Abstract
Nipah virus (NiV) is a highly pathogenic paramyxovirus with a high case fatality rate. Due to its high pathogenicity, pandemic potential, and lack of therapeutics or approved vaccines, its study requires biosafety level 4 (BSL4) containment. In this report, we developed a novel neutralization assay for use in biosafety level 2 laboratories. The assay uses a recombinant vesicular stomatitis virus expressing NiV glycoprotein and a fluorescent protein. The recombinant virus propagates as a replication-competent virus in a cell line constitutively expressing NiV fusion protein, but it is restricted to a single round of replication in wild-type cells. We used this system to evaluate the neutralization activity of monoclonal and polyclonal antibodies, plasma from NiV-infected hamsters, and serum from human patients. Therefore, this recombinant virus could be used as a surrogate for using pathogenic NiV and may constitute a powerful tool to develop therapeutics in low containment laboratories.
Keywords: Paramyxoviruses, Nipah virus, Neutralization assay, VSV-Nipah, Antibodies
1. Introduction
Nipah virus (NiV) is an emerging zoonotic virus that causes severe encephalitis and 45–70% case fatality rates (Lo and Rota, 2008). Recent annual outbreaks of NiV in India and recurrent outbreaks in Bangladesh have raised significant public health concerns (Islam et al., 2016; McKee et al., 2022; Soman Pillai et al., 2020; Spiropoulou, 2019; Whitmer et al., 2021; Yadav et al., 2019). NiV belongs to the Paramyxoviridae family and is a negative-sense, single-stranded RNA virus. Its 18.2 kb non-segmented genome encodes 6 structural proteins and 3 non-structural proteins; the structural proteins include nucleocapsid protein (N), phosphoprotein (P), matrix protein (M), fusion protein (F), glycoprotein (G), and RNA-dependent RNA polymerase (L) (Rota and Lo, 2012). Based on phylogenetic analysis, there are two clades of NiV, Bangladesh and Malaysia (Whitmer et al., 2021)..
Due to NiV’s high transmissibility, high fatality rate, and lack of effective vaccines or therapeutics, it is classified as a biosafety level 4 (BSL-4) pathogen (U.S. Dept. of Health and Human Services, 2020). Several candidate vaccines are at various stages of development, most based on inducing neutralizing antibodies produced against NiV-G and NiV–F proteins because these are responsible for viral entry and fusion to the host cells, respectively (de Wit et al., 2023; Foster et al., 2022; Lo et al., 2014a; Mire et al., 2019; Mire et al., 2013; van den Pol et al., 2017; Woolsey et al., 2023). Neutralization assays are a crucial tool for assessing the effectiveness of vaccines and therapeutics against NiV infection. BSL-4 containment is required for neutralization studies using infectious NiV, posing a challenge for countries lacking maximum containment facilities.
Several pseudotyped viruses have been developed to perform neutralization assays in low biocontainment, including murine Moloney leukemia virus (Bae et al., 2019), vesicular stomatitis virus (VSV) (Kaku et al., 2009, 2012; Tamin et al., 2009), and HIV-based pseudotypes (Luo et al., 2023). Pseudotyped viruses are single-cycle replicating viruses that present several advantages over wild-type viruses, including high sensitivity and specificity, low cost, ease of use, and the ability to be performed in low biocontainment facilities. However, the generation of a stock of pseudotyped viruses requires transfecting mammalian cells with multiple plasmids, which represent a serious limitation for a scaled-up manufacturing process.
To address the challenges associated with current pseudotype-based systems for NiV, we developed an efficient system for conducting neutralization studies in BSL-2 conditions. We devised a novel neutralization assay that uses a recombinant VSV virus expressing the reporter protein ZsGreen (ZsG) and NiV-G. This recombinant virus was efficiently propagated in a newly developed cell line, which constitutively expresses the NiV–F protein.
In this study, we demonstrate the use of the system for conducting neutralization studies in a rapid, sensitive, and quantitative manner. The results of neutralization assays using rVSVΔG-NiV-G are comparable to those of neutralization studies done using infectious NiV in BSL-4, making our VSV-based system a suitable surrogate for infectious NiV.
2. Materials and methods
2.1. Biosafety and ethics
All work with the infectious NiV or infected animals was done in a BSL-4 facility at the Centers for Disease Control and Prevention (CDC, USA) following established BSL-4 standard operating procedures. Experiments with recombinant VSV-based viruses were performed in a BSL-2 laboratory. All recombinant virus work was approved by the CDC Institutional Biosafety Committee. All animal experiments were approved by the CDC Institutional Animal Care and Use Committee and performed in an AALAC International-approved facility (2956SPEHAMC, 2798LOHAMC, 3113SPEMULC). Human serum samples were obtained from patients during an NiV outbreak in Bangladesh and were approved for use by CDC Institutional Review Board (CDC approved protocol #7276).
2.2. Cell cultures
Huh-7 (Apath LLC) and Vero-E6 cells (CDC Core Facility) were propagated in Dulbecco’s modified Eagle medium (Gibco) supplemented with 1 × non-essential amino acids, 5% (v/v) fetal bovine serum, 100 units/mL penicillin, and 100 μg/mL streptomycin (Gibco). All cells were incubated at 37°C in 5% CO2. Vero-Fco cells have been described previously (Welch et al., 2023). Briefly, a codon-optimized sequence encoding the Fusion protein of NiV strain Malaysia (Genbank AF212302) (Chua et al., 2000) was inserted into the cell genome using the Flp-In system (Invitrogen).
2.3. Generation of recombinant rVSVΔG-NiV-G
Recombinant rVSVΔG-NiV-G, expressing NiV G protein and fluorescent reporter ZsG, was generated using NiV prototype Malaysia strain (GenBank AF212302) as described previously (Shrivastava-Ranjan et al., 2023). Briefly, VSV glycoprotein was replaced with NiV-G and ZsG was inserted upstream of the VSV N (nucleoprotein) gene, separated from N by the self-cleaving 2A porcine teschovirus (P2A) sequence. To generate helper plasmids for rescue, VSV-G (glycoprotein), VSV-L (polymerase), VSV-N, VSV-P (phosphoprotein), and T7 RNA polymerase genes were cloned into a standard pol II expression vector (pCAGGS). To rescue rVSVΔG-NiV-G, different concentrations of full-length pVSVΔG-NiV-G, pCDNA-T7, pCDNA-VSV-L, pCDNA-VSV-N, pCDNA-VSV-P, and pCDNA-VSV-G were transfected into Huh-7 cells, and the supernatants were blind-passaged twice onto Vero-Fco cells, a cell line constitutively expressing NiV–F. Recombinant viruses were titered using a standard 50% tissue culture infectious dose (TCID50) using the Reed and Muench method in both Vero-Fco and wild-type Vero-E6 cells. Viral sequences were confirmed by next generation sequencing (NGS) on a MiniSeq platform (Illumina), and sequences were analyzed using CLC genomics workbench v 20.0 (Qiagen).
2.4. Immunofluorescence assay
For immunofluorescence assay (IFA), cells were seeded onto 6-well plates (Costar) and infected with recombinant virus at MOI of 0.1 or mock infected. Three days post infection, cells were fixed with 10% formalin for 30 min followed by permeabilization with 0.1% Triton X-100 in phosphate-buffered saline (PBS) for 15 min and blocking with 1% bovine serum albumin for 1 h. Either monoclonal anti-NiV F antibody (Absolute Antibody) or polyclonal antibody against Hendra virus soluble glycoprotein (HeV-sG) was used as the primary antibody, followed by two washes with PBS and treatment with secondary anti-rabbit Alexa 594 antibody. Cell nuclei were stained with NucBlue (Thermo-Fisher). Cells were observed and imaged using an EVOS digital inverted microscope (Thermo-Fisher) with 10 × objective.
2.5. Enzyme-linked immunosorbent assay
Enzyme-linked immunosorbent assay (ELISA) was performed as mentioned previously (Welch et al., 2023). Briefly, after overnight coating of Maxisorp plates (ThermoFisher) at 4°C with recombinant NiV strain Malaysia N or G diluted in coating buffer, the plates were washed 5 times using TBS-T (Thermo-Fisher) and a Biotek automated plate washer. Thereafter, wells were blocked for 1 h at 37°C with blocking buffer (5% milk TBS-T). Serially diluted sample in blocking buffer was added to the blocked plates and incubated for 1 h at 37°C. The plates were washed 5 times before secondary antibody (either HRP-conjugated goat monoclonal anti-hamster IgG [for hamster samples] or mouse anti-human HRP [for human samples] diluted in blocking buffer) was added and incubated 1h at 37°C. After washing, TMB-Ultra solution (Thermo-Fisher) was added and incubated at room temperature for 6 min. Reactions were stopped with Stop solution (Invitrogen SS04) and 450 nm absorbance was read on a Synergy HD1 Biotek plate reader.
2.6. Neutralization assays
Neutralization assays were performed on hamster plasma samples and human serum samples. Plasma was obtained from terminal intracardiac blood collected in EDTA from naïve hamsters (male and female; 5–10 week old HsdHan:AURA Syrian hamsters; Envigo no. 8903F or 8903 M) or hamsters inoculated intranasally with 103 to 107 TCID50 (100 μL total, divided bilaterally between the nares) of NiV strain Malaysia, recombinant NiV Malaysia, or recombinant reporter-expressing NiV Malaysia (rNIV-M-ZsG), as previously reported (Lo et al., 2014b; Welch et al., 2020). Antibodies against NiV–F (12B2) and henipavirus-G (7B7 and 5B1) were obtained from Absolute Antibody. For the neutralization assay, 10,000 cells/well were seeded onto 96-well plates one day prior to the experiment. Serial 5-fold dilutions of antibodies, hamster plasma, or human serum samples were mixed with 100 TCID50 of rVSVΔG-NiV-G or rNiV-M-ZsG (infectious NiV). After the virus-antibody/sample mixture was incubated for 1 h at 37°C, it was added to Vero-Fco (for rVSVΔG-NiV-G) or Vero-E6 (for rNiV-M-ZsG) monolayers in triplicate. Cells were incubated for 72 h at 37°C and the fluorescence signal was measured using a plate reader (BioTek).
2.7. Data analysis
All experiments were done in triplicate. Data were analyzed using GraphPad Prism v9 (GraphPad Software). Fluorescence values of ZsG expression were normalized to fluorescence in non-infected cells. The resulting normalized values were used to fit a 4-parameter equation to semi-log plots of the concentration-response data. Dilution of the antibodies/samples inhibiting 50% of ZsG expression (IC50) was calculated by interpolating the values.
3. Results
3.1. Generation and characterization of rVSVΔG-NiV-G based neutralization system
Using a standard reverse genetics approach, we first generated two recombinant viruses in Huh7 cells, rVSVΔG-NiV-F and rVSVΔG-NiV-G, expressing NiV F and G proteins respectively (data not shown). Co-infection of VeroE6 cells with the two complementing viruses yielded a virus mix, albeit with a low titer (~102 TCID50/mL) that prevented any further use in the current neutralization assay.
As an alternate strategy, we propagated rVSVΔG-NiV-G expressing NiV G and the fluorescent protein, ZsG (Fig. 1A) on a cell line constitutively expressing NiV F protein, which was previously developed in our lab (Welch et al., 2023). The expression of NiV F on Vero-Fco cells was confirmed by IFA (Fig. 1B). After infection of Vero-Fco cells with the rescued virus, rVSVΔG-NiV-G, a very efficient propagation was observed (Fig. 1C). The resulting virus stock was titered by TCID50 in both Vero-Fco (4*104 TCID50/mL) and Vero-E6 cells (6*103 TCID50/mL), and its genetic composition was confirmed by NGS. The complete strategy to generate an efficient neutralization assay for NiV is shown in Fig. 1D schematics.
Fig. 1.
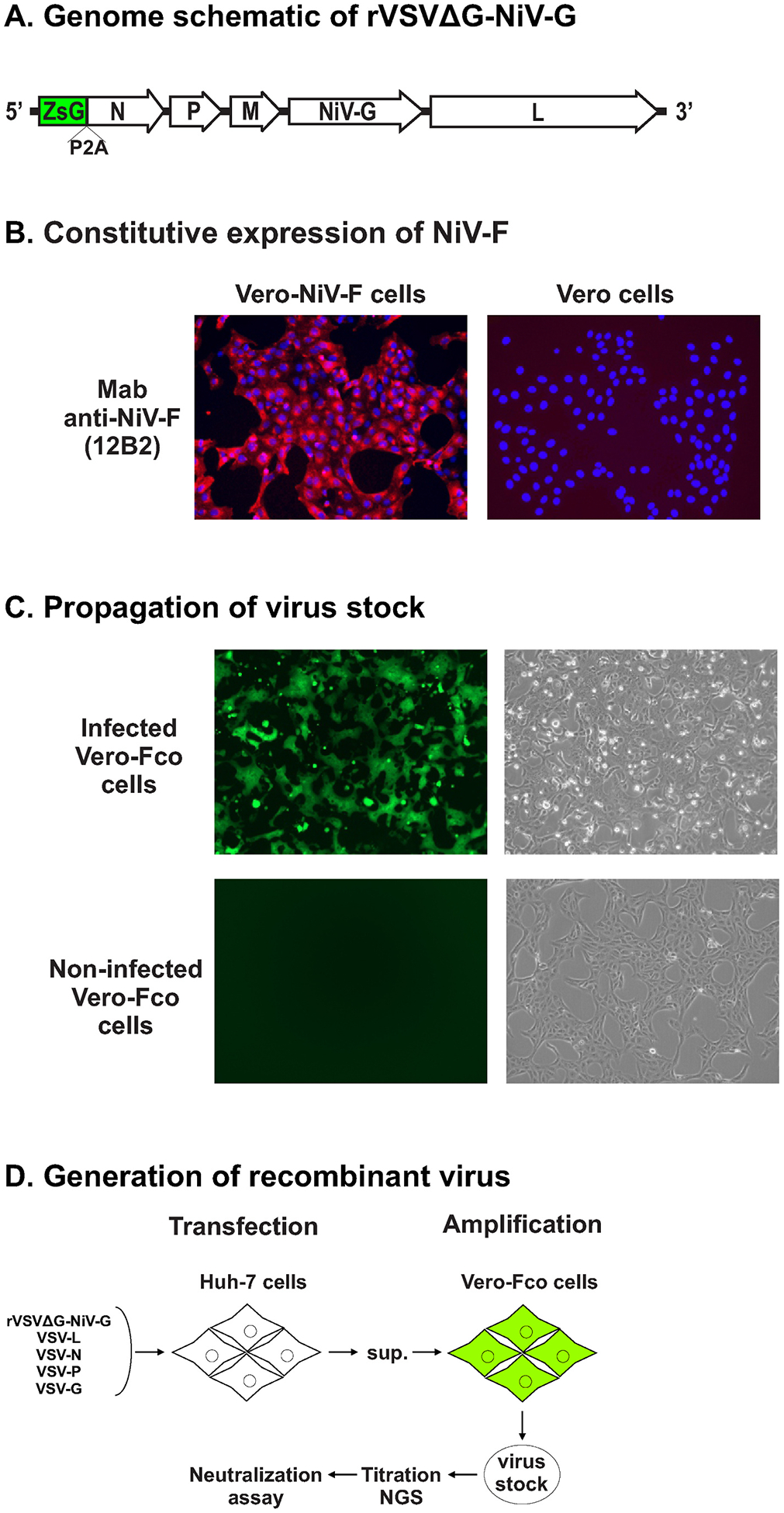
Construction of recombinant rVSVΔG-NiV-G
A) Genome schematic of rVSVΔG-NiV-G: The recombinant virus contains ZsGreen (ZsG) fused to vesicular stomatitis virus (VSV) nucleoprotein (N) via a porcine teshovirus-1 2A (P2A), VSV phosphoprotein (P), VSV matrix protein (M), Nipah virus (NiV) glycoprotein (G), and VSV-polymerase (L). B) Constitutive expression of NiV–F in Vero-Fco: Continuing expression of NiV F protein in Vero-Fco cells (Welch et al., 2023) was verified by immunofluorescence assays (IFA) performed on non-infected Vero-Fco and Vero-E6 cells using anti-NiV F protein antibody (12B2). Representative IFA images (magnification 10 ×) of non-infected Vero-Fco and Vero-E6 cells collected using EVOS microscope. C) Replication of recombinant virus in Vero-Fco cells: Representative images (magnification 10 ×; EVOS microscope) of Vero-Fco infected with rVSVΔG-NiV-G or mock infected. D) Strategy to generate rVSVΔG-NiV-G: Plasmids encoding VSVΔG-NiV-G, VSV-L, VSV-N, VSV-P, and VSV-G were co-transfected into Huh-7 cells to rescue rVSVΔG-NiV-G. The supernatant was blind-passaged onto Vero-Fco cells, and the resulting virus stock was titered using TCID50 determination method and sequenced by next-generation sequencing.
Moreover, a strong expression of NiV G was observed by IFA on Vero-Fco cells infected with rVSVΔG-NiV-G (Fig. 2A). It is also important to notice that the virus underwent multiple replication cycles in Vero-Fco cells, but only underwent a single-cycle-replication in Vero-E6 cells because of the expression of the fusion gene in the Vero-Fco cell line. (Fig. 2B).
Fig. 2.
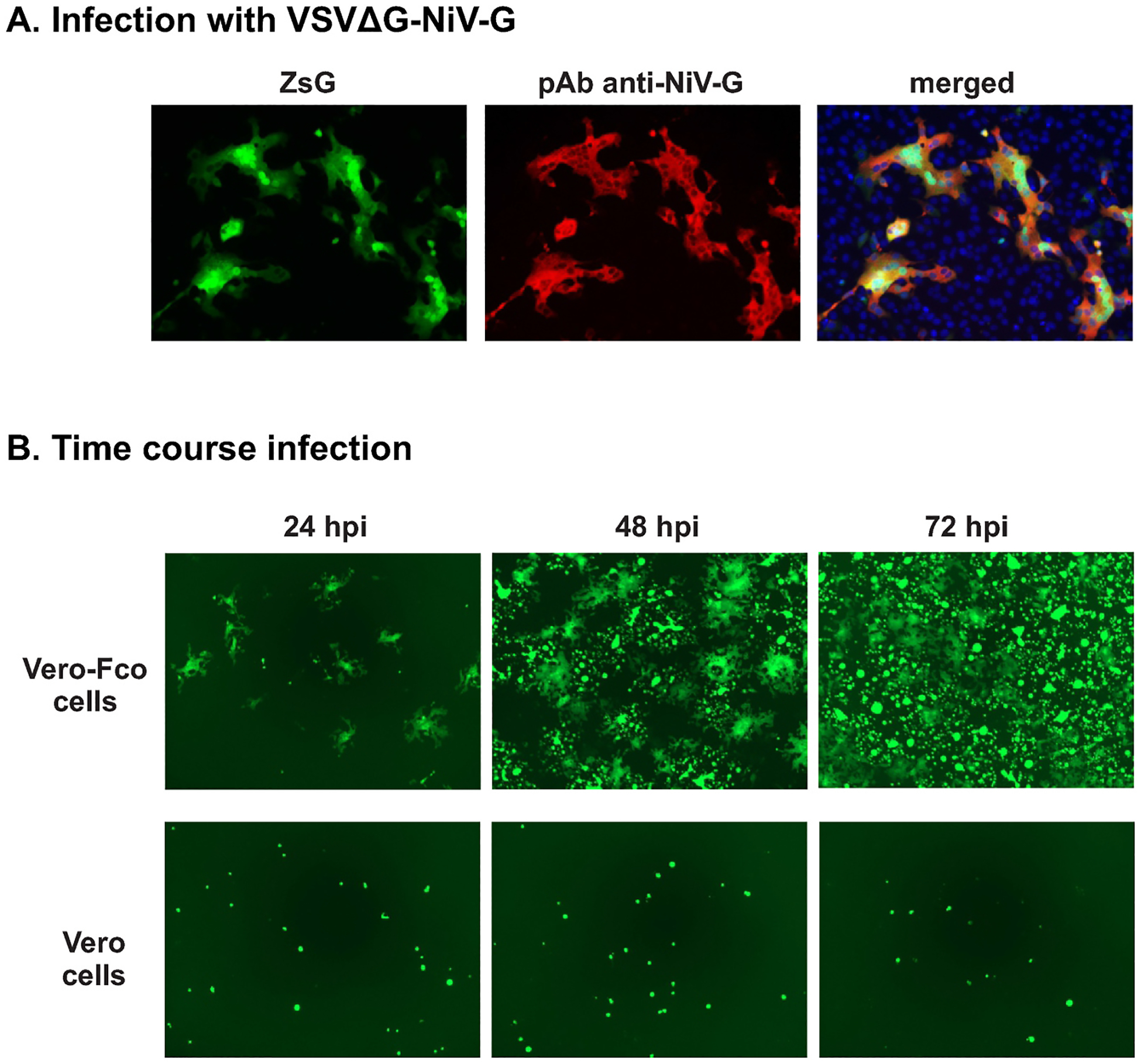
Infection of cells with rVSVΔG-NiV-G
A) rVSVΔG-NiV-G replication in Vero-Fco cells: Representative IFA images (magnification 10 ×; EVOS microscope) of Vero-Fco infected with rVSVΔG-NiV-G and probed with anti-NiV G antibody. B) Single-cycle replication in rVSVΔG-NiV-G in Vero-E6 cells: Vero-Fco and Vero-E6 cells were infected with rVSVΔG-NiV-G and ZsG fluorescence images (magnification 10 ×; EVOS microscope) were taken 24 h post infection (hpi), 48 hpi, and 72 hpi.
3.2. Neutralization assay
As a proof of concept, we tested rVSVΔG-NiV-G in a neutralization assay using a selected group of monoclonal and polyclonal antibodies against Nipah and Hendra virus F and G glycoproteins. As shown in Fig. 3A, the three antibodies targeting NiV–F, HeV-sG and Henipavirus-G efficiently neutralized rVSVΔG-NiV-G, while no neutralization activity was detected for the Rift Valley Fever (RVFV) control antibody. Moreover, quantitation of ZsG fluorescence indicated that the three antibodies neutralized rVSVΔG-NiV-G in a dose-dependent manner (Fig. 3B).
Fig. 3.
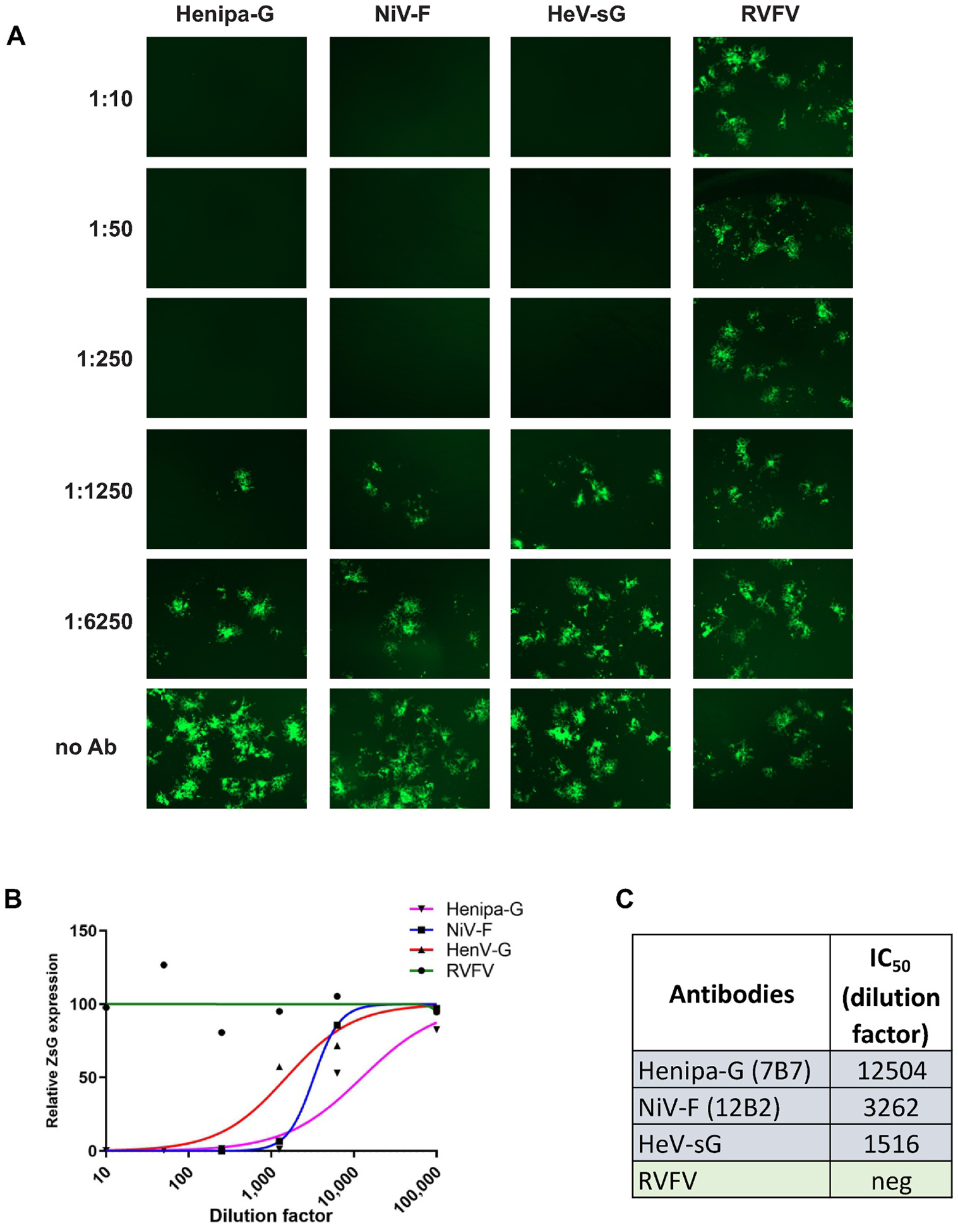
Neutralization assays using Henipavirus antibodies.
A) Neutralization assays using rVSVΔG-NiV-G: Vero-Fco cells were treated with serial 5-fold dilutions of indicated antibodies mixed with 100 TCID50 of the recombinant virus (rVSVΔG-NiV-G). After 72 h, fluorescence signal was measured using Synergy. Representative images of the neutralization activity of anti-Henipavirus glycoprotein (anti-Henipa-G-7B7), anti-NiV-F (12B2), rabbit polyclonal anti-Hendra virus glycoprotein (anti-HeV-sG), and anti-Rift Valley Fever Virus (anti-RVFV) antibodies in cells infected with recombinant virus. B) Concentration-response curves in Vero-Fco cells: Vero-Fco cells were infected with recombinant virus after neutralization with anti-Henipa-G (pink triangles), anti-HeV-G (red triangles), anti-NiV-F (blue squares), or anti-RVFV (green circles). Relative fluorescence units (RFU) are shown on the y-axis. Each point on the graph represents mean values, and error bars indicate standard deviations of triplicate wells. C) 50% effective inhibition concentration (IC50) values of each indicated antibody against rVSVΔG-NiV-G.
Furthermore, we sought to test a series of samples collected from hamsters infected with NiV-Malaysia, and their IgG specific antibodies were previously determined in our lab. As shown in Fig. 4A, all hamster samples with high IgG specific titers also exhibited neutralization activity against rVSVΔG-NiV-G in a dose-dependent manner. As expected, no neutralizing activity, even at lower dilutions, was observed in serum samples from non-infected hamsters, and thereby demonstrating the specificity of the current assay (Fig. 4B).
Fig. 4.
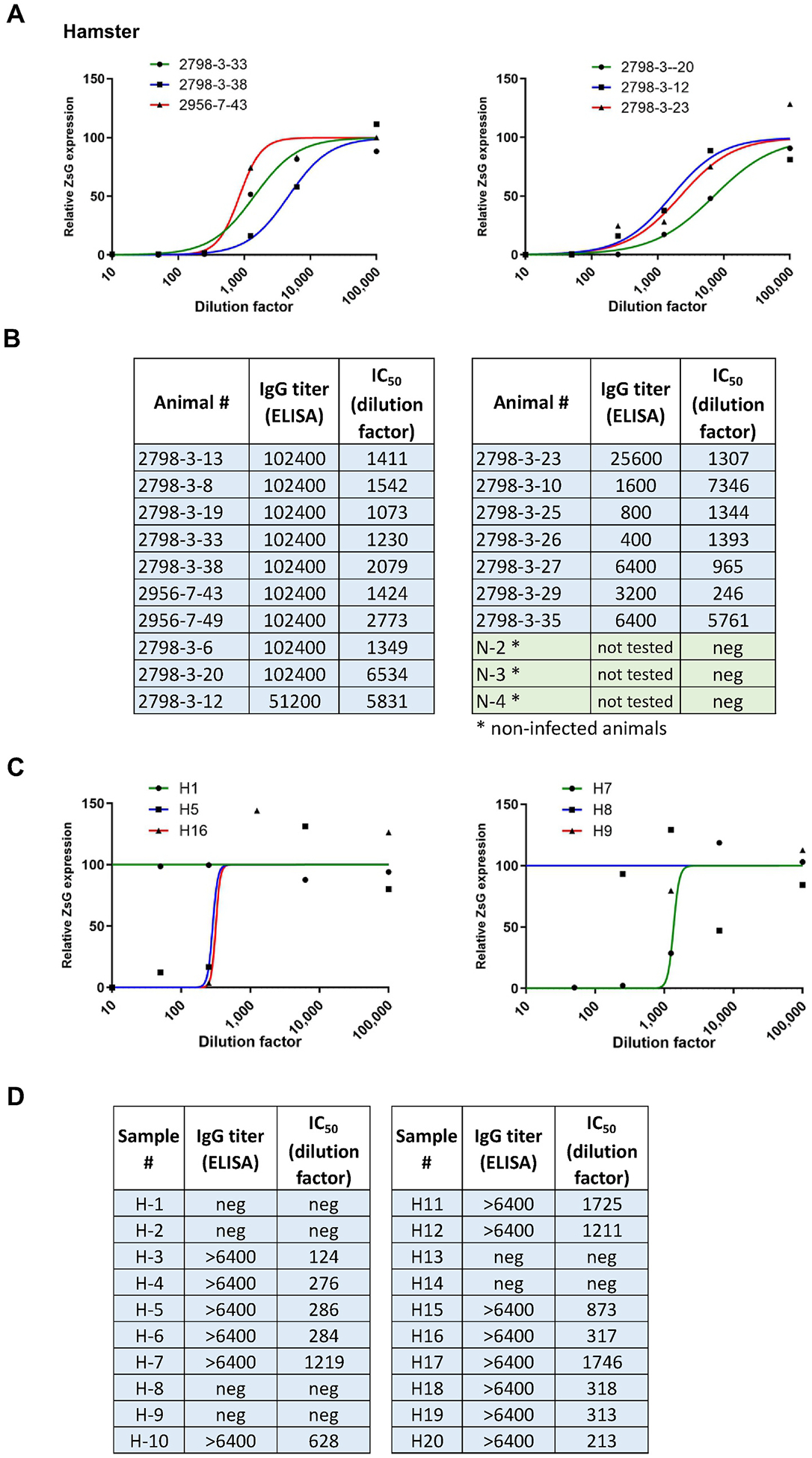
Neutralization assays using NiV-infected hamster plasma and human serum samples
A) Neutralization assays using rVSVΔG-NiV-G and plasma from infected hamsters: Vero-Fco cells were treated with serial 5-fold dilutions of different hamster serum samples mixed with 100 TCID50 of the recombinant virus. After 72 h, fluorescence signal was measured using Synergy (BioTek). The graphs show representative concentration-response curves in Vero-Fco cells infected with recombinant virus after neutralization with plasma samples obtained from hamsters infected with either NiV-M or NiV-M-ZsG, or uninfected (N). Each point on the graph represents mean and error bars indicate standard deviations of triplicate wells. N/A indicates negative for the assay. B) IC50 values of each hamster serum sample’s neutralization of rVSVΔG-NiV-G along with IgG ELISA titer values. C) Neutralization assays using rVSVΔG-NiV-G and human serum: Vero-Fco cells were treated with serial 5-fold dilutions of different human serum samples mixed with 100 TCID50 of the recombinant virus. After 72 h, fluorescence signal was measured using Synergy (BioTek). Figure shows concentration-response curves in Vero-Fco cells infected with recombinant virus after neutralization with human serum samples. Each point on the graph represents the mean and error bars indicate standard deviations of triplicate wells. D) IC50 values of each human sample’s neutralization of rVSVΔG-NiV-G along with IgG ELISA titer values.
In addition, we also tested a series of human samples collected from patients during the 2020 and 2021 seasonal NiV outbreaks in Bangladesh. All samples with high IgG titers, efficiently neutralized rVSVΔG-NiV-G in a dose-dependent manner, while those negative in the ELISA assay did not exhibit neutralization activity, even at low serum dilutions (Figure 4C and 4D).
In order to find whether the neutralization activity observed on the rVSVΔG-NiV-G assay was comparable with that using fully infectious virus, we tested representative samples using recombinant NiV-ZsG (Lo et al., 2014b) in our BSL4 lab. As expected, representative samples that exhibited neutralization activity against rVSVΔG-NiV-G also neutralized fully infectious NiV (Supplementary figure).
Finally, it is worth to notice that the current neutralization assay efficiently detected antibodies against both NiV Malaysia and Bangladesh strains obtained from lab-infected hamsters and human samples respectively. Overall, these results show that rVSVΔG-NiV-G can be efficiently used as a surrogate for infectious NiV, allowing the performance of neutralization assays in lower-biocontainment facilities.
4. Discussion
In this report, we successfully developed a novel VSV-based neutralization system for NiV that addresses several limitations of previous methodologies. This system offers a number of advantages, making it an ideal choice for neutralization and entry studies for NiV. One of the most significant benefits of this new system is that it expresses a fluorescent reporter, making quantitative studies easier and more efficient. In addition, our neutralization system has demonstrated high sensitivity and reproducibility in detecting neutralizing antibodies against both NiV-Malaysia infected hamster samples and NiV-Bangladesh infected human samples. This indicates that the neutralization assay can be used to detect the antibodies against both NiV strains. This is particularly important for evaluating potential antiviral therapeutics and antibodies as well as for monitoring the immune response in NiV infected individuals or in individuals in vaccine studies. This system can serve as proof-of-concept for developing similar systems for other paramyxoviruses and for investigating viral neutralization and entry mechanisms of paramyxoviruses.
Single-cycle replicating VSV viruses has been successfully used on studies of viral entry and as vaccines candidates (Chattopadhyay and Rose, 2011; Kaku et al., 2009; Lo et al., 2014a; Suda et al., 2016; Whitt, 2010). In particular, a single-cycle VSV-NiV-G has been reported as an effective vaccine candidate that conferred both rapid and long-lasting immunity against NiV (Foster et al., 2022; Woolsey et al., 2023). However, the propagation of large stocks of single-cycle pseudotyped viruses presents a serious manufacturing challenge. In contrast, the rVSVΔG-NiV-G presented in this report could be tested as another safe vaccine candidate, since it also exhibits a single-cycle replicating phenotype in wild-type cells, but could be propagated at large scale in cells constitutively expressing NiV–F.
In conclusion, our novel neutralization system for NiV offers significant improvements over existing methodologies, facilitating research on this highly pathogenic virus. The simplicity, ease of generating virus stocks, and reproducibility of this system make it an invaluable tool for studying NiV. This is particularly advantageous since NiV is a BSL-4 pathogen, which requires stringent safety measures and specialized laboratories for handling. By using a VSV-based system, the work with infectious NiV can be avoided, making it possible to conduct research in low containment laboratories.
Supplementary Material
Acknowledgements:
We thank Tatyana Klimova for excellent assistance with editing the manuscript.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the CDC.
Financial Support
Shilpi Jain holds a fellowship supported by the Research Participation Program at the CDC administered by the Oak Ridge Institute for Science and Education through an interagency agreement between the U.S. Department of Energy (DOE) and CDC.
This work was supported in part by the DARPA INTERfering and Co-Evolving Prevention and Therapy (INTERCEPT) program (DARPA-BAA-16-35).
Footnotes
CRediT authorship contribution statement
Shilpi Jain: Conceptualization, Methodology, Validation, Formal analysis, Writing – original draft. Michael K. Lo: Resources, Writing – review & editing. Markus H. Kainulainen: Resources, Writing – review & editing. Stephen R. Welch: Resources. Jessica R. Spengler: Resources, Writing – review & editing. Syed M. Satter: Resources. Mohammed Ziaur Rahman: Resources. Mohammad Enayet Hossain: Resources. Cheng-Feng Chiang: Resources. John D. Klena: Resources. Éric Bergeron: Resources, Writing – review & editing. Joel M. Montgomery: Resources, Supervision, Funding acquisition. Christina F. Spiropoulou: Resources, Supervision, Funding acquisition. César G. Albariño: Investigation, Methodology, Validation, Conceptualization, Formal analysis, Writing – original draft, Writing – review & editing, Resources, Supervision.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.virol.2023.109858.
References
- Bae SE, Kim SS, Moon ST, Cho YD, Lee H, Lee JY, Shin HY, Lee HJ, Kim YB, 2019. Construction of the safe neutralizing assay system using pseudotyped Nipah virus and G protein-specific monoclonal antibody. Biochem. Biophys. Res. Commun 513, 781–786. [DOI] [PubMed] [Google Scholar]
- Chattopadhyay A, Rose JK, 2011. Complementing defective viruses that express separate paramyxovirus glycoproteins provide a new vaccine vector approach. J. Virol 85, 2004–2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chua KB, Bellini WJ, Rota PA, Harcourt BH, Tamin A, Lam SK, Ksiazek TG, Rollin PE, Zaki SR, Shieh W, Goldsmith CS, Gubler DJ, Roehrig JT, Eaton B, Gould AR, Olson J, Field H, Daniels P, Ling AE, Peters CJ, Anderson LJ, Mahy BW, 2000. Nipah virus: a recently emergent deadly paramyxovirus. Science 288, 1432–1435. [DOI] [PubMed] [Google Scholar]
- de Wit E, Feldmann F, Cronin J, Goldin K, Mercado-Hernandez R, Williamson BN, Meade-White K, Okumura A, Callison J, Weatherman S, Rosenke R, Avanzato VA, Lovaglio J, Scott DP, Marzi A, Feldmann H, 2023. Distinct VSV-based Nipah virus vaccines expressing either glycoprotein G or fusion protein F provide homologous and heterologous protection in a nonhuman primate model. EBioMedicine 87, 104405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster SL, Woolsey C, Borisevich V, Agans KN, Prasad AN, Deer DJ, Geisbert JB, Dobias NS, Fenton KA, Cross RW, Geisbert TW, 2022. A recombinant VSV-vectored vaccine rapidly protects nonhuman primates against lethal Nipah virus disease. Proc. Natl. Acad. Sci. U. S. A 119, e2200065119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Islam MS, Sazzad HM, Satter SM, Sultana S, Hossain MJ, Hasan M, Rahman M, Campbell S, Cannon DL, Stroher U, Daszak P, Luby SP, Gurley ES, 2016. Nipah virus transmission from bats to humans associated with drinking traditional liquor made from date palm Sap, Bangladesh, 2011–2014. Emerg. Infect. Dis 22, 664–670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaku Y, Noguchi A, Marsh GA, Barr JA, Okutani A, Hotta K, Bazartseren B, Fukushi S, Broder CC, Yamada A, Inoue S, Wang LF, 2012. Second generation of pseudotype-based serum neutralization assay for Nipah virus antibodies: sensitive and high-throughput analysis utilizing secreted alkaline phosphatase. J. Virol Methods 179, 226–232. [DOI] [PubMed] [Google Scholar]
- Kaku Y, Noguchi A, Marsh GA, McEachern JA, Okutani A, Hotta K, Bazartseren B, Fukushi S, Broder CC, Yamada A, Inoue S, Wang LF, 2009. A neutralization test for specific detection of Nipah virus antibodies using pseudotyped vesicular stomatitis virus expressing green fluorescent protein. J. Virol Methods 160, 7–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo MK, Bird BH, Chattopadhyay A, Drew CP, Martin BE, Coleman JD, Rose JK, Nichol ST, Spiropoulou CF, 2014a. Single-dose replication-defective VSV-based Nipah virus vaccines provide protection from lethal challenge in Syrian hamsters. Antivir. Res 101, 26–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo MK, Nichol ST, Spiropoulou CF, 2014b. Evaluation of luciferase and GFP-expressing Nipah viruses for rapid quantitative antiviral screening. Antivir. Res 106, 53–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo MK, Rota PA, 2008. The emergence of Nipah virus, a highly pathogenic paramyxovirus. J. Clin. Virol 43, 396–400. [DOI] [PubMed] [Google Scholar]
- Luo X, Wang C, Huang Y, Cong S, Tan J, Hou W, Ma F, Zheng L, 2023. Establishment of a neutralization assay for Nipah virus using a high-titer pseudovirus system. Biotechnol. Lett 45, 489–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKee CD, Islam A, Rahman MZ, Khan SU, Rahman M, Satter SM, Islam A, Yinda CK, Epstein JH, Daszak P, Munster VJ, Hudson PJ, Plowright RK, Luby SP, Gurley ES, 2022. Nipah virus detection at bat roosts after Spillover events, Bangladesh, 2012–2019. Emerg. Infect. Dis 28, 1384–1392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mire CE, Geisbert JB, Agans KN, Versteeg KM, Deer DJ, Satterfield BA, Fenton KA, Geisbert TW, 2019. Use of single-injection recombinant vesicular stomatitis virus vaccine to protect nonhuman primates against lethal Nipah virus disease. Emerg. Infect. Dis 25, 1144–1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mire CE, Versteeg KM, Cross RW, Agans KN, Fenton KA, Whitt MA, Geisbert TW, 2013. Single injection recombinant vesicular stomatitis virus vaccines protect ferrets against lethal Nipah virus disease. Virol. J 10, 353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rota PA, Lo MK, 2012. Molecular virology of the henipaviruses. Curr. Top. Microbiol. Immunol 359, 41–58. [DOI] [PubMed] [Google Scholar]
- Shrivastava-Ranjan P, Jain S, Chatterjee P, Montgomery JM, Flint M, Albarino C, Spiropoulou CF, 2023. Development of a Novel Minigenome and Recombinant VSV Expressing Seoul Hantavirus Glycoprotein-Based Assays to Identify Anti-hantavirus Therapeutics. Antiviral Res, 105619. [DOI] [PubMed] [Google Scholar]
- Soman Pillai V, Krishna G, Valiya Veettil M, 2020. Nipah Virus: Past Outbreaks and Future Containment. Viruses 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spiropoulou CF, 2019. Nipah virus outbreaks: Still Small but extremely lethal. J. Infect. Dis 219, 1855–1857. [DOI] [PubMed] [Google Scholar]
- Suda Y, Fukushi S, Tani H, Murakami S, Saijo M, Horimoto T, Shimojima M, 2016. Analysis of the entry mechanism of Crimean-Congo hemorrhagic fever virus, using a vesicular stomatitis virus pseudotyping system. Arch. Virol 161, 1447–1454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamin A, Harcourt BH, Lo MK, Roth JA, Wolf MC, Lee B, Weingartl H, Audonnet JC, Bellini WJ, Rota PA, 2009. Development of a neutralization assay for Nipah virus using pseudotype particles. J. Virol Methods 160, 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Dept. of Health and Human Services, P.H.S, 2020. Biosafety in microbiological and biomedical laboratories. In: U.S. Dept. of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Institutes of Health, sixth ed. [Google Scholar]
- van den Pol AN, Mao G, Chattopadhyay A, Rose JK, Davis JN, 2017. Chikungunya, influenza, Nipah, and Semliki forest chimeric viruses with vesicular stomatitis virus: actions in the brain. J. Virol 91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welch SR, Scholte FEM, Harmon JR, Coleman-McCray JD, Lo MK, Montgomery JM, Nichol ST, Spiropoulou CF, Spengler JR, 2020. In Situ imaging of fluorescent Nipah virus respiratory and neurological tissue tropism in the Syrian hamster model. J. Infect. Dis 221, S448–S453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welch SR, Spengler JR, Genzer SC, Coleman-McCray JD, Harmon JR, Sorvillo TE, Scholte FEM, Rodriguez SE, Ritter JM, Ficarra G, Davies KA, Kainulanein MH, Karraslan E, Bergeron E, Goldsmith CS, Lo MK, Nichol ST, Montgomery JM, Spiropoulou CF, 2023. Single dose mucosal delivery of Nipah replicon-particle vaccine protects against lethal disease up to three days after vaccination. Sci. Adv (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitmer SLM, Lo MK, Sazzad HMS, Zufan S, Gurley ES, Sultana S, Amman B, Ladner JT, Rahman MZ, Doan S, Satter SM, Flora MS, Montgomery JM, Nichol ST, Spiropoulou CF, Klena JD, 2021. Inference of Nipah virus evolution, 1999–2015. Virus Evol 7 veaa062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitt MA, 2010. Generation of VSV pseudotypes using recombinant DeltaG-VSV for studies on virus entry, identification of entry inhibitors, and immune responses to vaccines. J. Virol Methods 169, 365–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolsey C, Borisevich V, Fears AC, Agans KN, Deer DJ, Prasad AN, O’Toole R, Foster SL, Dobias NS, Geisbert JB, Fenton KA, Cross RW, Geisbert TW, 2023. Recombinant vesicular stomatitis virus-vectored vaccine induces long-lasting immunity against Nipah virus disease. J. Clin. Investig 133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yadav PD, Shete AM, Kumar GA, Sarkale P, Sahay RR, Radhakrishnan C, Lakra R, Pardeshi P, Gupta N, Gangakhedkar RR, Rajendran VR, Sadanandan R, Mourya DT, 2019. Nipah virus sequences from humans and bats during Nipah outbreak, Kerala, India, 2018. Emerg. Infect. Dis 25, 1003–1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


