Abstract
Purpose
To investigate the prevalence of anogenital warts (AGW) caused by human papillomavirus in men and the characteristics and changes of the disease in Korea.
Materials and Methods
From 2007 to 2018, male AGW corresponding to the International Classification of Disease-10 A63.0 were targeted. Through a big data analysis of the Health Insurance Review & Assessment Service, data of patients diagnosed with AGW as either the main or secondary diagnosis were extracted. The overall prevalence and prevalence by age were calculated through the population by year and the population by 5-year-old unit of the National Statistical Office. Additionally, the amount accrued through the disease code was confirmed and compared as AGW-related medical expenses.
Results
The annual number of patients increased by 3.5 times from 32,709 in 2007 to 114,734 in 2018. Additionally, the annual prevalence increased by 3.34 times from 132.83 per 100,000 to 443.57. The age-specific prevalence was the highest among the 25- to 29-year age group. The highest prevalence was observed in the 25- to 29-year age group in 2018 (1,492.15 per 100,000), and the lowest was noted in the 10- to 14-year age group in 2014 (7.28 per 100,000). AGW-related medical expenses increased by approximately 9.76 times from US$ 2,789,215.1 in 2007 to US$ 27,227,254.9 in 2018.
Conclusions
In Korea, cases of male AGW are increasing yearly, with the 25- to 29-year age group having the highest prevalence. Medical costs related to AGW are also increasing tenfold. For male AGW, further studies and national interventions are needed.
Keywords: Condylomata acuminata, Human papillomavirus, Male, Prevalence
Graphical Abstract
INTRODUCTION
AGW are sexually transmitted infections caused by human papillomavirus (HPV) and are the most common HPV-related disease [1]. HPV is a small double-stranded DNA virus, with >220 types; of these, 40 types cause various diseases around the genital area [2]. It causes penile cancer in men, and cervical and vulvar cancers in women, and is closely related to head and neck cancers, AGW, and anal cancer in both men and women [3]. Malignant tumors are caused by high-risk HPV subtypes and low-risk subtypes associated with benign diseases, such as AGW [4,5]. Malignant tumors are caused by HPV, and vaccination against the virus prevents the development of cancer; this has attracted much attention worldwide. Many countries worldwide are making great efforts to combat these cancers in women. Contrarily, HPV infection in men has received relatively little attention, as compared to that in women. The names of the virus and vaccine were initially called “cervical cancer virus” and “cervical cancer vaccine,” respectively. The disease was recognized as being unrelated disease to men, as they have no uterus; therefore, it has been identified as a disease limited to women. For these reasons, there is a lack of interest in HPV-related diseases in men, resulting in a scarcity of related studies. Even in Korea, which has the highest number of HPV-related diseases in men, studies on AGW are few [6,7,8]. However, recently, the number of HPV-related head and neck cancers is higher in men than in women [9], resulting in changes in the U.S. Food and Drug Administration guidelines, including added indications for vaccines.
Cervical or head and neck cancers are the most commonly recognized HPV-related diseases. However, the disease with the highest number of cases induced by HPV is AGW. It occurs mainly in sexually active age groups and is also known as one of the most common sexually transmitted diseases [3]. In foreign countries, relatively many studies on AGW including the prevalence have been conducted. Contrarily, in Korea, epidemiologic studies on AGW or their disease characteristics are scarce. If various disease characteristics, such as prevalence, type of treatment, regional and age-specific characteristics, and cost can be found, then the disease characteristics of domestic AGW can be identified and used for treatment or prevention, or the rationale for male vaccination we can provide data on feasibility. Several cost-effectiveness studies conducted domestically to include boys in the national immunization program (NIP) have shown that the cost-effectiveness of vaccinating females is higher than that of males. However, during the evaluation of epidemiologic studies, there were opinions that the burden of HPV-related diseases in males has been underestimated due to a lack of prevalence studies on HPV-related diseases among men in Korea. Although a nationwide big data analysis study was conducted in 2018 [10], these findings were not fully incorporated into the analysis. In order to establish evidence for male vaccination, as done in other countries, there is a need for more detailed prevalence studies on AGW, which accounts for the largest proportion of HPV cases in men. Therefore, in addition to the study conducted in 2018 by Park et al. [10], there was a recognized need for a more detailed analysis focusing on specific age groups and male patients.
The present study aimed to investigate the prevalence of AGW caused by HPV in men and the characteristics and changes of the disease by analyzing big data on health care in Korea.
MATERIALS AND METHODS
1. Patients
Among the patient data registered in the National Health Insurance Review & Assessment Service (HIRA), men diagnosed with the International Classification of Disease (ICD)-10 code A63.0 anogenital (veneral) wart (AGW) from 2007 to 2018 were targeted. The prevalence and age-specific characteristics, related medical costs, treatment trends and analysis, and regional characteristics were analyzed. The data were extracted from the HIRA big data system, with project number M20200205277.
2. Prevalence (crude and age-specific)
1) Annual crude prevalence
The annual prevalence was analyzed as the number of patients extracted compared to the number of the population in that year. It was calculated based on the number of men among Korean citizens up to December of the year confirmed in the Republic of Korea Census by the National Statistical Office. It was calculated as the number of patients per 100,000 population, analyzed from 2007 to 2018. Additionally, the actual growth rate reflecting the population growth rate during the period was also confirmed.
2) Age-specific prevalence
Due to the nature of the disease, the prevalence by age is also an important indicator. Therefore, the population was divided into 5-year-old units, and the number of patients for each age group was extracted within the study period. Additionally, the prevalence by age was extracted from the number of patients in the relevant population group in the current year as the 5-year-old unit population confirmed through the Republic of Korea census. Moreover, the maximum and minimum values of the prevalence were confirmed.
3. AGW-related medical cost
During the entire period, the medical expenses of patients diagnosed with A63.0 due to the corresponding main disease or injury from the main disease were defined as disease-related expenses. Among the patients with the corresponding diagnosis, patients with 0 won in terms of the amount of treatment were excluded from the analysis. The cost was analyzed by including the entire amount entered in the specific disease, including diagnosis and treatment, as related costs, regardless of the treatment method. The won–dollar exchange rate was converted to the won–dollar exchange rate of 2018, which was the last year of the analysis period, and the exchange rate for that year was 1,100.58 won per dollar (based on data from the National Statistical Office, https://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_2KAA811).
4. Statistical analysis
The data were extracted from the HIRA big data system, with project number M20200205277. Analysis was performed at Wonju data center, and the SAS 9.4 program (SAS Institute) was used for statistical analysis. The data was analyzed using descriptive statistics.
5. Ethics statement
The study protocol was approved by the Institutional Review Board of The Catholic University of Korea (approval number: XC19ZIDI0101).
The requirement for obtaining consent from the research participants was waived as publicly available data were used and no personal information was included in the manuscript and accompanying documents.
RESULTS
1. Annual number of patients and prevalence
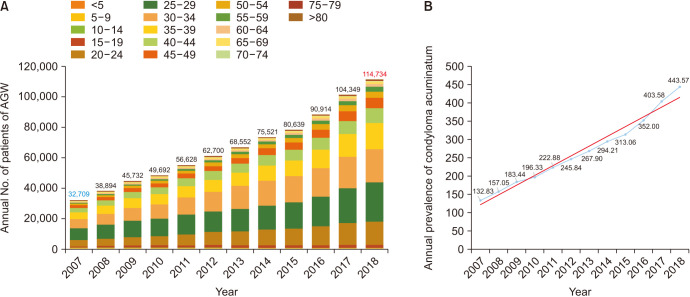
In 2007, the number of male patients diagnosed with AGW was 32,709, which increased steadily yearly; in 2018, it was 114,734, confirming an increase of 351% (Fig. 1A). The number of patients increased by approximately 6,835 per year. During the period, the male population increased by 5% from 24,624,127 to 25,866,129, indicating an actual increase rate of 334%, which confirms a more than threefold increase in patients. During the period, the annual prevalence increased by 334%, from 132.83 cases in 2007 to 443.57 cases in 2018 per 100,000 people (Fig. 1B). Overall, there was a steady increase in the number and prevalence of patients.
Fig. 1. Annual number of patients with and prevalence (per 100,000 person) of anogenital warts (AGW) from 2007 to 2018 (including the 5-year age group). (A) Annual number. The annual number of patients with AGW increased yearly, showing a 351% increase in the number of patients over 10 years. (B) Crude prevalence. In male AGW cases, the prevalence per 100,000 also showed an increase in the number of patients of more than three times.
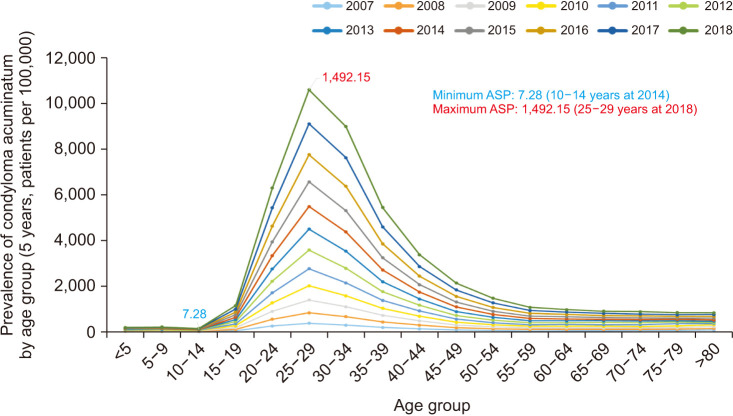
2. Age-specific prevalence
In the 5-year unit analysis, the 25- to 29-year age group had the highest number of patients in all years (Fig. 2). Additionally, starting from the 15- to 19-year age group, visible changes were observed until 50–54 years of age; after 55–59 years, a relatively plateau pattern was observed. Patients aged 15–59 years (red area) account for approximately 70% of the total population, but >93% of the patients and this age group accounts for most of the total number of patients. It can be seen that age is an important factor influencing the occurrence of the disease (Table 1).
Fig. 2. Prevalence of anogenital warts by age group (5 years, patients per 100,000). ASP, age-specific prevalence.
Table 1. Age-specific (sexually active age group) characteristics.
| 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patients | Population | Patients | Population | Patients | Population | Patients | Population | Patients | Population | Patients | Population | Patients | Population | Patients | Population | Patients | Population | Patients | Population | Patients | Population | Patients | Population | ||
| Age group | 32,709 | 24,624,127 | 38,984 | 24,822,897 | 45,732 | 24,929,939 | 49,692 | 25,310,385 | 56,628 | 25,406,934 | 62,700 | 25,504,060 | 68,552 | 25,588,336 | 75,521 | 25,669,296 | 80,639 | 25,758,186 | 90,914 | 25,827,594 | 104,349 | 25,855,919 | 114,734 | 25,866,129 | |
| <5 | 161 | 1,201,209 | 198 | 1,183,217 | 207 | 1,167,689 | 241 | 1,185,537 | 243 | 1,198,629 | 276 | 1,194,460 | 221 | 1,183,212 | 173 | 1,178,326 | 145 | 1,162,807 | 143 | 1,129,953 | 160 | 1,066,180 | 150 | 1,012,380 | |
| 5–9 | 311 | 1,589,915 | 255 | 1,464,571 | 252 | 1,385,903 | 296 | 1,278,040 | 265 | 1,218,866 | 225 | 1,214,863 | 200 | 1,199,677 | 208 | 1,184,754 | 231 | 1,203,174 | 166 | 1,215,209 | 192 | 1,211,669 | 180 | 1,196,477 | |
| 10–14 | 193 | 1,867,106 | 286 | 1,803,423 | 311 | 1,744,514 | 219 | 1,706,007 | 224 | 1,635,253 | 227 | 1,544,170 | 175 | 1,465,338 | 101 | 1,387,285 | 162 | 1,278,769 | 135 | 1,219,887 | 163 | 1,216,208 | 167 | 1,200,639 | |
| 15–19 | 804 | 1,722,229 | 1,153 | 1,804,831 | 1,411 | 1,854,634 | 1,641 | 1,892,719 | 1,567 | 1,882,958 | 1,788 | 1,846,162 | 1,617 | 1,801,265 | 1,764 | 1,743,200 | 1,831 | 1,702,043 | 1,905 | 1,632,122 | 2,112 | 1,541,483 | 2,210 | 1,461,559 | |
| 20–24 | 4,554 | 1,756,562 | 4,952 | 1,648,863 | 5,592 | 1,637,339 | 6,159 | 1,647,287 | 7,369 | 1,688,523 | 8,934 | 1,752,677 | 9,661 | 1,802,320 | 10,840 | 1,852,508 | 11,352 | 1,886,202 | 13,018 | 1,877,127 | 14,742 | 1,840,481 | 15,538 | 1,795,166 | |
| 25–29 | 7,836 | 2,056,125 | 9,491 | 2,079,081 | 11,285 | 1,999,170 | 11,936 | 1,918,337 | 13,482 | 1,811,906 | 13,947 | 1,706,803 | 15,218 | 1,649,886 | 16,147 | 1,638,106 | 17,749 | 1,641,611 | 19,966 | 1,682,988 | 23,651 | 1,747,478 | 26,809 | 1,796,667 | |
| 30–34 | 6,295 | 2,102,838 | 7,407 | 1,994,183 | 8,555 | 1,972,288 | 9,582 | 2,017,088 | 11,698 | 2,053,846 | 13,247 | 2,078,373 | 15,593 | 2,085,473 | 16,968 | 2,004,817 | 17,777 | 1,911,972 | 19,308 | 1,806,754 | 21,328 | 1,702,336 | 22,395 | 1,645,627 | |
| 35–39 | 4,630 | 2,328,233 | 5,493 | 2,326,763 | 6,626 | 2,297,210 | 6,966 | 2,255,652 | 7,537 | 2,157,764 | 8,029 | 2,085,311 | 8,687 | 2,005,223 | 10,182 | 1,980,982 | 10,695 | 2,007,424 | 12,493 | 2,045,265 | 15,372 | 2,070,532 | 17,593 | 2,077,946 | |
| 40–44 | 2,885 | 2,139,080 | 3,552 | 2,183,128 | 4,266 | 2,221,799 | 4,590 | 2,294,124 | 5,374 | 2,341,732 | 6,033 | 2,366,703 | 6,246 | 2,344,220 | 7,087 | 2,311,387 | 7,209 | 2,238,667 | 7,944 | 2,143,639 | 8,777 | 2,072,984 | 10,296 | 1,993,955 | |
| 45–49 | 1,862 | 2,194,686 | 2,196 | 2,227,093 | 2,591 | 2,217,365 | 2,714 | 2,219,528 | 3,107 | 2,176,857 | 3,355 | 2,143,613 | 3,706 | 2,196,548 | 4,630 | 2,232,995 | 4,863 | 2,266,945 | 5,654 | 2,317,182 | 6,581 | 2,343,868 | 7,006 | 2,322,659 | |
| 50–54 | 1,105 | 1,658,052 | 1,309 | 1,829,706 | 1,647 | 1,939,614 | 1,853 | 2,075,192 | 2,080 | 2,175,707 | 2,437 | 2,226,268 | 2,752 | 2,228,829 | 2,794 | 2,217,165 | 3,013 | 2,177,823 | 3,602 | 2,139,711 | 4,202 | 2,109,201 | 4,349 | 2,162,701 | |
| 55–59 | 525 | 1,193,630 | 828 | 1,249,093 | 858 | 1,322,034 | 1,032 | 1,468,249 | 1,117 | 1,598,548 | 1,400 | 1,689,298 | 1,669 | 1,812,276 | 1,832 | 1,920,820 | 2,200 | 2,018,507 | 2,510 | 2,120,391 | 2,765 | 2,172,196 | 3,073 | 2,176,502 | |
| 60–64 | 469 | 938,689 | 598 | 989,786 | 749 | 1,041,371 | 837 | 1,113,044 | 824 | 1,133,757 | 865 | 1,189,791 | 1,035 | 1,216,918 | 1,013 | 1,290,056 | 1,337 | 1,411,839 | 1,559 | 1,540,582 | 1,741 | 1,630,378 | 1,936 | 1,751,203 | |
| 65–69 | 399 | 830,648 | 544 | 879,481 | 570 | 878,816 | 659 | 886,479 | 625 | 886,144 | 825 | 893,794 | 711 | 943,198 | 716 | 994,183 | 749 | 1,050,474 | 981 | 1,072,395 | 1,010 | 1,128,219 | 1,106 | 1,155,935 | |
| 70–74 | 338 | 547,611 | 349 | 606,143 | 379 | 646,459 | 410 | 675,908 | 543 | 713,163 | 646 | 779,224 | 594 | 796,139 | 511 | 800,094 | 658 | 801,927 | 731 | 806,680 | 633 | 820,056 | 879 | 869,294 | |
| 75–79 | 162 | 284,446 | 208 | 319,313 | 222 | 350,568 | 324 | 394,812 | 425 | 433,883 | 327 | 467,062 | 279 | 503,314 | 320 | 540,915 | 324 | 564,174 | 429 | 600,607 | 499 | 662,122 | 607 | 680,342 | |
| >80 | 180 | 213,070 | 165 | 234,222 | 211 | 253,166 | 233 | 282,382 | 148 | 299,398 | 139 | 325,488 | 188 | 354,500 | 235 | 391,704 | 344 | 433,828 | 370 | 477,102 | 421 | 520,528 | 440 | 567,077 | |
| Ratio | 93% | 70% | 93% | 70% | 94% | 70% | 94% | 70% | 94% | 70% | 94% | 70% | 95% | 70% | 96% | 70% | 95% | 69% | 95% | 69% | 95% | 68% | 95% | 67% | |
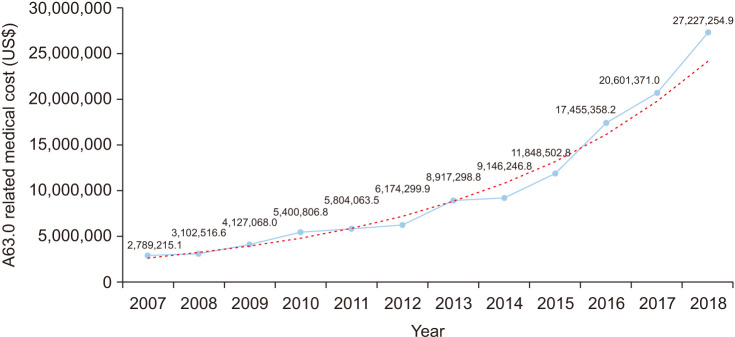
3. AGW-related medical cost
AGW-related medical costs increased from US$ 2,789,215.1 in 2007 to US$ 27,227,254.9 in 2018, showing an increase of 9.76 times (Fig. 3). Regarding the change in cost by age, a decrease of approximately 24% was confirmed in the 0- to 9-year age group, and an increase was observed in all other ages. In the 10-year age group, the increase in medical expenses in their 20s increased the most at 1,238.1%, followed by those in their 50s (1,019.5%) and those in their 30s (899.4%). Finally, the increase in cost was clearly noted even in the elderly population in their 70s (Table 2).
Fig. 3. Anogenital warts-related medical cost.
Table 2. Year-over-year costs and changes by age group in 10-year-old units.
| Age group | 2007 | 2018 | Increase rate (%) |
|---|---|---|---|
| 0–9 | 29,533.6 | 22,381.5 | -24.2 |
| 10–19 | 71,469.9 | 488,608.9 | 583.7 |
| 20–29 | 718,785.7 | 9,618,071.9 | 1,238.1 |
| 30–39 | 948,870.6 | 9,483,377.1 | 899.4 |
| 40–49 | 687,930.4 | 4,981,139.9 | 624.1 |
| 50–59 | 144,761.2 | 1,620,537.9 | 1,019.5 |
| 60–69 | 134,683.6 | 634,777.3 | 371.3 |
| 70–79 | 37,706.7 | 293,499.1 | 678.4 |
| >80 | 15,473.3 | 84,861.2 | 448.4 |
For all costs, the 2018 won-dollar exchange rate of 1,100.58 won per dollar was applied.
DISCUSSION
AGW is among the most common sexually transmitted infections and has the largest number of patients among the HPV-related diseases [1]. However, because it is not caused by high-risk groups such as 16 and 18, which cause malignant tumors, but by low-risk groups, 6 and 11, which are forms that cause benign skin diseases, it was considered a mild, non-life-threatening condition, thereby receiving relatively little attention [11]. In most cases, AGW was treated in clinics by excision, cryotherapy, and electrocauterization under local anesthesia, or by treatment with drugs, such as podophyllin or imiquimod [12]. In fact, most HPV-related diseases are related to cervical cancer; thus, research and policies focusing on women and those on vaccination have been mainly conducted.
Similar to our study findings, the prevalence of AGW is showing a gradual increase. Moreover, age is considered an important factor to consider and is thought to cause more serious problems in cases of HIV infection. In a systematic review, the global incidence of AGW was approximately 194.5 per 100,000, with the incidence being higher in men than in women. As of 2007, the prevalence was slightly lower than that of Spain or Canada, and much lower than that of Mexico or the United States [1]. In addition, there were no studies other than domestic data on continuous prevalence, and furthermore, population-based analysis studies were difficult to confirm. However, based on domestic data, AGW among men in Korea increases very steeply in about 10 years. It can be seen as having greater significance. The peak incidence for women and men is 20–24 years and 25–29 years, respectively, which was consistent with the peak age of men identified in our study. In Korea, the rate of increase was very steep, from approximately 132 to 443 per 100,000 people. Additionally, these diseases peak during the sexually active years, and, in 2018, there were 1,492.15 cases per 100,000 people (1.5 cases per 100 people). Therefore, it is thought that more intensive management, use of condoms, and publicity and notification of diseases should be implemented for this age group.
Additionally, the related cost increased by 9.76 times, which is a very rapid increase in a period of approximately 10 years, thereby increasing the burden. It was reported that the cost of illness in Peru in 2016 was USD 20,000,000 for men and USD 5,000,000 for women. In comparison, in Korea, the cost for men was USD 17,455,358, which was lower than that of Peru in the same year [13].
The number of HPV-related infections, including AGW, in men is increasing, and there are only few approaches to prevent them. In women, many efforts to prevent HPV-related diseases exist, such as early treatment through screening tests, national compulsory vaccination for adolescents, and follow-up vaccination. Further, in cervical cancer cases in Korea, the number of annual cases has been decreasing recently [14]. Moreover, for AGW, as of 2012, the number of cases decreased in women [10]. However, in men, a persistent increase in the number of AGW has been confirmed in some studies, including the present study. HPV-related diseases also showed a steady increase. Due to the characteristics of the disease, screening tests are difficult for men, and confirmation is possible only when the disease occurs; thus, it is practically difficult to confirm whether an asymptomatic person is infectious by contact with urine or skin [15]. In general, visual inspection of the AGW is the only management and no other interventions are recommended. Therefore, screening tests are not recommended [16]. Additionally, the possibility of infection should be mentioned to the current partners of AGW patients. However, there is no need to inform future partners because the remaining period is unknown. It is generally difficult to distinguish recurrence from reinfection, and infection by other genotypes may occur even after the visible wart is treated. Therefore, it may be necessary to monitor the patients to determine if gross lesions will develop even after treatment.
Among the HPV-related diseases, including those presented in this study, several methods are effective in preventing various HPV-related diseases, especially in men, in addition to AGW [17]. However, in the current situation, methods to slow or prevent the increase the prevalence of the disease in Korea are few. Typically, vaccination and circumcision are preventive methods, but there are many difficult parts in the current domestic situation.
HPV vaccines known to be protective against HPV are not included in the NIP for men in Korea. More than 140 countries worldwide have immunization programs for women; 62 of which include immunization for men. Among the countries included in the Organization for Economic Cooperation and Development, only six countries including Korea, which ranks 18th among the top 18 countries by GDP (gross domestic product), provide vaccination to women. This policy reflects that women are vaccinated and the age of adaptation through catch-up vaccination is more economically effective because cost-effectiveness is generally observed. Moreover, to acquire herd immunity, approximately >75% of the total population for female vaccination and >50% for sex-neutral vaccination should be achieved [18]. However, for HPV-related diseases, achieving herd immunity takes a long time, and the current domestic vaccination rate is very far to achieve this. Therefore, vaccination for men also reduces the time required to achieve herd immunity, and men also need vaccination to cope with not only benign diseases as in this study, but also various male diseases, especially head and neck cancers, which are on the rise.
In addition, circumcision reportedly has a preventive effect in various sexually transmitted diseases, including HPV, and it also shortens the period of natural elimination of the virus [19,20,21]. However, the circumcision rate has rapidly decreased in Korea and the procedure is currently hardly implemented. Moreover, for AGW, uncircumcised men with AGW on the penile skin have increased risk of developing urethral condyloma [22].
AGW needs to investigated differently. When the HPV genotype analysis is performed through polymerase chain reaction test for lesions in AGW patients, low-risk types 6 and 11 are confirmed in most cases, but high-risk genotypes are also identified in a relatively larger proportion [8,23]. Although the disease itself is benign, women can be symptomatic and asymptomatic carriers due to coinfection of a high-risk genotype, which is why AGW in men should not be considered as a mere benign disease. Moreover, there is a risk of transmitting a high-risk genotype to women from these men through heterosexual intercourse. This is one of the reasons why HPV vaccination should be included in the NIP even in men.
Our study also has several limitations. First, we could not confirm the recurrence or reinfection rate during the observation period. Second, it was difficult to ascertain the risk rate and location of the lesion according to the characteristics of the patient’s AGW. AGW occurring in the foreskin, urethra, or urethral meatus should be analyzed differently. Third, it was difficult to confirm the characteristics of the disease itself because the individual disease pattern of each patient was not investigated. This may be a common disadvantage of research using big data obtained from a health insurance database. In the future, studies on individual characteristics, such as the circumcision type, number of lesions, presence of recurrence or not, and others are warranted to identify the characteristics of the disease. Fourth, the study showed a significant increase in costs compared to the rise in prevalence. However, since the current research only analyzed the total costs, it did not conduct a detailed analysis to determine whether the increase in costs was due to advancements in diagnostic methods and the resulting increase in testing, or an increase in the cost of treatment itself. Therefore, this study could not identify which factor had a greater impact on the cost increase. Further research on the contributing factors to the cost increase would be necessary, including a detailed cost analysis. Fifth, one of the limitations of big data research is that, in the case of HIRA big data, the analysis relies on diagnoses entered by healthcare providers, which may not perfectly represent the actual number of patients. Although there may be some errors, the data still reflects population-based trends and continuous data, indicating the increasing trend of AGW in male patients.
According to our study data, the prevalence of AGW is rapidly increasing in Korea. However, measures to treat this disease are few. Thus, more research on the disease is needed along with national interest. Although circumcision does not easily address this problem due to cultural and social factors, it can have a positive effect on disease prevention along with other preventive efforts such as vaccination and inclusion of men in the NIP.
Considering the nature of the disease, especially as a sexually transmitted infection, the disease itself is significant, but the social burden it imposes and its impact on public health policies are equally important. Therefore, beyond treating the disease itself, there is a need for policy approaches that include awareness, education, and prevention. It is true that policies have primarily focused on women because HPV is known to cause cervical cancer in women. However, during the period when attention to HPV-related diseases in men was lacking, we observed a notable increase in HPV-related head and neck cancers and a sharp rise in AGW among men. While HPV is associated with diseases in women, it is also a significant health, policy, and public health issue for men. Recognizing this, it is essential for the community to work together to address it. This effort should include education, awareness, prevention, policy incorporation, and changes in perception. The need for male vaccination has become increasingly evident.
CONCLUSIONS
The prevalence of AGW in men is rapidly increasing yearly and it increased by more than 3 times, with the highest prevalence observed among those aged 25–29 years in Korea. Medical costs related to the diseases are also increasing tenfold. It is necessary to develop measures targeting men aged 25–29 years, where the incidence is highest, and to adopt policy, educational, and preventive approaches, including the introduction of the NIP for boys, to address the increase in AGW among males.
ACKNOWLEDGMENTS
We would like to thank everyone who has contributed to our research and investigations related to HPV. We would also like to thank professors Jee Hyun Kong, Garam Lee, Jun Young Lee, and Tae Hoon Kong researchers at Wonju Yonsei University for their efforts in statistical analysis. In addition, I would like to thank professors Jae Hung Jung and Tae Wook Kang, and professors Dong Kyun Kim and Kyoung Su Sung, who gave me a lot of advice during the research. We would also like to thank the Korean Association of Urogenital Tract Infection and Inflammation members who played a major role in HPV-related research.
Footnotes
CONFLICTS OF INTEREST: The authors have nothing to disclose.
FUNDING: This study was supported by the Foundation for Korean Urological Association in 2019 (FKUA-2019-001).
- Research conception and design: Sangrak Bae and Seung-Ju Lee.
- Data acquisition: Sangrak Bae and Hong Chung.
- Statistical analysis: Sooyoun Kim, Sangrak Bae, and Jin Bong Choi.
- Data analysis and interpretation: Hong Chung, Seung-Ju Lee, and Sangrak Bae.
- Drafting of the manuscript: Hong Chung and Sangrak Bae.
- Critical revision of the manuscript: Sangrak Bae and Seung-Ju Lee.
- Obtaining funding: Sangrak Bae and Seung-Ju Lee.
- Administrative, technical, or material support: Sooyoun Kim and Jin Bong Choi.
- Supervision: Seung-Ju Lee and Sangrak Bae.
- Approval of the final manuscript: all authors.
References
- 1.Patel H, Wagner M, Singhal P, Kothari S. Systematic review of the incidence and prevalence of genital warts. BMC Infect Dis. 2013;13:39. doi: 10.1186/1471-2334-13-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Smola S. Human papillomaviruses and skin cancer. Adv Exp Med Biol. 2020;1268:195–209. doi: 10.1007/978-3-030-46227-7_10. [DOI] [PubMed] [Google Scholar]
- 3.de Sanjosé S, Brotons M, Pavón MA. The natural history of human papillomavirus infection. Best Pract Res Clin Obstet Gynaecol. 2018;47:2–13. doi: 10.1016/j.bpobgyn.2017.08.015. [DOI] [PubMed] [Google Scholar]
- 4.Brown B, Poteat T, Marg L, Galea JT. Human papillomavirus-related cancer surveillance, prevention, and screening among transgender men and women: neglected populations at high risk. LGBT Health. 2017;4:315–319. doi: 10.1089/lgbt.2016.0142. [DOI] [PubMed] [Google Scholar]
- 5.Schiffman M, Doorbar J, Wentzensen N, de Sanjosé S, Fakhry C, Monk BJ, et al. Carcinogenic human papillomavirus infection. Nat Rev Dis Primers. 2016;2:16086. doi: 10.1038/nrdp.2016.86. [DOI] [PubMed] [Google Scholar]
- 6.Lee CB, Choe HS, Hwang SJ, Lee SJ, Cho YH. Epidemiological characteristics of genital herpes and condyloma acuminata in patients presenting to urologic and gynecologic clinics in Korea. J Infect Chemother. 2011;17:351–357. doi: 10.1007/s10156-010-0122-0. [DOI] [PubMed] [Google Scholar]
- 7.Kwon T, Moon KH, Yang SH, Roh MC, Lee SH, Kim JW, et al. Multiple human papillomavirus infection is associated with high-risk infection in male genital warts in Ulsan, Korea. J Korean Med Sci. 2016;31:371–375. doi: 10.3346/jkms.2016.31.3.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Park SJ, Seo J, Ha SH, Jung GW. Prevalence and determinants of high-risk human papillomavirus infection in male genital warts. Korean J Urol. 2014;55:207–212. doi: 10.4111/kju.2014.55.3.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Villa A, Patton LL, Giuliano AR, Estrich CG, Pahlke SC, O’Brien KK, et al. Summary of the evidence on the safety, efficacy, and effectiveness of human papillomavirus vaccines: umbrella review of systematic reviews. J Am Dent Assoc. 2020;151:245–254.e24. doi: 10.1016/j.adaj.2019.10.010. [DOI] [PubMed] [Google Scholar]
- 10.Park YJ, Kim JM, Lee BR, Kim TH, Lee EG. Annual prevalence and economic burden of genital warts in Korea: Health Insurance Review and Assessment (HIRA) service data from 2007 to 2015. Epidemiol Infect. 2018;146:177–186. doi: 10.1017/S0950268817002813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Egawa N, Doorbar J. The low-risk papillomaviruses. Virus Res. 2017;231:119–127. doi: 10.1016/j.virusres.2016.12.017. [DOI] [PubMed] [Google Scholar]
- 12.Yuan J, Ni G, Wang T, Mounsey K, Cavezza S, Pan X, et al. Genital warts treatment: beyond imiquimod. Hum Vaccin Immunother. 2018;14:1815–1819. doi: 10.1080/21645515.2018.1445947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Saldarriaga EM, Cárcamo CP, Babigumira JB, García PJ. The annual costs of treating genital warts in the Public Healthcare Sector in Peru. BMC Health Serv Res. 2021;21:1092. doi: 10.1186/s12913-021-07120-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim J, Lee D, Son KB, Bae S. The burden of cervical cancer in Korea: a population-based study. Int J Environ Res Public Health. 2020;17:6308. doi: 10.3390/ijerph17176308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.D’Hauwers KW, Tjalma WA. Screening for human papillomavirus: is urine useful? Indian J Cancer. 2009;46:190–193. doi: 10.4103/0019-509X.52952. [DOI] [PubMed] [Google Scholar]
- 16.Workowski KA, Bachmann LH, Chan PA, Johnston CM, Muzny CA, Park I, et al. Sexually transmitted infections treatment guidelines, 2021. MMWR Recomm Rep. 2021;70:1–187. doi: 10.15585/mmwr.rr7004a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chelimo C, Wouldes TA, Cameron LD, Elwood JM. Risk factors for and prevention of human papillomaviruses (HPV), genital warts and cervical cancer. J Infect. 2013;66:207–217. doi: 10.1016/j.jinf.2012.10.024. [DOI] [PubMed] [Google Scholar]
- 18.Ng SS, Hutubessy R, Chaiyakunapruk N. Systematic review of cost-effectiveness studies of human papillomavirus (HPV) vaccination: 9-Valent vaccine, gender-neutral and multiple age cohort vaccination. Vaccine. 2018;36:2529–2544. doi: 10.1016/j.vaccine.2018.03.024. [DOI] [PubMed] [Google Scholar]
- 19.Smith JS, Backes DM, Hudgens MG, Mei W, Chakraborty H, Rohner E, et al. Male circumcision reduces penile HPV incidence and persistence: a randomized controlled trial in Kenya. Cancer Epidemiol Biomarkers Prev. 2021;30:1139–1148. doi: 10.1158/1055-9965.EPI-20-1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Friedman B, Khoury J, Petersiel N, Yahalomi T, Paul M, Neuberger A. Pros and cons of circumcision: an evidence-based overview. Clin Microbiol Infect. 2016;22:768–774. doi: 10.1016/j.cmi.2016.07.030. [DOI] [PubMed] [Google Scholar]
- 21.Mehta KS, Marfatia YS, Jain AP, Shah DJ, Baxi DS. Male circumcision and sexually transmitted infections: an update. Indian J Sex Transm Dis AIDS. 2021;42:1–6. doi: 10.4103/ijstd.ijstd_20_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Park JK, Shin YS. Risk factors for urethral condyloma among heterosexual young male patients with condyloma acuminatum of penile skin. Infect Chemother. 2016;48:216–218. doi: 10.3947/ic.2016.48.3.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ryu KH, Cho JH, Lee MC, Jung TY. Type distribution of human papillomavirus in genital warts of Korean men. Urogenit Tract Infect. 2017;12:89–94. [Google Scholar]