Fig. 3 │. Typical pattern of GIST response and evolution during TKI treatment.
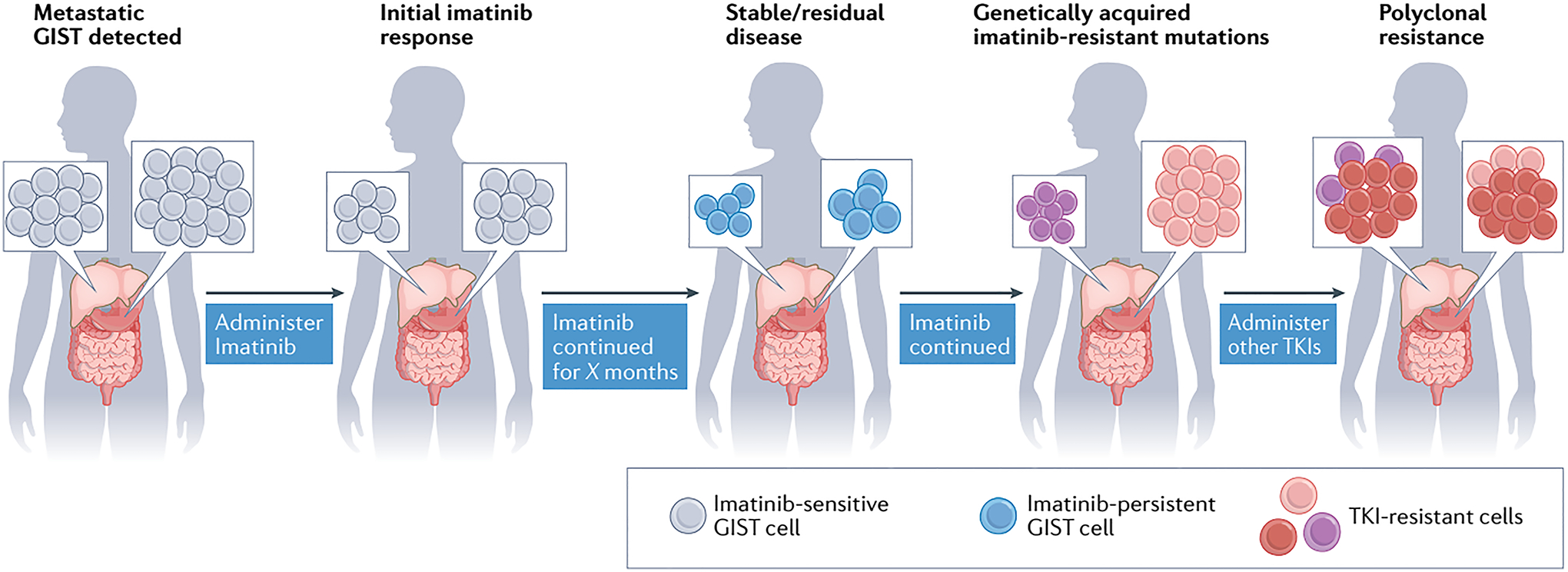
Patients diagnosed with metastatic KIT-mutant gastrointestinal stromal tumour (GIST; lesions indicated by grey cells) are initially treated with the KIT-targeting tyrosine kinase inhibitor (TKI) imatinib. Typically, imatinib induces tumour shrinkage by inducing apoptosis of GIST cells; however, not all GIST cells are eradicated, with a fraction persisting throughout treatment by entering a non-proliferative, quiescent state (imatinib-persistent GIST cells, shown in blue). Some of these persistent GIST cells will eventually acquire genetic mutations that confer resistance to imatinib, leading to tumour outgrowth and disease progression (pink and purple cells). Other KIT TKIs can be administered sequentially to patients with GISTs harbouring resistance mutations. Nevertheless, genetically heterogeneous subclones can arise across tumour lesions (shown as pink, purple and red cells), leading to polyclonal resistance of the tumours to multiple TKIs. Both intertumour and intratumour heterogeneity can be found in patients with TKI-resistant GIST. Intertumour heterogeneity is illustrated by the presence of different imatinib-resistant subclones, either pink or purple, across the two lesions. In the rightmost panel, intratumour heterogeneity is also depicted by the co-existence within a single lesion of newly emergent red subclones together with the pink or purple cell population.
