Abstract
Background:
This systematic review compared the efficacy of traditional Chinese medicine (TCM) treatments for outcomes of different stages and labor pain among pregnant women.
Methods:
Eight databases were electronically searched for TCM on labor pain between January 2012 and January 2022. The studies were recorded and screened according to inclusion criteria and subsequently entered in Note Express. The quality of the included studies was evaluated using the Cochrane risk of bias tool, and network meta-analysis was conducted with Stata 16.0. Forest plots and league tables were used to compare different treatment modalities’ effect sizes. Additionally, the probabilities of various treatment modalities for each outcome under the cumulative ranking curve were determined. The protocol was registered in PROSPERO (CRD42022336091). This study adhered to the Preferred Reporting Items for Systematic Reviews and Meta-analyses guidelines.
Results:
Thirty articles encompassing 3277 participants were included in the network meta-analysis with 9 different treatment modalities. In terms of pain of labor at 30 minutes, acupuncture + autonomic nerve block was the most effective treatment modality. With regard to the 60-minute pain and the first stage of labor, acupressure + acupuncture therapy was most effective.
Conclusion:
In general, a combined treatment with acupressure and acupuncture is the most effective approach for relieving labor pain and shortening the duration of labor. Based on these data, we intend to explore further clinical TCM therapy for relieving maternal pain.
Keywords: acupressure, acupuncture, network meta-analysis, pregnant women, traditional Chinese medicine
1. Introduction
Labor pain is an unavoidable fact of childbirth and one of the most important factors that can negatively affect the course of labor and the health of the fetus.[1] Pain is perceived during labor owing to cervical dilation, contractions of the uterus, and uterine extension for vaginal delivery.[2]
The inability to control the intensity of labor pain can cause stress, fear, and anxiety in women, and 10% to 50% of pregnant women have stated that they feel fear and even tend to avoid painful experiences arising from pregnancy.[3,4] It can even create resistance in the uterus, which has a negative effect on the health of the mother and the newborn/fetus.[3–8] A study has suggested that the management of labor pain is a crucial factor in the labor process and in enhancing pregnancy outcome-related maternal satisfaction and maternal–fetal safety.[6]
Labor pain relief methods can be classified into 2 major categories, namely, pharmacological and non-pharmacological.[7] Pharmacological interventions to relieve labor pain chiefly include the parenteral administration of opioids, including inhalation, and regional analgesia. Although several investigations have asserted the efficacy of pharmacological methods, potential adverse effects have also been identified.[3,4] For example, previous reviews have observed that epidural analgesia may cause women to experience hypotension, motor blockade, intrapartum fever, and urinary retention.[3,4,9] Moreover, certain opioids may cause neonatal health problems, such as respiratory depression and abnormal fetal heart rate.[3,4,7] Non-pharmacological interventions include a broad spectrum of physical therapies, such as massage, acupressure, yoga, aromatherapy, hypnosis, essential oils, cupping therapy, and acupuncture points.[8–16] To be precise, non-pharmacological intervention methods have few side effects, additional costs and contraindications can not only perceive pain and discomfort at the lowest level, but also improve the psychological, emotional, and spiritual dimensions of care, which are increasingly widespread worldwide.[17,18]
Traditional Chinese medicine (TCM) therapy, a common method of non-pharmacological treatment has been practiced throughout China for more than 2 millennia and is extensively employed to alleviate pain in pregnant women worldwide.[19] The therapeutic mechanism of TCM emphasizes enhancing the human body’s resistance to diseases and preventing them. This is achieved by improving the inter-connections among self-controlled systems in accordance with the fundamental theory of balance among Yin and Yang, 5 basic elements, as well as a correlation between humans and nature.[19] Acupuncture, massage, and acupressure are some of the forms of therapy frequently used in TCM. Acupressure works as a form of pain relief by moving the energy (qi) via energy pathways (meridians) in the body to establish a balance.[20] Massage, a complementary medicine technique, depends on augmenting the production of endorphins in the body.[9] Acupuncture needles stimulate the circulation to strengthen (tonify) qi and reduce stagnation or obstruction of blood. This technique alleviates pain by inserting needles into specific acupuncture points on the meridians.[20,21]
Although several meta-analyses have explored labor pain score as the outcome, combined application research involving multiple TCM therapies to compare each outcome of maternal delivery and obtain more general and accurate conclusions is lacking. Meta-analysis refers to a comprehensive analysis of existing research results and can avoid the influence of measurement errors caused by a single study.[22–25] Network meta-analysis (NMA) is a generalization of pairwise meta-analysis that permits the comparison of multiple interventions based on all available direct and indirect evidence and aids in the ranking of various interventions. This study aimed to compare the efficacies of the abovementioned non-pharmacological treatment modalities for labor pain as well as the durations of different stages among pregnant women. Our findings are expected to strengthen the evidence and provide recommendations for clinical practice.
2. Materials and methods
2.1. Registration
The methodology for this meta-analysis was based on the Preferred Reporting Items for Meta-analysis (PRISMA) guidelines (CRD42022336091).
2.2. Search strategy
Relevant articles were collected by searching PubMed, Cochrane Library, Web of Science, Embase, China National Knowledge Infrastructure, Wanfang Database, VIP Database, and Chinese Biomedical Database. All the collected randomized controlled trials (RCTs) were published between January 2012 and January 2022. The search words were obtained by combining the MeSH terms with relevant free words, including “Delivery, Obstetric” OR “Pregnancy” OR “Reproduction” AND “Electroacupuncture” OR “Moxibustion” OR “Acupuncture Points” OR “Acupuncture, Ear” OR “Acupuncture” OR “Acupuncture” OR “Massage” OR “Cupping therapy” AND “Labor Pain” AND “Randomized controlled trial.”
2.3. Inclusion criteria
Articles that met the following criteria were included:
(1) The participants were women who had given birth without other complications.
(2) TCM therapies, including different treatment modalities (e.g., acupuncture, massage, and acupuncture points), were studied in the intervention group (IG), and conventional labor treatment was applied in the control group (CG).
(3) The primary outcome was the pain condition during the phase of labor, measured using the Visual Analog Scale (VAS). The VAS is a tool with good reliability and validity for the measurement of pain. The scale involved a 100-mm long line with 2 extremes on the sides. The participants were required to indicate their current feelings on the line between the 2 extremes, with “0” indicating no pain and “10” denoting the most severe pain.
(4) The investigations were RCTs.
2.4. Exclusion criteria
(1) Animal studies, case reports, conferences, reviews, or meta-analyses.
(2) Duplicated articles or articles that have already been published in other journals.
(3) Articles with irrelevant content, unclear design, and inconsistent outcome indicators.
(4) Articles with incomplete data, especially for the lack of outcome indicators.
(5) Studies with unsuitable study design and/or unavailable data.
2.5. Data extraction and analysis
All articles included in the meta-analysis were screened and then extracted in accordance with the above inclusion/exclusion criteria independently by 2 researchers (Y.Y-.Y. and W.X-.J.). When they disagreed, the third researcher (D.N-.F.) made the final decision. All searched articles were downloaded from the literature management software Note Express.
Data were extracted in Excel, as follows: first author’s name, year of publication, publication country, characteristics of the participants such as age, sample size, treatment modalities of intervention and control groups, duration, etc.
2.6. Quality assessment
The quality of the included articles was evaluated using the Cochrane risk of bias tool, which included the following 6 aspects: selection bias, attrition bias, detection bias, reporting bias, performance bias, and other biases.
2.7. Data analysis
The data were statistically analyzed using Stata 16.0 software. The continuous variables were expressed as standardized mean difference (SMD) and 95% confidence interval (95% CI). The discontinuous variables were expressed as odds ratio (OR) and 95% Cl. The I2 statistic and P-values were adopted to investigate the statistical heterogeneity. First, a network plot was generated to comprehensively compare the direct and indirect evidence, and if it formed a closed loop, the inconsistency test was performed for exploration. Subsequently, a pairwise comparison of the different treatment modalities was drawn in the forest plot or league table. The probability comparison of different treatment modalities was then drawn based on the surface under the cumulative ranking curves (SUCRA) value. Finally, the funnel plot was constructed to identify publication bias.
3. Results
3.1. Literature selection
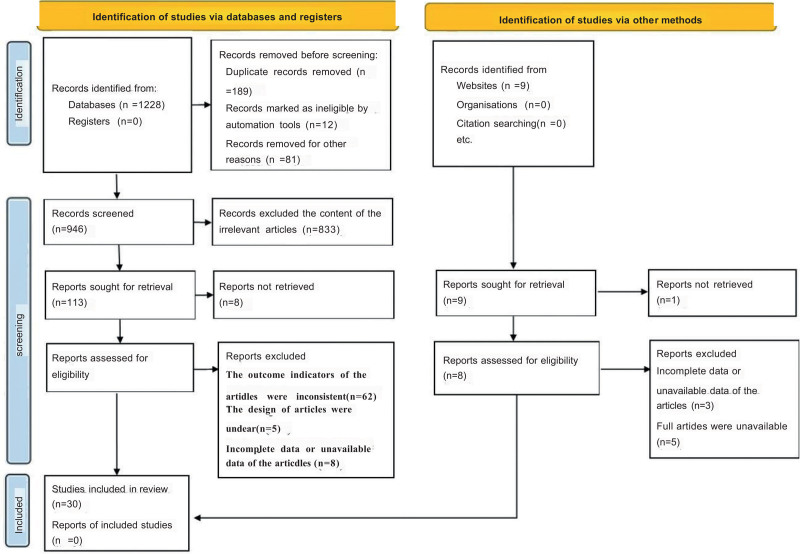
A total of 1228 articles were identified according to the above criteria. Initially, 282 articles were excluded, including 12 animal tests, 81 reviews or meta-analyses, and 189 duplicate papers. After reviewing the titles and abstracts, 900 articles were excluded because of irrelevant content (n = 833), unclear design (n = 5), and inconsistent outcome indicators (n = 62). Upon screening the full text of the remaining 46 articles, 8 articles were excluded owing to incomplete and unavailable data (n = 8). Finally, 30 articles were included in the NMAh (Fig. 1).
Figure 1.
Flow chart of study selection.
3.2. Characteristics of the studies involved
A total of 30 articles with 3277 participants (1923 people in the IG and 1354 individuals in the CG) were included in the NMA. All participants were pregnant women aged 21 to 29 years and a gestational age of 37 to 42 weeks. Table 1 lists the detailed characteristics of the included studies. Routine labor treatment included the use of a simple saline infusion, and the patients were made immobile and lying in a lateral position. Apart from the acupressure practice, the women were encouraged to get out of bed, sit, and/or walk around as a part of their routine care.
Table 1.
Characteristics of included articles.
| Study | Year | Participants | Sample size (IG/CG) |
Age (mean ± SD) (IG/CG) |
Gestational age (mean ± SD) (IG/CG) | Treatment modality | Outcomes | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Xin Y | 2021 | Pregnant women | 30/30 | 27.35 ± 2.56 | 28.58 ± 5.12 | 39.85 ± 0.57 | 40.05 ± 0.32 | d | a | ③④⑦⑧ |
| Liuru X | 2021 | Pregnant women | 48/48 | 23.62 ± 1.21 | 23.35 ± 1.06 | 39.52 ± 0.61 | 39.16 ± 0.53 | e + else | a | ⑥⑦⑧ |
| Yan Z | 2020 | Pregnant women | 43/43 | 26.12 ± 3.21 | 26.33 ± 3.12 | 38.69 ± 2.36 | 38.26 ± 2.25 | e | a | ⑥⑦⑧ |
| Shiyun C | 2019 | Pregnant women | 30/30 | 26.00 ± 5.00 | 28.00 ± 5.00 | 39.01 ± 0.79 | 39.06 ± 0.81 | d | a | ⑦⑧ |
| Xia S | 2019 | Pregnant women | 76/76 | 27.82 ± 3.14 | 27.63 ± 3.62 | 39.41 ± 0.34 | 39.27 ± 0.31 | d | a | ③④⑤⑥⑦⑨ |
| Dejuan C | 2019 | Pregnant women | 60/60 | 29.58 ± 2.47 | 29.54 ± 2.64 | 39.64 ± 1.37 | 39.62 ± 1.25 | e + else | a | ⑥⑦⑧ |
| Mei X | 2018 | Pregnant women | 62/62 | 26.40 ± 5.50 | 26.70 ± 5.60 | 39.50 ± 1.10 | 39.40 ± 1.00 | c + d | c | ①②⑨ |
| Junran C | 2018 | Pregnant women | 40/40 | 25.03 ± 1.93 | 25.36 ± 1.71 | 39.08 ± 0.71 | 39.32 ± 0.69 | e + else | a | ⑥⑦⑨ |
| Lingfei H | 2018 | Pregnant women | 35/35 | 25.60 ± 2.30 | 25.20 ± 2.70 | 38.00 ± 1.70 | 37.30 ± 1.50 | e | a | ⑥⑦⑨ |
| Fenglian Y | 2017 | Pregnant women | 160/160 | 27.20 ± 1.30 | 27.50 ± 1.60 | 38.90 ± 0.70 | 39.20 ± 0.90 | e + else | b | ⑦⑨ |
| Yan Z | 2017 | Pregnant women | 84/49 | 27.00 ± 3.00 | 27.00 ± 3.00 | 39.10 ± 4.80 | 39.30 ± 4.10 | d | a | ①②⑤⑦⑨ |
| 28/49 | 28.00 ± 3.00 | 27.00 ± 3.00 | 39.50 ± 3.90 | 39.30 ± 4.10 | c | a | ||||
| 30/49 | 27.00 ± 4.00 | 27.00 ± 3.00 | 39.10 ± 5.00 | 39.30 ± 4.10 | c + d | a | ||||
| Yan Z | 2016 | Pregnant women | 40/40 | 28.40 ± 5.30 | 28.10 ± 3.50 | 39.10 ± 4.80 | 39.30 ± 4.10 | d | a | ①②⑦⑨ |
| 40/40 | 27.50 ± 3.20 | 28.10 ± 3.50 | 39.50 ± 3.90 | 39.30 ± 4.10 | c | a | ||||
| Guangxia C | 2016 | Pregnant women | 60/60 | 28.60 ± 6.80 | 28.10 ± 6.30 | 39.10 ± 5.60 | 38.70 ± 5.20 | e + else | a | ⑥⑦⑧ |
| Jing L | 2016 | Pregnant women | 45/42 | 29.10 | 28.20 | 37.00–42.00 | e | a | ⑥⑦⑨ | |
| Chunhua Q | 2015 | Pregnant women | 24/24 | 23.20 ± 3.20 | 23.50 ± 3.50 | 40.10 ± 4.20 | 39.80 ± 4.50 | c + d | c | ⑤⑦⑧⑨ |
| Xiaohui L | 2015 | Pregnant women | 42/42 | 24.00 ± 3.00 | 26.00 ± 3.00 | 39.14 ± 1.13 | 39.83 ± 0.90 | d | a | ②③④⑤⑦⑧ |
| Li H | 2015 | Pregnant women | 64/64 | 27.45 ± 2.35 | 26.72 ± 2.01 | 38.13 ± 0.40 | 38.05 ± 0.42 | c + d | c | ⑥⑧ |
| Baohong W | 2015 | Pregnant women | 60/60 | 26.40 ± 2.10 | 25.40 ± 1.50 | 37.00–4l.00 | 37.00–40.00 | c + e | a | ⑤⑨ |
| Baohong W et al | 2015 | Pregnant women | 60/60 | 26.40 ± 2.10 | 37.00–42.00 | c + e | a | ⑤⑦⑨ | ||
| 60/60 | 26.40 ± 2.10 | 37.00–42.00 | c | a | ||||||
| Yanhui T | 2014 | Pregnant women | 35/35 | 26.20 ± 3.50 | 39.00 ± 1.00 | e | a | ⑥⑦⑧⑨ | ||
| Xiaoling Y | 2014 | Pregnant women | 75/90 | 28.42 ± 3.49 | 27.63 ± 4.28 | 39.71 ± 0.86 | 39.86 ± 1.00 | d + e | a | ②③④⑨ |
| Jinyan T | 2013 | Pregnant women | 40/40 | 26.00 ± 2.81 | 39.56 ± 6.62 | d | a | ⑤⑥⑦⑧ | ||
| Xiaohui L | 2013 | Pregnant women | 32/35 | 26.00 ± 3.45 | 26.00 ± 1.13 | 39.42 ± 1.13 | 39.85 ± 0.95 | d | a | ②③④ |
| 32/35 | 25.00 ± 3.18 | 26.00 ± 1.13 | 39.42 ± 0.91 | 39.85 ± 0.97 | c | a | ||||
| MIAO Jin | 2012 | Pregnant women | 40/30 | 22.00–38.00 | 22.00–38.00 | - | - | d | a | ①②③④⑥⑦⑧⑨ |
| Hamideh Torkiyan | 2021 | Pregnant women | 58/58 | 22.71 ± 3.54 | 22.14 ± 3.46 | 37.00–41.00 | e | a | ⑨ | |
| 58/58 | 23.17 ± 4.25 | 22.14 ± 3.46 | 37.00–41.00 | b | a | |||||
| Yasemin Hamlaci | 2017 | Pregnant women | 44/44 | 21.11 ± 3.83 | 37.00–40.00 | e | a | ⑦⑧ | ||
| Wu Lingling | 2017 | Pregnant women | 43/43 | 25.00 ± 3.20 | 25.80 ± 3.10 | 40.26 ± 1.06 | 39.89 ± 0.77 | d | a | ⑤⑦⑧ |
| 45/43 | 25.80 ± 3.30 | 25.80 ± 3.10 | 40.17 ± 1.07 | 39.89 ± 0.77 | c | a | ||||
| Reginaldo Roque Mafetoni | 2016 | Pregnant women | 10/10 | 22.20 ± 6.30 | 22.90 ± 4.50 | ≥37.00 | ≥37.00 | d | a | ①②⑨ |
| 10/10 | 22.80 ± 5.80 | 22.90 ± 4.50 | ≥37.00 | ≥37.00 | b | a | ||||
| Kiymet Yesilcicek Calik | 2014 | Pregnant women | 50/50 | - | - | 38.00–41.00 | e | a | ⑨ | |
| Fatemeh Dabiri and Arefeh Shahi | 2014 | Pregnant women | 50/49 | 25.46 ± 4.48 | 25.48 ± 5.7 | 39.22 ± 1.01 | 38.76 ± 0.91 | b | a | ①② |
| 50/49 | 25.00 ± 6.25 | 25.48 ± 5.70 | 39.98 ± 1.55 | 38.76 ± 0.91 | e | a | ||||
Notes: a: Routine labor treatment, b: placebos, c: autonomic nerve block, d: acupuncture, e: acupressure, d + e: acupressure + acupuncture, c + d: autonomic nerve block + acupuncture, c + e: acupressure + autonomic nerve block, e + else: acupressure + else. ① Pain of labor at the time of 30-minutes, ② pain of labor at the time of 60-minutes, ③ pain of the first stage of labor, ④ pain of the second stage of labor, ⑤ duration of active phase, ⑥ duration of the first stage of labor, ⑦ duration of the second stage of labor, ⑧ duration of the third stage of labor, ⑨ Apgar scores.
In this study, routine labor treatment (a), placebo (b), and autonomic nerve block (c) were applied in the CG, whereas TCM-related treatment modalities (acupuncture (d), acupressure (e), acupressure + acupuncture (d + e)) and the related combined treatment modalities (c + d, c + e, and e + else) were applied in the IG. To be specific, “else” included emotional intervention, Lamaze breath, and childbearing ball.
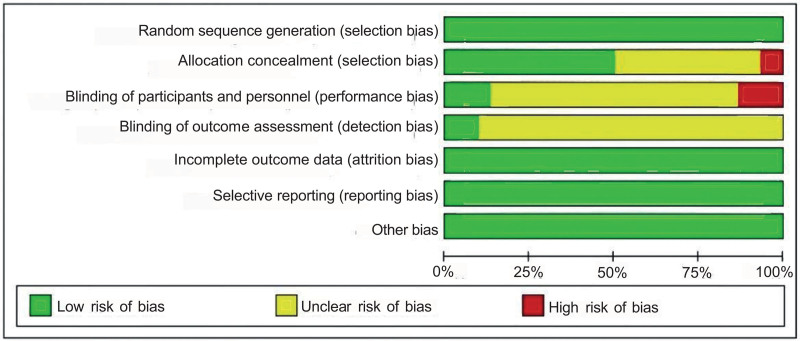
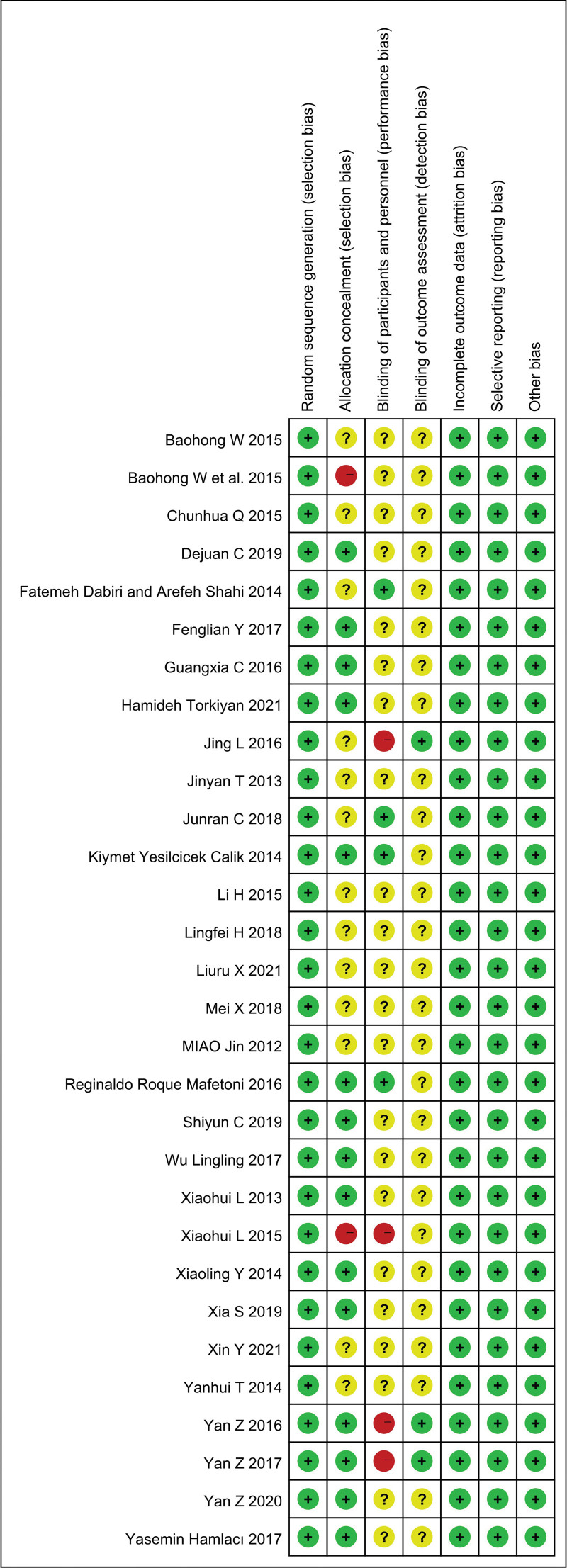
3.3. Quality assessment
The findings indicated that the quality of all the included articles was generally good, as assessed using the Cochrane risk of bias tool. For allocation concealment, 2 articles (Baohong W et al (2015) and Xiaohui L (2015)) were considered at high risk. For the blinding of participants and personnel, 4 (Jing L(2016), Xiaohui L (2015), Yan Z (2016), and Yan Z (2017)) were considered at high risk of bias. For the blinding of outcome assessment, most articles were considered unclear (Figs. 2 and 3).
Figure 2.
Risk of bias graph.
Figure 3.
Risk of bias summary.
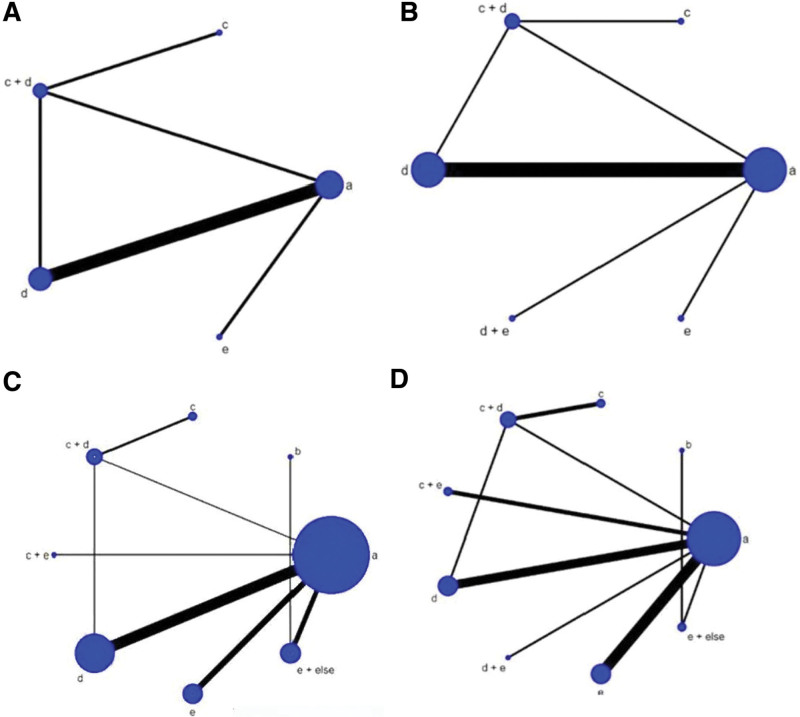
3.4. Network meta-analysis
The size of the nodes signified the number of participants in each group, and the width of lines between the nodes represented the number of articles for assessing each treatment modality. In the network plots, the combined treatment modalities were denoted with “+” signs.
The network plot is depicted in Figure 4A–D, including the pain at 30 minutes and 60 minutes, the duration of the second stage of labor, and Apgar scores, respectively. As shown in Figure 4, the number of articles comparing “routine labor treatment” and “acupuncture” was the largest, and the number of participants in “routine labor treatment” was the highest. Other related results are presented in Figure S1A–S1E, Supplemental Digital Content, http://links.lww.com/MD/N713 for the network of the duration of the stage of labor and the Apar score.
Figure 4.
(A–D) Network plots for the pain of stage of labor, duration of the stage of labor and Apgar scores. (a): Routine labor treatment, (b) placebo, (c) autonomic nerve block, (d) acupuncture; (e) acupressure, (d + e) acupressure + acupuncture, (c + d) autonomic nerve block + acupuncture, (c + e) acupressure + autonomic nerve block, (e + else) acupressure + else.
3.5. Pain of time of labor and duration of stage of labor
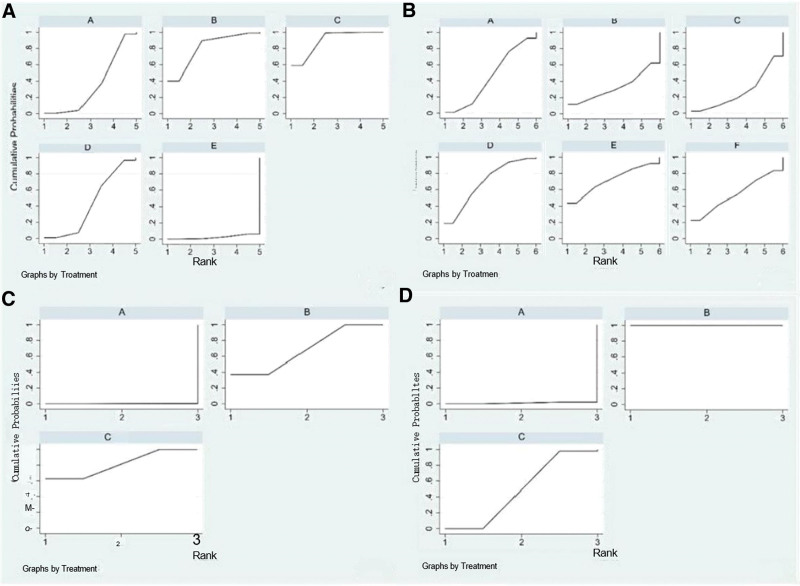
Regarding the pain of labor at the time of 30 minutes, 6 articles involving 5 treatment modalities and encompassing 556 participants (316 pregnant women were in the IG, and 240 pregnant women were in the CG) recorded the VAS at the 30-minute stage of labor. As depicted in Figure 5A, of the various treatment modalities, acupressure was found to be the optimum modality in terms of decreasing the pain of labor at the time of 30 minutes. This method was better than the autonomic nerve block of the CG and the combined acupuncture of the IG, and the difference was statistically significant (SMD = 5.76, 95% CI = [0.72, 10.80] and SMD = 6.09, 95% CI = [2.03, 10.16]). The league table is presented in Table S2A, Supplemental Digital Content, http://links.lww.com/MD/N714. The results of SUCRA indicated that autonomic nerve block + acupuncture had the highest probability of becoming the optimal treatment modality. The effect ranking of the treatment modalities for the pain of labor at 30 minutes was autonomic nerve block + acupuncture (SUCRA: 89.2%) > autonomic nerve block (SUCRA: 80.8%) > acupuncture (SUCRA: 42.8%) > routine labor treatment (SUCRA: 34.8%) > acupressure (SUCRA: 2.4%) (Fig. 6A).
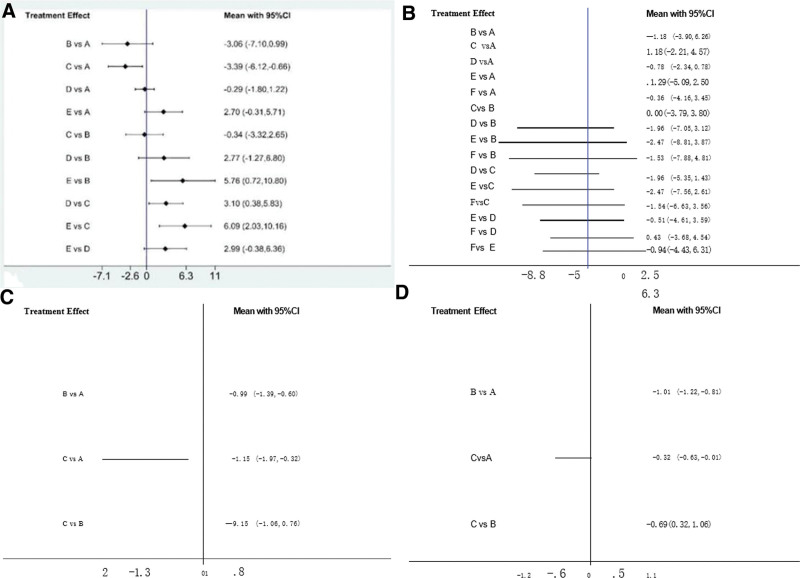
Figure 5.
(A–D) Forest plots for pain of time of labor and duration of stage of labor. Notes: Pain of 30-minutes labor stage: A: routine labor treatment, B: autonomic nerve block, C: autonomic nerve block + acupuncture, D: acupuncture, E: acupressure. Pain of 60-minute labor stage: A: routine labor treatment, B: autonomic nerve block, C: autonomic nerve block + acupuncture, D: acupuncture, E: acupressure + acupuncture, F: acupressure. Pain of the first labor stage: A: routine labor treatment, B: acupuncture, C: acupressure + acupuncture. Pain of the second labor stage: A: routine labor treatment, B: acupuncture, C: acupressure + acupuncture.
Figure 6.
(A–D) Treatment ranking (SUCRA) for pain of time of labor and duration of stage of labor. Notes: the meaning of the letters is given in Table S1 (see Table S1, Supplemental Digital Content, http://links.lww.com/MD/N714 which illustrates the meaning of the letters). Notes: Pain of 30-minute labor stage: A: routine labor treatment, B: autonomic nerve block, C: autonomic nerve block + acupuncture, D: acupuncture, E: acupressure. Pain of 60-minute labor stage: A: routine labor treatment, B: autonomic nerve block, C: autonomic nerve block + acupuncture, D: acupuncture, E: acupressure + acupuncture, F: acupressure. Pain of the first labor stage: A: routine labor treatment, B: acupuncture, C: acupressure + acupuncture. Pain of the second labor stage: A: routine labor treatment, B: acupuncture, C: acupressure + acupuncture.
Regarding the pain of labor at 60 minutes, 9 articles encompassing 872 participants (465 pregnant women were in the IG, and 470 were in the CG) in 6 treatment modalities contributed to this analysis. As depicted in Figure 5B, acupressure + acupuncture was better than the treatment modalities in the IG (autonomic nerve block + acupuncture [SMD = −2.47 95% CI = (−7.56, 2.61)] and acupuncture (SMD = −0.51 95% CI = [−4.61, 3.59])). Moreover, it was better than certain treatments in the CG (routine labor treatment [SMD = 1.29, 95% CI = (−5.09, 2.50) and autonomic nerve block [SMD = −2.47, 95% CI = (−8.81, 3.87)]). The league table is presented in Table S2B, Supplemental Digital Content, http://links.lww.com/MD/N714. The results of SUCRA indicated that acupressure + acupuncture had the highest probability of becoming the optimal treatment modality. As depicted in Figure 6B, the effect ranking of the treatment modalities from best to worst in terms of pain of labor at 60 minutes was as follows: acupressure + acupuncture (SUCRA: 71.9%) > acupuncture (SUCRA: 68.9%) > acupressure (SUCRA: 54.5%) > routine labor treatment (SUCRA: 45.0%) > autonomic nerve block (SUCRA: 32.7%) > autonomic nerve block + acupuncture (SUCRA: 26.9%).
Regarding pain in the first stage of labor, 6 articles that encompassed 598 participants (295 pregnant women in the IG, and 303 pregnant women in the CG) and 3 treatment modalities contributed to this analysis. Acupressure + acupuncture and acupuncture were the optimal treatment modalities for decreasing the pain in the first stage of labor compared with routine labor treatment, and the difference was statistically significant (SMD = −0.99 95% CI = [−1.39, −0.60] and SMD = −1.15, 95% CI = [−1.97, 0.32]). The forest plot is presented in Figure 5C. The league table is presented in Table S2C, Supplemental Digital Content, http://links.lww.com/MD/N714. Based on the ranking probabilities of Figure 6C, acupressure + acupuncture (SUCRA: 81.2%) had the optimal possible effect in reducing the pain in the first stage of labor, with acupuncture (SUCRA: 68.7%) ranking as the second and routine labor treatment (SUCRA: 0.1%) as the third.
Regarding pain in the second stage of labor, 6 articles measured pain using the VAS in the second stage of labor, and these included 3 treatment modalities and 598 participants (295 pregnant women were in the IG, and 303 pregnant women were in the CG). The findings suggested that compared with routine labor treatment, 2 TCM-related treatment modalities, namely acupuncture (SMD = −1.01, 95% CI = [−1.22, −0.81]) and acupressure + acupuncture (SMD = −0.32, 95% CI = [−0.63, −0.01]) (Figure 5D), significantly alleviated pain in the second stage of labor. Moreover, the league table is presented in Table S2D, Supplemental Digital Content, http://links.lww.com/MD/N714. Figure 6D depicts the probable ranking of pain in the second stage of labor. Acupuncture (SUCRA: 100.0%) had the highest probability of becoming the optimal treatment modality. Routine labor treatment (SUCRA: 1.0%) was likely to be the worst treatment modality.
3.6. Durations of each stage of labor
Regarding the duration of the first stage of labor, 11 articles with 5 treatment modalities and 1034 participants (522 pregnant women were in the IG, and 512 pregnant women were in the CG) recorded the duration of the first stage of labor. As demonstrated in Figure S2A (see Figure S2A, Supplemental Digital Content, http://links.lww.com/MD/N713 which illustrates a pairwise comparison of the different treatment modalities), acupressure combined with delivery ball, emotional intervention, etc, was the optimal treatment modality with regard to reducing the duration of the first stage of labor compared with other modalities (acupressure, acupuncture, and routine labor treatment), and the difference was statistically significant (SMD = −2.33 95% CI = [−4.08, −0.59]; SMD = −3.34, 95% CI = [−5.21, −1.46]; and SMD = −4.15, 95% CI = [−5.39, −2.90], respectively). The treatment modality of acupressure significantly alleviated the pain in the first stage of labor compared with routine labor treatment (SMD = −1.82, 95% CI = [−3.04, −0.59]). The league table is presented in Table S2E, Supplemental Digital Content, http://links.lww.com/MD/N714. Acupressure + else was probably the optimal treatment modality. The effect ranking of the treatment modalities from best to worst was acupressure combined with the delivery ball, emotional intervention, etc, (SUCRA: 99.8%) > acupressure (SUCRA: 61.8%) > acupuncture (SUCRA: 34.0%) > routine labor treatment (SUCRA: 4.4%) (see Figure S3A, Supplemental Digital Content, http://links.lww.com/MD/N713 which illustrates the effect ranking of the treatment modalities).
Regarding the duration of the second stage of labor, 22 articles that included 2268 participants (1173 pregnant women were in the IG and 1095 pregnant women are in the CG) and 8 treatment modalities contributed to this analysis. As demonstrated in Figure S2B (see Figure S2B, Supplemental Digital Content, http://links.lww.com/MD/N713 which illustrates a pairwise comparison of the different treatment modalities), the results showed that the treatment modality of acupressure combined with delivery ball, emotional intervention, etc, significantly reduced the duration of the second stage of labor compared with the CG (routine labor treatment [SMD = −2.39, 95% CI = (−3.30, −1.49)] and autonomic nerve block [SMD = −2.54, 95% CI = (−4.75, −0.33)]). Moreover, it was better than certain treatments in the IG (autonomic nerve block + acupuncture [SMD = −2.53, 95% CI = (−4.35, −0.72)]; acupressure + autonomic nerve block [SMD = −2.24, 95% CI = (−4.23, −0.26)]; acupuncture [SMD = −2.33, 95% CI = (−3.41, −1.25)]; and acupressure [SMD = −2.28, 95% CI = (−3.49, −1.07)]), and the difference was statistically significant. The league table is presented in Table S2F, Supplemental Digital Content, http://links.lww.com/MD/N714 for comprehensive analysis. Figure S3B (see Figure S3B, Supplemental Digital Content, http://links.lww.com/MD/N713 which illustrates the effect ranking of the treatment modalities) provides the ranking of the duration of the second stage of labor in the cumulative probability plots. The treatment modality of acupressure combined with delivery ball, emotional intervention, etc, (SUCRA: 93.7%) was probably the optimal option, and the treatment modality of autonomic nerve block + acupuncture (SUCRA: 30.9%) was probably the worst option.
Regarding the duration of the third stage of labor, 12 articles involving 4 treatment modalities and 1020 participants (515 pregnant women were in the IG, and 505 pregnant women were in the CG) recorded the duration of the third stage of labor. As depicted in Figure S2C (see Figure S2C, Supplemental Digital Content, http://links.lww.com/MD/N713 which illustrates a pairwise comparison of the different treatment modalities), acupressure combined with the delivery ball, emotional intervention, etc, was the optimal treatment modality for shortening the period of the third stage of labor. This method had a statistically significant effect in shortening the duration of this stage of labor when compared with acupuncture [SMD = −0.73, 95% CI = (−1.45, −0.02)] and routine labor treatment [SMD = −0.88, 95% CI = (−1.46, −0.30)]. The league table is presented in Table S2G, Supplemental Digital Content, http://links.lww.com/MD/N714 for comprehensive analysis. Based on the ranking probabilities of Figure S3C (see Figure S3C, Supplemental Digital Content, http://links.lww.com/MD/N713 which illustrates the effect ranking of the treatment modalities), acupressure combined with delivery ball, emotional intervention, etc, (SUCRA: 98.0%) had the probability of becoming the optimal TCM treatment modality for shortening the third stage of labor.
Regarding the duration of the active phase, 8 articles that included 5 treatment modalities and 851 participants (457 pregnant women were in the IG and 394 pregnant women were in the CG) contributed to this analysis. As depicted in Figure S2D (see Figure S2D, Supplemental Digital Content, http://links.lww.com/MD/N713 which illustrates a pairwise comparison of the different treatment modalities), the treatment modality of acupressure + autonomic nerve block was found to significantly reduce the duration of the active phase of labor compared with certain treatment modalities in the CG (autonomic nerve block [SMD = −1.98, 95% CI = (−3.71, −0.25)] and routine labor treatment [SMD = −2.17, 95% CI = (−3.26, −1.08)]). Moreover, it was better than some treatments in the IG (acupuncture [SMD = −1.63, 95% CI = (−0.45, −2.82)] and autonomic nerve block + acupuncture [SMD = −1.93, 95% CI = (−3.23, −0.63)]). The league table is presented in Table S2H, Supplemental Digital Content, http://links.lww.com/MD/N714 for comprehensive analysis. The results of SUCRA indicated that acupressure + autonomic nerve block (SUCRA: 99.5%) was probably the optimal treatment modality (see Figure S3D, Supplemental Digital Content, http://links.lww.com/MD/N713 which illustrates the effect ranking of the treatment modalities).
3.7. Apgar scores
A total of 12 articles (n = 1860; 944 pregnant women were in the IG, and 916 were in the CG) recorded the Apgar scores.[26] As depicted in Figure S2E (see Figure S2A, Supplemental Digital Content, http://links.lww.com/MD/N713 which illustrates a pairwise comparison of the different treatment modalities), the treatment modality of acupressure combined with the delivery ball, emotional intervention, etc, was the optimal one. This method exhibited statistically significant differences when compared with the placebo in terms of newborn safety [SMD = 0.72, 95% CI = (0.11, 1.33)]. The details are presented in Table S2I, Supplemental Digital Content, http://links.lww.com/MD/N714 for comprehensive analysis. Based on cumulative probability plots and SUCRA (see Figure S3E, Supplemental Digital Content, http://links.lww.com/MD/N713 which illustrates the effect ranking of the treatment modalities), acupressure combined with the delivery ball, emotional intervention, etc, (SUCRA: 82.9%) was probably the optimal option, and the placebo (SUCRA: 26.2%) was probably the worst option.
3.8. Publication bias
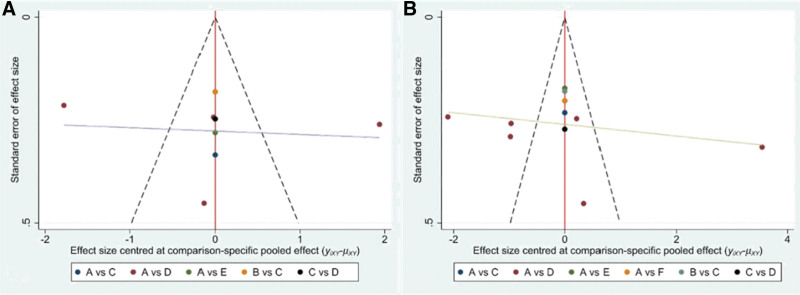
The funnel plots for the pain of the stage of labor at 30 minutes and 60 minutes are presented in Figure 7A and B to evaluate publication bias. The graphs were completely symmetrical visually, and each of the adjusted auxiliary lines was perpendicular to the center line. Thus, the results indicated the absence of significant publication bias. Other related findings are presented in Figures S4A–S4G, Supplemental Digital Content, http://links.lww.com/MD/N713 for the network of the funnel graph.
Figure 7.
(A and B) Funnel plots of publication bias.
4. Discussion
This NMA is a comprehensive analysis of currently available data regarding the effect of TCM-related treatment modalities on labor pain among pregnant women. This study examined the effects of diverse treatment modalities on different stages of labor pain, duration of labor, and newborn Apgar scores in pregnant women. Several systematic reviews have previously reported that acupuncture and/or acupressure might reduce pain when combined with pharmacological treatment methods.[1–14] However, to the best of our knowledge, studies on the direct or indirect effects of TCM non-pharmacological treatment methods on different stages of labor are insufficient. Several areas of uncertainty prevail, including the integration of these therapeutic modalities, the selection of the optimal point, and the length of time for point massage, which need to be investigated. Therefore, it is important to compare our findings with those of previous studies. The NMA results indicated that combined treatment modalities related to acupuncture exhibited the highest efficacy in decreasing pain in different stages of labor, shortening the stage of labor, and enhancing newborn safety.
The key findings of this study signify that combined treatment modalities pertaining to acupuncture were most effective in alleviating pain at different time points during labor, which agrees with previous research.[21] There are 2 main hypotheses regarding the mechanism by which acupressure exerts its positive effects on labor pain relief. Massage is known to stimulate large fast nerve fibers (unmyelinated C fibers) and block the smaller, slower nerve fibers (myelinated A fibers) that detect pain. This effect presumably produces a local lateral inhibition in the spinal cord [1-Hall-2016]. Massage can result in the secretion of various chemicals, such as endorphins, which are natural analgesics. According to the gate control theory, these chemicals may close nerve gates and prevent the stimulation signals from being transmitted to the central nervous system.[27] Regarding the mechanism of TCM, qi is one of the invisible circuitries of meridians (energy channels) in the body and could affect mental or physical health according to its flow.[6–29] During labor, obstruction of the meridians and blockage of the qi occur. During acupressure, pressure is applied with the fingers to stimulate the unblocking of the meridians, thereby correcting the flow of qi and restoring the equilibrium at certain acupuncture points.[6–30] Our research yielded definitive results, and the addition of acupuncture based on acupressure was most effective in reducing the VAS scores when the pain lasted 60 minutes. There was no significant difference between the various modalities, and the reason could be that the release of previous chemicals of blood was activated, the transmission of electromagnetic signals was accelerated, and the blood flow was regulated.[3–21] In our study results, the collected RCTs indicated that individual or combined acupressure treatments maintained an analgesic effect in the 1st and 2nd phases of labor compared with the CG (routine labor treatment, placebo, and autonomic nerve block). It is worth noting that our study differs from previous studies as acupressure was applied on LI4, which is better for relief from the pain of labor at 30 minutes and 60 minutes. Furthermore, our findings revealed that combining acupuncture with acupressure was effective in relieving pain in the first stage of labor. Therefore, we intend to further investigate the effect of acupressure and combined acupuncture with acupressure on pain in various stages of labor.
Moreover, this study suggested that acupressure-related combined TCM treatment modalities are the preferred choice to shorten the duration of the stage of labor. The findings further showed that acupressure combined with non-pharmacological methods, such as emotional intervention, Lamaze breath, and childbearing ball, is effective in shortening the duration of labor, especially in the first stage, which is consistent with previous findings.[31,32] A review has previously observed that massage can significantly shorten the duration of the stage of labor by increasing the secretion of oxytocin from the pituitary gland to regulate uterine contractions.[6–18] Furthermore, investigations have reported that the posture of applying non-pharmacological treatment methods, such as a childbearing ball or yoga, can promote the fetus to slide into the birth canal quickly via the forward-leaning movement and semi-recumbent position.[32] Therefore, we speculate that combined acupuncture related could had more effective outcome, acupressure combined with delivery ball, emotional intervention and so on, could produce effective outcomes. In addition, adding an autonomic nerve block is effective, especially in shortening in duration of the third and active phases, based on acupuncture. However, the overall duration of labor was not analyzed because of insufficient data in the included studies. Further studies are therefore required to confirm the above finding.
With regard to the Apar score, the optimum treatment modality for improving this score was acupressure-related combined non-pharmacological treatment modalities, according to the forest plot result (Figure S2E, Supplemental Digital Content, http://links.lww.com/MD/N713). Massage is known to offer numerous benefits (e.g., alleviating labor pain and shortening the stage of labor) although it has certain side effects on pregnant women.[27,33–35] Accordingly, we hypothesize that it could have a positive impact on newborn Apgar scores (The score comprises 5 components [heart rate, respiratory effort, muscle tone, reflex irritability, and color], and each is assigned a value from 0 to 2. Thus, total scores range from 0 to 10, with higher scores indicating a better physical condition. The Apgar score was developed primarily to assess term infants during a time when neonatal mortality was very high among preterm infants. The frequency of low Apgar scores increases with decreasing gestational age and may reflect biological immaturity in preterm infants) in some related indicators. However, more experimental articles should be included and researched to verify our conclusion in the future.
There are 2 limitations to this study. One of the limitations of the collected RCTs is that they cannot be generalized to all pregnant women as the outcomes were limited to labor pain experienced by limited women with fixed baseline data. The other limitation is that the main outcome of the VAS is based on personal subjective feelings without uniform objective criteria, which can considerably impact the accuracy of the results. Owing to the limitations of this meta-analysis, we hope to incorporate more investigations in future studies so that the findings can be generalized to other populations, albeit with caution.
5. Conclusion
According to the results of this NMA, TCM treatment modalities offered significantly higher efficacy than routine labor treatment in terms of decreased pain in various stages of labor, shortened stage of labor, and increased Apgar scores. Thus, the application of the combined TCM treatment modalities can be recommended according to the outcomes of the pregnant women, such as pain and duration of the stage of labor. Encouraged by these data, we aim to explore the clinical TCM therapy more accurately in further studies for relieving maternal pain. A combined treatment of acupressure and acupuncture is the most effective approach in relieving labor pain and shortening the duration of labor. Thus, based on this finding, more research should be conducted in the future on the combination of TCM therapy for various TCM treatment modalities.
Acknowledgments
Special gratitude is owed to information specialists and librarians at Inner Mongolia Minzu University who supported this review work.
Author contributions
Conceptualization: Danni Fu, Xue Bai, Song Zhang.
Data curation: Rui Chen.
Funding acquisition: Xue Bai.
Writing – original draft: Yangyang Yi, Wenxuan Ju.
Supplementary Material
Abbreviations:
- 95% CI
- 95% confidence interval
- CG
- control group
- IG
- intervention group
- NMA
- network meta-analysis
- RCT
- randomized controlled trials
- SMD
- standardized mean difference
- SUCRA
- the surface under the cumulative ranking curve
- TCM
- traditional Chinese medicine
- VAS
- Visual Analog Scale.
Inner Mongolia Minzu University medical information and data mining research team.
As this review was based on published research, no ethical approval was required.
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Supplemental Digital Content is available for this article.
The protocol was registered in PROSPERO (CRD42022336091).
How to cite this article: Yi Y, Ju W, Fu D, Chen R, Bai X, Zhang S. Effect of traditional Chinese medicine therapy on labor pain in patients with natural childbirth: A network meta-analysis. Medicine 2024;103:43(e39425).
YY, WJ, and DF contributed equally to this work.
Contributor Information
Yangyang Yi, Email: 13948509585@139.com.
Wenxuan Ju, Email: 454332672@qq.com.
Danni Fu, Email: fu_dan_ni@126.com.
Song Zhang, Email: zhangsong_0919@163.com.
References
- [1].Zaneta JS, Marcin S. Anaesthesia of pregnant women. Ginekol Pol. 2021;92:735–40. [DOI] [PubMed] [Google Scholar]
- [2].Afshin GB, Abolfazl F, Farshad HK, et al. Bolus administration of intravenous lidocaine reduces pain after an elective caesarean section: findings from a randomised, double-blind, placebo-controlled trial. J Obstet Gynaecol. 2017;37:566–70. [DOI] [PubMed] [Google Scholar]
- [3].Kerry S, Shannon LJ, Heather DH, Kristine K, Sherry HS. Prenatal fear of childbirth and anxiety sensitivity. J Psychosom Obstet Gynaecol. 2009;30:168–74. [DOI] [PubMed] [Google Scholar]
- [4].Waldenström U, Hildingsson I, Ryding E. Antenatal fear of childbirth and its association with subsequent caesarean section and experience of childbirth. BJOG. 2006;113:638–46. [DOI] [PubMed] [Google Scholar]
- [5].Bolbol Haghighi N, Shayan A, Kazemi F, Masumi Z. The effect of using birth ball on maternal and neonatal outcomes: a randomized clinical trial. Avicenna J Nurs Midwifery Care. 2017;25:18–23. [Google Scholar]
- [6].Fereshteh J, Fatemeh S, Hamid H, et al. Yoga during pregnancy: the effects on labor pain and delivery outcomes (A randomized controlled trial). Complement Ther Clin Pract. 2017;27:1–4. [DOI] [PubMed] [Google Scholar]
- [7].Mansoreh Y, Arezoo P. The effect of aromatherapy with lavender essence on severity of labor pain and duration of labor in primiparous women. Complement Ther Clin Pract. 2016;25:81–6. [DOI] [PubMed] [Google Scholar]
- [8].Semra AC, Serap K. The effect of sacral massage on labor pain and anxiety: a randomized controlled trial. Jpn J Nurs Sci. 2020;17:e12272. [DOI] [PubMed] [Google Scholar]
- [9].Dabiri F, Shahi A. The Effect of LI4 acupressure on labor pain intensity and duration of labor: a randomized controlled trial. Oman Med J. 2014;29:425–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Bolanthakodi C, Raghunandan C, Saili A, Mondal S, Saxena P. Prenatal yoga: effects on alleviation of labor pain and birth outcomes. J Altern Complement Med (New York, N.Y.). 2018;24:1181–8. [DOI] [PubMed] [Google Scholar]
- [11].Mohyadin E, Ghorashi Z, Molamomanaei Z. The effect of practicing yoga during pregnancy on labor stages length, anxiety and pain: a randomized controlled trial. J Complement Integr Med. 2020;18:413–7. [DOI] [PubMed] [Google Scholar]
- [12].Rajavadi T, Kuntharee T, Theera T. Efficacy of aromatherapy for reducing pain during labor: a randomized controlled trial. Arch Gynecol Obstet. 2018;297:1145–50. [DOI] [PubMed] [Google Scholar]
- [13].Kelly M, Philippa M, Allan MC, Mandy M, Leanne J. Hypnosis for pain management during labour and childbirth. Cochrane Database Syst Rev. 2016;2016:CD009356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Oso´rio SMB, Silva JLGD, Nicolau AIO. Assessment of the effectiveness of non-pharmacological methods in pain relief during labor. Northeast Network Nurs J. 2014;15:174–84. [Google Scholar]
- [15].Stephanie LS, Noelle MS, Nicole LH. Dry cupping therapy for improving nonspecific neck pain and subcutaneous hemodynamics. J Athl Train. 2020;55:682–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Yasemin H, Saadet Y. The effect of acupressure applied to point LI4 on perceived labor pains. Holist Nurs Pract. 2017;31:167–76. [DOI] [PubMed] [Google Scholar]
- [17].Lin JG, Chen YH. The mechanistic studies of acupuncture and moxibustion in Taiwan. Chin J Integr Med. 2011;17:177–86. [DOI] [PubMed] [Google Scholar]
- [18].John KB. Traditional Chinese drug therapy. Drug News Perspect. 2003;16:698–702. [DOI] [PubMed] [Google Scholar]
- [19].Judith MS, Elizabeth MG, Jeanie LB, et al. Acupuncture and acupressure in labor. J Midwifery Womens Health. 2017;62:12–28. [DOI] [PubMed] [Google Scholar]
- [20].Caroline AS, Carmel TC, Kate ML, et al. Acupuncture or acupressure for pain management during labour. Cochrane Database Syst Rev. 2020;2:CD009232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Wang Y, Dai S, Yang AM. Effect evaluation of acupuncture combined with nerve block treatment on patients with lumbar spondylolisthesis. Int J Burns Trauma. 2021;11:177–183. eCollection 2021. [PMC free article] [PubMed] [Google Scholar]
- [22].José ALL, Wim VDN, Emily ETS, Sandra JW, Mark WL. Assessing metaregression methods for examining moderator relationships with dependent effect sizes: a monte carlo simulation. Res Synthesis Methods. 2017;8:435–50. [DOI] [PubMed] [Google Scholar]
- [23].Lu G, Ades AE. Combination of direct and indirect evidence in mixed treatment comparisons. Stat Med. 2004;23:3105–24. [DOI] [PubMed] [Google Scholar]
- [24].Caldwell DM, Ades AE, Higgins JPT. Simultaneous comparison of multiple treatments: combining direct and indirect evidence. BMJ. 2005;331:897–900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Ferrán CL, Aurelio T, Chris C, David M, Brian H. Network meta-analysis for comparing treatment effects of multiple interventions: an introduction. Rheumatol Int. 2014;34:1489–96. [DOI] [PubMed] [Google Scholar]
- [26].Apgar V. A proposal for a new method of evaluation of the newborn infant. Curr Res Anesth Analg. 1953;32:260–7. [PubMed] [Google Scholar]
- [27].Kim SK, Min A, Jeon C, et al. Clinical outcomes and cost-effectiveness of massage chair therapy versus basic physiotherapy in lower back pain patients: a randomized controlled trial. Medicine (Baltim). 2020;99:e19514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Robert BK, Joel W. Acupuncture for Pain. Am Fam Physician. 2019;100:89–96. [PubMed] [Google Scholar]
- [29].Zhang RX, Lao LX, Ren K, Brian MB. Mechanisms of acupuncture-electroacupuncture on persistent pain. Anesthesiology. 2014;120:482–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Zahra H, Sirati NM, Abbas E, Afzali M, Ali AM. Comparing the effects of ice massage and acupressure on labor pain reduction. Complement Ther Clin Pract. 2012;18:169–72. [DOI] [PubMed] [Google Scholar]
- [31].Lucie B, George AW, Stéphane P, et al. Ottawa Panel evidence-based clinical practice guidelines on therapeutic massage for low back pain. J Bodyw Mov Ther. 2012;16:424–55. [DOI] [PubMed] [Google Scholar]
- [32].Xie L, Zhu F, Zeng X. Effect analysis of acupoint massage combined with delivery ball in parturient labor analgesia. Chin Commun Doctors. 2021;13:049. [Google Scholar]
- [33].Emine Y, Sultan A, Sule G. The effect of ice pressure applied on large intestinal 4 on the labor pain and labor process. Complement Ther Clin Pract. 2018;32:25–31. [DOI] [PubMed] [Google Scholar]
- [34].Ilknur MG, Füsun T. Effects of massage and acupressure on relieving labor pain, reducing labor time, and increasing delivery satisfaction. J Nurs Res. 2020;28:e68. [DOI] [PubMed] [Google Scholar]
- [35].Kamilya JB, Muhammad HR, Adibah HI, Lee K, Boon HC. Effectiveness of breathing exercises, foot reflexology and back massage (BRM) on labour pain, anxiety, duration, satisfaction, stress hormones and newborn outcomes among primigravidae during the first stage of labour in Saudi Arabia: a study protocol for a randomised controlled trial. BMJ Open. 2020;10:e033844. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.