Abstract
Emerging symmetrical limb weakness, altered sensory perception, and absent or reduced deep tendon reflexes are the hallmarks of Guillain-Barre syndrome (GBS). There are numerous studies that indicate up to two-thirds of patients with GBS may also have autonomic dysfunction. One uncommon presenting characteristic of GBS before motor weakness is evident is paralytic ileus, a sign of gastrointestinal dysautonomia. Here we describe the case of a 55-year-old man who was brought to the emergency room of our hospital with paralytic ileus, a less common symptom of early-stage GBS. The patient was initially treated with prokinetic drugs and total parenteral nutrition with no clinical improvement. The patient quickly developed ascending lower limb weakness that progressed to quadriplegia, which ultimately affected respiratory muscles, leading to respiratory failure requiring mechanical ventilation and intensive care unit hospitalization. A nerve conduction study showed demyelinating sensorimotor polyneuropathy. Analysis of cerebrospinal fluid revealed albumin-cytological dissociation. The patient was treated with intravenous immunoglobulin (IVIG) and other supportive treatments. Even though the patient’s enteral feeding support was uncomfortable due to a profound infection complicating lack of stomach emptying during the hospital stay, the patient passed away two months after being admitted. Lack of awareness about GBS gastrointestinal dysautonomia may cause delays in treatment initiation, and as a result, GBS may lead to life-threatening events. Reducing mortality and morbidity from GBS requires prompt diagnosis and treatment. This case reminds us that GBS may present as gastrointestinal dysautonomia.
Keywords: Gullian-Barre syndrome, paralytic ileus, quadraparesis, intravenous immunoglobulin
Introduction
Guillain-Barré syndrome(GBS) is a type of acute inflammatory polyradiculoneuropathy that is usually demyelinating. It was first described by Georges Guillain, Jean-Alexandre Barré, and André Strohl in 1916.1 In most cases, it is distinguished by ascending symmetrical limb weakness, sensory abnormalities, and absent or diminished deep tendon reflexes GBS results from an immunological response to peripheral nerves.2 Paralytic ileus occurs when the motor activity of the gastrointestinal system is impaired without associated physical or mechanical obstruction. Paralytic ileus presents with bowel distension, abdominal cramps, absent bowel sounds, loss of bowel movement, gastric stasis leading to hiccups, and bowel discomfort.3 Paralytic ileus results from a loss of motility in the intestinal musculature with no associated physical obstruction. Paralytic ileus has variable etiologies, including postoperative state, pharmacological, infection, and endocrinometabolic conditions.4 One of the common critical manifestations of GBS is the involvement of the autonomic nervous system. Features of dysautonomia are cardiac arrhythmias, fluctuations of blood pressure, paralytic ileus, and urinary retention. These autonomic dysfunctions complicate the management of GBS and increase mortality.5 This case study describes a 55-year-old male patient with GBS who first presented with paralytic ileus.
Case Presentation
After experiencing constipation and abdominal distension for three days, a 55-year-old man was brought to the emergency department for treatment. The patient had a fever following an upper respiratory illness 9 days before admission. He had neither a history of anticholinergic prescription use nor recent abdominal surgery. His vital signs upon arrival were as follows: His temperature was 37.8°C, his pulse rate was 92 beats per minute, his respiratory rate was 20 breaths per minute, and his blood pressure was recorded at 151/99 mmHg upon arrival. He had a swollen, non-tender, tympanitic belly and no audible bowel sounds during auscultation. Hepatosplenomegaly or peritoneal irritation signs were absent in the patient. Urinary retention was not noticed. Abdominal ultrasound revealed diffuse abdominal gas distention and a dilated small intestine. On auscultation, active peristalsis was absent.
Three days after abdominal distension, the patient developed ascending weakness in both upper and lower extremities. A neurological evaluation revealed sensory deficiencies (reduced sensation to touch and reduced sensitivity to pain, while vibration and joint position sense was intact) and decreased muscle strength (3/5 both upper and lower extremities based on the MRC scale). The patients’ s deep tendon reflexes were absent in both upper and lower extremities. Plantar reflexes were muted bilaterally. His initial bowel distension was not considered a neurological manifestation; however, the development of symmetrical quadriparesis caught the neurologist’s attention.
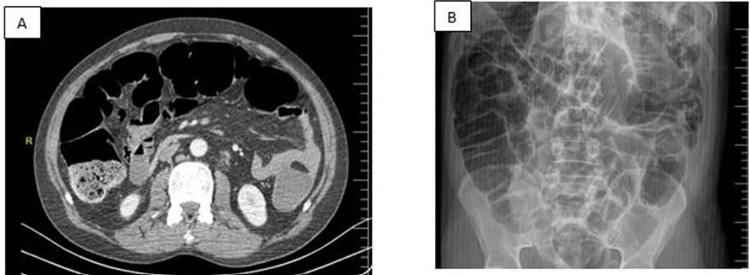
Routine biochemical studies, including serum potassium level (4 mEq/L) and other blood tests, showed no abnormal findings. Magnetic resonance imaging of the brain, cervical, and thoracic spinal cord did not reveal any underlying brain or spinal pathology. Abdominal CT with contrast showed markedly delayed bowel without mechanical obstruction, which suggested paralytic ileus, and no contrast passed through the duodenum during a 6-hour small bowel series examination (see Figure 1). Over the next few days of total parenteral feeding and prokinetic use (metoclopramide 10 mg IV TID), the patient showed persistent severe ileus. A nerve conduction study (done 4 days of symptom onset) demonstrated demyelinating sensorimotor polyneuropathy. Cerebrospinal fluid analysis showed a normal white blood cell count (2 WBC/μL), high protein (819.9 mg/L; reference: 150–450 mg/L), and a glucose level of 55 mg/dl. This showed albumin-cytological dissociation. Based on the clinical presentation, neurophysiologic findings, and CSF findings, we diagnosed him with Guillain-Barre syndrome. Immediate treatment with intravenous immunoglobulin (IVIG) 0.4 g/kg daily for 5 days was initiated. Five days after the onset of motor weakness, the patient’s condition rapidly progressed to involve bilateral facial paralysis (facial diplegia) and dysphagia. In the next few days, the patient developed respiratory failure requiring mechanical ventilation due to diaphragmatic weakness. The patient was transferred to the intensive care unit. After 2 months of intubation in the intensive care unit, the patient passed away due to septicemia. In this case, the patient presented with paralytic ileus as a type of dysautonomia; however, it was not recognized as GBS dysautonomia. The later emergence of motor weakness and sensory disturbances prompted the consideration of GBS.
Figure 1.
(A) Axial view of Abdominal CT with Contrast showing dilated loops without mechanical obstruction. (B) Plain abdominal X-ray showing dilated loops and blunt of abdominal gas. Typical air-fluid levels in the colon and small intestine are seen in the abdomen plain film after a contrast enema, which had been given 1.5 hours prior.
Discussion
Due to its subtle onset, paralytic ileus is an uncommon but troubling presenting symptom of GBS in certain patients. Paralytic ileus is caused by different pathogenic organisms and presents with overlapping clinical characteristics during their initial visit to the emergency room. However, treatment delays and the potential progression to life-threatening events can come from a lack of awareness of this peculiar prodrome of GBS.6 Such conditions might allow bacteria to enter the circulatory system through a damaged gut wall. The treatment of ileus should aim to address the underlying causes of the condition, as well as early enteral feeding and fluid management.6
The afferent fibers from arterial baroreceptors, the efferent parasympathetic fibers that innervate the heart, and the preganglionic sympathetic fibers that regulate pseudomotor and vasomotor functions are thought to be the mechanism, which is an imbalance in sympatho-vagal transmission shifted toward sympathetic predominance.7 Significant fluctuations in blood pressure and/or heart rate, hypo- or hyperthermia, pupil dysfunction, urine retention, and impaired bowel motility are among the early indicators of autonomic dysfunction from GBS. Autonomic instability has been linked to severe weakness, bulbar involvement, and respiratory failure, all of which may require mechanical ventilation.8
Numerous research investigations have documented elevated incidences of autonomic dysfunction (38%), correlated with a mortality risk of 6%. Some individuals with decreased gastrointestinal motility also need a longer stay in the hospital. However, the death rate for individuals with gastrointestinal dysfunction was 6%, while the rate for those without dysautonomia being 0%.9 Despite the fact that some patients do not fully recover after receiving an appropriate IVIG dose, there are many clinical factors that can affect a patient’s outcome, such as when GBS patients initially present with paralytic ileus.10,11
Bowel dysfunction in GBS patients has not yet been adequately treated. Any medicine that may have an impact on blood pressure or heart rate should be used with caution. The management of gastrointestinal paralysis or urinary retention typically requires bladder catheterization, intestinal and stomach decompression, and cautious use of pharmaceutical therapies due to potentially hemodynamic side effects. Since opioids can exacerbate the adynamic ileus, it is recommended to utilize them as seldom as possible.12 This unusual autonomic nervous system is mostly seen in severe cases with advanced stages of the disease, but it is rarely reported as a prior symptom or in mild forms of GBS.13
Paralytic ileus was the first symptom before the first signs of peripheral neuropathy appeared in a case alike to the one described above with a 74-year-old man. For the diagnostic confirmation of paralytic ileus in this previously case, gastric emptying scintigraphy was not used. Similarly, our case was not used for confirmation by gastric emptying scintigraphy.14 The autonomic, gastrointestinal, and respiratory systems are all involved, and the delayed diagnosis of GBS characterizes the history of our patient. Additionally, there was concurrent systemic invasive infection and bacterial translocation that continued to evolve. An unfavorable outlook may result from these factors. One limitation of this case is the lack of availability of antigangliosides, serological markers, and cultures for Campylobacter jejuni, which could help diagnose Guillain-Barré syndrome (GBS) in some cases. It’s important to note that the diagnosis of GBS mainly depends on clinical and electrodiagnostic findings, which include ascending paralysis, lack of reflexes, sensory abnormalities, and NCS/EMG findings.
Conclusion
Although rare, GBS may initially present as a paralytic ileus. Early identification and timely treatment are essential for lowering morbidity and mortality. Our case is instructive and draws the attention of clinicians towards GBS gastrointestinal dysautonomia.
Funding Statement
No particular money from a private, public, or nonprofit organization was given for this study.
Ethical Approval
No ethical approval is required for the publication of case reports from our hospital (Mogadishu Somalia Turkish Training and Research Hospital).
Consent for Publication
Written informed consent was obtained from the Family of the patient for publication of this case report and any accompanying images.
Author Contributions
The work reported has been significantly improved by the contributions of all authors, who participated in the drafting, revising, and critical review of the article, approved the final version to be published, chosen the journal to which the article has been submitted, and agreed to take responsibility for all aspects of the work.
Disclosure
There is no conflict of interest, according to the authors.
References
- 1.Willison HJ, Jacobs BC, van Doorn PA. Guillain-barre syndrome. Lancet. 2016;388(10045):717–727. doi: 10.1016/S0140-6736(16)00339-1 [DOI] [PubMed] [Google Scholar]
- 2.Leonhard SE, Mandarakas MR, Gondim FA, et al. Diagnosis and management of Guillain–Barré syndrome in ten steps. Nat Rev Neurol. 2019;15(11):671–683. doi: 10.1038/s41582-019-0250-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weledji EP. Perspectives on paralytic ileus. Acute Med Surg. 2020;7(1):e573. doi: 10.1002/ams2.573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kehlet H, Holte K. Review of postoperative ileus. Am J Surg. 2001;182(5):S3–10. doi: 10.1016/S0002-9610(01)00781-4 [DOI] [PubMed] [Google Scholar]
- 5.Chakraborty T, Kramer CL, Wijdicks EF, Rabinstein AA. Dysautonomia in Guillain–Barré syndrome: prevalence, clinical spectrum, and outcomes. Neurocritical Care. 2020;32:113–120. doi: 10.1007/s12028-019-00781-w [DOI] [PubMed] [Google Scholar]
- 6.Lee KH, Ho TH, Lee JT, et al. Paralytic ileus as the presenting symptom for Guillain–Barré syndrome: a case report. J Int Med Res. 2020;48(4):0300060519893169. doi: 10.1177/0300060519893169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mohammed J Autonomic (dys) function in patients with chronic obstructive pulmonary disease: evidence and non-pharmacological interventions; 2018.
- 8.Burns TM, Lawn ND, Low PA, Camilleri M, Wijdicks EF. Adynamic ileus in severe Guillain–Barré syndrome. Muscle Nerve. 2001;24(7):963–965. doi: 10.1002/mus.1095 [DOI] [PubMed] [Google Scholar]
- 9.Zaeem Z, Siddiqi ZA, Zochodne DW. Autonomic involvement in Guillain–Barré syndrome: an update. Clin Auton Res. 2019;29:289–299. doi: 10.1007/s10286-018-0542-y [DOI] [PubMed] [Google Scholar]
- 10.Sidow NO, Hassan MS. Intravenous immunoglobulin treatment with prognosis for the first six months of Guillain–Barré syndrome in Somalia: case series. Ann Med Surg. 2022;84:104816. doi: 10.1016/j.amsu.2022.104816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hassan MS, Osman N, Ali B. A young male with an unusual presentation of Guillain-Barré syndrome (GBS) mimicking stroke: a case report. PAMJ Clin Med. 2022;8(4). doi: 10.11604/pamj-cm.2022.8.4.32974 [DOI] [Google Scholar]
- 12.Lichtenfeld P. Autonomic dysfunction in the Guillain-Barré syndrome. Am J Med. 1971;50(6):772–780. doi: 10.1016/0002-9343(71)90185-9 [DOI] [PubMed] [Google Scholar]
- 13.Singh NK, Jaiswal AK, Misra S, Srivastava PK. Assessment of autonomic dysfunction in Guillain‐Barré syndrome and its prognostic implications. Acta Neurol Scand. 1987;75(2):101–105. doi: 10.1111/j.1600-0404.1987.tb07902.x [DOI] [PubMed] [Google Scholar]
- 14.Nowe T, Hüttemann K, Engelhorn T, Schellinger PD, Köhrmann M. Paralytic ileus as a presenting symptom of Guillain-Barré syndrome. J Neurol. 2008;255(5):756. doi: 10.1007/s00415-008-0783-0 [DOI] [PubMed] [Google Scholar]