FIGURE 3.
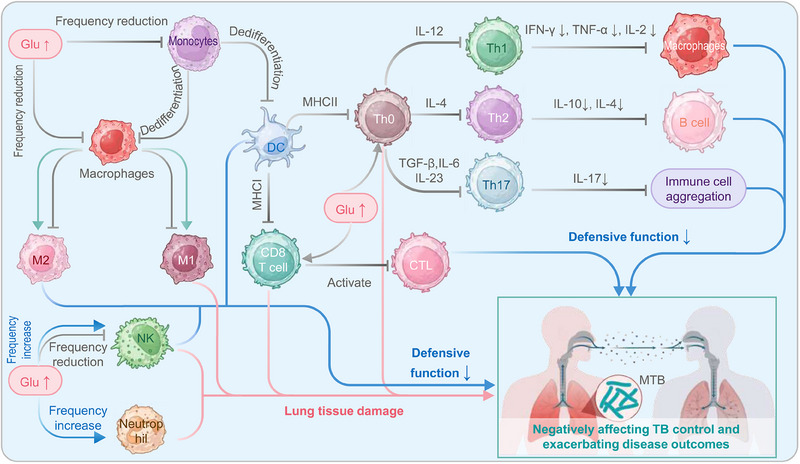
The influence of DM on the immune system of TB patients. On one hand, TB patients' elevated blood glucose levels hinder the differentiation of monocytes into DCs and macrophages. The reduction in DCs leads to a decline in antigen presentation and activation of CD4+ T cells (Th0). Consequently, the diminished Th0 differentiation results in decreased secretion of corresponding cytokines, affecting the activation of macrophages and humoral immunity and impairing the recruitment of immune cells. This poses a significant problem for TB patients as they are more susceptible to hyperglycemia. Additionally, high blood glucose levels also impact the polarization of macrophages, enhancing M2 activation and reducing M1 activation and affecting the frequency and cytotoxicity of DCs and natural killer (NK) cells. These effects compromise the ability to clear Mycobacterium tuberculosis infection. On the other hand, high blood glucose levels can also lead to increased M1 activation, decreased M2 activation, and increased frequency and activity of NK cells, neutrophils, CD4+ T lymphocytes, and CD8+ T lymphocytes, contributing to pathological damage in the host. Overall, diabetes disrupts the normal function and frequency of immune cells, negatively impacts TB control, and exacerbates disease outcomes. CTL, cytotoxic T lymphocyte; DC, dendritic cells; DM, diabetes mellitus; Glu, glutamate; IFN, interferon; IL, interleukin; NK cell, natural killer cell; MHC, major histocompatibility complex; TB, tuberculosis; TNF, tumor necrosis factor.
