Figure 1.
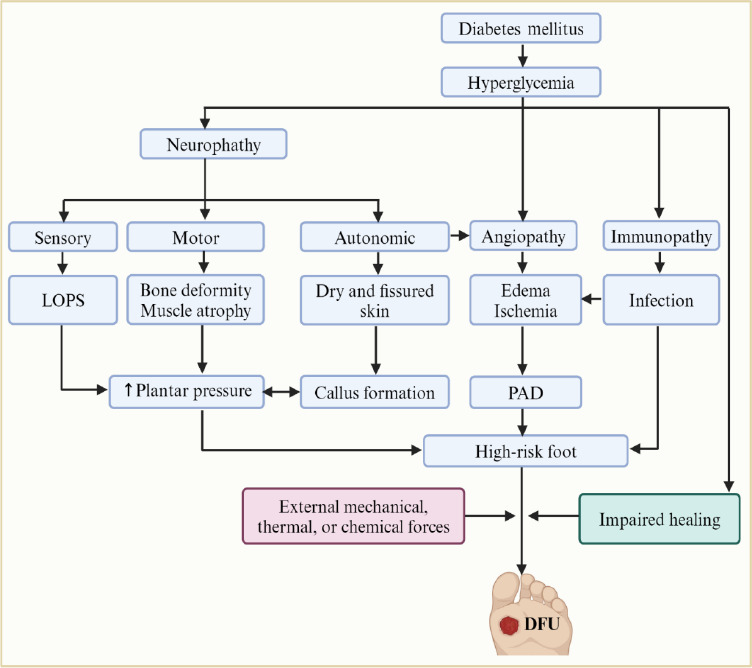
Pathophysiology of diabetic foot ulcer (DFU).
Hyperglycemia, a hallmark of diabetes mellitus (DM), initiates a cascade of pathologic conditions, including neuropathy, angiopathy, and immunopathy, leading to DFU. The hyperglycemia-induced neuropathy encompasses sensory, motor, and autonomic dysfunction. Sensory neuropathy results in loss of protective sensation (LOPS), leading to unnoticed injuries that can progress. Motor dysfunction can contribute to bone deformities and increased plantar pressures, promoting callus formation. Autonomic neuropathy manifests as dry and fissured skin, creating a favorable environment for fungal infections, further increasing vulnerability to ulceration. The hyperglycemia-induced angiopathy manifests as microvascular and macrovascular complications. Microvascular dysfunction disrupts blood flow, leading to ischemia and compromised oxygen and nutrient delivery necessary for healing. Additionally, microvascular complications associated with infections can cause edema. Macrovascular complications, such as peripheral artery disease (PAD), further exacerbate ischemia. On the other hand, hyperglycemia may impair the immune system, potentially increasing susceptibility to infections that further complicate wound healing. Consequently, the interplay between hyperglycemia-induced neuropathy, angiopathy, and immunopathy increases sensitivity to external forces, enhances the onset of lesions, and hinders the normal healing process, leading to the development of non-healing DM wounds, including DFUs. Created with BioRender.com.
