Glenolabral articular disruption (GLAD) lesions are uncommon traumatic shoulder injuries which are described as a combination of a superficial tear of the anteroinferior labrum and defect of the adjacent glenoid cartilage.8,11,14 The injury typically occurs during a fall with forced adduction while the arm is abducted and externally rotated and results in anterior shoulder pain.8,11,14 While the deep fibers of the labrum are still intact, the degree of the underlying cartilage defect is variable and range from minor fibrillation to complete cartilage loss.8,11
The treatment of both labral tear and chondral defect depends on the age and activity of the patient, the size, grade and localization of the chondral defect and concomitant injuries.8 In previous reported cases, the labral tear was arthroscopically débrided or repaired, while the glenoid defect was treated with débridement, chondroplasty or microfracture.1,8,14 These procedures result in pain relief but may not prevent the development of osteoarthritis.1,9,15 Treatment options of chondral defects range from joint preserving techniques such as arthroscopic débridement, microfracture, autologous matrix-induced chondrogenesis, osteochondral autologous transfer, autologous chondrocyte transplantation (ACT) and partial shoulder surfacing to total shoulder arthroplasty.5,7,9 The ACT has shown promising results for the treatment of isolated chondral defects of the humeral head.4 However, it is a 2-stage approach with high costs and limited availability. The minced cartilage as a 1-stage procedure represents a more cost-effective alternative, in which a mixture of autologous cartilage chips and platelet-rich plasma (PRP) is brought into the defect. The technique has recently been published for the treatment of isolated humeral cartilage lesions.9 To the best of our knowledge no clinical date are available for the usage of minced cartilage for glenoid chondral lesions.
We present the case of a GLAD lesion with a grade 4 chondral defect that was treated with an autologous minced cartilage procedure and labral repair and report on the clinical and radiological outcome at 1-year follow-up.
Case report
A 32-year-old male patient presented to our clinic, 3 weeks after a climbing accident where he fell, involving a distortion and adduction of the shoulder. Since then, he experienced movement-related pain. There was no dislocation of the shoulder reported.
Active range of motion (ROM) was limited to 90° forward flexion and abduction, 40° external rotation and internal rotation to the sacroiliac joint due to pain. Passive ROM was free. Rotator cuff testing (external rotation, Belly-Press-, Jobe-Test) revealed full muscle strength for external rotation, internal rotation, and abduction.
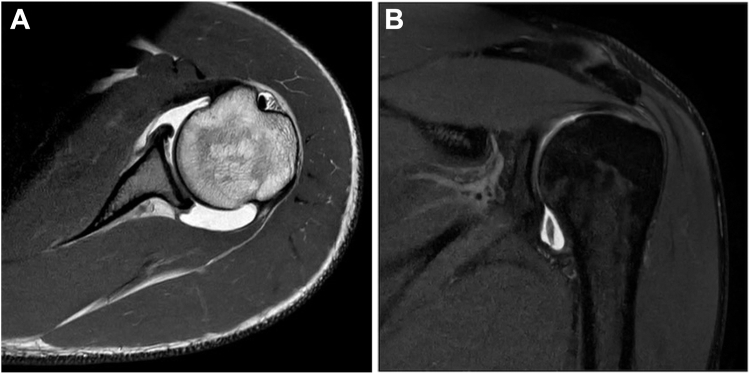
Magnetic resonance arthrography showed an anteroinferior GLAD lesion with a loose body in the axillary recess (Fig. 1) and a partial articular-sided tear of the supraspinatus tendon (Fig. 2, A).
Figure 1.
(A) Axial plane, MR arthrography depicting a glenolabral articular disruption (GLAD) lesion. (B) Coronal plane, MR arthrography depicting a loose body. MR, magnetic resonance.
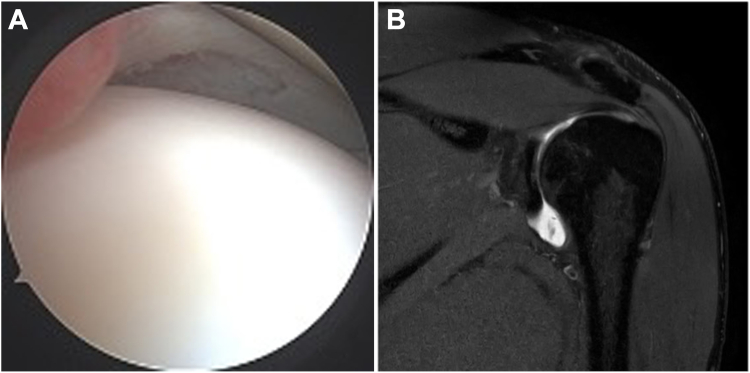
Figure 2.
(A) Preoperative coronal plane, MR arthrography depicting a partial articular-sided tear of the supraspinatus tendon. (B) Arthroscopic visualization of the small undersurface partial tear. MR, magnetic resonance.
Due to the GLAD lesion with labral tear, Outerbridge grade 4 chondral defect and loose bodies, an arthroscopic labral repair, minced cartilage procedure and loose body removal was indicated, as well as a débridement of the supraspinatus tendon.
The patient was informed that data concerning the case would be submitted for publication and he provided consent.
Surgical technique
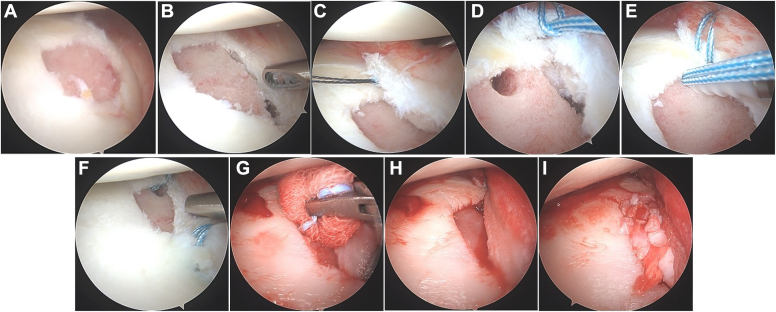
Under general anesthesia, the patient was placed in the lateral decubitus position. A diagnostic arthroscopy was performed with a 30° scope via a posterior viewing portal. The GLAD lesion was localized anteroinferior with an Outerbridge grade 4 chondral defect and loose bodies (Fig. 3, A). Apart from the partly ruptured supraspinatus tendon, other pathologies could be excluded arthroscopically.
Figure 3.
(A) Arthroscopic visualization of the GLAD lesion with the grade 4 chondral defect. (B) Débridement of the chondral defect. (C) Perforation of the capsulolabral complex with a suture lasso. (D) Cinch stitch around the capsulolabral complex. (E) Knotless refixation of the labrum. (F) Arthroscopic visualization of the decreased size of the exposed chondral defect by fixing the labrum with 2 anchors. (G) Drying the chondral defect for the minced cartilage. (H) Arthroscopic visualization of the dried chondral defect. (I) Arthroscopic visualization of the chondral lesion covered with cartilage fragments mixed with PRP and thrombin. GLAD, glenolabral articular disruption; PRP, platelet-rich plasma.
At first the supraspinatus tendon was débrided via an anteroinferior working portal with no further need for a reconstruction (Fig. 2, B). Then the scope was switched to the suprabicipital portal and two transparent twist-in cannulas were inserted in the anteroinferior and posterior working portals.
Afterward the free loose bodies consisting of displaced chondral layer were prepared and cut into small chondral fragments (1x1x1mm) for the minced cartilage procedure with AutoCart (Arthrex, Naples, FL, USA).
The labrum was mobilized, and the débrided chondral defect (Fig. 3, B) measured: 2,5 cm superoinferior × 1,5 cm anteroposterior. The labrum was fixed using two 2,9 mm PushLock anchors (Arthrex, Naples, FL, USA) (Fig. 3, E) and knotless cinch stitches (Fig. 3, D). This way the size of the exposed chondral defect decreased to 1,5 × 1 cm (Fig. 3, F). To cover the grade 4 chondral defect, the AutoCart procedure was used as described in the following.
Blood from the patient was processed into PRP with the ACP double syringe (Arthrex, Naples, FL, USA). The cartilage fragments were mixed with the PRP into a pasty mass, according to the manufacturer. After draining the arthroscopic fluid from the shoulder and drying the chondral lesion (Fig. 3, G), the fragment mixture was applied into the lesion. The fragment paste was covered with a thrombin serum which was prepared out of PRP and sealed with a mixture of PRP and thrombin (Fig. 3, I).
For the first 2 after surgery the shoulder was immobilized in a shoulder sling with only elbow and wrist mobilization allowed, followed by the standard rehabilitation protocol for labral repair.
The patient was discharged 2 days postsurgery with his shoulder immobilized in a shoulder sling for 4 weeks.
Rehabilitation involved passive ROM of the shoulder during physical therapy for the first 6 weeks to 90° flexion and abduction while external rotation was limited to 0°. After 6 weeks active exercises were started to train the deltoid muscle and the rotator cuff as well as the mobilization of the external rotation. After 12 weeks sport specific training was allowed.
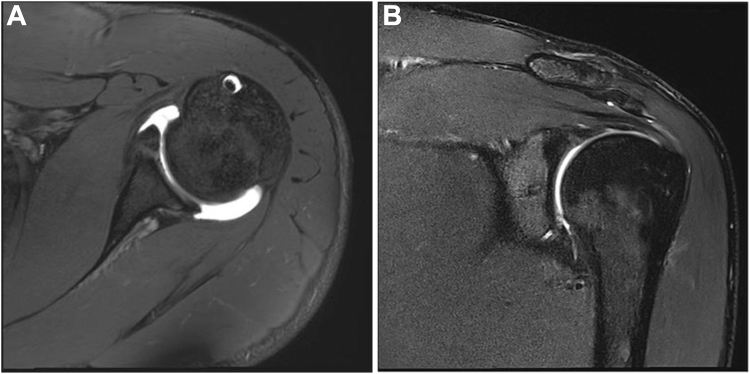
The patient was finally evaluated at one year including magnetic resonance arthrography (Fig. 5).
Figure 5.
(A and B) MR arthrography at one year follow-up depicting a healed labrum and an adequate defect coverage. MR, magnetic resonance.
Outcome and follow-up
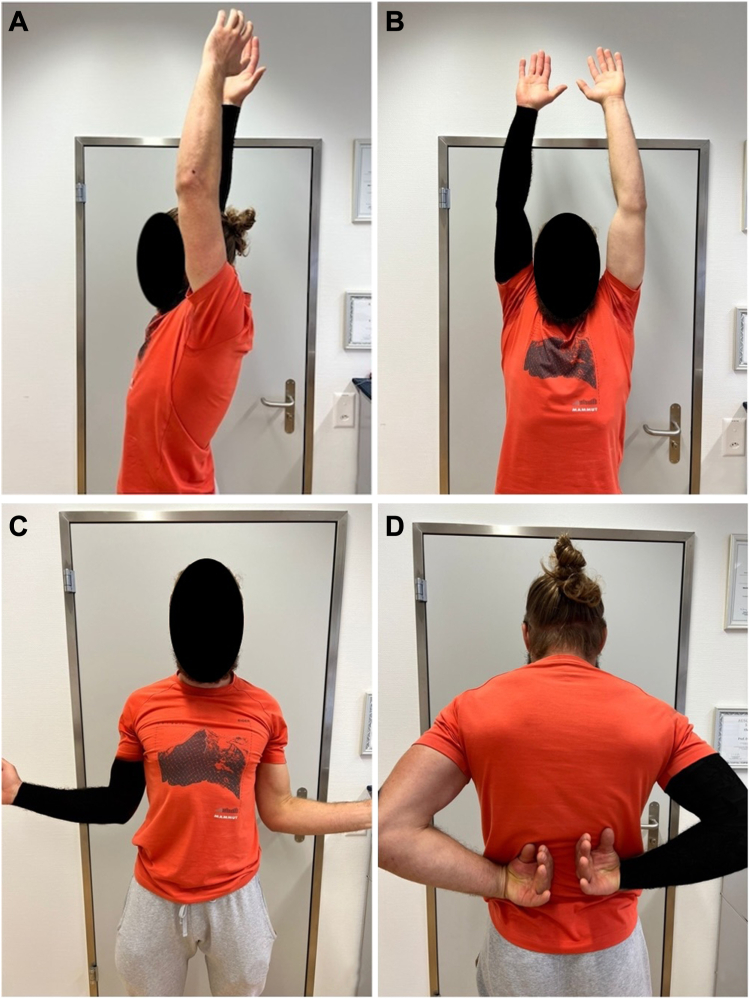
At 1-year follow-up the patient was pain free with unrestricted shoulder function and returned to his climbing sport. The active and passive ROM improved to 170° forward flexion (Fig. 4, A) and abduction (Fig. 4, B), 60° external rotation (Fig. 4, C) and internal rotation to the T10 level (Fig. 4, D). The subjective shoulder value was 95%, the Constant Score 95 points on both sides and the abduction strength 10 kg on both sides. The magnetic resonance arthrography showed a good defect coverage of the cartilage lesion (Fig. 5).
Figure 4.
At 1-year follow-up the patient shows full range of motion, including (A) 170° forward flexion, (B) 170° abduction, (C) 60° external rotation and (D) Internal rotation to the T10 level.
Discussion
Only sporadic case reports on the surgical techniques and clinical outcomes of GLAD lesions have been described.
Neviaser originally described GLAD lesions in 1993 as a cause of anterior shoulder pain but no sign of instability.11,14 Since the radiologic case study of Amrami et al in 2002, the GLAD lesion was associated with shoulder instability and shoulder dislocation or subluxation was considered as a main mechanism.2,14
Management of GLAD lesions depends on the size, grade, and localization the chondral defect. Whereas the repair of the labral tear is mandatory for shoulder stability, no consensus exists regarding the treatment of the articular cartilage defect.1,14
Neviaser recommended an arthroscopic débridement of the labral tear and glenoid cartilage defect as the treatment of choice.11 While this technique results in pain relief, it may not prevent the progression of osteoarthritis and should therefore be reserved for smaller lesions and low-demand patients.3 When a small defect is encountered, the unstable articular flap can the débrided, the subchondral bone microfractured and the labrum advanced into the defect5 as described by Pogorelski et al.13 This way the defect is reduced, and the underlying bone partly protected. However the remaining of the underlying bone is exposed and may predispose the patients to osteoarthritis.1
Surgical techniques with restoration of the articular surface have been reported. Galano et al used a chondral fixation device (SmartNail PLA 1,5 × 25 mm; ConMed Linvatec, Largo, FL, USA) to reattach the cartilage flap to the glenoid and repaired the labrum.6
Paige and Bhatia used suture anchors to reconstruct the labrum to overlap and stabilize the chondral flap, then used a meniscal repair device to further stabilize the flap.
A novel technique was described by Agarwalla et al to concurrently repair both chondral and labral lesion, utilizing a single suture anchor construct to reduce the cartilage flap to the glenoid.1 In our patient, the chondral part was detached from the glenoid as a loose body and could not be reattached.
Further, more operative treatment options for chondral defects have been described. While total shoulder arthroplasty may be a sufficient option for the low-demand elderly, a joint-preserving method is aimed for the younger, more active patients because of the limited life span and higher demand.5,7 Débridement and microfracture result in pain relief but may not prevent the progression of osteoarthritis.3
The current gold standard in treating large chondral defects is the ACT. However, it is a 2-stage procedure with high cost and limited availability due to the restriction of specialized laboratories. The minced cartilage procedure might be a cost effective, 1-stage procedure alternative. First clinical trials have shown promising results, especially in knee surgery.10
To our knowledge, no case report regarding the treatment of GLAD lesions with the ACT or minced cartilage procedure was published. Because our patient was a young, active, high demand case, the minced cartilage procedure as a restorative technique was chosen to potentially repair the lesion effectively and durably.12 In this case, the autologous cartilage from the loose body was sufficient to cover the whole defect. However, additional cartilage can be harvested from the surrounding defect wall or nonweightbearing areas as shown in the knee, such as the intercondylar notch. We used the ACP double syringe (Arthrex, Naples, Florida) for the PRP but other systems such as the Angel system (Arthrex, Naples, Florida) work equally well and additionally allow control over the final platelet and leukocyte concentration.
The partial tear of the supraspinatus tendon shown on the magnetic resonance imaging (Fig. 2, A) was only a small undersurface partial tear without significant footprint exposure (Fig. 2, B). Hence there was no need for a reconstruction and the débridement was sufficient. With this procedure the patient was able to restore his shoulder function and return to his sport without restrictions. The good defect coverage in this case report may prevent the progression of osteoarthritis.
However, it is not possible to know, whether it is hyaline cartilage or fibrocartilage covering the defect, which may result in different mechanical qualities.
Yet, further clinical studies with long-term outcomes are necessary to determine the optimal treatment of these lesions.
Conclusion
The treatment of GLAD lesion with the autologous minced cartilage procedure and labral repair offers a viable option with good clinical and radiological outcomes in this single case report.
Disclaimers:
Funding: No funding was disclosed by the authors.
Conflicts of interest: The authors, their immediate families, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Patient consent: Obtained.
Footnotes
Institutional review board approval was not required for this case report.
References
- 1.Agarwalla A., Puzzitiello R.N., Leong N.L., Forsythe B. Concurrent primary repair of a glenoid labrum articular disruption and a Bankart lesion in an adolescent: a case report of a novel technique. Case Rep Orthop. 2019;2019 doi: 10.1155/2019/4371860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Amrami K.K., Sperling J.W., Bartholmai B.J., Sundaram M. Radiologic case study. Glenolabral articular disruption (GLAD) lesion. Orthopedics. 2002;25(29):95–96. doi: 10.3928/0147-7447-20020101-11. [DOI] [PubMed] [Google Scholar]
- 3.Bhatia S., Hsu A., Lin E.C., Chalmers P., Ellman M., Cole B.J., et al. Surgical treatment options for the young and active middle-aged patient with glenohumeral arthritis. Adv Orthop. 2012;2012 doi: 10.1155/2012/846843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boehm E., Minkus M., Scheibel M. Autologous chondrocyte implantation for treatment of focal articular cartilage defects of the humeral head. J Shoulder Elbow Surg. 2020;29:2–11. doi: 10.1016/j.jse.2019.07.030. [DOI] [PubMed] [Google Scholar]
- 5.Elser F., Braun S., Dewing C.B., Millett P.J. Glenohumeral joint preservation: current options for managing articular cartilage lesions in young, active patients. Arthroscopy. 2010;26:685–696. doi: 10.1016/j.arthro.2009.10.017. [DOI] [PubMed] [Google Scholar]
- 6.Galano G.J., Weisenthal B.M., Altchek D.W. Articular shear of the anterior-inferior quadrant of the glenoid: a glenolabral articular disruption lesion variant. Am J Orthop (Belle Mead NJ) 2013;42:41–43. [PubMed] [Google Scholar]
- 7.Gross C.E., Chalmers P.N., Chahal J., Van Thiel G., Bach B.R., Jr., Cole B.J., et al. Operative treatment of chondral defects in the glenohumeral joint. Arthroscopy. 2012;28:1889–1901. doi: 10.1016/j.arthro.2012.03.026. [DOI] [PubMed] [Google Scholar]
- 8.Hay B., Fraser-Moodie J.A. StatPearls; Treasure Island, FL: 2023. Glenolabral Articular Disruption (GLAD) [PubMed] [Google Scholar]
- 9.Lorenz C.J., Freislederer F., Salzmann G.M., Scheibel M. Minced cartilage procedure for one-stage arthroscopic repair of chondral defects at the glenohumeral joint. Arthrosc Tech. 2021;10:e1677–e1684. doi: 10.1016/j.eats.2021.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Massen F.K., Inauen C.R., Harder L.P., Runer A., Preiss S., Salzmann G.M. One-step autologous minced cartilage procedure for the treatment of knee joint chondral and osteochondral lesions: a series of 27 patients with 2-year follow-up. Orthop J Sports Med. 2019;7 doi: 10.1177/2325967119853773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Neviaser T.J. The GLAD lesion: another cause of anterior shoulder pain. Arthroscopy. 1993;9:22–23. doi: 10.1016/s0749-8063(05)80339-1. [DOI] [PubMed] [Google Scholar]
- 12.Ossendorff R., Walter S.G., Schildberg F.A., Spang J., Obudzinski S., Preiss S., et al. Biologic principles of minced cartilage implantation: a narrative review. Arch Orthop Trauma Surg. 2023;143:3259–3269. doi: 10.1007/s00402-022-04692-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pogorzelski J., Fritz E.M., Horan M.P., Katthagen J.C., Provencher M.T., Millett P.J. Failure following arthroscopic Bankart repair for traumatic anteroinferior instability of the shoulder: is a glenoid labral articular disruption (GLAD) lesion a risk factor for recurrent instability? J Shoulder Elbow Surg. 2018;27:e235–e242. doi: 10.1016/j.jse.2018.02.055. [DOI] [PubMed] [Google Scholar]
- 14.Porcellini G., Cecere A.B., Giorgini A., Micheloni G.M., Tarallo L. The GLAD Lesion: are the definition, diagnosis and treatment up to date? A systematic review. Acta Biomed. 2020;91(14-S) doi: 10.23750/abm.v91i14-s.10987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang K.C., Frank R.M., Cotter E.J., Davey A., Meyer M.A., Hannon C.P., et al. Long-term clinical outcomes after microfracture of the glenohumeral joint: average 10-year follow-up. Am J Sports Med. 2018;46:786–794. doi: 10.1177/0363546517750627. [DOI] [PubMed] [Google Scholar]