Abstract
Cutaneous tuberculosis is an infection caused by Mycobacteria tuberculosis, the rare Mycobacterium bovis and the bacillus Calmette-Guérin vaccine. This disease has many clinical types with diverse clinical manifestations, mainly includes lupus vulgaris, tuberculosis verrucosa cutis, orificial tuberculosis and scrofuloderma that are difficult to identify. We report a case of cutaneous tuberculosis in a female who presented with disseminated papular and nodular lesions on her face and hands. The results of skin biopsy, PCR, and IGRA test contributed to the diagnosis. All lesions were resolved leaving only superficial scars after 5 months treatment.
Keywords: mycobacterium infection, Mycobacterium tuberculosis, cutaneous tuberculosis, drug therapy
Introduction
Tuberculosis is a contagious disease that circulates widely and has infected approximately one-quarter of the global population.1 It causes infection in the lungs and other tissues, however the extrapulmonary tuberculosis are not notifiable in many regions. In recent years, due to the slower decrease comparing with pulmonary tuberculosis, there was an increase in proportion of extrapulmonary tuberculosis.2 Cutaneous tuberculosis is an uncommon form of extrapulmonary tuberculosis. It could arise through exogenous inoculation but is more frequently through endogenous spread of the pathogen.3 This disease could manifest as different clinical types include primary inoculation tuberculosis, tuberculosis verrucosa cutis, lupus vulgaris, scrofuloderma, metastatic tuberculosis abscesses, orificial tuberculosis, and miliary tuberculosis. The patients commonly have no tuberculosis infection symptoms or records, and endure a prolonged misdiagnosis. This is a rare case of disseminated cutaneous tuberculosis in a 38-year-old female.
Case Presentation
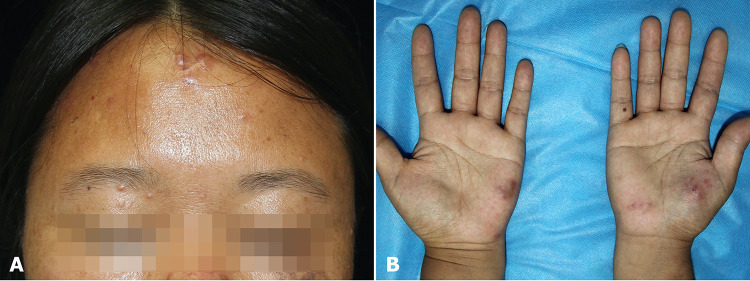
An otherwise healthy 38-year-old female presented with multiple erythematous nodules and papules for 4 months (Figure 1A and B) and was admitted to our hospital. Initially, the lesions occurred on her forehead and gradually spread to the eyelids and hands within 1 month. In the first 2 months, the patient visited multiple medical institutions and was successively administered a series of drug treatments, including prednisolone 20 mg/day for 1 week, topical ofloxacin and polymyxin B for 2 weeks, and itraconazole 200 mg/day for 1 week. However, no improvement was observed. The lesions on the hands suppurated, healed, and recurred spontaneously. The patient reported no other symptoms, such as pain or itching, fever, arthralgia, fatigue, or previous injury. Cutaneous examination revealed grouped erythematous papules distributed on the eyelids and multiple separate dull red nodules with smooth surfaces on the sinciput area, bilateral palmar, and fingers. The nodules were firm, with slight tenderness. The elevated erythrocyte sedimentation rate (28–36 mm/h) persisted. Other laboratory examinations, including autoantibody, complement, immunoglobulins, and HIV test demonstrated no significant findings, as did chest computed tomography.
Figure 1.
(A) Grouped erythematous papules on the eyelids and dull red nodules on the sinciput area. (B) Dull red nodules on bilateral palmar.
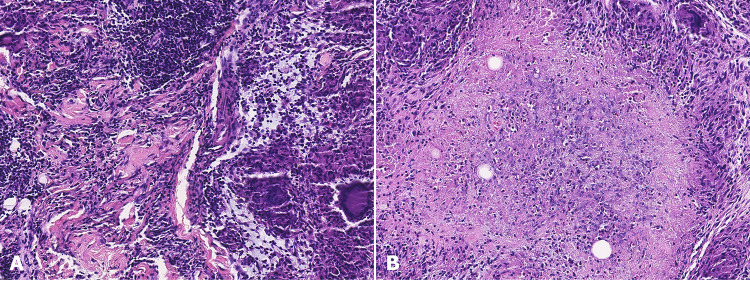
A skin biopsy was performed 4 months after onset (Figure 2A and B). The sinciput area sections revealed infiltration of large numbers of lymphocytes, neutrophils, histiocytes, and multinucleated giant cells within the dermis (Figure 2A). Granulomatous inflammation with central caseating necrosis was observed on palmar biopsy (Figure 2B). Punch biopsies were performed on the sinciput area and buccal area for mycobacterial and fungal cultures, and PCR assays. The culture results were negative. Mycobacteria-specific nuclear DNA was detected with rpoB primers in both specimens, and with hsp65 primers in lesions on the buccal area. This sequence showed the highest identity with Mycobacterium tuberculosis (> 99%). The IGRA test results were positive (Panel A/B - Nil= 20/23; >6 positive). The final diagnosis of cutaneous tuberculosis was made on the basis of skin manifestations, granulomatous inflammation with caseating necrosis on biopsy, positive PCR amplification results for Mycobacterium tuberculosis, and positive IGRA test results.
Figure 2.
Biopsies from the left buccal area (A) and the right palmar (B): infiltration of lymphocytes with neutrophils, histiocyte, multinucleated and giant cells, forming the granulomatous inflammation (A and B) with central caseating necrosis in the dermis (B).
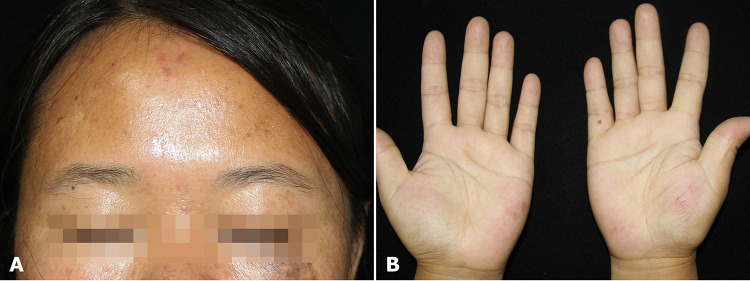
The patient was prescribed a combination of isoniazid, rifampin, and ethambutol for 4 months, followed by isoniazid and rifampin for 2 months. The lesions fully recovered after 5-months of treatment (Figure 3A and B). A good response to anti-tuberculosis therapy also supports this diagnosis.
Figure 3.
Lesions on the sinciput area (A) and palmar (B) improved after 5 months of anti-tuberculosis treatment.
Discussion
Tuberculosis is the leading cause of death from a single infectious agent, with globally more than 10 million infections occurring every year and estimated 1.30 million deaths in 2022.1 Cutaneous tuberculosis is a rare form of infection comprising 1–1.5% of extrapulmonary cases.3 The infection spreads via different routes in individuals with different immune statuses and has multiple clinical classifications, including plaques, papules, nodules, abscesses, erosions, and ulcers, mimicking diverse skin diseases.4 There are four major forms that account for most of cutaneous tuberculosis, including lupus vulgaris, tuberculosis verrucosa cutis, orificial tuberculosis, scrofuloderma. Those patients usually present with various slowly progressive skin lesions with no pulmonary infection symptoms or history, making diagnosis difficult. Moreover, lesion recurrence may lead to tissue destruction or carcinoma in the long-term.5 The diagnosis of cutaneous tuberculosis depends on laboratory confirmation of the pathogen. In most cases, a low mycobacterial load on the skin biopsy leads to a negative AFB smear test.6 A previous treatment history may strongly influence bacterial culture results. Currently, PCR amplification is the most rapid and sensitive method for the detection of Mycobacterium tuberculosis DNA. The IGRA test is also helpful for the clinical diagnosis of cutaneous tuberculosis.
Based on clinical and histological manifestations, we believe that this case should be classified as lupus vulgaris.7 Lupus vulgaris is a major type of cutaneous infection caused by the hematogenous spread of endogenous agents in patients with robust antituberculosis immunity. It typically presents as a red–brown plaque composed of papulonodules on the face with an “apple-jelly” color on the diascopy and with a tendency to fuse, ulcerate, and scar.3 A representative pathological feature is a tuberculoid granuloma with central caseation necrosis in the upper dermis. Disseminated multiple erythematous papules and nodules is a rare form of lupus vulgaris that should be differentiated from a series of facial disorders that share overlapping clinical and histological features, including lupus miliaris disseminatus faciei, rosacea, and perioral dermatitis.8–10 These diseases have similar clinical manifestations, and histologically show granulomatous infiltration in different patterns. Evidence of etiological agents could discriminate them from cutaneous tuberculosis.
The estimated global prevalence of multidrug-resistant tuberculosis is 11.6%; however, Mycobacterium tuberculosis isolates from skin infections have a low rate of mono-drug-resistant mutations.11,12 We suggest that the lower drug resistance rate may be due to long-term infection, limited chance of transmission and the reduced use of antibiotics for this disease. Since a 6-month course of combined antibiotics is generally effective in treating cutaneous tuberculosis, the drug sensitivity test is considered unnecessary before empirical therapy.13
The clinical diagnosis of cutaneous tuberculosis can be challenging because of its diverse clinical phenotypes. The present case highlights the importance of etiological examination for refractory facial granulomatous dermatoses. The limitation of this study is a lack of positive culture result, which is the golden diagnostic standard for cutaneous tuberculosis. As mycobacterial culture requires a long time and can be influenced by prior antibiotic history, the detection of Mycobacterium tuberculosis-derived DNA could be essential for accurate diagnosis.
Acknowledgments
We are grateful for the grants from the National Natural Science Foundation of China (Grant 81972950, 82173431, 82103748, 82203940), Jiangsu Provincial Medical Key Laboratory, Jiangsu Province Capability Improvement Project through Science, Technology and Education (ZDXYS202204).
Ethics and Consent
The waiver of ethic review in publications of photograph and medical records in single-case report is comply with the Declaration of Helsinki and was approved by the Medical Ethics Committee, Chinese Academy of Medical Sciences Hospital (Institute) of Dermatology. According to patient data confidentiality principle, the patient’s written informed consent was obtained for publications of all the images and case details.
Disclosure
All authors agree with the submission and declare that they have no conflict of interest.
References
- 1.World Health Organization. Global Tuberculosis Report 2023. Geneva: World Health Organization; 2023. [Google Scholar]
- 2.Peto HM, Pratt RH, Harrington TA, LoBue PA, Armstrong LR. Epidemiology of extrapulmonary tuberculosis in the United States, 1993-2006. Clin Infect Dis. 2009;49(9):1350–1357. doi: 10.1086/605559 [DOI] [PubMed] [Google Scholar]
- 3.Brito AC, Oliveira CMM, Unger DA, Bittencourt MJS. Cutaneous tuberculosis: epidemiological, clinical, diagnostic and therapeutic update. An Bras Dermatol. 2022;97(2):129–144. doi: 10.1016/j.abd.2021.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen Q, Chen W, Hao F. Cutaneous tuberculosis: a great imitator. Clin Dermatol. 2019;37(3):192–199. doi: 10.1016/j.clindermatol.2019.01.008 [DOI] [PubMed] [Google Scholar]
- 5.Yates VM. Mycobacterial infection. In: Burns T, Breathnach S, Cox N, editors. Rook’s Textbook of Dermatology, 8th. Oxford: Blackwell Science Ltd; 2010:16–19. [Google Scholar]
- 6.Kathuria P, Agarwal K, Koranne RV. The role of fine-needle aspiration cytology and Ziehl Neelsen staining in the diagnosis of cutaneous tuberculosis. Diagn Cytopathol. 2006;34(12):826–829. doi: 10.1002/dc.20534 [DOI] [PubMed] [Google Scholar]
- 7.Wang H, Wu Q, Lin L, Cui P. Cutaneous tuberculosis: a diagnostic and therapeutic study of 20 cases. J DermatolTreat. 2011;22(6):310–314. doi: 10.3109/09546634.2010.487889 [DOI] [PubMed] [Google Scholar]
- 8.Hruza GJ, Posnick RB, Weltman RE. Disseminated lupus vulgaris presenting as granulomatous folliculitis. Int J Dermatol. 1989;28(6):388–392. doi: 10.1111/j.1365-4362.1989.tb02486.x [DOI] [PubMed] [Google Scholar]
- 9.Kaushik A, Kumaran MS, Chatterjee D, De D. The search for a uniformly effective treatment in patients with lupus miliaris disseminatus faciei. JAMA Dermatol. 2020;156(10):841–842. doi: 10.1001/jamadermatol.2020.1069 [DOI] [PubMed] [Google Scholar]
- 10.Wilkin J, Dahl M, Detmar M, et al. Standard classification of rosacea: report of the national rosacea society expert committee on the classification and staging of rosacea. J Am Acad Dermatol. 2002;46(4):584–587. [DOI] [PubMed] [Google Scholar]
- 11.Salari N, Kanjoori AH, Hosseinian-Far A, Hasheminezhad R, Mansouri K, Mohammadi M. Global prevalence of drug-resistant tuberculosis: a systematic review and meta-analysis. Infect Dis Poverty. 2023;12(1):57. doi: 10.1186/s40249-023-01107-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mei YM, Zhang WY, Sun JY, et al. Genomic characteristics of Mycobacterium tuberculosis isolates of cutaneous tuberculosis. Front Microbiol. 2023;14:1165916. doi: 10.3389/fmicb.2023.1165916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Singal A, Kaur I, Jakhar D, et al. Clinicoepidemiological characteristics of cutaneous tuberculosis in 1458 Indian patients: a retrospective analytical study from a tertiary care center. Int J Dermatol. 2022;61(8):1012⁃1022. doi: 10.1111/ijd.16267 [DOI] [PubMed] [Google Scholar]