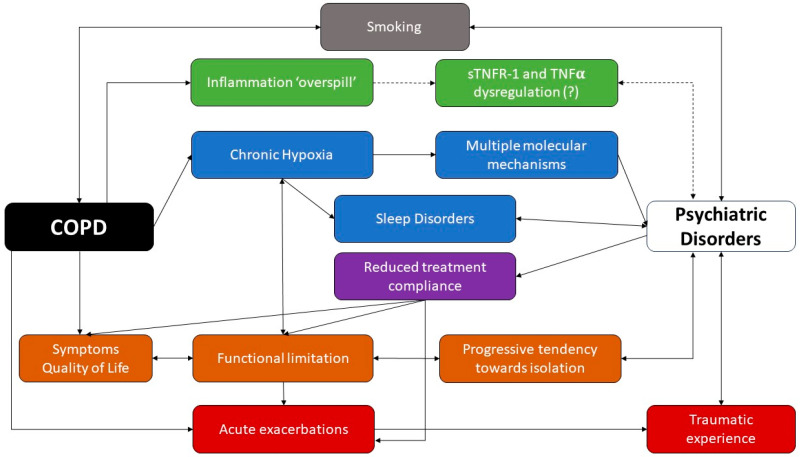
Figure 1.
COPD and psychiatric disorders: a complex liaison. While smoking seems to be a relevant risk factor for both conditions, the chronic local inflammation observed in COPD patients might occasionally undergo a ‘spillover’, with an increased systemic circulation of some inflammatory cytokines and chemokines. Chronic hypoxia has been linked to neuronal and hormonal alterations through multiple mechanisms, while sleep disorders have been linked to intermittent hypoxia, which is extremely common among psychiatric patients. Patients with COPD tend to experience isolation and limitations due to their impaired quality of life. Moreover, COPD patients may undergo acute exacerbations, which contribute to the worsening of the quality of life and to the progression toward disability; however, sometimes, they might be perceived as traumatic experiences. Finally, psychiatric disorders have been linked to a reduced compliance with pharmacological treatment, which impairs the patient’s quality of life and might be a risk factor for acute exacerbations. Full arrows show established relationships between items, while dashed arrows have been used to show unclear/uncertain relationships.