements included.
Acknowledgements
The study team thanks Dr Mary Halter at St. Georges University, London, for her continued support and supervision. The team are also grateful for the contribution and support of colleagues at the Air Ambulance Charity Kent Surrey and Sussex from the inception of the PFAS through to the completion of this study. We would specifically like to thank those individuals whom participated in the study. We also thank the patients themselves, and indeed their families who have taken their time to support, and continue to support the growth and development of the PFAS. We would also like to express a special thank you to Katie Robson.
Patient and public involvement
The Research and Innovation Department at KSS actively involve patient representatives in every aspect of strategic delivery. Patient representatives acted as stakeholders in the implementation of the PFAS through the Board of Trustees.
Abbreviations
- HEMS
Helicopter Emergency Medical Services
- UK
United Kingdom
- NHS
National Health Service
- NICE
National Institute of Clinical Excellence
- ICU
Intensive Care Unit
- GAD-7
Generalised Anxiety Disorder Score
- EMT
Emergency Medical Technician
- EMS
Emergency Medical Service
- STAI
State and Trait Anxiety Inventory
- BAI
Becks Anxiety Inventory
- HAS
Hamilton Anxiety Score
- REDCap
Research Electronic Data Capture
- PFAS
Patient and Family Aftercare Services
- MTC
Major Trauma Centre
- TU
Trauma Unit
- RSI
Rapid Sequence Induction
- EOC
Emergency Operations Centre
- RCT
Randomised Controlled Trials
- PIS
Patient Information Sheet
- ROB
Risk of Bias
- SRQR
Standards for Reporting Qualitative Research
- HRA
Health Research Authority
- REC
Research Ethics Committee
- SGREC
St Georges University Ethical Committee
- TRiM
Trauma Risk Management
- VAS
Visual Analogue Scale
- HSSIB
Health Services Safety Investigation Board
Authors’ contributions
All authors have fulfilled the ICMJE criteria for authorship. SP/ST/JG/AAR conceived of the study. SP/ST retrieved data. SP/JG performed statistical analyses. SP/JG/RL drafted the manuscript. AAR/RL/LC provided critical contextual oversight. All authors contributed to the interpretation of the results. All authors have read and approved the final manuscript.
Funding
Not applicable.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The Health Research Authority (HRA) Medical Research Council decision tool was used to establish the need for Research Ethical Committee (REC) approval. The toolkit advised that REC approval would not be required. St. Georges University Ethical Committee (SGREC) was required, and the study was registered (ID-SE0123). Prior to commencing the study, the KSS Research and Innovation Committee approved the protocol and the research materials.
A ‘Consent to Participate’ form was appended to the patient information sheet (PIS) that was installed into REDCap. Respondent completion of this was essential prior to study inclusion to ensure maintenance of anonymity and confidentiality. Respondents were advised that no identifiable information should be discussed within the questionnaire itself, including any reference to colleagues or patients. All data were immediately checked and anonymised thus mitigating any risk to confidentiality [46, 47]. The researcher reserved the right to withdraw and delete parts of the questionnaire if confidentiality was compromised. Due to the nature of the questions asked and the minimal opportunity to write free text, breaking confidentiality was unanticipated and considered low risk. In addition, respondents have organisational access to a governed TRiM service, which was highlighted to all participants prior to commencing the study. To maintain a robust research process, the Standards Reporting Qualitative Research (SRQR) was used [25].
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Cole E. The national major trauma system within the United Kingdom: inclusive regionalized networks of care. Emerg Crit Care Med. 2022;2(2):76. [Google Scholar]
- 2.Sanger H. How early is early? When should rehabilitation begin in critical illness? J Assoc Chart Physiother Respir Care Vol 52 Issue 1 2020 [Internet]. 2020 Sep 1 [cited 2024 Feb 1]; https://www.acprc.org.uk/publications/acprc-journal/2020-journal-vol-52/how-early-is-early-when-should-rehabilitation-begin-in-critical-illness/.
- 3.Connolly B, Milton-Cole R, Adams C, Battle C, McPeake J, Quasim T, et al. Recovery, rehabilitation and follow-up services following critical illness: an updated UK national cross-sectional survey and progress report. BMJ Open. 2021;11(10):e052214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bonifacio GB, Ward NS, Emsley HCA, Cooper J, Bernhardt J. Optimising rehabilitation and recovery after a stroke. Pract Neurol. 2022;22(6):478–85. [DOI] [PubMed] [Google Scholar]
- 5.Kirby K, Caswell K, Petheram J, Hyde P, Crouch R. Mapping the patient and family Liaison Role in UK Helicopter Emergency Medical services: a service evaluation. Air Med J. 2022;41(5):458–62. [DOI] [PubMed] [Google Scholar]
- 6.Phung VH, Sanderson K, Pritchard G, Bell F, Hird K, Wankhade P, et al. The experiences and perceptions of wellbeing provision among English ambulance services staff: a multi-method qualitative study. BMC Health Serv Res. 2022;22(1):1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rauvola RS, Vega DM, Lavigne KN. Compassion fatigue, secondary traumatic stress, and vicarious traumatization: a qualitative review and research agenda. Occup Health Sci. 2019;3(3):297–336. [Google Scholar]
- 8.Sapra A, Bhandari P, Sharma S, Chanpura T, Lopp L. Using generalized anxiety Disorder-2 (GAD-2) and GAD-7 in a primary care setting. Cureus. 2020;12(5):e8224. [DOI] [PMC free article] [PubMed]
- 9.Durand AC, Bompard C, Sportiello J, Michelet P, Gentile S. Stress and burnout among professionals working in the emergency department in a French university hospital: prevalence and associated factors. Work J Prev Assess Rehabil. 2019;63(1):57–67. [DOI] [PubMed] [Google Scholar]
- 10.Miller E. The prevalence of stress and burnout in UK emergency ambulance service workers and its impact on their mental health and well-being. Br Paramed J. 2021;5(4):62–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Charzyńska E, Habibi Soola A, Mozaffari N, Mirzaei A. Patterns of work-related stress and their predictors among emergency department nurses and emergency medical services staff in a time of crisis: a latent profile analysis. BMC Nurs. 2023;22(1):98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carmassi C, Gesi C, Corsi M, Cremone IM, Bertelloni CA, Massimetti E et al. Exploring PTSD in emergency operators of a major University Hospital in Italy: a preliminary report on the role of gender, age, and education. Ann Gen Psychiatry. 2018;17:17. [DOI] [PMC free article] [PubMed]
- 13.Hird K, Bell F, Mars B, James C, Gunnell D. OP6 an investigation into suicide amongst ambulance service staff. Emerg Med J. 2019;36(1):e3–3. [Google Scholar]
- 14.Bouillon-Minois JB, Outrey J, Pereira B, Adeyemi OJ, Sapin V, Bouvier D, et al. The impact of Job-Demand-Control-Support on leptin and ghrelin as biomarkers of stress in Emergency Healthcare Workers. Nutrients. 2022;14(23):5009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Armour C, Ross J. The health and well-being of military drone operators and intelligence analysts: a systematic review. Mil Psychol. 2017;29(2):83–98. [Google Scholar]
- 16.Powell C, Fylan B, Lord K, Bell F, Breen L. A qualitative analysis of stressors affecting 999 ambulance call handlers’ mental health and well-being. Int J Emerg Serv. 2022;12(2):231–42. [Google Scholar]
- 17.Dasan S, Gohil P, Cornelius V, Taylor C. Prevalence, causes and consequences of compassion satisfaction and compassion fatigue in emergency care: a mixed-methods study of UK NHS consultants. Emerg Med J EMJ. 2015;32(8):588–94. [DOI] [PubMed] [Google Scholar]
- 18.Reid BO, Haugland H, Abrahamsen HB, Bjørnsen LP, Uleberg O, Krüger AJ. Prehospital stressors: a cross-sectional study of Norwegian Helicopter Emergency Medical Physicians. Air Med J. 2020;39(5):383–8. [DOI] [PubMed] [Google Scholar]
- 19.Palinkas LA, Horwitz SM, Green CA, Wisdom JP, Duan N, Hoagwood K. Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Adm Policy Ment Health. 2015;42(5):533–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baker T. A changing view on patient safety: how the Healthcare Safety Investigation Branch has brought system-focused investigations to the fore. Future Healthc J. 2023;10(1):10–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Patridge EF, Bardyn TP. Research Electronic Data Capture (REDCap). J Med Libr Assoc JMLA. 2018;106(1):142–4. [Google Scholar]
- 22.Kertz S, Bigda-Peyton J, Bjorgvinsson T. Validity of the generalized anxiety Disorder-7 scale in an acute psychiatric sample. Clin Psychol Psychother. 2013;20(5):456–64. [DOI] [PubMed] [Google Scholar]
- 23.Generalized anxiety disorder questionnaire |. Diagnosis | Generalized anxiety disorder | CKS | NICE [Internet]. [cited 2024 Jan 18]. https://cks.nice.org.uk/topics/generalized-anxiety-disorder/diagnosis/generalized-anxiety-disorder-questionnaire/.
- 24.Plummer F, Manea L, Trepel D, McMillan D. Screening for anxiety disorders with the GAD-7 and GAD-2: a systematic review and diagnostic metaanalysis. Gen Hosp Psychiatry. 2016;39:24–31. [DOI] [PubMed] [Google Scholar]
- 25.Jordan P, Shedden-Mora M, Löwe B. Psychometric analysis of the generalized anxiety disorder scale (GAD-7) in primary care using modern item response theory. PLoS ONE. 2017;12:183. [DOI] [PMC free article] [PubMed]
- 26.Richards SH, Campbell JL, Walshaw E, Dickens A, Greco M. A multi-method analysis of free-text comments from the UK General Medical Council Colleague questionnaires. Med Educ. 2009;43(8):757–66. [DOI] [PubMed] [Google Scholar]
- 27.Humble N, Mozelius P. Content analysis or thematic analysis: Similarities, differences and applications in qualitative research. Vol. 21, European Conference on Research Methodology for Business and Management Studies. 2022.
- 28.Notarnicola I, Stievano A, Gregorio R, Trullo R, Appolloni P, Polletta A, et al. The role of coping styles and stressors on professional quality of life (Pro-QoL) among in a health emergency operating center workers: a preliminary cross-sectional study. Prof Inferm. 2020;73:306–13. [DOI] [PubMed] [Google Scholar]
- 29.Ramage L, McLachlan S, Williams K. Determining the top research priorities in UK prehospital critical care: a modified Delphi study. Emerg Med J. 2023;40(4):271–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Burnett C, Jeter L, Duva I, Giordano N, Eldridge R. Resilience training in the Emergency Department. J Nurse Pract. 2023;19(9):104760. [Google Scholar]
- 31.Greinacher A, Nikendei A, Kottke R, Wiesbeck J, Herzog W, Friederich HC, et al. Secondary traumatisation in psychosocial emergency care personnel-A longitudinal study accompanying German trainees. Health Soc Care Community. 2022;30(3):957–67. [DOI] [PubMed] [Google Scholar]
- 32.Cieslak R, Anderson V, Bock J, Moore BA, Peterson AL, Benight CC. Secondary traumatic stress among mental health providers working with the military: prevalence and its work- and exposure-related correlates. J Nerv Ment Dis. 2013;201(11):917–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Willis CD, Cameron PA, Bernard SA, Fitzgerald M. Cardiopulmonary resuscitation after traumatic cardiac arrest is not always futile. Injury. 2006;37(5):448–54. [DOI] [PubMed] [Google Scholar]
- 34.Ducar DM, Penberthy JK, Schorling JB, Leavell VA, Calland JF. Mindfulness for healthcare providers fosters professional quality of life and mindful attention among emergency medical technicians. Explore N Y N. 2020;16(1):61–8. [DOI] [PubMed] [Google Scholar]
- 35.Cardile D, Corallo F, Ielo A, Cappadona I, Pagano M, Bramanti P, et al. Coping and quality of life differences between Emergency and Rehabilitation Healthcare Workers. Healthc Basel Switz. 2023;11(16):2235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Allen RL, Davis AS. Hawthorne Effect. In: Goldstein S, Naglieri JA, editors. Encyclopedia of Child Behavior and Development [Internet]. Boston, MA: Springer US; 2011 [cited 2024 Jan 23]. pp. 731–2. 10.1007/978-0-387-79061-9_1324.
- 37.Fleet D, Burton A, Reeves A, DasGupta MP. A case for taking the dual role of counsellor-researcher in qualitative research. Qual Res Psychol. 2016;13(4):328–46. [Google Scholar]
- 38.Bourdeau B. Dual Relationships in Qualitative Research. Qual Rep. 2000. 10.46743/2160-3715/2000.2081.
- 39.Garcia KKS, Abrahão AA. Research Development using REDCap Software. Healthc Inf Res. 2021;27(4):341–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hammarberg K, Kirkman M, de Lacey S. Qualitative research methods: when to use them and how to judge them. Hum Reprod. 2016;31(3):498–501. [DOI] [PubMed] [Google Scholar]
- 41.Chun Tie Y, Birks M, Francis K. Grounded theory research: a design framework for novice researchers. SAGE Open Med. 2019;7:2050312118822927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Monteiro RP, Nascimento BS, Monteiro TMC, da Silva PDG, Ferreira AJC. Psychometric evidence of the 7-Item generalized anxiety disorder questionnaire in Brazil. Int J Ment Health Addict. 2022;20(2):1023–34. [Google Scholar]
- 43.Talari K, Goyal M. Retrospective studies - utility and caveats. J R Coll Physicians Edinb. 2020;50(4):398–402. [DOI] [PubMed] [Google Scholar]
- 44.Hakamata Y, Mizukami S, Izawa S, Okamura H, Mihara K, Marusak H, et al. Implicit and explicit emotional memory recall in anxiety and depression: role of basolateral amygdala and cortisol-norepinephrine interaction. Psychoneuroendocrinology. 2022;136:105598. [DOI] [PubMed] [Google Scholar]
- 45.Bartels EM. How to perform a systematic search. Best Pract Res Clin Rheumatol. 2013;27(2):295–306. [DOI] [PubMed] [Google Scholar]
- 46.Rodrigues V. Publication and reporting biases and how they impact publication of research. Ed Insights29-10-2013 [Internet]. 2013 Oct 29 [cited 2017 Nov 26]; https://www.editage.com/insights/publication-and-reporting-biases-and-how-they-impact-publication-of-research.
- 47.O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med J Assoc Am Med Coll. 2014;89(9):1245–51. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material 1. Pre- and post-patient aftercare visit questionnaires.
Supplementary Material 2. Structured literature review undertaken to inform the Contextualised Statements included.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.