Abstract
Background:
Charles Bonnet syndrome (CBS) refers to the presence of visual hallucinations experienced by people, without cognitive, or psychiatric deficits that are related to sight loss. This study surveyed younger adults (18–60 years) with visual impairments, to assess the impact of anxiety, depression, loneliness, and the COVID-19 lockdowns on their visual hallucinations.
Objectives:
To examine the association between depression, anxiety, loneliness, the COVID-19 lockdowns, and visual hallucinations in younger adults with CBS.
Design:
An online survey was used with an opportunistic sample of people with sight loss.
Methods:
A survey assessed the frequency, duration, and valence of visual hallucinations using a five-point Likert scale, and assessed anxiety, depression, and loneliness using the Hospital Anxiety and Depression Scale and UCLA (University of California, Los Angeles) loneliness scale, respectively.
Results:
Twenty-nine young adults (21 female), aged 22–59 years with vision loss from a range of causes, who experience visual hallucinations, were included in the survey. The majority (76%) of participants had experienced hallucinations within the past week, with 83% stating they occurred frequently or very frequently. For 59% of participants, the hallucinations were of short duration (<2 min), but 34% experienced them continuously. Hallucinations were regarded as being unpleasant by 34% of participants, while 59% rated them as being neutral. The incidence of depression and anxiety was high in the sample (48% and 65%, respectively), and 65% experienced loneliness. Participants with scores indicating anxiety or borderline anxiety had significantly more frequent hallucinations than other participants and a similar trend was found for depression. The COVID-19 lockdowns exacerbated hallucinations in 24% of cases, but for 68% they remained unchanged.
Conclusion:
The study demonstrated that CBS is observed in people of all ages, with sight loss arising from a wide range of underlying causes. Depression, anxiety, and loneliness are observed in many cases of CBS. While there was some indication that high anxiety, and to some extent depression, was associated with frequent hallucinations, no other relationships were found between the psychosocial factors (depression, anxiety, and loneliness) and the frequency, duration, or valence of their visual hallucinations.
Keywords: anxiety, Charles Bonnet syndrome, depression, loneliness, visual hallucinations
Introduction
The presence of visual hallucinations following vision loss was first described by Charles Bonnet in the 1760s and is now referred to as Charles Bonnet syndrome (CBS).1,2 CBS has been associated with a range of ocular pathologies, most commonly age-related macular degeneration, diabetic retinopathy, glaucoma, corneal disease, and cataracts,3,4 and also with visual impairments arising from deafferentation of the visual cortex.3,5 The prevalence of CBS observed in ophthalmology patients is thought to be around 11%–20%,6,7 although estimates vary from as low as 0.4% in a study of Asian ophthalmology patients 8 to 27% in an Australian study. 9 Age is often associated with CBS, but eye diseases, such as macular degeneration and cataracts, are themselves age-related and poor visual acuity is the key risk factor for developing CBS. 9 Furthermore, as age-related eye diseases (macular degeneration, cataracts, etc.) are the most common cause of CBS many studies have naturally tended to focus on studies of older-age patients. There are, however, reports of hallucinations in younger-age adults 10 and children11,12 following vision loss.
A distinction can be made between the purely visual hallucinations associated with sight loss (Charles Bonnet syndrome, or CBS) and the hallucinations associated with neurological and psychiatric conditions such as Parkinson’s Disease, Alzheimer’s disease, Lewy-body dementia, and Schizophrenia. 2 The visual hallucinations associated with eye disease (CBS), lack any auditory component, and range from simple flashes, lines, dots, colors, grid-like patterns, networks and lattices (tessellopsia ), as well as more complex percepts, including faces (distorted and gargoyle like), people in bizarre costumes often with hats and landscapes. Faces and figures of a person have been found to be the most common ‘object’ hallucinated. 13
Santhouse et al. 14 examined the content of the visual hallucinations experienced in 34 cases of CBS and revealed 28 different categories. A factor analysis found that 12 of these experiences could be grouped broadly into three categories: (a) figures including with hats and costumes, children and small figures and landscapes; (b) faces, grotesque and distorted faces, cartoon and sketch-like faces; (c) simple flashes, after-images (palinopsia). The different visual phenomena were attributed to activity in specialized regions of the visual cortex that are regarded as forming a hierarchy for processing low-level and higher-level visual attributes.2,14,15 The content of hallucinations typically varies both within and between individuals. There are also individual differences in terms of the frequency of occurrence, how long hallucinations last, and the subjective impact that they have on the person.13,16 The majority of people report hallucinations occurring frequently (weekly/daily – Schultz et al., 13 ), while others report them infrequently (every few weeks or monthly) with frequency diminishing with time. 2 The duration of hallucinations is typically brief lasting for seconds to minutes, 13 but in some cases they occur for hours or continuously. 2
Psychological and social factors have been thought to contribute to the severity and perceived impact of the visual hallucinations in CBS (for a review see Jones et al. 11 ). Contributory factors include depression16,17 and anxiety, 3 although it is not clear if this is due to the negative impact of the hallucinations, or the high incidence of depression and anxiety in the visually impaired.18–20 Although some people with CBS regard their hallucinations as being unpleasant the majority do not,9,21 with factors such as the duration and frequency of hallucinations, although not age, gender, or their content, are thought to contribute to the subjective experience of hallucinations. 21 A lack of social support22–24 and loneliness3,24,25 are also factors that may contribute to the symptoms of CBS, although it has been noted that the quality of social interactions and loneliness are potentially more important than the quantity of social support per se. 25 Loneliness is one factor that is thought to have led to an increase in the perceived negative impact of hallucinations during the COVID-19 lockdowns, elderly people being more susceptible due to reduced social support. 11
Much of the literature on CBS has tended to focus on older adults as they are more likely to have ocular conditions, but aging naturally increases the presence of additional confounding factors such as cognitive and neurological impairments as well as additional psychosocial risk factors. The present study focused on surveying CBS in younger adults (age 18–60 years), with sight loss arising from any underlying cause, and examining the potential contributions of depression, anxiety, and loneliness to their symptoms. A modified version of the hallucination questionnaire developed by Santhouse et al. 14 was used to assess the frequency and duration of their hallucinations, the emotional effect (valence) of their hallucinations, and if their symptoms increased during the COVID-19 lockdowns. The Hospital Anxiety and Depression Scale (HADS 26 ) and the UCLA Loneliness scale 27 were used to examine the contribution of psychosocial factors. The survey was administered using the Qualtrics online platform (Qualtrics, Provo, UT, USA). The aim was to examine the prevalence of depression, anxiety, and loneliness in younger-age adults with vision loss and CBS and to see if the frequency, severity, and valence of their hallucinations were related to these factors. The subjective impact of the COVID-19 lockdowns on symptoms was also examined.
Methods
Ethical approval
Ethics approval was obtained from the Royal Holloway Department of Psychology Ethics Committee and the study was conducted in adherence to the tenets of the Declaration of Helsinki. Informed consent was obtained electronically.
Study design and sample
The study inclusion criteria were adults aged from 18 to 60 years with a visual deficit of any underlying origin, who are registered as blind, and who experience visual hallucinations without an auditory component. The exclusion criteria were a history of stroke or epilepsy, a psychiatric or neurological disorder, or the experienced visual hallucinations being associated with dizziness, strange smells, or other unusual sensations. The recruitment strategy aimed to recruit visually impaired individuals who experienced CBS and targeted members of organizations, including the Macular Society UK, the Royal National Institute of Blind People, Esme’s Umbrella (a charity specifically for people with CBS), and Facebook groups for people with vision loss. The messaging used included the following statement that specifically mentioned hallucinations and CBS: ‘We are carrying out a study on the effect of anxiety, depression, and loneliness on the severity of visual hallucinations in people with visual impairments (a condition known as Charles Bonnet syndrome).’
The survey was constructed and administered using Qualtrics (Qualtrics, Provo, UT, USA) and was open to people including those outside the UK. Information was collected regarding the participants’ age, gender, and details of their visual impairment, including when it was acquired. Participants were also asked to state if they had a past history of stroke, psychiatric illness, or epilepsy if they experienced visual hallucinations, and if so, if they were associated with sounds or talking, dizziness, smells, or other strange sensations. The Hospital Anxiety and Depression Scale (HADS) and UCLA inventories were used (with permission) to assess anxiety, depression, and loneliness, respectively. The participants’ experience of hallucinations was probed via the following questions, all of which required responses to be made on a five-point Likert scale: (a) How long ago was your last hallucination? (1 – A year ago or longer, 2 – over a month ago, 3 – within the last month, 4 – within the last week, 5 – today); (b) How often do they occur? (1 – Very rare, 2 – rarely, 3 – occasionally, 4 – frequently, 5 – very frequently or always present); (c) How long do they last? (1 – Under a minute, 2 – several minutes, 3 – one or several hours, 4 – one or several days, 5 – they are always present); (d) Are they pleasant or unpleasant? (1 – Very pleasant, 2 – pleasant, 3 – neutral, 4 – unpleasant, 5 – very unpleasant). A final question asked them about their hallucinations during the COVID-19 lockdowns (1 – They decreased a lot 2 – they decreased a bit 3 – they stayed the same 4 – they increased a bit 5 – they increased a lot). The study was conducted between October 2021 and March 2022.
Results
Participants
Of the initial 58 responses, 23 were excluded from further analysis because the participants had completed an insufficient number of the survey questions. Participants were also excluded (n = 6) if they stated that they did not experience hallucinations if their hallucinations included an auditory component, dizziness, or smells, or if they reported a history of a psychiatric disorder or epilepsy. The remaining 29 participants (21 female) had an average age of 44 years (range 22–59 years). A summary of the average scores for the group on the hallucination experience questions (frequency, duration, and valence of hallucinations, and impact of the Covid-19 lockdowns), the HADS anxiety and depression scales, and the UCLA loneliness scale are shown in Table 1. The range of eye conditions reported by participants (where stated) are shown in Table 2.
Table 1.
Mean, or median scores (Standard Deviation in parenthesis), and range for the group of (N = 29) participants for age; number of years since first experienced hallucinations; score for each of the hallucination experience questions; anxiety and depression scores from the HADS, and score from the UCLA loneliness scale.
| Questionnaire | Mean (M) or Median (Mdn) and (SD) | Range |
|---|---|---|
| Age | M – 43.75 years (11.70) | 22–59 |
| Number of years since first experienced hallucinations? | M – 5.23 (7.63) | 1–38 |
| When was your last vision? (1 = over a year, 5 = today) | Mdn – 4.00 (1.23) | 1–5 |
| How often do they occur? (1 = very rarely, 5 = very frequently) | Mdn – 5.00 (1.18) | 1–5 |
| How long do they typically last? (1 = under a minute, 5 = always present) | Mdn – 2.00 (1.66) | 1–5 |
| Are they pleasant, or unpleasant? (1 = very pleasant, 5 = very unpleasant) | Mdn – 3.00 (0.81) | 1–5 |
| Did your hallucinations worsen during the COVID-19 pandemic lockdown? (1 = decreased a lot, 5 = increased a lot) | Mdn – 3.00 (0.76) | 2–5 |
| HADS depression scale (0–7 normal range) | M – 7.76 (5.65) | 0–20 |
| HADS anxiety scale (0–7 normal range) | M – 9.86 (5.43) | 0–19 |
| UCLA loneliness scale | M – 54.00 (13.78) | 22–75 |
HADS, Hospital Anxiety and Depression Scale.
Table 2.
Self-reported eye condition (where stated) and number of cases reporting each condition.
| Eye condition | Number of cases |
|---|---|
| Accident, retinal detachment, or damage | 5 |
| Myopic macular degeneration | 1 |
| Macular dystrophy (Stargardt’s disease) | 1 |
| Leber’s hereditary optic neuropathy | 1 |
| Retinal dystrophy | 1 |
| Diabetic, or hypertensive retinopathy | 3 |
| Retinal dystrophy (Cone-Rod) | 1 |
| Retinal dystrophy (Retinitis pigmentosa) | 3 |
| Glaucoma | 1 |
| Congenital glaucoma | 1 |
| Closed-angle glaucoma/Retinopathy | 1 |
| Congenital cataracts | 1 |
| Cataracts + optic nerve damage | 1 |
| Not specified | 8 |
There was a bias for the female gender with 21 females and 8 males who met the inclusion criteria. The underlying causes of the participants’ visual impairments (where stated) were varied (see Table 2) and included accidents, cataracts, glaucoma and congenital and hereditary eye conditions such as macular, retinal, and diabetic retinopathy, cataracts and glaucoma. The average age of participants was 43.75 years with almost half (44%) under the age of 40 years, and one-third aged 50–60 years. The average number of years since participants first experienced visual hallucinations was reported as just over 5 years, although four cases had experienced hallucinations for more than 10 years and one person (aged 50 years) first hallucinated as a child 38 years ago. When mentioned, their hallucinations typically started in the first 1–2 years following their vision loss.
The hallucination questions revealed that 22 participants (76%) had experienced hallucinations within the last day, or week, 4 people stated within the past month or more, and 3 who had not experienced a hallucination for over a year. Some 24 participants (88%) stated that they experienced hallucinations frequently or very frequently, with only 3 people experiencing them rarely or very rarely. The duration of hallucinations experienced by 17 participants (59%) was brief, lasting for several minutes or less than a minute, but 10 (35%) stated that they were always present. The valence of hallucinations showed that only 2 participants (7%) rated their hallucinations as being pleasant or very pleasant, while 10 (34%) regarded them as being unpleasant or very unpleasant, and the remaining 17 participants (59%) rated them as being neutral. The responses to the question ‘Did your hallucinations worsen during the COVID-19 lockdowns?’ (average score = 3.29) revealed that 7 people thought their CBS had worsened, while 19 stated there had been no change, and for 2 people their symptoms improved. A negative correlation was observed between the ratings for the influence of the COVID-19 lockdowns on CBS and the number of years since first experiencing hallucinations (Spearman’s Rank correlation r(28) = −0.42, p < .05)). Thus, people who had experienced hallucinations for a longer period appeared to be less impacted by the effects of the COVID-19 lockdowns. Reports of a negative emotional impact of hallucinations were correlated with how frequently the hallucinations occurred (Spearman’s Rank correlation r(28) = 0.47, p < .01)), with more frequent episodes being related to them being regarded as being more unpleasant.
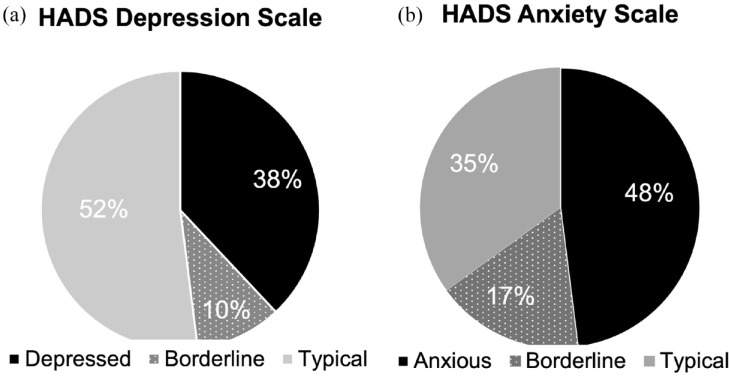
The mean score from the HADs depression scale was 7.76, with 38% of participants falling into the range for depression and a further 10% being borderline depressed (Figure 1(a)). The mean score on the anxiety scale was 9.86, with 48% of participants being classed as anxious and a further 17% as borderline anxious (Figure 1(b)). Thus half of the participants had indications of depression and two-thirds for anxiety, with these two measures being significantly correlated (r(28) = 0.72, p < 0.001). Spearman’s rank correlations revealed a significant negative correlation between the participant’s age and anxiety (r(28) = −0.46, p < 0.05) with younger participants scoring more highly on the anxiety scale. The average score on the UCLA loneliness scale was 54, with 66% of participants being 1SD over the mean scores of students and nurses reported by Russell (1996) and 45% having scores 2SD above the mean of students and nurses. There was a significant correlation between anxiety and loneliness (Spearman’s Rank r(28) = 0.55, p < 0.001)) and also between depression and loneliness (Spearman’s Rank r(28) = 0.65, p < 0.001)). The measures of depression, anxiety, and loneliness were not correlated with either the frequency, duration, or valence of hallucinations.
Figure 1.
(a) Percentage of participants who would be classed as being depressed, borderline depressed, or within the normal range from the HADS depression scale. (b) Percentage of participants who would be classed as being anxious, borderline anxious, or within the normal range from the HADS anxiety scale.
HADS, Hospital Anxiety and Depression Scale.
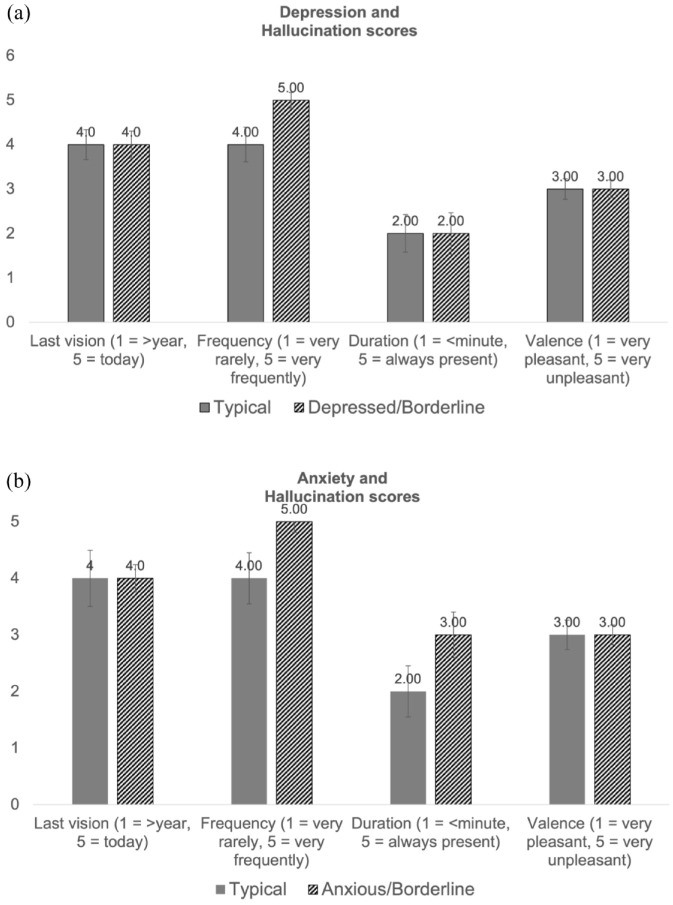
Depression and Anxiety and the Hallucinations
The relationship between depression and anxiety on the main hallucination measures of interest was further examined by splitting the data in terms of participants who scored in the normal or typical range and those in the abnormal or borderline range on the HADS depression and anxiety scales. For depression 15 participants obtained a score of 7 or lower (normal or typical) and the remaining 14 participants scored higher than 7 (depressed or borderline depressed). The mean scores for these two groups on the main hallucination measures are shown in Figure 2(a). For the anxiety scale, 10 participants were in the normal-typical range and 19 were anxious or borderline anxious and the mean scores on the hallucination measures for these two groups are shown in Figure 2(b).
Figure 2.
(a) Mean scores on the hallucination measures for participants who scored in the normal/typical, or abnormal range on HADS depression scale (error bars indicate standard error). (b) Mean scores on the hallucination measures for participants who scored in the normal/typical, or abnormal range on HADS anxiety scale (error bars indicate standard error).
HADS, Hospital Anxiety and Depression Scale.
Figure 2(a) shows the mean scores on the hallucination questions split in terms of participants who were classed as being in the typical or normal range (n = 15) and those who were depressed or borderline depressed (n = 14) using the cut-off scores for the HADS depression scale. The mean hallucination scores appear to be broadly comparable for the depressed and typical groups of participants. The frequency of hallucinations was higher for depressed/borderline individuals (Mdn = 5.00) than those in the typical range (Mdn = 4.00), but this difference was not statistically significant (Mann–Whitney U(79), p = 0.217 two-tailed). The variance of the frequency scores was lower in the depressed than the typical group (standard deviation = 0.65 and 1.46, respectively). An F-test comparing the variance of the frequency of hallucinations in the two groups was significant (F(15, 14) = 5.08, p(one-tailed) = 0.002). This indicates that the depressed participants had consistently more hallucinations than those in the normal range who showed more variability in the frequency of hallucinations.
Anxiety and hallucinations
Figure 2b shows the scores on the mean hallucination questions split in terms of participants who were classed as being in the typical or borderline range (n = 10) and those who were anxious or borderline anxious (n = 19). The frequency of hallucinations is higher for the anxious group (Mdn = 5.00) than typical group (Mdn = 4.00, SD–0.84), a difference that was statistically significant (Mann–Whitney U,43 p = 0.009 two-tailed). None of the other measures were found to be significantly different compared between the anxious and typical groups. The variance of the frequency of hallucinations was lower in the anxious compared to the typical group (standard deviation = 0.84 and 1.43, respectively), which an F-test showed was significant (F(9,18) = 2.93, p(one-tailed) = 0.024). Thus, participants who were outside the typical range on the anxiety scale more consistently reported a greater frequency of hallucinations than those in the typical range.
Discussion
The findings from the present survey confirm that visual hallucinations (CBS) are observed in younger-age adults with a bilateral loss of vision resulting from a wide range of underlying causes.3,4 The presence of CBS in younger adults here included three participants who reported first experiencing hallucinations in their teens (ages 12–17 years), which is consistent with other reports of hallucinations in young people and children.10,12 The tendency to associate CBS with aging 4 may be attributed to the greater incidence of eye diseases in the elderly rather than age itself being a risk factor.2,3,9,28 Poor visual acuity, irrespective of the eye condition that caused their vision loss appears to be the main causal factor in developing visual hallucinations.4,6,9,29,30
A much higher proportion of female than male participants responded to this survey, which is consistent with other reports of an apparent gender bias in CBS, although the reasons for this apparent bias are not clear.4,24,28,30 A meta-analysis of glaucoma patients 30 reported female gender, along with high age, reduced contrast sensitivity and not living alone as risk factors for CBS. An evaluation of Canadian patients, attending a low-vision clinic, also noted a higher prevalence of CBS in females than males, but this was attributed to a reluctance of males to report hallucinations rather than any physiological or genetic difference. 6 This apparent gender bias was not found in a retrospective case study of children and younger people from the case reports of patients attending the Moorfields Eye Hospital (UK) that identified hallucinations in nine male and four female patients. 10 The higher ratio of females to males in the present study most likely reflects a greater willingness for females to engage with a study that relates to sensitive personal experiences rather than reflecting a gender bias in risk of CBS, but it remains possible that other risk factors could contribute to this bias.
In the present study over half of the participants reported experiencing visual hallucinations for 3–4 years, but some had experienced hallucinations for around 10 years, and one for as long as 38 years. Most participants stated they had experienced hallucinations – within the last day or week (76%) and that their hallucinations occurred frequently or very frequently (88%). Only three people reported not having experienced a hallucination for a year or more, or that they rarely occurred. This high frequency of hallucinations in this study is comparable with the findings of Schultz et al. 13 and Cox and ffytche. 21 The duration of hallucinations reported was bimodal, with just over half of the participants stating that they were short-lasting (minutes or less), but a third of people stated that they were always present. Over half of the participants rated their hallucinations as being of neutral valence, with a third regarding them as being unpleasant or very unpleasant, and only a small minority regarded them as being pleasant. There was an association between how pleasant/unpleasant people regarded their hallucinations and how frequently they occurred with participants experiencing more frequent hallucinations reporting these as less pleasant.
The sample of younger adults in the present study revealed a high proportion scoring highly on scales of depression, anxiety, and loneliness. Depression was observed in 38% of participants with a further 10% being borderline depressed. Depression is known to be higher in people with visual impairment (VI) than in those without vision loss, but the sample of younger adults surveyed here is higher than in other studies. Evans et al. 20 reported that 13% of older adults (over 75 years) with VI, attending a GP health screening clinic were depressed, compared to 4% of those without VI. 20 Rovner et al. 31 found that 33% of newly diagnosed cases of age-related macular degeneration were depressed, which was higher than observed in people diagnosed with other diseases (16% depressed). A Norwegian study found that some 15%–20% of younger adults (age 18–50 years) with VI were depressed, 32 which is lower than for the young adults in the present study. There was no relationship between depression and the measures of visual hallucinations, except for a correlation with reports of CBS worsening during the COVID-19 lockdowns and a potential relationship with the frequency of hallucinations. Thus, depression is not associated with the severity of hallucinations experienced in CBS, consistent with the numerous cases who are not depressed,3,16 but it may interact with other psychosocial factors (including anxiety, loneliness, and social isolation) to exacerbate the subjective impact the hallucinations have on the individual. 11
Some 65% of participants scored highly on the anxiety scale, which is consistent with reports of high levels of anxiety in people with CBS.3,33 There was a correlation between age and anxiety with the younger participants scoring more highly on the anxiety scale. Anxiety and loneliness are both correlated with depression. Anxiety was related to more frequent hallucinations but was not related to the other hallucination measures. The direction of the relationship between anxiety and frequency of hallucinations is unclear with it being possible that frequent hallucinations may increase anxiety of those experiencing them, while also possible that high anxiety could result in more frequent hallucinations. Loneliness appeared not to be related to any of the hallucination measures. Neither anxiety nor loneliness were related to a worsening of symptoms during the COVID-19 lockdowns. The majority of participants stated that their hallucinations had not changed during the lockdowns (e.g. ‘I was with my wife and children during covid so I saw no difference’; ‘No different from any other time’; ‘It was okay’; ‘No difference’), but seven participants reported that their CBS had worsened during the COVID-19 lockdowns (e.g. ‘During the pandemic I believe that my hallucinations started. I didn’t have them before and I noticed halfway through that I started to get vivid lights in my eyes which I had never seen before’; ‘My flashing lights increased at times they wouldn’t normally happen, I’ve had a great deal more fly/spider/bug like visual hallucinations than before’; ‘They started during lockdown. I have never had any before. I kept getting bright lights similar to spotlights in my face’), although in one case this was attributed to changes in their vision (e.g. ‘I lost a bunch of vision during the pandemic and this triggered the CBS symptoms. I don’t think it was related to lockdown it was related to the vision loss’). This is consistent with the report from Jones et al. 34 who found an increase in the frequency of hallucinations in some cases of CBS that may reflect wider psychosocial factors such as loneliness (see Teunisse et al. 25 ) and other environmental triggers, but similar to the findings from the present study loneliness was not associated with the frequency or emotional reaction to hallucinations. The negative association here between CBS worsening during the COVID-19 lockdowns and how many years people had experienced hallucinations may reflect the use of coping strategies, or habituation, that meant they were less impacted than people who had more recently started to experience hallucinations. It should be noted that participants were not required to state which country they experienced the COVID-19 lockdowns and some may have experienced rather different situations to those in the UK.
This study has confirmed the presence of visual hallucinations in younger-age adults with visual impairments resulting from a wide range of eye conditions. Depression, anxiety, and loneliness are known to be more prevalent in people with vision loss than people of a similar age with intact vision, but the prevalence in the sample in the present study appears to be particularly high. Just under half of the participants would be classed as being depressed and more than half scored highly for the presence of anxiety and loneliness. There was some indication that depression and anxiety were related to the frequency of hallucinations, but no other relationships were found between the psychosocial factors and hallucination measures. This may reflect low statistical power, due to the small sample size, and a larger sample may demonstrate a relationship between these psychosocial measures and further hallucination measures. Another possibility is that the psychosocial measures may interact with many other factors (both external environmental factors and those relating to the person and their sight loss condition) to modulate hallucinations in ways not captured by the survey used here. There remain many unanswered questions worthy of further investigation, including the possibility of a gender bias, cultural differences, the role of psychosocial factors, differences in hallucination duration, and evaluations of treatment options. Given CBS is not uncommon, there is a clear need for further research that could test a wider sample of younger people with sight loss, including those who do and do not experience hallucinations.
Limitations of the study
The conclusions that can be drawn from the present study are naturally limited by the use of an online survey resulting in a lack of quality control, that relies on self-reporting, including clinical details regarding eye condition and visual acuity. Our recruitment strategy targeted individuals with CBS which may have skewed the sample of participants included (e.g. self-selecting participants with more severe symptoms) that may have biased the sample toward those who experience more frequent hallucinations. An apriori power calculation was not performed, but based on the effect size in the data the study is underpowered, and a larger sample would be needed to reliably detect significant effects. The high drop-out rate contributed to the small sample and may also have given a biased sample, this could be addressed by having greater researcher engagement with the participants in future work. The survey did not include questions regarding the content of the hallucinations, which is a factor that may influence ratings on measures such as the emotional impact of hallucinations, that would be useful to include in subsequent studies.
Supplemental Material
Supplemental material, sj-docx-1-oed-10.1177_25158414241294177 for Are depression, anxiety and loneliness associated with visual hallucinations in younger adults with Charles Bonnet syndrome? by Robin Walker, Caecilie Valla Broman, Sam Hopkins, Mark Gould and Juliet Holdstock in Therapeutic Advances in Ophthalmology
Acknowledgments
We are grateful to the Macular Society UK and Esme’s Umbrella for their assistance with participant recruitment.
Footnotes
ORCID iD: Robin Walker  https://orcid.org/0000-0002-5277-1195
https://orcid.org/0000-0002-5277-1195
Supplemental material: Supplemental material for this article is available online.
Contributor Information
Robin Walker, Department of Psychology, Royal Holloway, University of London, Egham Hill, Egham, TW20 0EX, UK.
Caecilie Valla Broman, Department of Psychology, Royal Holloway, University of London, Egham, UK.
Sam Hopkins, Department of Psychology, Royal Holloway, University of London, Egham, UK.
Mark Gould, Department of Psychology, Royal Holloway, University of London, Egham, UK.
Juliet Holdstock, Department of Psychology, Royal Holloway, University of London, Egham, UK.
Declarations
Ethics approval and consent to participate: Ethics approval was obtained from the Royal Holloway Department of Psychology Ethics Committee (REC Project ID: 3419) and the study was conducted in adherence to the tenets of the Declaration of Helsinki. Informed consent was obtained electronically.
Consent for publication: Participants gave their consent to take part in the study and for their data and any direct quotes to be used in anonymized form in any subsequent presentations or publications.
Author contributions: Robin Walker: Conceptualization; Data curation; Formal analysis; Methodology; Project administration; Resources; Supervision; Writing – original draft; Writing – review & editing.
Caecilie Valla Broman: Conceptualization; Investigation; Methodology; Project administration; Writing – original draft.
Sam Hopkins: Conceptualization; Investigation; Methodology; Project administration; Writing – original draft.
Mark Gould: Investigation; Project administration; Supervision; Writing – original draft; Writing – review & editing.
Juliet Holdstock: Data curation; Formal analysis; Writing – original draft; Writing – review & editing.
Funding: The authors acknowledge the Macular Society UK for financial support to the first author for the research, and publication of this article.
Competing interests: The authors declare that there is no conflict of interest.
Availability of data and materials: The data is available on request to the corresponding author
References
- 1. de Morsier G. The Charles Bonnet syndrome: visual hallucinations in the aged without mental deficiency. Ann Medico Psychologiques 1967; 2: 678–702. [PubMed] [Google Scholar]
- 2. Ffytche DH. Visual hallucinations and the Charles Bonnet syndrome. Curr Psychiatry Rep 2005; 7: 168–179. [DOI] [PubMed] [Google Scholar]
- 3. Menon GJ, Rahman I, Menon SJ, et al. Complex visual hallucinations in the visually impaired: the Charles Bonnet syndrome. Surv Ophthalmol 2003; 48: 58–72. [DOI] [PubMed] [Google Scholar]
- 4. Teunisse RJ, Cruysberg JRM, Verbeek A, et al. The Charles Bonnet syndrome: a large prospective study in The Netherlands. A study of the prevalence-of the Charles Bonnet syndrome and associated factors in 500 patients attending the University Department of Ophthalmology at Nijmegen. Br J Psychiatry 1995; 166: 254–257. [DOI] [PubMed] [Google Scholar]
- 5. Rovner BW. The Charles Bonnet syndrome: a review of recent research. Curr Opin Ophthalmol 2006; 17: 275–277. [DOI] [PubMed] [Google Scholar]
- 6. Gordon KD. Prevalence of visual hallucinations in a national low vision client population. Can J Ophthalmol 2016; 51: 3–6. [DOI] [PubMed] [Google Scholar]
- 7. Manford M, Andermann F. Complex visual hallucinations. Clin Neurobiol Insights. Brain 1998; 121: 1819–1840. [DOI] [PubMed] [Google Scholar]
- 8. Tan CSH, Yong VKY, Eong KGA. Onset of Charles Bonnet syndrome (formed visual hallucinations) following bilateral laser peripheral iridotomies. Eye 2004; 18: 647–649. [DOI] [PubMed] [Google Scholar]
- 9. Khan JC, Shahid H, Thurlby DA, et al. Charles Bonnet syndrome in age-related macular degeneration: the nature and frequency of images in subjects with end-stage disease. Ophthalm Epidemiol 2008; 15: 202–208. [DOI] [PubMed] [Google Scholar]
- 10. Jones L, Moosajee M. Visual hallucinations and sight loss in children and young adults: a retrospective case series of Charles Bonnet syndrome. Br J Ophthalmol 2021; 105: 1604–1609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Jones L, Ditzel-Finn L, Enoch J, et al. An overview of psychological and social factors in Charles Bonnet syndrome. Ther Adv Ophthalmol 2021; 13: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Schwartz TL, Vahgei L. Charles Bonnet syndrome in children. J AAPOS 1998; 2: 310–313. [DOI] [PubMed] [Google Scholar]
- 13. Schultz G, Needham W, Taylor R, et al. Properties of complex hallucinations associated with deficits in vision. Perception 1996; 25: 715–726. [DOI] [PubMed] [Google Scholar]
- 14. Santhouse AM, Howard RJ, Ffytche DH. Visual hallucinatory syndromes and the anatomy of the visual brain. Brain 2000; 123: 2055–2064. [DOI] [PubMed] [Google Scholar]
- 15. Ffytche DH, Howard RJ, Brammer MJ, et al. The anatomy of conscious vision: An fMRI study of visual hallucinations. Nat Neurosci 1998; 1: 738–742. [DOI] [PubMed] [Google Scholar]
- 16. Schultz G, Melzack R. Visual hallucinations and mental state: a study of 14 charles bonnet syndrome hallucinators. J Nerv Mental Dis 1993; 181: 639–643. [DOI] [PubMed] [Google Scholar]
- 17. Jackson M, Bassett K, Nirmalan P. Charles Bonnet hallucinations: natural history and risk factors. In: International Congress Series 2005. Elsevier, 2005, pp.592–595. [Google Scholar]
- 18. Boxerman H, Wittich W, Overbury O. Charles Bonnet syndrome in older adults with age-related macular degeneration: Its relationship to depression and mild cognitive impairment. British J Visual Impairm 2015; 33: 19–30. [Google Scholar]
- 19. Casten R, Rovner B. Depression in age-related macular degeneration. J Visual Impairment Blindn 2008; 102: 591–599. [PMC free article] [PubMed] [Google Scholar]
- 20. Evans JR, Fletcher AE, Wormald RP. Depression and anxiety in visually impaired older people. Ophthalmology 2007; 114: 283–288. [DOI] [PubMed] [Google Scholar]
- 21. Cox TM, Ffytche DH. Negative outcome Charles Bonnet syndrome. British Journal of Ophthalmology 2014; 98: 1236–1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Holroyd S, Rabins PV, Finkelstein D, et al. Visual hallucinations in patients from an ophthalmology clinic and medical clinic population. J Nerv Mental Dis 1994; 182: 273–276. [DOI] [PubMed] [Google Scholar]
- 23. Holroyd S, Rabins PV, Finkelstein D, et al. Visual hallucinations in patients with macular degeneration. Am J Psychiatry 1992; 149: 1701–1706. [DOI] [PubMed] [Google Scholar]
- 24. Teunisse RJ, Zitman FG, Raes DC. Clinical evaluation of 14 patients with the Charles Bonnet syndrome (isolated visual hallucinations). Compr Psychiatry 1994; 35: 70–75. [DOI] [PubMed] [Google Scholar]
- 25. Teunisse RJ, Cruysberg JR, Hoefnagels WH, et al. Social and psychological characteristics of elderly visually handicapped patients with the Charles Bonnet syndrome. Compr Psychiatry 1999; 40: 315–319. [DOI] [PubMed] [Google Scholar]
- 26. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983; 67: 361–370. [DOI] [PubMed] [Google Scholar]
- 27. Russell DW. UCLA Loneliness Scale (Version 3): Reliability, validity, and factor structure. J Personal Assessm 1996; 66: 20–40. [DOI] [PubMed] [Google Scholar]
- 28. Gold K, Rabins PV. Isolated visual hallucinations and the Charles Bonnet syndrome: a review of the literature and presentation of six cases. Compr Psychiatry 1989; 30: 90–98. [DOI] [PubMed] [Google Scholar]
- 29. Subhi Y, Nielsen MA, Scott DAR, et al. Prevalence of Charles Bonnet syndrome in low vision: a systematic review and meta-analysis. Ann Eye Sci 2022; 7: 12. [Google Scholar]
- 30. Subhi Y, Schmidt DC, Bach-Holm D, et al. Prevalence of Charles Bonnet syndrome in patients with glaucoma: a systematic review with meta-analyses. Acta Ophthalmologica 2021; 99: 128–133. [DOI] [PubMed] [Google Scholar]
- 31. Rovner BW. The Charles Bonnet syndrome: visual hallucinations caused by vision impairment. Geriatrics 2002; 57: 45–46. [PubMed] [Google Scholar]
- 32. Brunes A, Heir T. Visual impairment and depression: age-specific prevalence, associations with vision loss, and relation to life satisfaction. World J Psychiatry 2020; 10: 139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Geueke A, Morley MG, Morley K, et al. Anxiety and charles bonnet syndrome. J Visual Impairment Blindness 2012; 106: 145–153. [Google Scholar]
- 34. Jones L, Ditzel-Finn L, Potts J, et al. Exacerbation of visual hallucinations in Charles Bonnet syndrome due to the social implications of COVID-19. BMJ Open Ophthalmol 2021; 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-oed-10.1177_25158414241294177 for Are depression, anxiety and loneliness associated with visual hallucinations in younger adults with Charles Bonnet syndrome? by Robin Walker, Caecilie Valla Broman, Sam Hopkins, Mark Gould and Juliet Holdstock in Therapeutic Advances in Ophthalmology