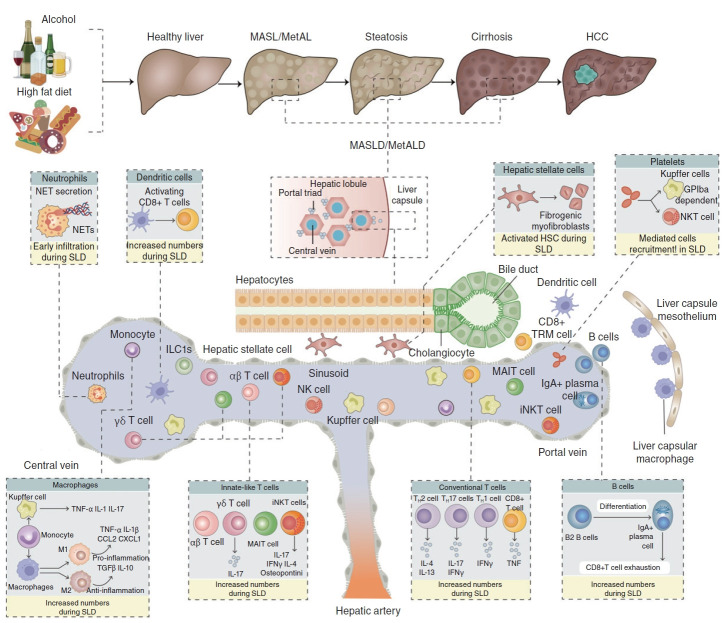
Figure 3.
Immune modulations of SLD pathogenesis. The hepatic immune cell repertoire is altered and participates in the uncontrolled inflammatory environment that promotes hepatocyte death and liver fibrosis. These immune cells include innate-like T cells, such as iNKT cells, MAIT cells and γδ T cells, as well as conventional CD8+ T cells and CD4+ T cell subsets, including IFNγ-producing TH1 cells [156], IL-4- and/or IL-13-producing TH2 cells [169], and IL-17-producing TH17 cells [157]. NETs are secreted or released during NETosis. Neutrophil accumulation is a precursor to SLD that causes inflammation and liver damage [189, 190]. The population of DCs and type 1 conventional DCs (cDC1s in particular) increases, promoting hepatic damage and liver inflammation by activating CD8+ T cells [131, 132]. Monocytes are also quickly recruited to the liver, where they can develop into pro-inflammatory macrophages or differentiate into KCs, which are derived from monocytes [194, 195]. Platelets are more numerous and more active, which promotes liver steatosis, inflammation, and damage. This suggests that platelets may activate and directly bind to KCs in a glycoprotein GPIb-dependent manner. B lymphocytes, particularly IgA+ plasma cells, accelerate the development of SLD by exhausting CD8+ T lymphocytes, which is one of their immunosuppressive actions [185, 186]. Additionally, the cytotoxic actions of fatty acids reduce the anti-injury potential of CD4+ T cells, promoting SLD progression to HCC [142, 143]. Moreover, CD8+ T cells and, particularly, the auto-aggressive CXCR6+ subset promote liver damage and the SLD-HCC transition by secreting pro-inflammatory cytokines like TNF and directly killing hepatocytes in a FASL-dependent and TNF-dependent manner [159, 160]. SLD, steatotic liver diseases; NKT cell, natural killer T cells; MAIT, Mucosal Associated Invariant T cells; IFNγ, interferon γ; NETs, neutrophil extracellular traps; SLD, steatotic liver diseases; DCs, dendritic cells; KCs, Kupffer cells; HCC, hepatocellular carcinoma.