Abstract
Objective
Distraction osteogenesis is a primary treatment for severe mandibular hypoplasia. Achieving the ideal mandible movement direction through precise distraction vector control is still a challenge in this surgery. Therefore, the aim of this study was to apply Optical See-Through (OST) Augmented Reality (AR) technology for intraoperative navigation during mandibular distractor installation and analyze the feasibility to evaluate the effectiveness of AR in a phantom experiment.
Methods
Phantom was made of 3D-printed mandibular models based on preoperative CT scans and dental arch scans of real patients. Ten sets of 3D-printed mandible models were included in this study, with each set consisting of two identical mandible models assigned to the AR group and free-hand group. 10 sets of mandibular distraction osteogenesis surgical plans were designed using software, and the same set of plans was shared between the AR and free-hand groups. Surgeons performed bilateral mandibular distraction osteogenesis tasks under the guidance of AR navigation, or the reference of the preoperative surgical plan displayed on the computer screen. The differences in angular errors of distraction vectors and the distance errors of distractor positions under the guidance of the two methods were analyzed and compared.
Results
40 distractors were implanted in both groups, with 20 cases in each. In intra-group comparisons between the left and right sides, the AR group exhibited a three-dimensional spatial angle error of 1.88 (0.59, 2.48) on the left and 2.71 (1.33, 3.55) on the right, with P = 0.085, indicating no significant bias in guiding surgery on both sides of the mandible. In comparisons between the AR group and the traditional free-hand (FH) group, the average angle error was 1.94 (1.30, 2.93) in the AR group and 5.06 (3.61, 9.22) in the free-hand group, with P < 0.0001, resulting in a 61.6% improvement in accuracy. The average displacement error was 1.53 ± 0.54 mm in the AR group and 3.56 ± 1.89 mm in the free-hand group, with P < 0.0001, indicating a 57% improvement in accuracy.
Conclusion
Augmented Reality technology for intraoperative navigation in mandibular distraction osteogenesis is accurate and feasible. A large randomized controlled trial with long-term follow-up is needed to confirm these findings.
Trial Registration
The project has been registered with the Chinese Clinical Trial Registry, with registration number ChiCTR2300068417. Date of Registration: 17 February 2023.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12903-024-05105-9.
Keywords: Augmented reality, Mixed reality, Distraction osteogenesis, Surgical navigation
Introduction
The innovation of mandibular distraction osteogenesis (MDO) has revolutionary significance for patients with severe mandibular hypoplasia, hemifacial hypoplasia, and some syndromic disorders. McCarthy conducted the first MDO in 1992 [1, 2], . After decades of development, MDO has become the primary method for treating such conditions [3].
However, the stability and accuracy of MDO surgeries have been a subject of ongoing debate. Due to distraction osteogenesis being a continuous process, the results of distraction may not always align with the intended outcomes for various reasons. This could potentially lead to: ①Anterior or posterior open bite, malocclusion. ②Mandibular rotation, resulting in deviation or asymmetry [4].
Because the mandible moves for a long time, it is better to use internal distractors for installation. Hence, the precision of MDO surgery can be enhanced by focusing on vector control and carefully selecting the place for distractor installation [5–7]. Due to the widespread use of digital technology, virtual surgical planning(VSP) has become a standard preoperative preparation process. The vector of distraction is also determined during the simulated surgery. The traditional process for distraction osteogenesis involves three main stages. First, computer-assisted design is used to plan the surgery. Second, the distractors are pre-bent to fit the bone surface based on the surgical plan and applied to 3D-printed skull models. Finally, the pre-bent distractors are implanted into the surgical area during the actual procedure [8]. In each of these stages, the virtual surgical plan undergoes two transfers, and errors may occur at each step. These errors are challenging to detect or estimate and may accumulate over the process. Therefore, the challenge lies in how to transfer the designed distraction vector into the actual surgical procedure.
To enhance the transfer of distraction vectors from VSP to the actual surgical procedure, the current mainstream approach involves the use of CAD/CAM (Computer-Aided Design/Computer-Aided Manufacturing) templates to assist in the positioning of distractors [9]. While most studies have reported positive outcomes with this method, CAD/CAM templates still have some limitations, including: ①The preoperative design process can be time-consuming and labor-intensive, requiring multiple preoperative preparations. ②The limited space within the mandibular surgical field can make distractor placement challenging. Inserting guide plate and other instruments deeply into this confined area can lead to excessive soft tissue dissection and, in some cases, necessitate extraoral incisions. ③Distractors may not adequately adapt to irregular bone surfaces, potentially causing deformation and altering their distraction vectors after fixation [10, 11]. Some researchers have proposed the use of surgical navigation to guide the implantation of distractors for controlling distraction vectors [12]. However, traditional navigation devices in surgery have substantial drawbacks. To enhance tracking accuracy, they often require extraoral incisions, resulting in additional open scars. Moreover, traditional navigation systems have long suffered from significant hand-eye coordination issues. Surgeons frequently need excellent visual-spatial skills, memory, and extensive experience in surgical navigation to operate effectively. Some researchers have also experimented with using robots to help place distractors in animal models. However, this research is still in its preliminary stages and requires further development and validation.
Utilizing augmented reality (AR) navigation technology may be an innovative approach to address these issues. AR is a technology that combines computer-generated virtual information with the real world to provide an enhanced visual and perceptual experience. During surgery, if we can use optical see-through (OST) head-mounted display devices (HMD) to project the preoperative virtual surgical plan directly onto the surgical area through holographic projection [13]. Surgeons obtain guidance on surgical targets from a first-person perspective, facilitating three-dimensional vector control and placement of distractors. This provides the most direct intraoperative guidance. Currently, in fields such as spinal surgery and neurosurgery, there are already precedents for using AR navigation for intraoperative guidance. Notably, Augmedics has developed an AR-guided spinal screw placement system that has received FDA (Food and Drug Administration of America) approval [14].
Therefore, this study will explore a surgical navigation approach utilizing OST-AR to guide distraction vectors in MDO surgery. The efficacy of this method will be compared with that of traditional MDO surgery. This study is a research experiment conducted using a phantom.
Materials and methods
Research subjects
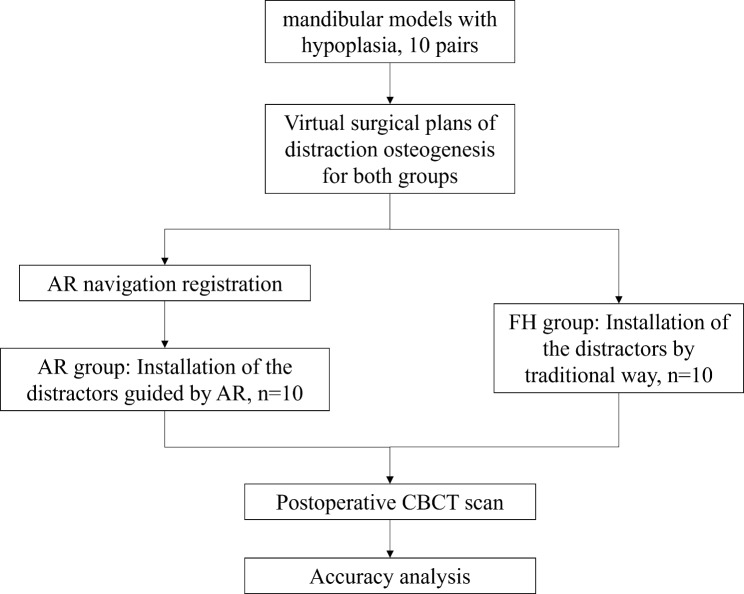
This manuscript complies with the Consolidated Standards of Reporting Trials (CONSORT) guidelines. A CONSORT checklist has been completed and is attached as an additional file to provide detailed information on the trial’s design, analysis, and interpretation. This paper is a randomized trial. In this section, the research subjects consist of 3D-printed mandibular models based on preoperative CT scans and dental arch scans of real patients. The positioning and fixation tasks of the distractors in the study are all based on these models. Inclusion criteria are as follows: (1) Bilateral mandibular hypoplasia; (2) Intact mandibular anatomical structure; (3) Patients aged over 18 years. Exclusion criteria included: (1) Refusal to participate in the study; (2) Patients with abnormal mandibular morphology due to conditions such as tumors, unsuitable for distractor fixation. In the pilot phase of our experiment, we aimed to establish the minimum sample size required to achieve a 90% statistical power at a 5% significance level for detecting differences between two methods, augmented reality and free-hand. The sample size was determined through a power analysis using the independent samples t-test. This analysis was conducted using the TTestIndPower tool from the Statsmodels library, which calculated that approximately 10 samples per group are necessary to ensure robust and statistically significant results. A total of 10 patients were included in this study, comprising 6 males and 4 females, with an average age of 23.6 years, ranging from 18 to 39 years. Among them, 4 patients presented with mandibular body hypoplasia, 3 with mandibular ramus hypoplasia, and 3 with total mandibular hypoplasia. Then we using Proplan CMF 3.0, real CT and dental scan data of 10 patients were computationally matched to generate mandibular Stereolithography (STL) models with high-precision dental data. These models were then imported into a high-precision 3D printing resin printer for mandibular model printing. 20 mandibles, comprising 10 pairs, were printed. These 3D-printed models, scaled at a 1:1 ratio, accurately replicated the patients’ mandibular anatomical structure and morphology, with the dental portion precision suitable for bite plate placement. Thus, we established a total of 20 phantom samples comprising 10 pairs of mandibular hypoplasia deformities as the subjects for this experiment.The overall workflow is illustrated in Fig. 1. This part of the research adheres to the relevant regulations concerning human research as outlined in the “Helsinki Declaration” and has been approved by the Medical Ethics Committee of Guangxi Medical University Affiliated.
Fig. 1.
Overall workflow diagram
Stomatological Hospital, with ethics number 2,023,005. The project has been registered with the Chinese Clinical Trial Registry, with registration number ChiCTR2300068417 at 2023-02-17.
Equipment and software requirements
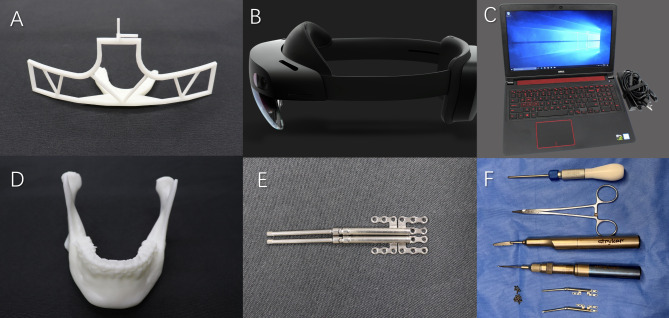
The study utilized a range of equipment and software, including the Microsoft HoloLens 2 Developer Edition from Microsoft (USA), an Augmented Reality Medical Imaging System V1.2.6 from Ziweidixing Digital Technology Co., Ltd. (China) is used for ntraoperative navigation. Proplan CMF 3.0 is used for preoperative virtual surgical planning. 3-Matic 13.0 is used for model editing and postoperative measurements. Mimics 21.0 is used for importing CT data, all from Materialize (Belgium). Stryker equipment, including the TPS power unit and MD Series Micro-Drill, was employed, sourced from Stryker Corporation (USA). The study also used the NewTom VGI High-Definition Large-Field CBCT machine provided by QR-S.R.L. (Italy) and 3Shape TRIOS A/S oral scanner (Tæven Intraoral Scanning Equipment Ltd., Denmark); Cibei Titanium Mandibular Distractors (model numbers X0101L-20 and X0101R-20) from Cibei Medical Equipment Co., Ltd. (China). Additionally, 3DS Max 2021 software from Autodesk (USA) and a Dell Inspiron 15-1577 laptop computer from Dell Inc. (USA) were included in the research equipment and software inventory (Fig. 2).
Fig. 2.
The main equipment and materials needed for the experiment (A. dental arch-based registration device, B. Microsoft HoloLens 2, C. Dell laptop D. phantom mandible., E. Distractor, F. Surgical tool)
Preoperative planning preparation
In Proplan CMF3.0, point-to-point and global registration were performed to merge the mandibular bone data obtained from CBCT scans with dental arch scan data, resulting in high-definition dental and mandibular STL models. These STL models served as the mandibular models used in this study. In Proplan CMF, a bite plate based on the high-definition dental arch was created. The generated STL model was then imported into 3DSMax 2021 software, where a “T-shaped frame,” as shown in the diagram below, was designed. This frame was combined with the bite plate model, thus completing the three-dimensional model design for the dental arch-based registration device.
Dental arch-based registration device three-dimensional model, and the digital three-dimensional model of the distractor used in this study (provided by Cibei Medical Equipment Co., Ltd.) were imported into 3-Matic 13.0 software. Using a combination of rotation and translation, the distractor three-dimensional model was positioned in either the mandibular ramus or the body’s bone surface, with the reference to clinical real cases to design the specific fixation location and direction of distraction, ensuring bilateral distraction vectors remain parallel in the sagittal plane. Mild overlap between the distractor’s fixation arm and the mandibular model was permitted. Following the adjustment of bilateral distractor positions as described above, the preoperative planning for distraction vectors in this part of the study was completed.
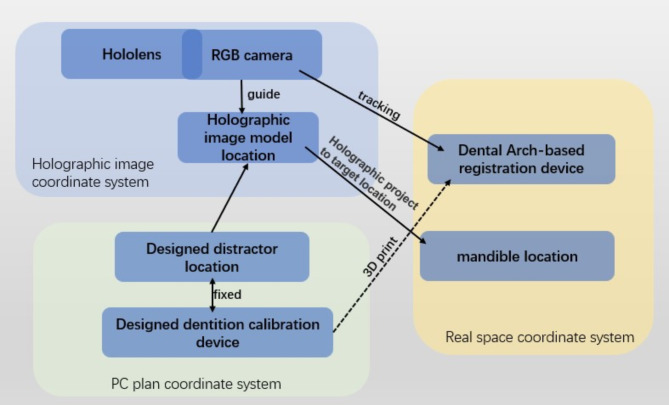
Dental arch-based augmented reality holographic projection registration device and holographic image production
We used the Vuforia software development kit, which can utilize the contour feature points of targets combined with the Hololens2 built-in inertial measurement unit to accurately identify and track the spatial position of the target model and perform precise image projection. To facilitate the positioning of mandible, we designed this registration device based on the dental arch. Its main structure consists of an occlusal splint and an inverted T-shape frame. The occlusal splint allows the device to accurately fit into the lower dental arch. With the use of appropriate temporary bonding materials, the registration device and the mandible become a rigidly fixed structure. The inverted T-shaped frame serves two functions: firstly, it can be recognized by the binocular RGB camera of the HoloLens using contour recognition technology to locate its three-dimensional spatial position, thereby enabling accurate projection of holographic image guidance information in three-dimensional space. Secondly, we have designed an observation module at the top of the frame with parallel xyz axes, allowing us to observe during surgery whether the holographic image overlaps with it, thereby assessing the accuracy of the current holographic image projection. The positioning method of this registration device is similar to that of the real surgical occlusal splint, thus it can realistically simulate the wearing situation during actual surgery.
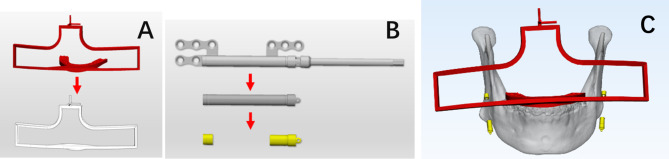
When using augmented reality glasses to view the world, one may encounter challenges with perceiving depth and experiencing cognitive interference when interacting with holographic displays. Instead of using the conventional method of projecting images throughout the whole observation and operation area, we utilize a simpler image model strategy. The team trims the digital model of the distractor to retain only the front and rear segments of the sleeve, minimizing information interference in the surgical area and ensuring the effectiveness of navigational information. The resulting in-surgery projected images are as shown in the figure (Fig. 3) and video (Link). The flow chart of the system is shown in the figure (Fig. 4).
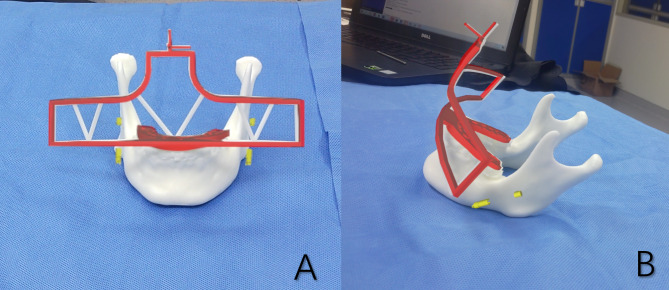
Fig. 3.
(A) dental arch-based registration device and its contour. (B) simplified image model strategy of the distractor. (C) holographic Image illustration: registration device (red) and simplified distractor (yellow), mandible is invisible
Fig. 4.
The flow chart of AR-based MDO navigation system
Surgical tasks
All surgical tasks were performed by one orthognathic surgeon from our hospital. The study used a paired design with two sets of surgical tasks, each consisting of 10 surgical tasks. The same surgical plan was used for both the experimental group and the control group. The experimental group, consisting of 10 cases, was guided by AR navigation for distractor installation (n = 10). The control group, on the other hand, was the free-hand group, and the installation of the distractors was guided by the surgical plan on a computer and the surgeon’s experience. Distractors were installed bilaterally in both groups (Figs. 5 and 6).
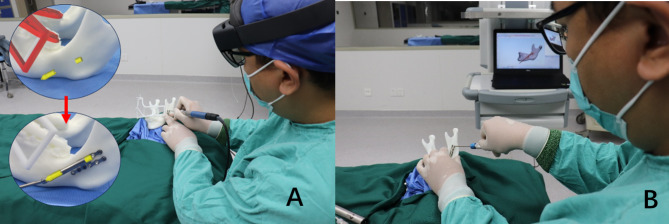
Fig. 5.
Actual image projection captured by HoloLens 2 (A. front view B. lateral view)
Fig. 6.
Surgery task of (A) AR group and (B) free-hand group
The surgical sequence for the subjects in the same group was conducted randomly. To prevent potential bias in the study results due to the surgeon’s memory of distractor placement, the surgeon initially completed all the surgical tasks for the AR group. After an interval of 15 days (about 2 weeks), the surgeon began performing the tasks for the free-hand group.
During the surgical procedures in the AR group, the surgeon positioned the dental arch-based registration device on the mandibular dental arch to ensure its correct placement. After confirming the accurate placement, the surgeon donned the Microsoft HoloLens 2 and operated it through “air tapping” and voice commands. The first step involved aligning the holographic images. After achieving precise overlap through automatic registration based on the three-dimensional contour of the registration device, combined with coordinate fine-tuning, the sleeve was aligned with its holographic image following guidance from the holographic image of the distractor’s sleeve. Simultaneously, the fixation arm of the distractor was shaped. Once the sleeve and its holographic image were perfectly aligned, reaching the target position, and the fixation and opposing arms conformed entirely to the bone surface, titanium screws were used to temporarily secure the distractor. A CBCT scan was performed to record the actual postoperative distraction vector and distractor position.
The distinction between the surgical tasks performed by the free-hand group and the AR group is that in the free-hand group, the surgeon determined the distraction vectors and fixed positions of the distractor during the surgery by observing a computer screen and referring to the three-dimensional models of the mandible and distractor from the virtual surgical plan. The other jobs in the workflow were identical to those in the AR group. After reconstructing three-dimensional models from the captured CBCT DICOM data using Proplan 3.0, they were imported into 3-Matic 13.0 alongside the preoperative planned three-dimensional models. The reconstruction threshold for the three-dimensional models was kept consistent with the preoperative settings. Using the point-to-point registration and global registration functions in the 3-matic13.0, the mandibular portion of the preoperative plan was precisely aligned with the corresponding segment in the postoperative 3D model. This process allowed for the spatial matching of the preoperative and postoperative mandibles in the coordinate system, with the positional differences of the distractor before and after surgery representing the surgical deviations from the preoperative design. A line that runs parallel to the distractor sleeve was drawn at the middle of the outer surface at both ends of the three-dimensional models of the planned distractor sleeve before surgery and the actual distractor sleeve after surgery. This line represented the distraction vector, with the midpoint of this line indicating the distractor’s position. The angle and distance differences between the lines in the preoperative planned and postoperative actual models respectively represented the angle error of the postoperative actual distraction vector and the position error of the distractor.
Statistical analysis
The data were analyzed using SPSS software version 18.0 (SPSS Inc., Chicago, IL, USA). We used the Shapiro-Wilk test to verify the normality of data distribution for both groups. Normally distributed data, such as Distractor Position Translation Errors, were analyzed using an independent t-test. For non-normally distributed data, like Distraction Vector Errors, we employed the Mann-Whitney test. Statistical significance was determined at p < 0.05.
Results
Comparison of left and right side of distraction vector errors in both experimental and control groups
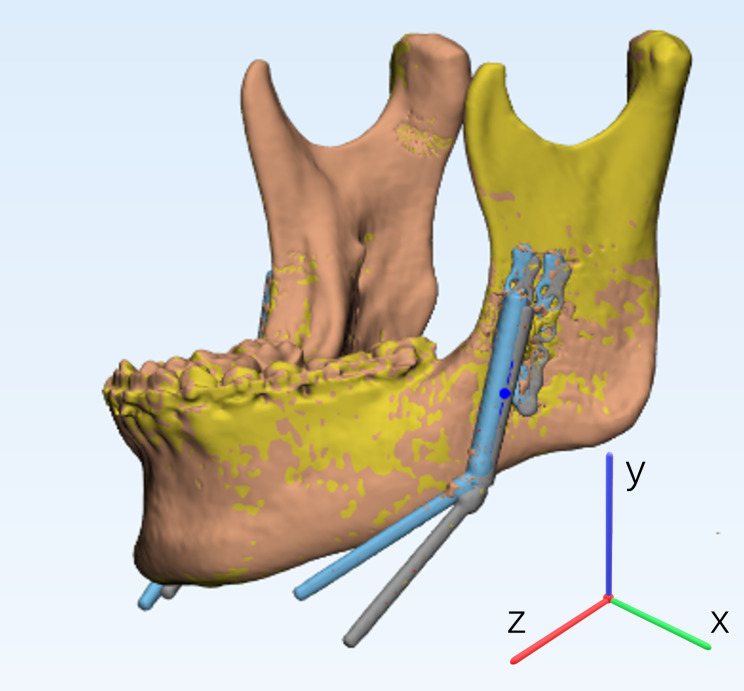
20 distractors were implanted in each group, with 10 placed on each side. The table displays the angle errors of distraction vectors for each side, as indicated in Tables 1 and 2. The registration of preoperative and postoperative models, along with the schematic of the coordinate axes, is shown in Fig. 7. The differences between the left and right sides were not statistically significant in three-dimensional space (P = 0.085), coronal plane (P = 0.436), horizontal plane (P = 0.529), and sagittal plane (P = 0.726). This suggests that the accuracy in determining distraction vectors on the left and right sides under augmented reality holographic image guidance did not exhibit significant differences.
Table 1.
The angle errors for distraction vectors in degrees for both sides in the AR group
| AR Group - Left | AR Group - Right | P Value | |
|---|---|---|---|
| Three-Dimensional Space (°) | 1.88 (0.59, 2.48) | 2.71 (1.33, 3.55) | 0.085 |
| Coronal Plane, xy (°) | 2.09 (0.49, 3.51) | 2.22 (0.95, 4.22) | 0.436 |
| Horizontal Plane, xz (°) | 1.00 (0.70, 2.66) | 2.23 (0.58, 6.04) | 0.529 |
| Sagittal Plane, yz (°) | 1.68 (0.42, 2.04) | 0.77 (0.42, 3.05) | 0.726 |
Note: Data are represented by the median (P25, P75)
Abbreviation: AR: Augmented Reality
Table 2.
Angle errors for the Free-Hand Group on both sides
| FH Group - Left | FH Group - Right | P Value | |
|---|---|---|---|
| Three-Dimensional Space (°) | 3.99 (3.58, 9.60) | 7.10 (3.33, 9.85) | 0.739 |
| Coronal Plane, xy (°) | 0.91 (0.56, 6.85) | 2.80 (1.56, 9.52) | 0.21 |
| Horizontal Plane, xz (°) | 4.51 (2.05, 10.35) | 4.73 (0.87, 10.17) | 0.684 |
| Sagittal Plane, yz (°) | 3.77 (1.83, 9.73) | 5.75 (2.53, 9.49) | 0.853 |
Note: Data are represented by the median (P25, P75)
Abbreviation: FH: Free Hand
Fig. 7.
Registration of preoperative and postoperative models & Coordinate axis diagram of the mandible
Comparison of distraction vector errors between the AR group and free-hand group
As shown in Table 3, the data indicates significant differences compared AR group with FH group in three-dimensional space, angle errors in the horizontal and sagittal planes. However, there were no significant differences in errors in the coronal plane.
Table 3.
The angle errors in various dimensions between the AR group and FH group
| AR Group | FH Group | P Value | Accuracy promotion | |
|---|---|---|---|---|
| Three-Dimensional Space (°) | 1.94 (1.30, 2.93) | 5.06 (3.61, 9.22) | < 0.0001**** | 61.6% |
| Coronal Plane, xy (°) | 2.22 (0.73, 3.79) | 1.89 (0.64, 7.12) | 0.784 | - |
| Horizontal Plane, xz (°) | 1.48 (0.69, 3.76) | 4.51 (2.04, 9.44) | 0.0095** | 67.2% |
| Sagittal Plane, yz (°) | 1.24 (0.44, 2.72) | 3.87 (2.37, 9.17) | 0.0005*** | 68.0% |
Note: Data are represented by the median (P25, P75).
Abbreviation: AR: Augmented Reality; FH: Free Hand
Comparison of preoperative planned and postoperative actual distractor position translation errors in the AR group and free-hand group
The translational errors between preoperative planned and postoperative actual distractor positions for the AR group and free-hand group are presented below (Table 4). Both sets of data followed a normal distribution, and statistical analysis was performed using Student’s t-test. In the AR group, the distance error between preoperative planned and postoperative actual distractor positions was significantly smaller in terms of Euclidean distance (P < 0.001), horizontal direction (P = 0.004), and vertical direction (P < 0.001) when compared to the free-hand group. However, there was no significant difference between the two groups in the anterior-posterior direction (P = 0.121).
Table 4.
Preoperative Planned and Postoperative Actual Distractor Position Translation Errors
| AR Group | FH Group | P Value | Accuracy promotion | |
|---|---|---|---|---|
| Euclidean Distance (mm) | 1.53 ± 0.54 | 3.56 ± 1.89 | < 0.0001**** | 57% |
| Horizontal (mm) | 0.39 ± 0.26 | 0.75 ± 0.43 | 0.003** | 48% |
| Vertical (mm) | 0.99 ± 0.56 | 2.95 ± 1.81 | < 0.0001**** | 66.4% |
| Anterior-Posterior (mm) | 0.91 ± 0.57 | 1.43 ± 1.33 | 0.117 | - |
Note: Data is presented as `X ± SD.
Abbreviation: AR: Augmented Reality; FH: Free Hand; mm: millimeter
Discussion
Although VSP technology has been widely used, the precision of distraction osteogenesis procedures for the mandible has not yet reached the level of orthognathic surgery, limiting the use and development of this technique { [15] #61} { [16] #98} {Wang, 2019 #38}. According to the definition by Cleary and Peters of surgical guidance or image-guided surgery: surgeons use computer-based virtual images, preoperative or intraoperative, overlaid for visualization and targeting patient anatomy during medical procedures { [17], #44}. Undoubtedly, augmented reality navigation fits this concept most aptly. Utilizing HMD-AR technology, the surgical plan is directly displayed in the surgeon’s field of view, facilitating the guidance of the surgical process and even allowing for real-time verification of surgical accuracy { [18] #67}. Gibby utilized augmented reality technology to assist in spinal screw implantation, and they achieved implantation angles and distances that were non-inferior to those in the conventional control group [19]. However, they find significant advantages in terms of surgery time and the elimination of the need for additional X-ray imaging during surgery. In the earlier phase of our research team’s work, we use HoloLens 2 for positioning of maxillary distractors, we achieved improved control of distraction vectors [20]. Nevertheless, in contrast to our prior research, the current study encompasses not only the control of distraction vectors but also the bone-surface fit between the distractor’s fixed arm and the resisting arm. Importantly, this study is the first to use AR technology as a bridge between VSP and the surgical process, directly guiding the distraction osteogenesis procedure at surgeon’s field of view.
From the results of this experiment, it is evident that the AR group achieved better control over the distraction vectors, especially in the sagittal and horizontal planes. Moreover, the level of control over the position of the distractor was higher compared to the conventional approach of doing it by hand. This has profound ramifications for enhancing the precision of MDO. In bilateral mandibular distraction, the sagittal plane control of both distractors is crucial, as it determines the overall anterior movement of the mandible. If there is an overall counterclockwise rotation, it results in posterior tooth separation, while a clockwise rotation leads to anterior tooth separation. Furthermore, if the distraction directions on both sides are not parallel, the mandible’s proximal segment undergoes coronal plane rotation, resulting in occlusal plane rotation. Poor control of the horizontal plane distraction vectors can also lead to changes in the horizontal direction of both mandibles, causing mandibular tilting. In this study, the angle error in three-dimensional space was 1.94° (1.30, 2.93), and the position error was 1.53 ± 0.54 mm. Compared to other scholars’ data, Cai et al. used optical navigation in their sheep mandibular distraction osteogenesis experiment, achieving an average error of 2.56° [21]. Li and others employed surgical guides for mandibular distraction osteogenesis, with a root mean square deviation (RMSD) of 0.93 mm for surgical errors, and RMSDs of angular errors across three axes being 4.64°, 2.03°, and 2.88°, respectively [10]. The results of this experiment are undoubtedly very encouraging. If such results can be replicated in clinical settings, the precision and efficiency of surgery provided by AR navigation could significantly enhance the accuracy of distraction osteogenesis, thus achieving more precise postoperative distraction outcomes and improving surgical results.
Another noteworthy topic for consideration is the process of registering and monitoring holographic pictures. Currently, a few studies use planar QR codes for holographic image registration and target tracking [22–25]. In this study, we utilized a dental arch-based registration system. When the “bite plate” section of the registration system is accurately positioned on the mandibular dental arch, HoloLens uses its binocular RGB cameras to recognize the three-dimensional contour of the “inverted T” section and project the holographic image to the target location. This contour is designed to be arc-shaped for HoloLens 2 to recognize it from different angles. For the convenience of surgeons to check the accuracy of holographic image projection and make coordinate adjustments to the holographic image, we designed three mutually perpendicular cylindrical structures at the top of the inverted T contour. The manufacturing of this registration device is simple, and if needed for different patients, only the registration contour needs to be connected to different bite plates, providing greater flexibility for clinical use. Moreover, the positioning and surgical guidance accuracy of occlusal splints have been widely utilized in actual orthognathic surgeries. By employing this registration method, we can realistically simulate the installation and positioning of the device as it would be used in a real surgical setting.
This study differs from many applications of AR technology, as most research emphasizes the ability of AR technology to load more information in the surgical area. For example, it may emphasize loading information about bone density in the case of oral implant surgery or overlay complete brain models on the patient’s head [26–28]. While these pieces of information can enhance our understanding of the patient’s surgical area, in actual clinical use, an overload of virtual and real-world information in the field of view can easily cause cognitive interference with real-world objects [29]. This can affect our depth perception of objects, which is a significant concern during human surgeries as it can increase visual fatigue among surgeons and even lead to surgical errors. In oral and maxillofacial surgery, this problem becomes even more pronounced. Manuel Birlo suggested that in human-computer interaction using HMD-AR, efforts should focus on achieving low-perception task modes and reducing the use of modes that stack effective tasks [30]. This study follows a more reasonable concept of human-computer interaction in the use of AR technology. We have made efforts to simplify the information displayed in the field of view through the AR device and, for guidance on the target location, employed a simplified structure for the distraction device. This design does not interfere with the observation of the actual distraction device, while also providing motion parallax through multiple angles for better depth perception in virtual projections. This approach ensures the seamless integration of virtual and real-world information, reduces visual interference caused by holographic projections, and enhances the usability of the navigation system. This aspect has been less emphasized in previous related studies.
This study employed a systematic registration approach, performing global registration of preoperative and postoperative models. By using computational algorithms to process the models, the method replaces manual point marking and line drawing for measurements [31, 32]. In both orthognathic surgery and distraction osteogenesis, this model registration technique for postoperative analysis is increasingly favored by surgeons. It enhances the efficiency of postoperative evaluation and reduces the potential for human error in the process.
However, this study has several limitations. First, the experiments were conducted on models, whereas achieving such optimal visibility is not feasible in actual clinical surgeries. Additionally, the study did not account for the impact of the temporomandibular joint on the actual distraction vectors. Moreover, during the experiments, we identified several issues under the current experimental conditions: (1) Display capabilities of the HoloLens 2 device: The ability of the HoloLens 2 to display images effectively in the brightly lit environment of an operating room presents a challenge. Furthermore, the depth perception issues associated with merging virtual and real images could complicate observation. (2) Soft tissue obstruction: Whether the surgery is performed intraorally or externally, the surgical area is often obscured by soft tissues. Navigating with AR during tissue retraction, especially when using multiple surgical hooks, significantly increases the complexity. (3) Constrained surgical space: Our registration device is relatively bulky, which can complicate surgeries in the spatially constrained environment typical of maxillofacial surgery. The team will continue with animal experiments and clinical trials based on real patients in the next phase of research.
Conclusion
Dental arch-based registration method and augmented reality technology demonstrates feasibility in intraoperative navigation for mandibular distraction osteogenesis. It offers high precision in installing the distractors and controlling distraction vectors, along with the convenience and intuitiveness of the navigation process. Advances in relevant software and hardware technologies are expected to enhance its clinical value.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
No applicable.
Author contributions
Shi-xi He and Cheng Ma designed the research plan, participated in the main experimental procedures, collected experimental data, and contributed to the writing and revision of the manuscript. Zong-Yi Yuan conducted the main experiments, analyzed the data, and contributed to the writing of the manuscript. Tian-feng Xu assisted in data collection and analysis, and participated in drafting the initial manuscript. Qing-tiao Xie assisted in experimental design and execution, and took part in data analysis. Ya-xi Wang provided the resources and tools necessary for data collection, and reviewed and edited the manuscript. Xuan-ping Huang guided the research direction, provided the research facilities, and advised on the manuscript writing.
Funding
1. Guangxi Science and Technology Base and Talents Special Project (2021AC18031). 2. National Natural Science Foundation of China under Grant (82360187). 3. Guangxi Medical and health suitable technology development and popularization applications project (S2021085). 4. Nanning Qingxiu District Science and Technology Plan (2021004).
Data availability
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request. The data are located at the Orthognathic Center of College & Hospital of Stomatology, Guangxi Medical University.
Declarations
Financial disclosure
The authors declare that there are no conflicts of interest in relation to the subject matter or materials discussed in this manuscript. No financial support was received for this study or preparation of this article.
Human ethics
This paper was approved by the Medical Ethics Committee of College & Hospital of Stomatology, Guangxi Medical University (number: 2023005), and we were in accordance with the 1975 Helsinki declaration and its later amendments.
Consent for publication
Not applicable.
Consent to participate
Informed consent was obtained from all individual participants included in the study. All participants were provided with detailed information about the study’s aims, procedures, potential risks, and benefits before their participation. Participants were informed that their participation was voluntary and that they could withdraw from the study at any time without penalty or loss of benefits to which they are otherwise entitled.
Author agreement
This manuscript is original and there is no conflict of interest to disclose. Neither the entire paper nor any part of its content has been accepted or published elsewhere. All authors have seen the manuscript and approved to submit to your journal.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.McCarthy JG, Schreiber J, Karp N, Thorne CH, Grayson BH. Lengthening the human mandible by gradual distraction. Plast Reconstr Surg, 1992;89(1):1–8; discussion 9–10. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/1727238 [PubMed]
- 2.McCarthy JG, Staffenberg DA, Wood RJ, Cutting CB, Grayson BH, Thorne CH. Introduction of an intraoral bone-lengthening device. Plast Reconstr Surg. 1995;96(4):978–81. 10.1097/00006534-199509001-00034. [DOI] [PubMed] [Google Scholar]
- 3.Rossini G, Vinci B, Rizzo R, Pinho TMD, Deregibus A. Mandibular distraction osteogenesis: a systematic review of stability and the effects on hard and soft tissues. Int J Oral Maxillofac Surg. 2016;45(11):1438–44. 10.1016/j.ijom.2016.08.012. [DOI] [PubMed] [Google Scholar]
- 4.Kim MJ, Seo J, Kim DK, Baek SH. Three-dimensional virtual-surgery simulation-assisted asymmetric bilateral mandibular distraction osteogenesis for a patient with bilateral condylar fractures. Am J Orthod Dentofac Orthop. 2017;151(1):186–200. 10.1016/j.ajodo.2015.11.033. [DOI] [PubMed] [Google Scholar]
- 5.Verlinden CR, van de Vijfeijken SE, Tuinzing DB, Becking AG, Swennen GR. Complications of mandibular distraction osteogenesis for acquired deformities: a systematic review of the literature. Int J Oral Maxillofac Surg. 2015;44(8):956–64. 10.1016/j.ijom.2014.12.008. [DOI] [PubMed] [Google Scholar]
- 6.Dec W, Peltomaki T, Warren SM, Garfinkle JS, Grayson BH, McCarthy JG. The importance of vector selection in preoperative planning of unilateral mandibular distraction. Plast Reconstr Surg. 2008;121(6):2084–92. 10.1097/PRS.0b013e31817081b6. [DOI] [PubMed] [Google Scholar]
- 7.Grayson BH, McCormick S, Santiago PE, McCarthy JG. Vector of device placement and trajectory of mandibular distraction. J Craniofac Surg. 1997;8(6):473–80. 10.1097/00001665-199711000-00009. discussion 481 – 472. [DOI] [PubMed] [Google Scholar]
- 8.Davidson EH, Brown D, Shetye PR, Greig AVH, Grayson BH, Warren SM, McCarthy JG. The evolution of mandibular distraction: device selection. Plast Reconstr Surg. 2010;126(6):2061–70. 10.1097/PRS.0b013e3181f526d9. [DOI] [PubMed] [Google Scholar]
- 9.Chen K, Xiao D, Abotaleb B, Chen H, Li Y, Zhu S. Accuracy of virtual Surgical Planning in Treatment of Temporomandibular Joint Ankylosis using distraction osteogenesis: comparison of Planned and actual results. J Oral Maxillofac Surg. 2018;76(11):e24222421–24222420. 10.1016/j.joms.2018.07.003. [DOI] [PubMed] [Google Scholar]
- 10.Li B, Sun H, Zeng F, Zhang T, Wang X. Accuracy of a CAD/CAM surgical template for mandibular distraction: a preliminary study. Br J Oral Maxillofac Surg. 2018;56(9):814–9. 10.1016/j.bjoms.2018.09.001. [DOI] [PubMed] [Google Scholar]
- 11.Tan A, Chai Y, Mooi W, Chen X, Xu H, Zin MA, Chai G. Computer-assisted surgery in therapeutic strategy distraction osteogenesis of hemifacial microsomia: Accuracy and predictability. J Craniomaxillofac Surg. 2019;47(2):204–18. 10.1016/j.jcms.2018.11.014. [DOI] [PubMed] [Google Scholar]
- 12.Badiali G, Cutolo F, Roncari A, Marchetti C, Bianchi A. Simulation-guided navigation for vector control in pediatric mandibular distraction osteogenesis. J Craniomaxillofac Surg. 2017;45(6):969–80. 10.1016/j.jcms.2017.02.006. [DOI] [PubMed] [Google Scholar]
- 13.Condino S, Carbone M, Piazza R, Ferrari M, Ferrari V. Perceptual limits of Optical see-through visors for Augmented reality Guidance of Manual tasks. IEEE Trans Biomed Eng. 2020;67(2):411–9. 10.1109/TBME.2019.2914517. [DOI] [PubMed] [Google Scholar]
- 14.Rush AJ 3rd, Shepard N, Nolte M, Siemionow K, Phillips F. Augmented reality in spine surgery: current state of the art. Int J Spine Surg. 2022;16(S2):S22–7. 10.14444/8273. [DOI] [PMC free article] [PubMed]
- 15.Vanesa V, Irene MP, Marta AS, Jose F, Miguel PF, Mireia BS, R. M., Josep RP. Accuracy of virtually planned mandibular distraction in a pediatric case series. J Craniomaxillofac Surg. 2021;49(2):154–65. 10.1016/j.jcms.2020.12.012. [DOI] [PubMed] [Google Scholar]
- 16.Hu KG, Aral A, Rancu A, Alperovich M. Computerized Surgical Planning for Mandibular Distraction Osteogenesis. Semin Plast Surg. 2024;38(3):234–41. 10.1055/s-0044-1786757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cleary K, Peters T,M. Image-guided interventions: Technology Review and clinical applications. Annu Rev Biomed Eng. 2010;12(1):119–42. [DOI] [PubMed] [Google Scholar]
- 18.Lex JR, Koucheki R, Toor J, Backstein DJ. Clinical applications of augmented reality in orthopaedic surgery: a comprehensive narrative review. Int Orthop. 2023;47(2):375–91. 10.1007/s00264-022-05507-w. [DOI] [PubMed] [Google Scholar]
- 19.Gibby J, Cvetko S, Javan R, Parr R, Gibby W. Use of augmented reality for image-guided spine procedures. Eur Spine J. 2020;29(8):1823–32. 10.1007/s00586-020-06495-4. [DOI] [PubMed] [Google Scholar]
- 20.Yuan Z, He S, Jiang T, Xie Q, Zhou N, Huang X. Augmented reality hologram combined with pre-bent distractor enhanced the accuracy of distraction vector transfer in maxillary distraction osteogenesis, a study based on 3D printed phantoms. Front Surg. 2022;9:1018030. 10.3389/fsurg.2022.1018030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cai M, Chen Y, Lu X, Xu L, Wang X, Shen G. Application of a newly designed mandibular distraction device for navigation surgery in goats. J Craniomaxillofac Surg. 2017;45(10):1704–9. 10.1016/j.jcms.2017.08.003. [DOI] [PubMed] [Google Scholar]
- 22.Shao L, Yang S, Fu T, Lin Y, Geng H, Ai D, Yang J. Augmented reality calibration using feature triangulation iteration-based registration for surgical navigation. Comput Biol Med. 2022;148:105826. 10.1016/j.compbiomed.2022.105826. [DOI] [PubMed] [Google Scholar]
- 23.Jun EK, Lim S, Seo J, Lee KH, Lee JH, Lee D, Koh JC. Augmented reality-assisted Navigation System for Transforaminal Epidural Injection. J Pain Res. 2023;16:921–31. 10.2147/JPR.S400955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Andrews CM, Henry AB, Soriano IM, Southworth MK, Silva JR. Registration techniques for clinical applications of three-dimensional augmented reality devices. IEEE J Transl Eng Health Med. 2021;9:4900214. 10.1109/JTEHM.2020.3045642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lin L, Gao Y, Aung ZM, Xu H, Wang B, Yang X, Xie L. Preliminary reports of augmented-reality assisted craniofacial bone fracture reduction. J Plast Reconstr Aesthet Surg. 2022;75(11):e1–8. 10.1016/j.bjps.2022.06.105. [DOI] [PubMed] [Google Scholar]
- 26.Liu L, Wang X, Guan M, Fan Y, Yang Z, Li D, Li H. A mixed reality-based navigation method for dental implant navigation method: a pilot study. Comput Biol Med. 2023;154:106568. 10.1016/j.compbiomed.2023.106568. [DOI] [PubMed] [Google Scholar]
- 27.Van Gestel F, Frantz T, Buyck F, Geens W, Neuville Q, Bruneau M, Duerinck J. Neuro-oncological augmented reality planning for intracranial tumor resection. Front Neurol. 2023;14:1104571. 10.3389/fneur.2023.1104571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Saito Y, Sugimoto M, Imura S, Morine Y, Ikemoto T, Iwahashi S, Shimada M. Intraoperative 3D Hologram support with mixed reality techniques in liver surgery. Ann Surg. 2020;271(1):e4–7. 10.1097/SLA.0000000000003552. [DOI] [PubMed] [Google Scholar]
- 29.Rojas-Munoz E, Cabrera ME, Lin C, Andersen D, Popescu V, Anderson K, Wachs JP. The system for telementoring with augmented reality (STAR): a head-mounted display to improve surgical coaching and confidence in remote areas. Surgery. 2020;167(4):724–31. 10.1016/j.surg.2019.11.008. [DOI] [PubMed] [Google Scholar]
- 30.Birlo M, Edwards PJE, Clarkson M, Stoyanov D. Utility of optical see-through head mounted displays in augmented reality-assisted surgery: a systematic review. Med Image Anal. 2022;77:102361. 10.1016/j.media.2022.102361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tondin GM, Leal M, Costa ST, Grillo R, Jodas CRP, Teixeira RG. Evaluation of the accuracy of virtual planning in bimaxillary orthognathic surgery: a systematic review. Br J Oral Maxillofac Surg. 2022;60(4):412–21. 10.1016/j.bjoms.2021.09.010. [DOI] [PubMed] [Google Scholar]
- 32.De Riu G, Virdis PI, Meloni SM, Lumbau A, Vaira LA. Accuracy of computer-assisted orthognathic surgery. J Craniomaxillofac Surg. 2018;46(2):293–8. 10.1016/j.jcms.2017.11.023. [DOI] [PubMed] [Google Scholar]
- 33.Haas OL Jr., Becker OE, de Oliveira RB. Computer-aided planning in orthognathic surgery-systematic review. Int J Oral Maxillofac Surg. 2014. 10.1016/j.ijom.2014.10.025. [DOI] [PubMed] [Google Scholar]
- 34.Kim BS, Zhang Z, Sun M, Han W, Chen X, Yan Y, Chai G. Feasibility of a Robot-assisted Surgical Navigation System for Mandibular Distraction Osteogenesis in Hemifacial Microsomia: a model experiment. J Craniofac Surg. 2023;34(2):525–31. 10.1097/SCS.0000000000009028. [DOI] [PubMed] [Google Scholar]
- 35.W D, Roberts W, Strohbehn J, Hatch FJ, Kettenberger. A frameless stereotaxic integration of computerized tomographic imaging and the operating microscope. Journal of neurosurgery; 1986. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request. The data are located at the Orthognathic Center of College & Hospital of Stomatology, Guangxi Medical University.