Abstract
Objective:
The purpose of this randomized clinical study was to investigate the influence of occlusal surface reduction on postendodontic pain.
Methodology:
Sixty patients were included with a diagnosis of acute irreversible pulpitis and acute apical periodontitis and divided randomly into two groups. In the intervention group, occlusal surfaces were reduced and left intact in the control group. Postoperative pain was evaluated at the 6th, 12th, 24th, and 48th h after the root canal instrumentation and 6th and 12th h following obturation using visual analog scale. Data were evaluated using the Chi-square test, t-test, Friedman test, Mann–Whitney U-test, and Wilcoxon rank test.
Results:
Postoperative pain levels in both groups were reduced significantly over the time period evaluated, however, between the two groups, there was no difference evident.
Conclusion:
Occlusal surface reduction did not influence the pain following root canal instrumentation and obturation.
Keywords: Occlusal reduction, postoperative pain, randomized clinical trial
INTRODUCTION
Pain following an endodontic procedure remains a critical distress for both patients and clinicians.[1] Incidence of postendodontic pain ranges from 3% to 80% and it occurs immediately after the procedure, lasting up to several days; if not managed, it may escalate the anxiety and fear of the patient.[2,3] Thus, it is very crucial for clinicians to manage the postoperative pain in patients undertaking endodontic procedures.[4]
Postoperative endodontic pain is of multifactorial origin.[2] Mechanical factors associated with instrumentation, chemical factors related to irrigation, and microbial factors elevate the inflammatory mediators, that excite/sensitize the nerve endings, resulting in the activation of algesic mediators.[5,6]
Various treatment approaches have been in clinical practice for managing postoperative endodontic pain that includes the use of preoperative medication,[7] administration of long-acting anesthesia,[8] shaping the root canal with rotary instruments,[9] disinfecting the root canals with sodium hypochlorite (NaOCl), and placement of intracanal medication,[10] obturating the root canal with cold lateral compaction technique,[11] light-mediated photo-biomodulation therapy,[12] intracanal cryotherapy application,[13] and occlusal reduction.[14,15,16]
The biological rationale behind the occlusal surface reduction is a significant reduction of mechanical allodynia by minimizing the provoking of sensitized nociceptors.[17] However, the clinical impact of occlusal reduction in managing postoperative endodontic pain remains controversial. Several investigators[14,15,16] have suggested that occlusal surface reduction decreases the postoperative pain following endodontic procedure; however, Creech et al.,[18] Jostes and Holland,[19] Parirokh et al.,[20] and Arslan et al.[21] stated that occlusal reduction does not significantly produce any improvement in managing postoperative endodontic pain.
Recently Nguyen-Nhon et al.[1] and Shamszadeh et al.[4] also mentioned that there is a lack of clinical evidence about the significance of occlusal surface reduction on postendodontic pain in teeth with different pulpal and periapical diagnoses in their systematic review and meta-analysis.
Hence, the objective of this randomized double-blinded clinical study was to assess the influence of occlusal surface reduction on postendodontic pain in maxillary and mandibular posterior teeth (molars and premolars). The null hypothesis tested was that occlusal surface reduction does not influence postendodontic pain.
METHODOLOGY
Clinical protocol approval and registration
The study protocol was accepted by the ethical committee of Sri Ramachandra Institute of Higher Education and Research (Reference no: IEC/19/JUL/152/50). This study was enrolled in the National Clinical Trials Registry (CTRI/2019/09/021104) and reported following the preferred reporting items for randomized trials in endodontics 2020 guidelines.[22]
Sample size calculation
With 80% statistical power and 5% alpha error, a minimum sample size requirement of 22 per group was derived.[23] Considering attrition/dropout in the study, it was decided to enroll at least 30 patients in both treatment groups.
Setting/environment of the study
This study was planned as a prospective, parallel, randomized double-blinded clinical study with a total of 78 patients evaluated for eligibility from the pool of patients referred to outpatient clinics of the Department of Conservative Dentistry and Endodontics, Sri Ramachandra Dental College and Hospital, from September 2019 to March 2023.
Inclusion criteria
Systemically healthy adult patients (ASA I) aged between 18 and 50 years with spontaneous moderate-to-severe preoperative pain and painful response affiliated with mastication in posterior teeth were included and diagnosed with acute irreversible pulpitis (pulpal) and acute apical periodontitis (periapical). The diagnosis was confirmed by a continuous exaggerated response lasting beyond 10 s with moderate-to-severe pain to cold and electric pulp test after the removal of stimuli[20] along with a painful response to percussion with radiographic evidence of slight periodontal ligament space widening and absence of periapical radiolucency.[15,16]
Exclusion criteria
Patients categorized other than ASA I, pregnant women, teeth with no opposing teeth/occlusal contact or premature contact, patients with occlusal disorders, those who took preoperative analgesic medication, patients with periapical or periodontal abscess, periodontal probing or pocket depth more than 5 mm, nonrestorable teeth, and previously root canal treated teeth were excluded.[15,16,20]
All the included patients were briefed about the clinical procedures, number of visits, possible discomforts/risks, and benefits associated. Informed consent was signed and a copy was given to all the included patients.
Randomization
To eliminate the bias of investigators and also to distribute the patients uniformly in the treatment groups, randomization was developed. Permuted block randomization was carried out for two groups (intervention: occlusal reduction and control: nonocclusal reduction) with 30 patients in each group using computer-generated randomization (Research randomizer-Version 4.0 Computer Software) with an allocation ratio of 1:1 and all patients were given an individual number which was placed separately in a sealed envelope. Each patient selected one sealed envelope and based on the number; they were allotted to one of the two treatment groups. Throughout the study, patients were unaware of their assigned group (intervention: occlusal reduction and control: nonocclusal reduction).
Preoperative pain assessment
The patient’s preoperative pain levels were documented using visual analog scale (VAS) score sheet. Patients were described and instructed about the VAS scoring sheet and how to use it. All the included patients rated their preoperative pain before the commencement of the clinical procedure ranging from 0 to 9 (0, no pain; 1–3, mild pain; 4–6, moderate pain; and 7–9, severe pain).[20]
Clinical procedures
Two-visit endodontic procedures were performed. During the first appointment, all the included tooth was anesthetized with two cartridges (3.6 Ml) of local anesthesia (2% lignocaine with 1:100,000 adrenaline). Mandibular nerve block was performed for mandibular posteriors and for maxillary posteriors, buccal and palatal infiltration was given.[21]
Under rubber dam isolation, after the complete elimination of caries or existing faulty restoration, access opening was done and canal patency was achieved with #10 K-File (Mani Inc., Utsunomiya, Japan). Using an electronic apex locator (Root ZX, J. Morita USA, Irvine, CA, USA), the working length was determined at 0.5 mm short of the “0” reading and confirmed with a digital radiograph. Shaping of the canal was done in a crown-down manner with rotary instruments using an endodontic motor.
Master apical preparation size for palatal root with one canal (maxillary molar), distal root with one canal (mandibular molar), and premolars with single canal in both maxillary and mandibular teeth was F3 (#30.09) ProTaper gold (PTG). Buccal and lingual/palatal canals of the molars and premolars were instrumented up to size F2 PTG (#25.08). Between instrumentation, 2 ml of 3% NaOCl was irrigated, after final instrumentation, 5 mL of 17% ethylenediaminetetraacetic acid for a minute, and a final rinse with 5 mL of 3% NaOCl was done in all the canals and dried with paper points. At the end of the shaping and cleaning procedure, without placing intracanal medication,[14,15,16] access cavity was sealed with provisional restorative cement.
Using the articulating paper, the occlusal surface was evaluated and patients in the intervention group (occlusal surface reduction) received a reduction of both functional and nonfunctional cuspal contact along with the marginal ridges under copious water spray in a high-speed handpiece with round-end tapered diamond abrasive (TR 14 – Mani Inc., Utsunomiya, Japan). After the reduction, occlusal surfaces were re-evaluated using articulating paper to confirm the absence of contact. In the control group (nonocclusal reduction), all the occlusal contacts were left untouched. However, to ascertain the patients in the control group, copious water spray high-speed handpiece was activated in their mouth without contacting the occlusal surface.[16]
During the second appointment (3 days later), under rubber dam isolation, provisional restorative cement was removed followed by canal irrigation and dried with paper points similar to the first appointment and obturated using cold lateral compaction technique with gutta-percha and resin sealer (AH Plus; Dentsply DeTrey, Konstanz, Germany). After obturation, occlusion was re-evaluated to confirm the absence of contact in the intervention group and left intact in the control group. Patients were then recalled and postendodontic restoration was given.
Postoperative pain assessment
The patients were informed to complete their VAS scoring sheet for postoperative endodontic pain at the 6th, 12th, 24th, and 48th h after the first visit (after root canal instrumentation) and the 6th and 12th h following the second visit (after obturation). One of the co-investigators who was not aware of the patient treatment groups (intervention or control) contacted them at each time interval over the phone to remind them of scoring the postendodontic pain.
Symptomatic patients were advised to take analgesics (ibuprofen 600 mg) if they were in need of pain relief[14] and they were also informed to record the intake of analgesic medication in the VAS scoring sheet.[20]
Statistical analysis
Statistical analysis was performed with IBM SPSS software (IBM SPSS Statistics for Windows, Version 20.0 Armonk, NY, USA: IBM Corp). To compare the demographics of the patients, type of teeth, and analgesic intake among the groups, t-test and Chi-square test were used. Mann–Whitney U-test was performed to compare the VAS scores between the two treatment groups. Friedman test and Wilcoxon signed-rank test were done to assess the pain reduction following instrumentation and obturation. A value of P ≤ 0.05 was considered to be statistically significant.
RESULTS
Sixty patients were included and randomly allotted to either the occlusal reduction or nonocclusal reduction group. Thirteen patients were excluded since they did not give back their VAS scoring sheet and also did not come for further treatment. The remaining 47 patients (25 in intervention and 22 in the control group) completed the study, of which 20 were males (10 in both the treatment groups) and 27 were females (15 in occlusal reduction and 12 in nonocclusal reduction). The age group was from 19 to 48 years with a mean of 32.36 years in the intervention and 31.77 years in the control group. With regard to the type of teeth included, 19 were premolars (11 in the intervention and 8 in the control group) and 28 were molars (14 in the intervention and 14 in the control group). Patient distribution during each phase of the study was shown in the PRIRATE 2020 flowchart [Figure 1].
Figure 1.
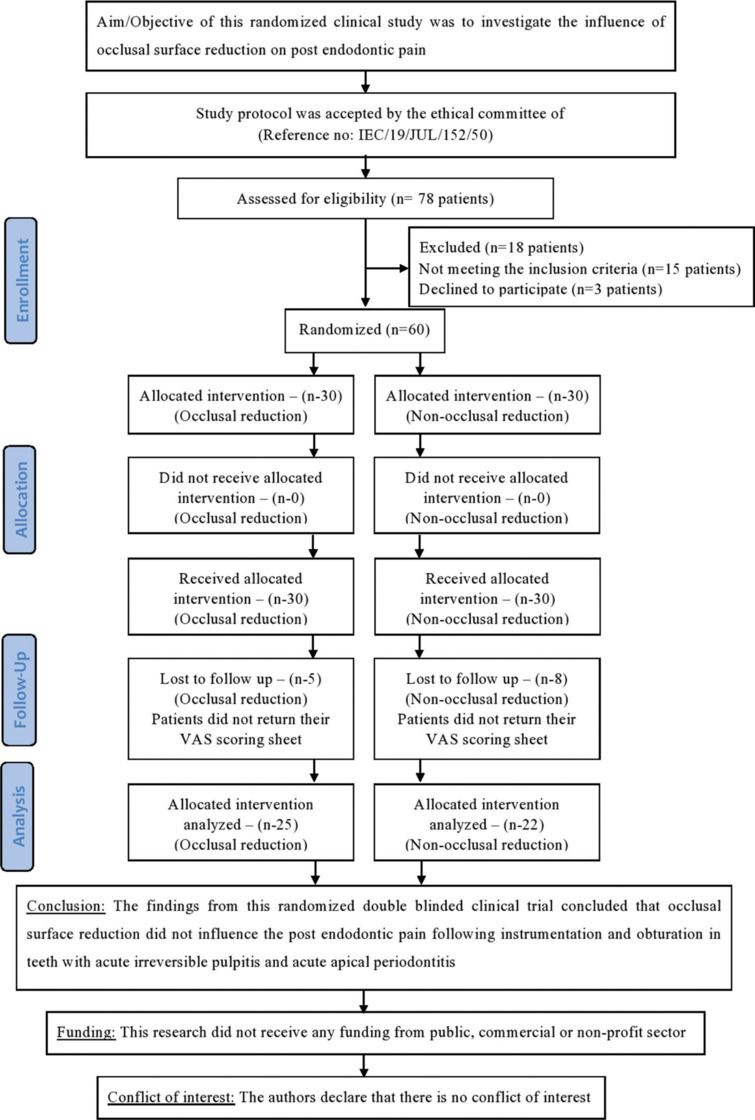
2020 PRIRATE Flowchart
Patient’s demographics, type of included teeth, and preoperative pain does not have any significant difference among the treatment groups [Tables 1 and 2]. The postoperative pain levels significantly reduced in both groups over the time period following instrumentation and obturation, but there was no significance in pain reduction and analgesics taken by patients between the two groups [Tables 3 and 4].
Table 1:
Demographic data and tooth type
| Variables | Intervention - OR (n=25), n (%) | Control - NOR (n=22), n (%) | P |
|---|---|---|---|
| Age (years), mean±SD | 32.36±8.05 | 31.77±8.44 | 0.80 |
| Gender | |||
| Male | 10 (40) | 10 (45.5) | 0.85 |
| Female | 15 (60) | 12 (54.5) | |
| Tooth type | |||
| Premolar | 11 (44) | 8 (36.4) | 0.82 |
| Molar | 14 (56) | 14 (63.6) |
OR: Occlusal reduction, NOR: Non-OR, SD: Standard deviation
Table 2:
Intensity of patient’s preoperative pain
| Time period | Group | Mean rank | Sum of ranks | P |
|---|---|---|---|---|
| Preoperative pain | OR | 23.88 | 597.00 | 0.94 |
| NOR | 24.14 | 531.00 |
OR: Occlusal reduction, NOR: Non-OR
Table 3:
Intensity of patients postoperative pain at different time intervals
| Time period | Group | Mean rank | Sum of ranks | P |
|---|---|---|---|---|
| Postinstrumentation pain (h) | ||||
| 6th | OR | 25.92 | 648.00 | 0.29 |
| NOR | 21.82 | 480.00 | ||
| 12th | OR | 24.48 | 612.00 | 0.79 |
| NOR | 23.45 | 516.00 | ||
| 24th | OR | 22.84 | 571.00 | 0.52 |
| NOR | 25.32 | 557.00 | ||
| 48th | OR | 23.98 | 599.50 | 0.99 |
| NOR | 24.02 | 528.50 | ||
| Postobturation pain (h) | ||||
| 6th | OR | 22.00 | 550.00 | 0.27 |
| NOR | 26.27 | 578.00 | ||
| 12th | OR | 23.52 | 588.00 | 0.79 |
| NOR | 24.55 | 540.00 |
OR: Occlusal reduction, NOR: Non-OR
Table 4:
Incidence of analgesic intake
| Group | Analgesic taken | n (%) | P |
|---|---|---|---|
| OR | No | 19 (76.0) | 0.79 |
| Yes | 6 (24.0) | ||
| NOR | No | 16 (72.7) | |
| Yes | 6 (27.3) |
OR: Occlusal reduction, NOR: Non-OR
DISCUSSION
Management of postoperative pain in endodontics is very critical, which may be appraised as an important source of patient satisfaction[4] and occlusal reduction has been suggested in managing the postendodontic pain.[14,15,16]
Homogenized treatment protocol can eliminate the influence of intraoperative variables on analyzing the postendodontic pain[16] and various researchers have also insisted on the need of well-designed randomized clinical trials to provide strong recommendations about the occlusal surface modification in postendodontic pain.[1,4] Hence, the current study was designed as a double-blinded randomized clinical trial to evaluate the influence of occlusal reduction on postendodontic pain.
Preoperative pain, pulpitis, tenderness on percussion, the absence of periapical radiolucency, molar teeth, and mandibular teeth were the strong predictors of postendodontic pain.[2,14] Thus, in our present study, patients reported with all the aforementioned factors were included. Sensibility tests (cold and electric pulp testing) were performed to determine the pulpal status and it was confirmed with hemorrhage in the pulp chamber following access opening[20] since it is considered the gold standard in recognizing the pulpal status.[24] In our study, all the included patients had bleeding upon the access opening indicating the intact blood supply of pulp.
Previously Arslan et al.[21] have evaluated the effect of occlusal reduction on postendodontic pain in maxillary and mandibular molars; Emara et al.[15] and Ahmed et al.[16] have evaluated only the mandibular posteriors (molars and premolars). Furthermore, most of the previous researchers evaluated the significance of occlusal surface reduction following root canal instrumentation pain alone.[14,18,19,20,21,25,26,27,28] To the best of our literature search, the present randomized controlled clinical trial is the first study to evaluate the influence of occlusal surface reduction on postendodontic pain following root canal instrumentation and obturation in both the maxillary and mandibular posterior teeth (molars and premolars).
The choice of endodontic shaping instrument plays a critical role in postendodontic pain.[9] Recently published meta-analysis of a randomized clinical study by Hou et al.[9] has stated that rotary instrumentation resulted in less incidence of postendodontic pain. Thus, in our study, root canal instrumentation was performed with rotary instruments. Intracanal medication was not kept in the root canal after the instrumentation to rule out its confounding effect[29,30] and also extrusion of an interappointment medicament can influence postoperative pain.[9]
Assessment of pain was done at the 6th, 12th, 24th, and 48th h following the root canal instrumentation and 6th and 12th h following the obturation[15,16] since the postoperative pain substantially reduced after 48 h of the procedure.[2,3] In our study, postoperative endodontic pain was evaluated using the VAS since it is a highly reliable, valid tool and most of the previous literature used the same.[15,20,25,26,27,28]
In the present study, the occlusal surface reduction does not influence the postendodontic pain which was in correspondence with Creech et al.,[18] Jostes and Holland,[19] Parirokh et al.,[20] and Arslan et al.;[21] while confounding with Rosenberg et al.,[14] Emara et al.,[15] and Ahmed et al.,[16] following the root canal obturation, again reducing the occlusal surface does not influence the postendodontic pain, which was in accordance with Ahmed et al.[16] Thus, the null hypothesis (occlusal reduction does not reduce the postendodontic pain) was accepted in our study.
When undermined enamel is present on one or more than one wall of the cavity and when the clinician has ensured that the patient will receive the full coverage occlusal restoration following the endodontic treatment, performing occlusal reduction is acceptable.[20] However, if the patient fails to receive a full coverage restoration after occlusal reduction to prevent post operative pain, it will remain nonfunctional and may lead to occlusal disharmony. Hence, both the clinician and the patient should understand the limitations associated with occlusal reduction.
Postoperative pain following endodontic procedure may require analgesic medication. Sutherland and Matthews[31] in their systematic review strongly recommended the intake of nonopioid analgesics for management of pain in acute apical periodontitis. However, in our study, there was no influence of analgesic in both the treatment groups. This was in accordance with Parirokh et al.,[20] Emara et al.,[15] and Ahmed et al.[16] studies.
Finally, the smaller sample size and dropouts were limitations of this study. Further clinical trials with more number of samples have to be evaluated to assess the influence of occlusal surface reduction on postendodontic pain.
CONCLUSION
The findings from this randomized double-blinded clinical trial concluded that occlusal surface reduction did not influence the postendodontic pain following instrumentation and obturation in teeth with acute irreversible pulpitis and acute apical periodontitis.
Author contributions
Kuzhanchinathan Manigandan: Concept, design, literature search, data acquisition, data analysis, manuscript preparation, manuscript edition
Soundararajan Karthick: Concept, design, data acquisition, data analysis
Rajendran Mathan Rajan: Concept, project supervision, manuscript review
Kalaiselvam RajeswariGopal: Concept, project supervision, manuscript review.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Nguyen-Nhon D, Nagendrababu V, Pulikkotil SJ, Rossi-Fedele G. Effect of occlusal reduction on postendodontic pain: A systematic review and meta-analysis of randomised clinical trials. Aust Endod J. 2020;46:282–94. doi: 10.1111/aej.12380. [DOI] [PubMed] [Google Scholar]
- 2.Ng YL, Glennon JP, Setchell DJ, Gulabivala K. Prevalence of and factors affecting post-obturation pain in patients undergoing root canal treatment. Int Endod J. 2004;37:381–91. doi: 10.1111/j.1365-2591.2004.00820.x. [DOI] [PubMed] [Google Scholar]
- 3.Mittal N, Baranwal HC, Gupta S, Shankari T, Gupta S, Kharat S. Comparative analysis of reduction in pain scores after single visit root canal treatment using endodontic irrigation protocols, namely, conventional needle irrigation, PUI, PIPS and SWEEPS: A randomized control trial. J Conserv Dent. 2023;26:143–9. doi: 10.4103/jcd.jcd_450_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shamszadeh S, Shirvani A, Asgary S. Does occlusal reduction reduce post-endodontic pain? A systematic review and meta-analysis. J Oral Rehabil. 2020;47:528–35. doi: 10.1111/joor.12929. [DOI] [PubMed] [Google Scholar]
- 5.El Mubarak AH, Abu-bakr NH, Ibrahim YE. Postoperative pain in multiple-visit and single-visit root canal treatment. J Endod. 2010;36:36–9. doi: 10.1016/j.joen.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 6.Marshall JG, Liesinger AW. Factors associated with endodontic posttreatment pain. J Endod. 1993;19:573–5. doi: 10.1016/S0099-2399(06)81290-2. [DOI] [PubMed] [Google Scholar]
- 7.Nagendrababu V, Pulikkotil SJ, Jinatongthai P, Veettil SK, Teerawattanapong N, Gutmann JL. Efficacy and safety of oral premedication on pain after nonsurgical root canal treatment: A systematic review and network meta-analysis of randomized controlled trials. J Endod. 2019;45:364–71. doi: 10.1016/j.joen.2018.10.016. [DOI] [PubMed] [Google Scholar]
- 8.Parirokh M, Yosefi MH, Nakhaee N, Manochehrifar H, Abbott PV, Reza Forghani F. Effect of bupivacaine on postoperative pain for inferior alveolar nerve block anesthesia after single-visit root canal treatment in teeth with irreversible pulpitis. J Endod. 2012;38:1035–9. doi: 10.1016/j.joen.2012.04.012. [DOI] [PubMed] [Google Scholar]
- 9.Hou XM, Su Z, Hou BX. Post endodontic pain following single-visit root canal preparation with rotary versus reciprocating instruments: A meta-analysis of randomized clinical trials. BMC Oral Health. 2017;17:86.. doi: 10.1186/s12903-017-0355-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gama TG, de Oliveira JC, Abad EC, Rôças IN, Siqueira JF., Jr Postoperative pain following the use of two different intracanal medications. Clin Oral Investig. 2008;12:325–30. doi: 10.1007/s00784-008-0199-3. [DOI] [PubMed] [Google Scholar]
- 11.Kandemir Demirci G, Çalışkan MK. A prospective randomized comparative study of cold lateral condensation versus core/gutta-percha in teeth with periapical lesions. J Endod. 2016;42:206–10. doi: 10.1016/j.joen.2015.10.022. [DOI] [PubMed] [Google Scholar]
- 12.Lopes LP, Herkrath FJ, Vianna EC, Gualberto Júnior EC, Marques AA, Sponchiado Júnior EC. Effect of photobiomodulation therapy on postoperative pain after endodontic treatment: A randomized, controlled, clinical study. Clin Oral Investig. 2019;23:285–92. doi: 10.1007/s00784-018-2435-9. [DOI] [PubMed] [Google Scholar]
- 13.Gundogdu EC, Arslan H. Effects of various cryotherapy applications on postoperative pain in molar teeth with symptomatic apical periodontitis: A preliminary randomized prospective clinical trial. J Endod. 2018;44:349–54. doi: 10.1016/j.joen.2017.11.002. [DOI] [PubMed] [Google Scholar]
- 14.Rosenberg PA, Babick PJ, Schertzer L, Leung A. The effect of occlusal reduction on pain after endodontic instrumentation. J Endod. 1998;24:492–6. doi: 10.1016/S0099-2399(98)80054-X. [DOI] [PubMed] [Google Scholar]
- 15.Emara RS, Abou El Nasr HM, El Boghdadi RM. Evaluation of postoperative pain intensity following occlusal reduction in teeth associated with symptomatic irreversible pulpitis and symptomatic apical periodontitis: A randomized clinical study. Int Endod J. 2019;52:288–96. doi: 10.1111/iej.13012. [DOI] [PubMed] [Google Scholar]
- 16.Ahmed YE, Emara RS, Sarhan SM, El Boghdadi RM, El-Bayoumi MA, El-Far HM, et al. Post-treatment endodontic pain following occlusal reduction in mandibular posterior teeth with symptomatic irreversible pulpitis and sensitivity to percussion: A single-centre randomized controlled trial. Int Endod J. 2020;53:1170–80. doi: 10.1111/iej.13328. [DOI] [PubMed] [Google Scholar]
- 17.Rosenberg PA. Clinical strategies for managing endodontic pain. Endod Top. 2002;3:78–92. [Google Scholar]
- 18.Creech JL, 3rd, Walton RE, Kaltenbach R. Effect of occlusal relief on endodontic pain. J Am Dent Assoc. 1984;109:64–7. doi: 10.14219/jada.archive.1984.0294. [DOI] [PubMed] [Google Scholar]
- 19.Jostes JL, Holland GR. The effect of occlusal reduction after canal preparation on patient comfort. J Endod. 1984;10:34–7. doi: 10.1016/S0099-2399(84)80251-4. [DOI] [PubMed] [Google Scholar]
- 20.Parirokh M, Rekabi AR, Ashouri R, Nakhaee N, Abbott PV, Gorjestani H. Effect of occlusal reduction on postoperative pain in teeth with irreversible pulpitis and mild tenderness to percussion. J Endod. 2013;39:1–5. doi: 10.1016/j.joen.2012.08.008. [DOI] [PubMed] [Google Scholar]
- 21.Arslan H, Seckin F, Kurklu D, Karatas E, Yanikoglu N, Capar ID. The effect of various occlusal reduction levels on postoperative pain in teeth with symptomatic apical periodontitis using computerized analysis: A prospective, randomized, double-blind study. Clin Oral Investig. 2017;21:857–63. doi: 10.1007/s00784-016-1835-y. [DOI] [PubMed] [Google Scholar]
- 22.Nagendrababu V, Duncan HF, Bjørndal L, Kvist T, Priya E, Jayaraman J, et al. PRIRATE 2020 guidelines for reporting randomized trials in endodontics: A consensus-based development. Int Endod J. 2020;53:764–73. doi: 10.1111/iej.13294. [DOI] [PubMed] [Google Scholar]
- 23.Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–91. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- 24.Jafarzadeh H, Abbott PV. Review of pulp sensibility tests. Part II: Electric pulp tests and test cavities. Int Endod J. 2010;43:945–58. doi: 10.1111/j.1365-2591.2010.01760.x. [DOI] [PubMed] [Google Scholar]
- 25.Asghar S, Fatima F, Ali A. Occlusal reduction reduces postoperative pain after endodontic instrumentation. Pak Oral Dent J. 2014;34:539–42. [Google Scholar]
- 26.Sheikh H, Ahmed MA, Jouhar R, Choudhry Z. Comparison of post instrumentation pain in teeth during root canal treatment with or without occlusal reduction. Pak Oral Dent J. 2015;35:699–701. [Google Scholar]
- 27.Raza I, Ahmed A, Khalid N, Batool F. Effect of occlusal reduction on frequency of post operative pain relief, following an endodontic instrumentation. Pak Oral Dent J. 2016;36:650–3. [Google Scholar]
- 28.Zaman H, Ahmed SS. Effect of occlusal reduction on post instrumentation pain in patients with acute irreversible pulpitis. Pak Oral Dent J. 2016;36:119–21. [Google Scholar]
- 29.Ghoddusi J, Javidi M, Zarrabi MH, Bagheri H. Flare-ups incidence and severity after using calcium hydroxide as intracanal dressing. N Y State Dent J. 2006;72:24–8. [PubMed] [Google Scholar]
- 30.Hegde VR, Jain A, Patekar SB. Comparative evaluation of calcium hydroxide and other intracanal medicaments on postoperative pain in patients undergoing endodontic treatment: A systematic review and meta-analysis. J Conserv Dent. 2023;26:134–42. doi: 10.4103/jcd.jcd_501_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sutherland S, Matthews DC. Emergency management of acute apical periodontitis in the permanent dentition: A systematic review of the literature. J Can Dent Assoc. 2003;69:160.. [PubMed] [Google Scholar]


