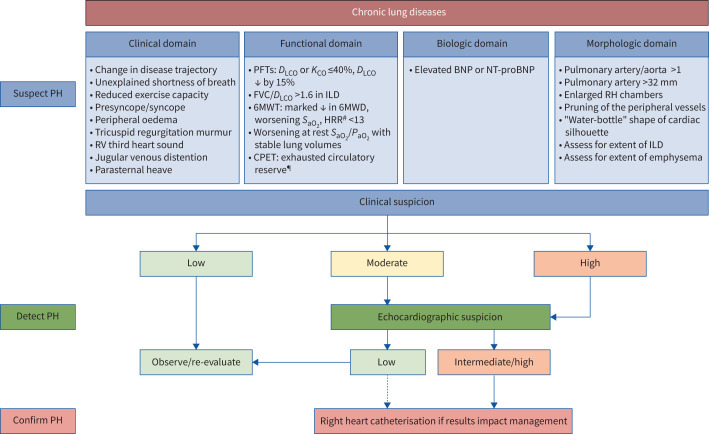
FIGURE 2.
Diagnostic algorithm for pulmonary hypertension (PH) in the setting of COPD and interstitial lung disease (ILD). The decision to perform a right heart catheterisation should be predicated by a clinical or research need that would impact management and/or provide prognostic information, such as considerations of disease phenotyping and therapeutic interventions, clinical trial enrolment, pre-operative clearance/assistance with perioperative management, evaluation for lung transplantation and, in COPD, assessment for lung volume reduction therapy. A multimodal assessment, including lung function, functional, radiographic and echocardiographic data is recommended to determine when to proceed with haemodynamic assessment. Given that in patients with chronic lung diseases the performance characteristics of transthoracic echocardiography are worse due to poor windows, altered location of the heart in the chest cavity and interference due to the lung tissue overlying the heart, in patients with moderate or high clinical suspicion for PH, right heart catheterisation can be considered irrespective of the transthoracic echocardiography findings (as indicated by the dotted line). RV: right ventricular; PFTs: pulmonary function tests; DLCO: diffusion capacity of the lung for carbon monoxide; KCO: carbon monoxide transfer coefficient; FVC: forced vital capacity; 6MWT: 6-min walk test; 6MWD: 6-min walk distance; SaO2: arterial haemoglobin oxygen saturation; HRR: heart rate recovery; PaO2: arterial partial pressure of oxygen; CPET: cardiopulmonary exercise testing; BNP: brain natriuretic peptide; NT-proBNP: N-terminal pro-BNP; RH: right heart. #: in idiopathic pulmonary fibrosis; ¶: especially in severe PH.