Abstract
Aim and Objectives:
The aim of the study was to compare and evaluate the push-out bond strength (POBS) of epoxy resin-based and calcium silicate-based sealers with and without incorporating chitosan nanoparticles (CSNPs).
Methodology:
Eighty human mandibular premolars with a single canal were taken. A standard root length of 15 mm was established. Canals were instrumented with Neoendo files up to size 30, 4% and were irrigated with 5 ml of 2.5% NaOCl, and 5 ml of ethylenediaminetetraacetic acid 17%. Then, samples were obturated using the size 30, 4% gutta-percha, single-cone technique using respective sealers. For POBS, it was grouped as Group 1 Adseal, Group 2 CeraSeal, Group 3 Adseal + 2% wt/vol CSNP, and Group 4 CeraSeal + 2% wt/vol CSNP. Samples embedded in acrylic resin were sectioned transversely at 11 and 7 mm from the apex. Dislodgment resistance was calculated using a universal testing machine. The data were analyzed using a one-way ANOVA test, followed by Tukey’s post hoc analysis. The level of significance (P value) was set at P < 0.05.
Results:
At 7 mm from the apex, Group 4 (CeraSeal + 2% wt/vol CSNP) demonstrated significantly higher mean POBS. However, no significant difference was observed between Groups 1 (Adseal), Group 2 (CeraSeal), and Group 3 (Adseal + 2% wt/vol CSNP). At 11 mm from the apex, Group 2 (CeraSeal) and Group 4 (CeraSeal + 2% wt/vol CSNP) demonstrated significantly higher mean POBS. On comparison between POBS at 7 mm and 11 mm from the apex, the mean POBS at the 11 mm region from the apex was significantly higher in all study groups, which was statistically significant.
Conclusion:
Within the limitations of the study, it has been concluded that Group 4 (CeraSeal + 2% wt/vol CSNP) has better bond strength compared to the other groups.
Keywords: Adseal, CeraSeal, chitosan nanoparticle, pushout bond strength
INTRODUCTION
A good endodontic treatment outcome requires complete three-dimensional root canal cleaning, shaping, and obturation using an impermeable, biocompatible, and dimensionally stable filling material.[1] To attain this fluid-tight seal, many endodontic obturation materials and sealers are being used.
Gutta-percha (GP) is considered a gold standard material for obturation.[2] However, it lacks adhesive quality.[3] Hence, sealers are used as a thin, tacky paste to fill these voids, lateral canals, and accessory canals where core obturation materials cannot infiltrate.[4] They are commercially available with different main compositions. When it comes to the physicochemical properties of sealers that are on the market, resin-based sealers are commonly utilized because they have characteristics such as low solubility and adequate dimensional stability. However, they have drawbacks such as the possibility of mutagenicity, cytotoxicity, hydrophobicity, and eliciting an inflammatory response.[5] Unfortunately, they also lack biomimetic properties that are essential for the long-term sealing of root canal systems. In this regard, bioactive calcium silicate-based sealers have been introduced to overcome these demerits and give satisfactory clinical results.[6] Recently, premixed bioceramics are available; one such is CeraSeal, a tricalcium silicate-based sealer. As they are premixed,[7] they help in avoiding operator errors, have homogeneous consistency, avoid wastage of material, have no cross-contamination, have easy delivery to nonaccessible areas, and have superior handling characteristics. In addition, they become hard and expand slightly on the setting, which provides a superior long-term seal.[8]
Despite the myriad of commercially available options, presently, there is no ideal sealer. To enhance their properties, modifications have been made to root canal sealers.
The primary focus of these endeavors led to the integration of bioactive and soluble additives[9] such as chitosan to yield enduring outcomes. Chitosan nanoparticles (CSNPs) have the ability to strengthen and stabilize dentin collagen by increasing the number of cross-links between collagen fibers and neutralizing the matrix metalloproteinases, which improves the bond strength. However, an increase in CSNP content may cause obliteration of the fibrillar spaces, negatively affecting the bonding, which makes the concentration of chitosan an important factor. Studies have proved that 2% CSNP oligosaccharide resulted in the lowest average loss of calcium ions[10] and better bonding. In addition, in a study conducted by Diatri Nari Raith it was found that sealers modified with CSNP are in accordance with ISO 6876 criteria, exhibiting acceptable qualities in terms of setting time, flowability, and solubility.[11]
To the best of our knowledge, no other study has been conducted to evaluate the bond strength of sealers modified with CSNPs.
Hence, the present in vitro study aimed to “compare and evaluate the push-out bond strength (POBS) of calcium silicate and epoxy resin-based sealers incorporated with and without CSNPs.”
Sample size estimation
The sample size was estimated using the G*Power software v. 3.1.9.4 (Franz Faul, Universität Kiel, Germany). Considering the effect size to be measured (f) at 40% (based on the results from previous literature), the power of the study at 80% and the alpha error at 5%, the sample size needed was 76, which was rounded off to 80. The total samples required for the present study was 80 which resulted in 20 samples per group.
This ex vivo study was conducted in the Department of Conservative Dentistry and Endodontics, Krishnadevaraya College of Dental Sciences, Yelahanka, India, from 2020 to 2023. The study was approved by the authorities of the Institutional Ethical Committee: KCDS/Ethical comm/026/2020-2021.
A convenience sample of 80 (20 in each group) freshly extracted human permanent mandibular premolars for orthodontic or periodontal reasons were selected.
Inclusion criteria
Human mandibular premolar teeth with a single straight (curvature <5) root canal and a single apical foramen.
Exclusion criteria
Teeth with decay, severe attrition, erosion, with fracture and cracks
Root canal treated teeth and teeth with anatomical variations.
METHODOLOGY
Eighty human mandibular premolar teeth that were recently extracted were used in this study. After extraction, teeth were immediately placed under running water to remove blood, followed by curettage to remove soft tissue and subsequently stored in saline solution at room temperature until used. Decoration was done, and the root canal length was standardized to 15 mm. Working length was established by inserting the #10 K file (Mani Inc., Tochigi Ken, Japan) into each root canal until it was visible at the apical foramen and then subtracting 1 mm from the recorded length.
Canals were instrumented up to size 30, 4% taper (Neoendo files, Orikam, India).
Irrigation was performed using 5 mL 2.5% NaOCl (Parcan, Septodont, India) between each instrument, and the smear layer was finally removed using 5 mL 17% ethylenediaminetetraacetic acid (Prevest Denpro, Jammu, India).
Preparation of chitosan nanoparticle-incorporated sealer
Two grams of CSNP with an 85% degree of deacetylation (SRL Pvt. Ltd., Hyderabad, India) was diluted with 100 mL of 1% acetic acid (SRL Pvt. Ltd., Hyderabad, India), and the mixture was stirred for 2 h using a magnetic stirrer. Then, the freshly prepared 2% CSNP solution was further added to sealers (Adseal and CeraSeal) in a 1:1 ratio and mixed thoroughly to obtain a homogeneous mix and placed into the root canals with a Lentulo spiral filler.
For push-out bond strength
The samples were divided randomly into four groups of 20 teeth each, based on the sealers used for obturation. Samples were obturated using GP 30, 4% taper, and respective sealers according to the group:
Group 1: Adseal (n = 20), Group 2: CeraSeal (n = 20), Group 3: Adseal + 2% wt/vol CSNP (n = 20), and Group 4: CeraSeal + 2% wt/vol CSNP (n = 20).
Samples were stored at 37°C and 100% humidity in an incubator for a week to ensure the complete setting of the sealers. Two transverse sections of thickness 1 mm were obtained, one at 11 mm from the apex (junction of the coronal and middle third) and another at 7 mm from the apex (junction of the middle and apical third). Above procedures were carried out by a single clinician to eliminate operator errors. To calculate the POBS, a universal testing machine (Instron, Canton, MA, USA) was used. A standard-size plunger with a tip of 0.6 mm diameter was used at a speed of 1 mm/min [Figure 1].
Figure 1.
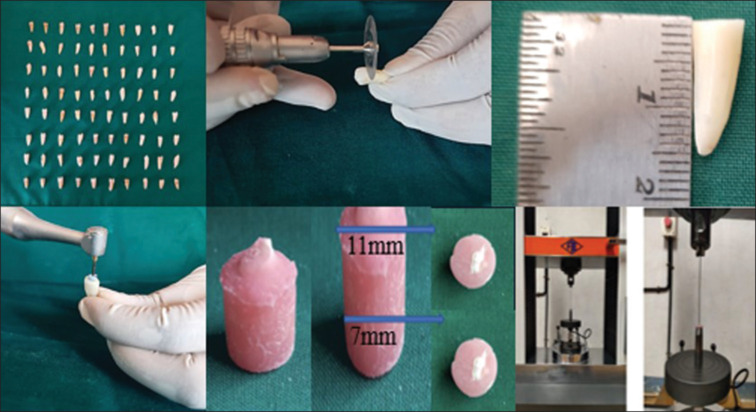
Preparation and analysis of samples for pushout bond strength
Statistical analysis
The Statistical Package for the Social Sciences (SPSS) for Windows Version 22.0 released 2013. Armonk, NY, USA: IBM Corp., was used to perform statistical analyses.
Descriptive statistics
Descriptive analysis includes expression of POBS and sealer penetration in terms of mean and standard deviation for each study group.
Inferential statistics
One-way ANOVA test followed by Tukey’s post hoc analysis was used to compare the mean POBS and sealer penetration between 4 groups.
The level of significance (P value) was set at P < 0.05.
RESULTS
Group 4 demonstrated significantly higher mean POBS at 7 mm from the apex as compared to Group 1 at P < 0.001, Group 2 at P = 0.04, and Group 3 at P = 0.001. However, no significant difference in the mean POBS was observed between Groups 1, 2, and 3 [Table 1].
Table 1:
Comparison of mean push-out bond strength at 7 mm between different groups using one-way ANOVA test
| Comparison of mean push-out bond strength (in MPa) at 7 mm between different groups using one - way ANOVA test | |||||
|---|---|---|---|---|---|
| Groups | n | Mean±SD | Minimum | Maximum | P |
| Group 1 | 20 | 4.778±0.480 | 3.95 | 5.30 | <0.001* |
| Group 2 | 20 | 5.304±0.690 | 4.58 | 6.85 | |
| Group 3 | 20 | 4.931±0.432 | 4.05 | 5.45 | |
| Group 4 | 20 | 6.012±0.730 | 5.03 | 6.99 | |
*Statistically significant. SD: Standard deviation
Group 4 exhibited significantly higher mean POBS at 11 mm from the apex, followed by Group 2, and less so in Group 3 and Group 1 [Table 2].
Table 2:
Comparison of mean push-out bond strength at 11 mm from apex between different groups using one-way ANOVA test
| Comparison of mean push-out bond strength (in MPa) at 11 mm between different groups using one-way ANOVA test | |||||
|---|---|---|---|---|---|
| Groups | n | Mean±SD | Minimum | Maximum | P |
| Group 1 | 20 | 8.642±1.214 | 6.96 | 10.99 | 0.004* |
| Group 2 | 20 | 9.825±0.884 | 7.95 | 10.98 | |
| Group 3 | 20 | 8.865±0.922 | 7.09 | 9.95 | |
| Group 4 | 20 | 10.037±0.699 | 8.50 | 10.95 | |
*Statistically significant. SD: Standard deviation
The test results demonstrated that the mean POBS at the 11 mm region (8.642 ± 1.214, 9.825 ± 0.884, 8.865 ± 0.922, and 10.037 ± 0.699) was significantly higher in all study groups as compared to the 7 mm region (4.778 ± 0.480, 5.304 ± 0.690, 4.931 ± 0.432, and 6.012 ± 0.730), and the mean differences between these two regions in all study groups were statistically significant at P < 0.001 [Table 3].
Table 3:
Comparison of mean Pushout Bond Strength at 7 and 11 mm from the apex in each group using Student Paired t-Test
| Comparison of mean push-out bond strength between 7 and 11 mm region in each group using Student’s paired t-test | |||||
|---|---|---|---|---|---|
| Groups | Region (mm) | n | Mean±SD | Mean difference | P |
| Group 1 | At 7 | 20 | 4.778±0.480 | −3.864 | <0.001* |
| At 11 | 20 | 8.642±1.214 | |||
| Group 2 | At 7 | 20 | 5.304±0.690 | −4.521 | <0.001* |
| At 11 | 20 | 9.825±0.884 | |||
| Group 3 | At 7 | 20 | 4.931±0.432 | −3.934 | <0.001* |
| At 11 | 20 | 8.865±0.922 | |||
| Group 4 | At 7 | 20 | 6.012±0.730 | −4.025 | <0.001* |
| At 11 | 20 | 10.037±0.699 | |||
*Statistically significant. SD: Standard deviation
DISCUSSION
Ensuring that root canal filling material adheres to the dentinal walls is a highly desirable physical feature for the long-term clinical efficacy of endodontic therapy, as it prevents fluid from percolating between the regions of obturation.
Endodontic sealers aid in adhesion to root canal dentin, preserving the integrity of the sealer-dentin interface, and prevent dislodgement. The push-out test is reproducible and can be interpreted easily among the various bond strength tests available. It is effective as it allows the evaluation of root canal sealers even with low bond strength and in thin sections.[12] The push-out test method generates fractures parallel to the dentin-sealer interface;[13] hence, it is a more clinically reliable bond strength test for a sealer. Therefore, in the present study, we used a push-out test, which Haller first designed to compare the bond strength of sealers to root dentin.
In the current study on the comparison between the unmodified groups, it was revealed that Group 2 (CeraSeal) has a higher bond strength than Group 1 (Adseal). However, these differences in bond strength were not statistically significant. The higher bond strength exhibited by Group 2 might be due to its tag-like micromechanical interaction[14] between the root canal wall and calcium silicate-based sealer and chemical interaction by mineral infiltration, as reported in previous studies.[14] Therefore, greater bond strength might have been the outcome of these sealer’s interfacial interactions with surrounding tissue.[15]
On comparing the modified and unmodified groups, a higher mean POBS was seen in groups modified with CSNPs. This might have been due to the greater surface area and the presence of reactive functional amino groups on the surface of CSNPs, which provide avenues for hydrogen bonding.[16]
Multiple comparisons between groups revealed that Group 4 (CeraSeal + CSNP) demonstrated significantly higher mean POBS (6 Mpa). However, no significant difference in the mean POBS was observed between Groups 1, 2, and 3. This improved strength might be due to the synergistic effect of CeraSeal properties such as sufficient sealing qualities, high bond strength, flow, and dimensional stability,[17] along with chitosan’s inherent toughness due to its interfibrillar hydrogen bonding and its hydrophilic nature that facilitates collagen adsorption. The covalent immobilization of chitosan on dentinal collagen induces remineralization of the exposed and demineralized dentin structure due to its functional phosphate groups that might bind to calcium ions, forming a favorable surface for crystal nucleation, resulting in the formation of a calcium phosphate layer,[18] a strong bond.
Furthermore, in the current investigation, push-out strength was assessed at two distinct points in relation to the apex: one at 11 mm from the apex and another at 7 mm from the apex. The results revealed that the POBS in the 11-mm region from the apex was significantly higher in all groups as compared to 7 mm from the apex, and it was statistically significant. This might have been due to the presence of dentinal tubules with larger diameters at the coronal portion when tested against the apical part. In addition, it is a well-known fact that as one moves from the crown to the root apex, there are fewer dentinal tubules,[19] and adhesion improves when there is more sealer penetration into these tubules. Therefore, a stronger connection would be anticipated in the coronal portion, where more tubules per millimeter are seen.
Wang et al. stated that despite the kind of sealers or obturation techniques used, the sealer penetration percentages into the dentinal tubules of the root canal increase from the apical to the coronal part due to the amount of eliminated smear layer in the coronal portion of the root canal.[20] Moreover, dentin in the coronal, intermediate, and apical portions has variable surface energies, in conjunction with challenges experienced during the complete removal of the smear layer from the apical region.[20] These might have led to lower bond strength in sections obtained at 7 mm from the apex. These results were in accordance with studies conducted by Huang et al.[21] and Eid et al.[22]
To the best of our knowledge, there are very few studies that provide information concerning the dislodgement resistance of sealers modified with chitosan. Regarding the different POBS values of these chitosan-modified sealers, further evaluation of these sealers under experimental and clinical conditions is required.
CONCLUSION
In the confines of this investigation, the following conclusions can be drawn:
Adding CSNPs to sealers (Group 4 and Group 3) increased POBS, which can be inferred from the comparison of their results with the unmodified group (Group 1 and Group 2).
The sealer POBS at the 11 mm region from the apex was significantly higher in all groups as compared to 7 mm from the apex.
Group 4 displayed better bond strength than other groups.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Kamin R, Vikram R, Meena N, Kumari RA, Adarsha MS, Murthy CS. Effect of final irrigating solutions on penetration depth of resin-based sealers into dentinal tubules. J Conserv Dent. 2021;24:374–8. doi: 10.4103/jcd.jcd_209_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vishwanath V, Rao HM. Gutta-percha in endodontics – A comprehensive review of material science. J Conserv Dent. 2019;22:216–22. doi: 10.4103/JCD.JCD_420_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pedrinha VF, Alencar CM, Jassé FA, Zaniboni JF, Dantas AA, de Andrade FB, et al. Effect of the several epoxy resin-based sealer compositions on adhesion interface in radicular dentin after calcium hydroxide intracanal medication removal. J Clin Exp Dent. 2021;13:e913–9.. doi: 10.4317/jced.58375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Komabayashi T, Colmenar D, Cvach N, Bhat A, Primus C, Imai Y. Comprehensive review of current endodontic sealers. Dent Mater J. 2020;39:703–20. doi: 10.4012/dmj.2019-288. [DOI] [PubMed] [Google Scholar]
- 5.Song M, Park MG, Kwak SW, Kim RH, Ha JH, Kim HC. Pilot evaluation of sealer-based root canal obturation using epoxy-resin-based and calcium-silicate-based sealers: A randomized clinical trial. Materials (Basel) 2022;15:5146.. doi: 10.3390/ma15155146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chopra V, Davis G, Baysan A. Physico-chemical properties of calcium-silicate versus resin based sealers – A systematic review and meta-analysis of laboratory-based studies. Materials (Basel) 2021;15:229.. doi: 10.3390/ma15010229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kumar A, Kour S, Kaul S, Malik A, Dhani R, Kaul R. Cytotoxicity evaluation of Bio-C, CeraSeal, MTA – Fillapex, and AH plus root canal sealers by microscopic and 3-(4, 5 dimethythiazol-2yl)-2, 5-diphenyltetrazolium bromide (MTT) assay. J Conserv Dent. 2023;26:73–8. doi: 10.4103/jcd.jcd_320_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Motwani N, Ikhar A, Nikhade P, Chandak M, Rathi S, Dugar M, et al. Premixed bioceramics: A novel pulp capping agent. J Conserv Dent. 2021;24:124–9. doi: 10.4103/JCD.JCD_202_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baras BH, Melo AS, Thumbigere-Math V, Tay FR, Fouad AF, Oates TW, et al. Novel bioactive and therapeutic root canal sealers with antibacterial and remineralization properties. Materials (Basel) 2020;13:1096.. doi: 10.3390/ma13051096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Abidin T, Geovani G. The Effect of 2% Chitosan Oligosaccharides and 15% EDTA on Calcium Loss in the Root Canal. Journal of Syiah Kuala Dentistry Society. 2023;8:9–15. [Google Scholar]
- 11.Ratih DN, Enggardipta RA, Kusumo AN, Hadriyanto W. Setting time, flowability, and solubility of epoxy resin-based sealer mixed with chitosan nanoparticles. Int J Appl. 2021;13:122–6. [Google Scholar]
- 12.Abada HM, Farag AM, Alhadainy HA, Darrag AM. Push-out bond strength of different root canal obturation systems to root canal dentin. Tanta Dent J. 2015;12:185–91. [Google Scholar]
- 13.Dayanand Chole D, Vaidya DM, Shashank Kundoor D, Srinivas Bakle RD, Gandhi DN, Hatte DN. Comparative evaluation of push-out bond strength of different endodontic sealers: An in vitro study. IOSR-JDMS. 2019;18:59–62. [Google Scholar]
- 14.Sfeir G, Zogheib C, Patel S, Giraud T, Nagendrababu V, Bukiet F. Calcium silicate-based root canal sealers: A narrative review and clinical perspectives. Materials (Basel) 2021;14:3965.. doi: 10.3390/ma14143965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Donnermeyer D, Bürklein S, Dammaschke T, Schäfer E. Endodontic sealers based on calcium silicates: A systematic review. Odontology. 2019;107:421–36. doi: 10.1007/s10266-018-0400-3. [DOI] [PubMed] [Google Scholar]
- 16.Harugade A, Sherje AP, Pethe A. Chitosan: A review on properties, biological activities and recent progress in biomedical applications. React Funct Polym. 2023:105634. [Google Scholar]
- 17.Abdelrahman MH, Hassan MY. Comparison of root canal walls cleanliness obturated with two commercially available; calcium silicate sealers and a resin sealer after retreatment. International Journal of Dentistry Research. 2020;5:20–3. [Google Scholar]
- 18.Del Carpio-Perochena A, Bramante CM, Duarte MA, de Moura MR, Aouada FA, Kishen A. Chelating and antibacterial properties of chitosan nanoparticles on dentin. Restor Dent Endod. 2015;40:195–201. doi: 10.5395/rde.2015.40.3.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gülmez HK, Kaya S, Özata MY. Comparison of dentinal tubule penetration of three different root canal sealers by confocal laser scanning microscopy. Endodontology. 2023;35:107–12. [Google Scholar]
- 20.Wang Y, Liu S, Dong Y. In vitro study of dentinal tubule penetration and filling quality of bioceramic sealer. PLoS One. 2018;13:e0192248.. doi: 10.1371/journal.pone.0192248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Huang Y, Orhan K, Celikten B, Orhan AI, Tufenkci P, Sevimay S. Evaluation of the sealing ability of different root canal sealers: A combined SEM and micro-CT study. J Appl Oral Sci. 2018;26:e20160584.. doi: 10.1590/1678-7757-2016-0584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Eid BM, Waly AS, Princy P, Venkatesan R. Scanning electron microscope evaluation of dentinal tubules penetration of three different root canal sealers. EC Dent Sci. 2019;18:1121–7. [Google Scholar]


