Abstract
Research indicates that a significant proportion of people living with HIV/AIDS report symptoms of posttraumatic stress disorder (PTSD). Moreover, attachment style has been associated with psychological and behavioral outcomes among persons living with HIV/AIDS. Attachment style may influence the ability to cope with traumatic stress and affect PTSD symptoms. To examine the association between attachment style and coping with PTSD symptoms, we assessed 94 HIV-positive adults on self-report measures of posttraumatic stress, coping, and attachment style. In multiple regression analysis, avoidant attachment and emotion-focused coping were positively and significantly associated with greater PTSD symptomatology. Support was also found for the moderating effects of avoidant and insecure attachment styles on emotion-focused coping in relation to greater PTSD symptoms. Taken altogether, these results suggest that interventions that develop adaptive coping skills and focus on the underlying construct of attachment may be particularly effective in reducing trauma-related symptoms in adults living with HIV/AIDS.
Keywords: HIV/AIDS, Attachment, PTSD, Stress, Trauma, Coping
Introduction
The prevalence of posttraumatic stress disorder (PTSD) in the general population is estimated to be 9.7% for women and 3.6% for men (Kessler et al., 2005); however, it is much higher in certain groups, including individuals living with HIV/AIDS (Hoff et al., 1997). For example, research conducted on a diverse sample of men and women living with HIV/AIDS found that almost a quarter of the sample met full criteria for PTSD (Gore-Felton & Koopman, 2002). Moreover, research among HIV-positive women found that more than one-third (35%) reported a history of trauma and met criteria for PTSD (Kimerling et al., 1999).
More research is needed to fully understand why there are such high rates of PTSD symptoms among adults living with HIV/AIDS. For instance, the rates may be higher among those with HIV infection due, in part, to lifestyle and contextual factors that are associated with elevated disease risk. Moreover, there is growing evidence that individuals living with HIV/AIDS are often either living in the presence of repetitive traumatic experiences or have experienced substantial trauma and stress in their past (Gore-Felton & Koopman, 2002; Gore-Felton et al., 2001; Kimerling et al., 1999; Wyatt et al., 2002). Indeed, previous trauma has been associated with experiencing HIV diagnosis as a traumatic stressor among individuals living with HIV (Nightingale et al., 2011). Furthermore, an HIV diagnosis that is perceived as a traumatic stressor has been associated with deleterious physical and mental health outcomes (Nightingale et al., 2011).
Regardless of the reasons why individuals living with HIV/AIDS experience significant amounts of trauma, there is compelling evidence that indicates exposure to trauma is associated with behavior that puts some individuals at increased risk for acquiring or transmitting HIV. For example, women who have experienced sexual trauma are more likely to report greater numbers of sexual partners, use alcohol or drugs while having sex, engage in unprotected sex, and to have sex with a high-risk partner (Lang et al., 2003) compared to women without a sexual trauma history. Thus, effective prevention and intervention efforts need to consider the influence of trauma in behavioral patterns that convey risk of transmitting or acquiring HIV.
Attachment and coping among HIV-positive adults
Since Bowlby’s original work on attachment (1969/1982), research has consistently supported the existence of secure and several types of insecure styles of attachment which include avoidant, ambivalent, and disorganized (Ainsworth et al., 1978); enmeshed and disengaged (Olson, 1986); and avoidant, anxious, or anxious-ambivalent (Hazan & Shaver, 1987; Hazan & Diamond, 2000).
Adult attachment styles are largely based on the assumption that the factors which characterize parent–child relationships are highly similar to ones that characterize intimate relationships among adults. Attachment theory generally considers the formation of a child’s early relationships, which is usually with parents or primary caregivers, as providing the child with internal working models for forming future relationships and understanding the emotional availability and responsiveness of those around them (Bowlby, 1969/1982, 1979; Gwadz et al., 2004; Hill, 2002).
In addition to relationships, attachment styles have also been associated with the ability, or inability to adaptively cope with a chronic illness (Schmidt et al., 2001; West et al., 1986). Among adults living with HIV/AIDS, insecure attachment and greater use of coping strategies like behavioral or emotional disengagement have been associated with greater perceived stress (Koopman et al., 2000). Also among adults living with HIV/AIDS, those who are less securely attached, compared to those more securely attached, are more depressed and report greater perceived stress (Riggs et al., 2007). Moreover, secure attachment and reduced reliance on behavioral disengagement is associated with increased satisfaction with social support and greater positive mood among a diverse sample of adults living with HIV/AIDS (Turner-Cobb et al., 2002), suggesting that it is quite possible that attachment style and an inability to cope effectively with stressful life events increases an individual’s susceptibility to psychopathology—including PTSD. This is important because there is a body of research that demonstrates secure attachment is critical in the development of children’s capacity for emotion regulation (Diamond & Hicks, 2004; Repetti et al., 2002).
Clinically, emotional dysregulation is often the focus of psychotherapy and pharmacological interventions among patients with PTSD. Many of the psychotherapeutic interventions share a commonality with best parenting practices that tend to develop secure attachment such as providing a safe and secure environment, establishing and maintaining interpersonal boundaries, developing self-efficacy, building self-esteem, and establishing a sense of personal agency as well as control (Gore-Felton & DiMarco, 2007).
According to the Diagnostic and Statistical Manual of Mental Disorders, one of the hallmark symptoms of PTSD is avoidance (DSM-IV-TR; American Psychiatric Association, 2000) and avoidant attachment style has been associated with not seeking help (Collins & Feeney, 2000). Consistent with these findings, avoidant attachment has been associated with a pattern of stress reactivity characteristic of repressive coping such that avoidant individuals show a progressive increase in physiological stress reactivity in response to laboratory emotional and stress tasks (Diamond et al., 2006). Thus, it is clear that emotional regulation, attachment and coping are associated with one another. While the literature consistently demonstrates a linear relationship between coping and attachment, very little research has examined the interaction effect of coping and attachment particularly in the context of stress symptoms.
Lazarus (1993) asserted that coping was a way of dealing with stressors and coping strategies were either problem-focused or emotion-focused. Moreover, to effectively deal with a stressor the coping strategy needs to be applied appropriately to different types of stressors. For instance, if the stressor is within the individual’s control the best coping strategy is a problem-focused one. Alternatively, if the stressor is not within the individual’s control, an emotion-focused strategy is better. Most stressors are complex, and individuals often need to use both types of coping to effectively deal with life’s problems. Difficulties arise when individuals either over or under use a particular coping strategy regardless of the type of stressor and often these strategies are developed early in one’s development. Indeed, experiences as children are likely to influence coping strategies used as adults (Crittenden, 1992). Thus, it is highly probable that attachment style has a moderating effect on coping which influences psychological functioning.
Emotion-focused coping has been strongly and consistently associated with PTSD (Brown et al., 2003), which is not surprising given a hallmark feature of PTSD is lack of emotion regulation which is linked to neurobiological factors (Lanius et al., 2010). Few studies have examined the association between PTSD symptoms and coping with HIV illness and to our knowledge no study has examined this relationship within the context of attachment styles. Thus, given the prevalence of current and lifetime trauma experiences and subsequent stress reactivity that significantly impairs psychosocial functioning among persons living with HIV/AIDS (Gore-Felton et al., 2001; Gore-Felton & Koopman, 2002; Kimerling et al., 1999; Koopman et al., 2002), increasing our understanding of factors associated with PTSD symptomatology is an important first step to developing effective interventions. To that end, we focused on the relationship between attachment style, PTSD, and emotion-focused coping. We hypothesized that (1) insecure, avoidant, and anxious attachment styles would be associated with greater PTSD symptoms; and (2) greater use of emotion-focused coping would be associated with greater PTSD symptoms. Furthermore, we were interested in the moderating effects of attachment on coping with relationship to PTSD symptoms and hypothesized that (3) individuals with greater avoidant attachment and greater emotion focused coping would report greater PTSD symptoms; (4) individuals with greater anxious attachment and greater emotion focused coping would report greater PTSD symptoms; and (5) individuals with greater insecure attachment and greater emotion focused coping would report greater PTSD symptoms.
Method
Participants
Participants were enrolled in a randomized clinical trial “An Evaluation of Group Psychotherapy for People with HIV,” designed to examine the effects of Supportive Expressive Group Psychotherapy (Spiegel et al., 1989) on quality of life and health behavior among HIV-positive adults. All participants completed informed consent forms after the study was explained to them and prior to completing study questionnaires. We received additional funding to include measures of trauma after the study began. The current study examined the baseline questionnaires, prior to randomization, on a sub-sample of 94 subjects (from a larger study of 187 participants) who completed measures on trauma experiences and symptoms. Participants were recruited through newspaper advertisements, fliers, and medical clinics. The measures of PTSD symptoms and attachment styles were administered to only a subset of this larger sample who also completed self-report measures on demographics and coping.
Inclusion criteria were as follows: (1) documentation of seropositive status; (2) 18 years or older; (3) willingness to and ability to provide informed consent; and (4) English proficiency sufficient to comprehend and complete questionnaires as well as participate in group psychotherapy. Exclusion criteria included either of the following: (1) persons with schizophrenia or other psychotic disorders that prevent the ability to provide informed consent; (2) persons acutely at risk of physical harm to self (suicidal) or others (homicidal); and (3) untreated drug dependence.
Measures
Demographic variables and medical status
Participants completed the Stanford Psychosocial Oncology Questionnaire, a brief demographic survey that assesses age, marital status, family size, religious affiliation, ethnicity, education, employment, sexual orientation, and family income. HIV infection and AIDS diagnoses were verified by written documentation provided by attending physicians.
Posttraumatic stress disorder symptoms
Current PTSD symptoms were assessed using the PTSD Checklist-Civilian version (PCL-C; Weathers et al., 1991). The PCL-C was developed to assess PTSD symptoms among civilian (i.e., non combat) populations. The self-report measure has 17 items, each corresponding to a specific diagnostic and statistical manual of mental disorders, fourth edition (DSM-IV) PTSD symptom (American Psychiatric Association (APA), 1994). Participants report how much they have been bothered by each symptom in the past month using a 5-point Likert-type scale with 1 equal to ‘not at all’ and 5 equal to ‘extremely.’
Because of the self-report nature of the PCL-C, we were unable to provide a definitive diagnosis of PTSD for our sample. However, based on the DSM-IV (APA, 1994), participants were identified as having symptoms consistent with full PTSD according to the following criteria: endorsement of at least one intrusive symptom; at least three avoidant symptoms; and at least two hyperarousal symptoms, with an item score of 3 for symptom criterion (Forbes et al., 2001). This scale also assesses the severity of PTSD, ranging from 17 to 85. The scale demonstrated strong internal consistency (Cronbach’s alpha = 0.91).
Trauma experiences
To assess traumatic experiences that meet criterion A of the PTSD diagnosis (i.e., actual or potential death or life-threatening injury) we used the Trauma History Questionnaire (THQ; Green, 1996). The THQ is a 24-item questionnaire that assesses the lifetime occurrence of a variety of traumatic events in three categories: crime, general disaster/trauma, and sexual and physical assault experiences. The participant responds “yes/no” to the specific event, the number of times the event occurred, and the age of the occurrence.
Coping
Coping strategies were assessed using the Brief COPE, an abridged form of the COPE (Carver, 1997). The Brief COPE has 12 subscales comprised of two items each, measuring the frequency an individual uses a particular coping strategy to deal with a specific stressor. The stressor in this study was ‘dealing with the stress of HIV or AIDS in the previous 3 months.’ Items were rated on a 4-point Likert-type scale, ranging from 1 “I have not done this at all” to 4 “I have been doing this a lot.” The strength of the Brief COPE is that it can be modified to meet specific research needs (Carver, 1997). Therefore, we modified the use of this instrument by only using four subscales related to emotion-focused coping: (1) seeking social support for emotional reasons (“I’ve been getting emotional support from others” and “I’ve been getting comfort and understanding from someone”); (2) acceptance (“I’ve been accepting the reality of the fact that it has happened” and “I’ve been learning to live with it”); (3) denial (“I’ve been saying to myself, ‘this isn’t real’” and “I’ve been refusing to believe that it has happened”); (4) religion (“I’ve been trying to find comfort in my religion or spiritual beliefs” and “I’ve been praying or meditating”). The scale demonstrated moderate internal consistency with a Cronbach’s alpha of 0.65.
Attachment styles
Participants completed the Adult Romantic Attachment measure (Hazan & Shaver, 1987). The self-report instrument contains three brief paragraphs, one for each of the following three attachment styles: (1) secure, (2) anxious, and (3) avoidant. Participants were instructed to rate on a 9-point, Likert-type scale (with 1 equal to ‘extremely uncharacteristic’ and 9 equal to ‘extremely characteristic’) the extent to which each of the attachment prototypes represented how they typically felt in close relationships. A large nationally representative study provides support for the construct and predictive validity of this measure (see Mickelson et al., 1997).
Procedure
Participants provided written, informed consent prior to participating in the screening interview. Interviewees who met inclusion criteria provided written, informed consent to complete the study questionnaires. Those who completed the screening interview and study questionnaires received $25.
Data analysis
Spearman correlations were computed among the predictors to test for multicollinearity. Then, simultaneous multiple regression analysis was conducted, with PTSD symptoms as the dependent variable and attachment styles (anxious/ambivalent, avoidant, and secure), emotion-focused coping, and the interactions among them, as the independent variables. All independent variables were standardized (Z scores) before they were entered into the multiple regression analysis. Power calculations were conducted using G*Power 3 and based on a priori hypotheses (Faul et al., 2007, 2009). We calculated our effect size from predictor and outcome correlation values (f2 = .46), which is considered large (Aiken & West, 1991, pp. 158). We set alpha at .05 with power .80 and deter- mined that we needed a sample of at least 39. A moderate effect size (f2 = .15), required a sample of 94 at the sample alpha and power level.
Results
The participants in this study did not differ from those with missing data in age, employment, or number of years of education. However, there was a difference found in gender (X2 = 25.97, P < .001), household income (X2 = 21.86, P < .001), sexual identification (X2 = 16.41, P = .003), and AIDS diagnosis (X2 = 4.83, P = .028), such that participants included in this study are comprised of more women (62.8%); reported lower household income (77.8% < $20,000, compared to 50.5%), and identify as heterosexual (54 vs. 31%). In addition, fewer participants (34.1%) in this study were diagnosed with AIDS.
Demographic characteristics are summarized in Table 1. Participants included slightly more females (63%) than males (37%) and the average age was 39.7 years (SD = 7.5). The sample was ethnically diverse. About a fifth of the sample had completed less than 12 years of education, two-thirds were unemployed, and the majority had household incomes under $20,000 per year. Slightly over half identified as heterosexual, with over a third identifying as homosexual and 11% identifying as bisexual or other. Almost half identified as single.
Table 1.
Demographic and medical characteristics of the participants
| Characteristic | n | % |
|---|---|---|
| Gender | ||
| Male | 35 | 37.2 |
| Female | 59 | 62.8 |
| Age | ||
| 21–30 | 13 | 13.8 |
| 31–40 | 38 | 40.4 |
| 41–50 | 40 | 42.5 |
| 51+ | 3 | 3.3 |
| Ethnic backgrounda | ||
| African Americans | 40 | 42.6 |
| Asian Americans | 1 | 1.1 |
| Caucasian | 49 | 52.1 |
| Filipino | 1 | 1.1 |
| Mexican Americans/Latino | 5 | 5.3 |
| Native Americans | 7 | 7.4 |
| Others | 6 | 6.4 |
| Years of education | ||
| <12 | 20 | 21.5 |
| 12 | 23 | 24.7 |
| >12 | 50 | 53.8 |
| Employment | ||
| Not employed | 65 | 65.6 |
| Part-time | 15 | 16.1 |
| Full-time | 17 | 19.3 |
| Household income | ||
| <$20,000 | 70 | 77.8 |
| $20,000–$39,999 | 13 | 14.4 |
| $40,000–$59,999 | 2 | 2.2 |
| $60,000–$79,999 | 3 | 3.4 |
| $80,000–$99,999 | 2 | 2.2 |
| Religion | ||
| Protestant | 11 | 11.8 |
| Jewish | 2 | 2.2 |
| Catholic | 20 | 21.5 |
| Other | 35 | 35.3 |
| None | 26 | 29.2 |
| Sexual identification | ||
| Heterosexual | 51 | 54.3 |
| Homosexual | 33 | 35.1 |
| Bisexual | 9 | 9.6 |
| Other | 1 | 1.1 |
| Current relationship | ||
| Single | 44 | 46.8 |
| Married/similar relations | 23 | 24.5 |
| Separated | 9 | 9.6 |
| Divorced | 8 | 8.5 |
| Widowed | 5 | 5.3 |
| Other | 5 | 5.3 |
| AIDS diagnosis | ||
| Yes | 30 | 34.1 |
| No | 58 | 65.9 |
| Time elapse since AIDS diagnosis (months) | ||
| <12 | 1 | 4.2 |
| 12–24 | 2 | 8.4 |
| 25–36 | 6 | 25.2 |
| 37–60 | 10 | 42.0 |
| 61–84 | 4 | 16.8 |
| 85+ | 1 | 4.2 |
Several participants reported more than one ethnic background
Twenty-eight participants (30%) reported symptoms that were consistent with a diagnosis of PTSD. It is important to note that these individuals also reported a traumatic event consistent with criterion A that was assessed by the THQ. The most common type of violence endorsed was interpersonal violence and has been reported in detail elsewhere (see Gore-Felton et al., 2001).
Descriptive statistics for the attachment styles and PTSD symptoms are presented in Table 2, which also summarizes bivariate correlation and descriptive analyses on attachment styles, emotion-focused coping, and PTSD symptoms. Secure attachment style was inversely and significantly associated with both avoidant and anxious/ambivalent attachment styles. Anxious and avoidant attachment styles were significantly and positively correlated with one another. Emotion-focused coping was not significantly associated with attachment style. These results supported the inclusion of all of these variables in the multiple regression model as independent variables, as no pair of variables of interest showed a strong correlation.
Table 2.
Bivariate correlations and descriptive statistics among attachment styles and emotion-focused coping
| Avoidant style | Anxious style | Secure style | Emotion focus | |
|---|---|---|---|---|
| Avoidant style | – | |||
| Anxious style | .23* | – | ||
| Secure style | −.35*** | −.21* | – | |
| Emotion focus | −.01 | .14 | .06 | – |
| PTSD symptoms | .24** | .14 | −.21* | .23** |
| Descriptive statistics and measures of central tendency | |||
|---|---|---|---|
| Range | Mean (SD) | Median | |
| Avoidant style | 1–9 | 4.70 (2.35) | 5.00 |
| Anxious style | 1–9 | 4.10 (2.58) | 4.50 |
| Secure style | 1–9 | 5.05 (2.58) | 5.00 |
| Emotion focus | 1.10–3.10 | 2.05 (0.58) | 2.00 |
| PTSD symptoms | 17–85 | 34.32 (13.43) | 30.50 |
P < .05;
P < .02;
P < .001
Confirming our hypotheses, correlational analysis found that greater avoidant, anxious, and insecure attachment styles were associated with greater PTSD symptoms. We were interested in simultaneously examining the effect of the different attachment types and coping on PTSD symptoms as well as the interaction or moderating effects of attachment and coping on PTSD symptoms. To that end, we conducted a multiple regression analysis.
The multiple regression model had an overall adjusted R2 = .39 [F (7, 93) = 9.37, P < .001]. Avoidant attachment and emotion-focused coping were positively and significantly associated with PTSD symptoms (see Table 3) such that endorsing a characteristically stronger avoidant attachment style and using emotion-focused coping to deal with the stress of being HIV-positive were each significantly associated with greater PTSD symptom severity.
Table 3.
Results of multiple regression analysis on PTSD symptoms by attachment styles and emotion-focused coping and interactions
| B | SE | β | t | |
|---|---|---|---|---|
| Avoidant attachment | 4.02 | 1.27 | .28 | 3.16** |
| Anxious attachment | .22 | 1.12 | .02 | .19 |
| Secure attachment | −.39 | 1.25 | −.03 | .32 |
| EF coping | 4.49 | 1.28 | .32 | 3.50*** |
| Avoidant attachment × EF coping | −2.86 | 1.44 | −.21 | 1.99* |
| Anxious attachment × EF coping | −2.23 | 1.20 | −.16 | −1.85 |
| Secure attachment × EF coping | −4.97 | 1.26 | −.42 | 3.93*** |
EF Emotion focused
P < .05;
P < .002;
P < .001
In addition to the main effects, the following two significant interactions were found: (1) greater avoidant attachment style and greater emotion-focused coping was associated with greater PTSD; and (2) greater insecure attachment style and greater emotion-focused coping was associated with greater PTSD. Both of these interactions confirmed our a priori hypotheses. Interestingly, we did not find an interactive effect between anxious attachment and emotion focused coping.
To get a better understanding of the interaction effects, we show the plot of PTSD symptom severity analyzed by avoidant attachment style and emotion-focused coping in Fig. 1. Figure 1 indicates that avoidant attachment style has differential effects on PTSD symptoms and that avoidant attachment style interacts with coping resulting in greater PTSD symptoms. Indeed, PTSD symptoms were greater among the high-avoidant attachment subgroup; however, the greater the use of emotion focus coping the less difference there was between high avoidant and low avoidant attachment styles with respect to PTSD symptoms.
Fig. 1.
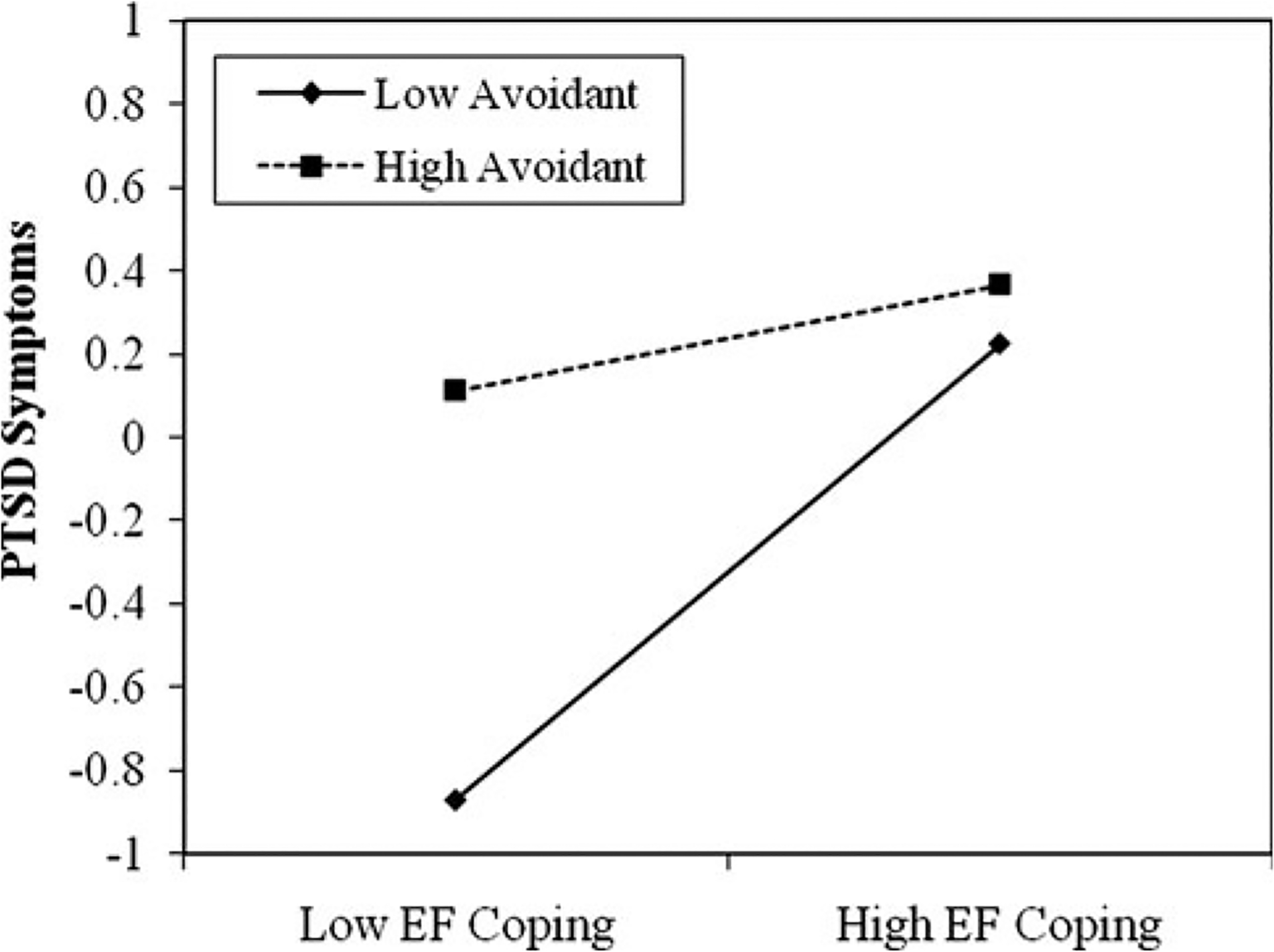
Moderating effect of avoidant attachment style on emotion-focused coping in relation to PTSD symptoms
Similarly, Fig. 2 illustrates the plot of PTSD symptom severity analyzed by secure attachment style and emotion-focused coping. The plot indicates that among insecure individuals those with greater emotion focus coping reported greater PTSD symptoms whereas among the securely attached individuals it didn’t make a difference whether they engaged in low or high emotion focused coping because regardless of their coping, their PTSD symptoms remained relatively constant. Interestingly, insecure individuals with low emotion focus coping report fewer PTSD symptoms compared to secure individuals who low emotion focus coping. We did not find a moderating effect for anxious attachment (see Table 3).
Fig. 2.
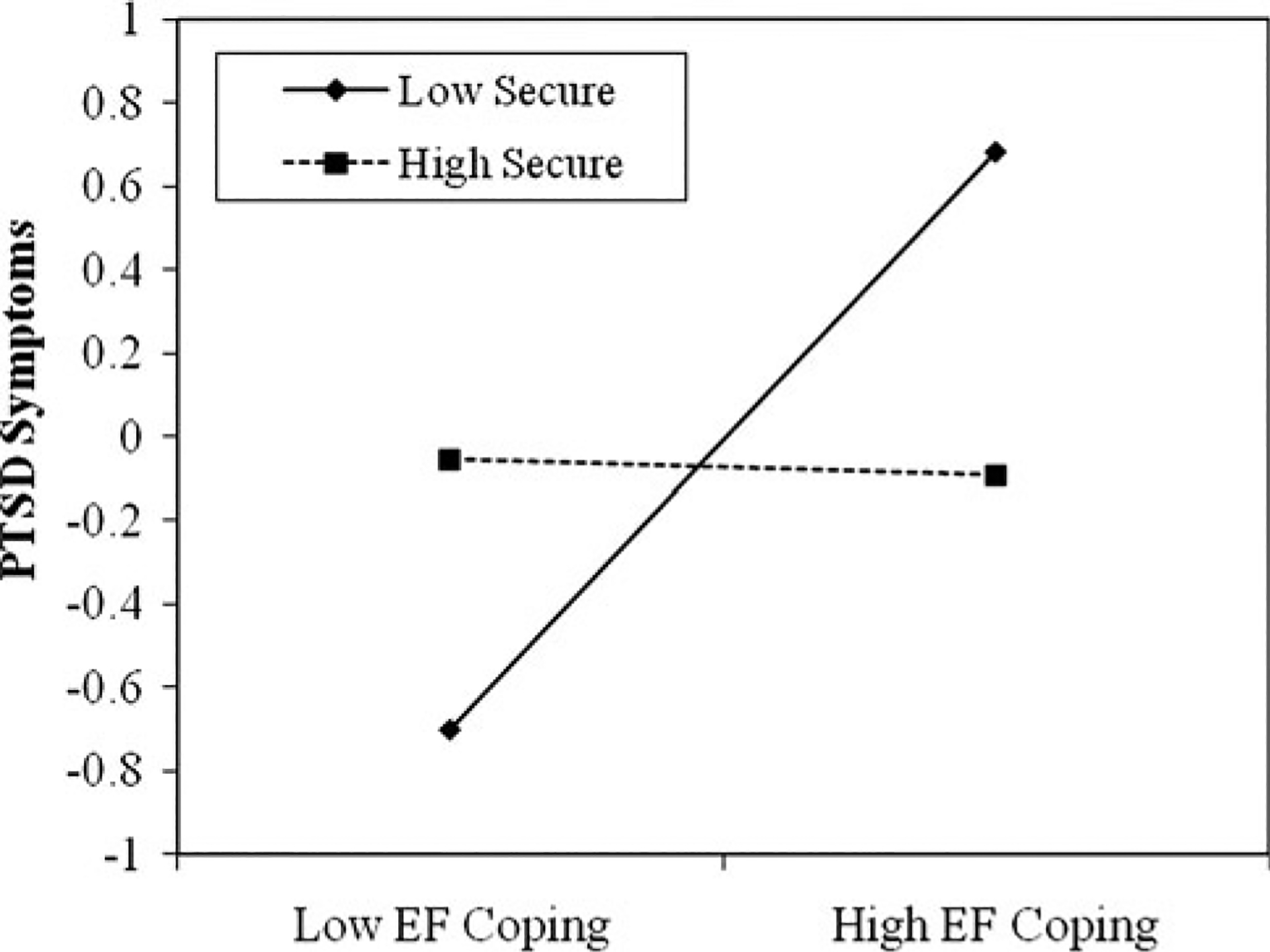
Moderating effect of insecure attachment style on emotion-focused coping in relation to PTSD symptoms
Discussion
In a diverse sample of adults living with HIV/AIDS, a significant proportion (30%) met symptom criteria consistent with a diagnosis of PTSD. Moreover, PTSD symptoms were significantly related to individuals’ attachment style and coping behavior, providing further evidence suggesting that attachment styles formed early in development are associated with psychological functioning in adulthood. However, the findings are complex in that attachment style interacts with coping, specifically emotion-focused coping behavior, such that increased use of emotion-focused coping in the context of low-avoidant attachment or low-secure (i.e., insecure) attachment was associated with greater PTSD symptoms. However, there was almost no difference in the severity of PTSD symptomatology for participants endorsing higher levels of avoidant attachment regardless of their level of emotional coping, suggesting that PTSD symptoms remain high no matter what type of coping strategy highly avoidant individuals use. One explanation for this may be that highly avoidant individuals are generally less likely to seek out resources such as social support in times of distress, and therefore, the nature of their coping (i.e., low or high emotion focused) may not affect psychological functioning. This is an important consideration because there is evidence indicating that social support can be an effective buffer against general psychological distress (Turner-Cobb et al., 2002) as well as PTSD symptoms (Martinez et al., 2002).
For individuals who are low avoidant, they may be more likely to seek some type of social support and rely to some degree on interpersonal relationships to buffer stress that is likely to be affected by the level of their emotional coping. This appears to be the case in this study because low-avoidant individuals who were less reliant on emotional coping reported lower severity of PTSD symptoms. Our findings are also consistent with previous research conducted among HIV-positive women that found that low social support was associated with greater incidence of PTSD and greater avoidance symptoms compared to women with higher social support (Jones, 1999). Future research will need to examine the relationships among emotion focused coping, social support, and PTSD to determine whether emotion focused coping moderates and/or mediates the effects of social support on PTSD symptoms.
Similar to our findings among low-avoidant individuals, we found that individuals who are characterized by an insecure attachment style and reported greater use of emotion-focused coping also reported greater PTSD symptoms. Insecure attachment is often characterized by a dependent, needy or clingy personality as well as an inability to develop and maintain friendships that is marked by difficulty to develop genuine trust, intimacy, and affection (Hazan & Shaver, 1987; Prager, 1995). Our findings suggest that insecure attachment by itself may not affect PTSD symptoms, but it may when coupled with high levels of emotion-focused coping. However, because the current study is cross-sectional and non-experimental, interpretations of the direction of causality among any of the variables cannot be made with any degree of confidence.
Our findings highlight the association between HIV-related coping and PTSD symptoms which is consistent with Nightingale et al. (2011) in demonstrating a significant association between previous trauma and HIV as a stressor with a corresponding coping response.
Although our study design prevents us from determining causality, previous research indicates that traumatic stress can have negative health consequences. For instance, a higher cumulative average of stressful life events has been found to be associated with faster progression of AIDS, with every severely stressful life event doubling the risk of progression to AIDS (Leserman et al., 2000). Thus, understanding factors associated with stress responses among HIV-positive individuals are needed to develop effective interventions to improve quality of life and to decrease morbidity and mortality.
Overall, our findings indicate that the clinical treatment for PTSD symptoms, particularly among adults living with HIV/AIDS, should consider a client’s attachment style such that the treatment focus and content is tailored according to the client’s ability to engage with others for resources and support. In addition, an assessment of coping skills and predilection for using a particular type of coping needs to be done routinely so that adaptive coping skills within the context of attachment style can be enhanced.
Study limitations
The interpretation of these study results need to done in consideration of the methodological limitations. First, the use of self-report measures may introduce reporting error or bias into the data. Second and as previously noted, the cross-sectional design of the study precludes the possibility of establishing the direction of causality between the variables that were examined. Therefore, it is possible that the attachment and coping factors that were associated with PTSD symptoms may, indeed, influence PTSD symptoms, or be affected by PTSD symptoms, or be related to a third, unknown, variable or set of variables not included in this study. Third, we are reporting on individuals with self-reported PTSD symptoms, and therefore we do not know how many of these individuals would meet full criteria for PTSD diagnosis using gold standards for clinical assessment and evaluation which limits our ability to generalize to PTSD populations. Finally, we are limited in our ability to generalize the findings only to persons living with HIV/AIDS because we did not include a comparison group of individuals who were seronegative for HIV. However, even with these study limitations, we believe that our findings supports the assertion that type of attachment and coping style are important factors that may influence the course and treatment of PTSD symptoms, and warrant further investigation, particularly in efforts aimed at increasing mental as well as physical health outcomes among persons living with HIV/AIDS.
Implications
The complex interactions of living with HIV and other trauma experiences combined with invalidating and often dangerous environmental components are challenging for researchers to examine and health providers to treat. Clinically, emotional dysregulation is often the focus of psychotherapy and pharmacological interventions among patients with PTSD (van der Kolk et al., 1996). Additionally, exposure-based therapy, which is repetitive exposure to stimuli associated with the original trauma, has demonstrated efficacy in the treatment of PTSD (Foa et al., 2005). Among HIV-positive adults with trauma symptoms, combining exposure-based paradigms with psychotherapeutic interventions that enhance secure attachment and improve HIV-related coping maybe effective in reducing trauma-related symptoms. We know that efficacious attachment interventions share commonality with best parenting practices such as providing a safe and secure environment, establishing and maintaining interpersonal boundaries, developing self-efficacy, building self-esteem, and establishing a sense of personal agency as well as control (Gore-Felton & DiMarco, 2007). Tailoring therapeutic practices to consider the interactive effect of attachment and coping style is likely to affect psychological functioning. Thus, including attachment and coping style assessments when assessing trauma experiences and symptoms may be particularly helpful as an initial step to developing efficacious treatment plans that are tailored to individual styles of relating and coping.
There is evidence suggesting that attachment styles can be altered by life events among adults (Davila et al., 1997; Lopez & Gormley, 2002). The evidence for instability in attachment styles has primarily come from studies conducted among young adults, making it difficult to generalize the findings to older adult populations. Moreover, we could find no studies that examined changes in attachment style over time in relationship to PTSD. Most research examines an attachment style construct, usually secure versus insecure in relationship to coping or mood symptoms over time, creating an important gap in our knowledge related to factors that can alter attachment style particularly in older adults. Longitudinal studies are needed to further examine the underlying influences of attachment style on individuals who report trauma-related symptoms as well as those who meet full criteria for PTSD. Clearly, the meaning of traumatic experiences by an individual are formed within the context of their existing attachment style which undoubtedly influences how they cope with everyday as well as traumatic stressors. Moreover, future research needs to explore the influence of socio-demographic factors on attachment, coping, and stress-related symptoms.
Addressing PTSD symptoms without targeting the factors that facilitate or maintain them, will have limited effects on the long-term course of the psychopathology associated with traumatic stress. Thus, a more complex approach to the treatment of PTSD is likely to be more effective in reducing psychological morbidity and would involve treatment that not only focused on developing adaptive coping, but also addressed the underlying construct of attachment style which can serve to maintain PTSD symptoms despite acquiring more adaptive coping skills.
Acknowledgments
We wish to acknowledge the contributions of Margaret Chesney, Xin-Hua Chen, Sue DiMiceli, Ron Durán, Michael Edell, Jason Flamm, Michele Gill, Peea Kim, Dennis Israelski, David Lewis, José Montoya, Kristen O’Shea, Jan Porter, Rachel Power, Andrew Zolopa, and the men and women living with HIV/AIDS who devoted their time to assist in this research. Also, this research was funded by the National Institute of Mental Health (NIMH) Grant #MH54930 (PI, David Spiegel, M.D.). Preparation of this manuscript was supported, in part, by NIMH Grant #MH63643 (PI: Cheryl Gore-Felton, Ph.D.).
Contributor Information
Cheryl Gore-Felton, Department of Psychiatry and Behavioral Sciences, Stanford University Medical Center, Stanford University School of Medicine, 401 Quarry Road, Stanford, CA 94305-5718, USA.
Karni Ginzburg, School of Social Work, Tel Aviv University, Tel Aviv, Israel.
Maggie Chartier, University of California, San Francisco, CA, USA.
William Gardner, PGSP-Stanford Psy.D Consortium, Pacific Graduate School of Psychology, Palo Alto, CA, USA.
Jessica Agnew-Blais, School of Public Health, Harvard University, Cambridge, MA, USA.
Elizabeth McGarvey, Department of Public Health Sciences, University of Virginia, Charlottesville, VA, USA.
Elizabeth Weiss, PGSP-Stanford Psy.D Consortium, Pacific Graduate School of Psychology, Palo Alto, CA, USA.
Cheryl Koopman, Department of Psychiatry and Behavioral Sciences, Stanford University Medical Center, Stanford University School of Medicine, 401 Quarry Road, Stanford, CA 94305-5718, USA.
References
- Aiken LS, & West SG (1991). Multiple regression: Testing and interpreting interactions. Thousand Oaks, CA: Sage Publications, Inc. [Google Scholar]
- Ainsworth MDS, Blehar C, Waters E, & Wall S (1978). Patterns of attachment: A psychological study of the strange situation. Hillsdale, NJ: Lawrence Erlbaum. [Google Scholar]
- American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders, fourth edition (DSM-IV). Washington, DC: American Psychiatric Association. [Google Scholar]
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders, fourth edition-text revision (DSM-IV-TR). Washington, DC: American Psychiatric Association. [Google Scholar]
- Bowlby J (1969/1982). Attachment and loss. Attachment (Vol. 1). New York: Basic Books. [Google Scholar]
- Bowlby J (1979). The making and breaking of affectional bonds. New York: Routledge. [Google Scholar]
- Brown PJ, Read JP, & Kahler CW (2003). Comorbid PTSD and substance use disorders: Treatment outcomes and role of coping. In Ouimette PC & Brown PJ (Eds.), Trauma and substance abuse: Causes, consequences, and treatment of comorbid disorders (pp. 171–190). Washington, D.C.: American Psychological Association. [Google Scholar]
- Carver CS (1997). You want to measure coping but your protocol’s too long: Consider the brief COPE. International Journal of Behavioral Medicine, 4, 92–100. [DOI] [PubMed] [Google Scholar]
- Collins NL, & Feeney BC (2000). A safe haven: An attachment theory perspective on support seeking and caregiving in intimate relationships. Journal of Personality and Social Psychology, 78, 1053–1073. [DOI] [PubMed] [Google Scholar]
- Crittenden PM (1992). Children’s strategies for coping with adverse home environments: An interpretation using attachment theory. Child Abuse and Neglect, 16, 329–343. [DOI] [PubMed] [Google Scholar]
- Davila J, Burge D, & Hammen C (1997). Why does attachment style change? Journal of Personality and Social Psychology, 73, 826–838. [DOI] [PubMed] [Google Scholar]
- Diamond LM, & Hicks AM (2004). Psychobiological perspectives on attachment: Implications for health over the lifespan. In Simpson JA & Rholes WS (Eds.), Adult attachment: New directions and emerging issues (pp. 240–263). New York: Guilford Press. [Google Scholar]
- Diamond LM, Hicks AM, & Otter-Henderson K (2006). Physiological evidence for repressive coping among avoidantly attached adults. Journal of Social and Personal Relationships, 23, 205–229. [Google Scholar]
- Faul F, Erdfelder E, Buchner A, & Lang AG (2009). Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behavior Research Methods, 41, 1149–1160. [DOI] [PubMed] [Google Scholar]
- Faul F, Erdfelder E, Lang AG, & Buchner A (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39, 175–191. [DOI] [PubMed] [Google Scholar]
- Foa EB, Hembree EA, Cahill SP, Rauch SAM, Riggs DS, Feeny NC, et al. (2005). Randomized trial of prolonged exposure for posttraumatic stress disorder with and without cognitive restructuring: outcome at academic and community clinics. Journal of Consulting and Clinical Psychology, 73, 953–964. [DOI] [PubMed] [Google Scholar]
- Forbes D, Creamer M, & Biddle D (2001). The validity of PTSD checklist as a measure of symptomatic change in combat-related PTSD. Behaviour Research and Therapy, 39, 977–986. [DOI] [PubMed] [Google Scholar]
- Gore-Felton C, Butler LD, & Koopman C (2001). HIV disease, violence, and posttraumatic stress. Focus, 16, 5–6. [PubMed] [Google Scholar]
- Gore-Felton C, & DiMarco M (2007). AIDS & trauma in the 21st century: Implications for prevention, treatment, and policy. In Carll EK (Ed.), Volume on trauma psychology (pp. 79–107). New York, NY: Greenwood Praeger. [Google Scholar]
- Gore-Felton C, & Koopman C (2002). Traumatic experiences: Harbinger of risk behavior among HIV-positive adults. Journal of Trauma and Dissociation, 3, 121–135. [Google Scholar]
- Green BL (1996). Psychometric review of trauma history questionnaire (self-report). In Stamm BH (Ed.), Measurement of stress, trauma, and adaptation (pp. 366–369). Lutherville, MD: Sidran Press. [Google Scholar]
- Gwadz MV, Clatts MC, Leonard NR, & Goldsamt L (2004). Attachment style, childhood adversity, and behavioral risk among young men who have sex with men. Journal of Adolescent Health, 34, 402–413. [DOI] [PubMed] [Google Scholar]
- Hazan C, & Diamond LM (2000). The place of attachment in human mating. Review of General Psychology, 4, 132–154. [Google Scholar]
- Hazan C, & Shaver P (1987). Romantic love conceptualized as an attachment process. Journal of Personality and Social Psychology, 52, 511–524. [DOI] [PubMed] [Google Scholar]
- Hill J (2002). Biological, psychological and social processes in the conduct disorders. Journal of Child Psychology and Psychiatry and Allied Disciplines, 43, 133–164. [DOI] [PubMed] [Google Scholar]
- Hoff RA, Beam-Goulet J, & Rosenheck RA (1997). Mental disorder as a risk factor for human immunodeficiency virus infection in a sample of veterans. Journal of Nervous and Mental Disease, 185, 556–560. [DOI] [PubMed] [Google Scholar]
- Jones DL (1999). Conceptual structure of HIV+ women with PTSD: Trauma construct elaboration. Dissertation Abstracts International, 59(7-B). [Google Scholar]
- Kessler RC, Berglund PA, Demler O, Jin R, Merikangas KR, & Walters EE (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication (NCS-R). Archives of General Psychiatry, 62, 593–602. [DOI] [PubMed] [Google Scholar]
- Kimerling R, Calhoun KS, Forehand R, Armistead L, Morse E, Morse P, et al. (1999). Traumatic stress in HIV-infected women. AIDS Education and Prevention, 11, 321–330. [PubMed] [Google Scholar]
- Koopman C, Gore-Felton C, Azimi N, O’Shea K, Ashton E, Power R, et al. (2002). Acute stress reactions among men and women living with HIV/AIDS. International Journal of Psychiatry in Medicine, 32, 361–378. [DOI] [PubMed] [Google Scholar]
- Koopman C, Gore-Felton C, Marouf F, Butler LD, Field N, Gill M, et al. (2000). Relationships between perceived stress and attachment, social support, and coping among HIV-positive persons. AIDS Care, 12, 663–672. [DOI] [PubMed] [Google Scholar]
- Lang A, Rodgers C, Laffaye C, Satz L, Dresselhaus T, & Stein M (2003). Sexual trauma, posttraumatic stress disorder, and health behavior. Behavioral Medicine, 28, 150–158. [DOI] [PubMed] [Google Scholar]
- Lanius RA, Vermetten E, Loewenstein RJ, Brand B, Schmahl C, Bremner JD, et al. (2010). Emotion modulation in PTSD: Clinical and neurobiological evidence for a dissociative subtype. American Journal of Psychiatry, 167, 640–647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus RS (1993). Coping theory and research: Past, present, and future. Psychosomatic Medicine, 55, 234–247. [DOI] [PubMed] [Google Scholar]
- Leserman J, Pettito JM, Golden RN, Gaynes BN, Gu H, Perkins DO, et al. (2000). Impact of stressful life events, depression, social support, coping and cortisol on progression to AIDS. American Journal of Psychiatry, 157, 1221–1228. [DOI] [PubMed] [Google Scholar]
- Lopez FG, & Gormley B (2002). Stability and change in adult attachment style over the first-year college transition: relations to self-confidence, coping, and distress patterns. Journal of Counseling Psychology, 49, 355–364. [Google Scholar]
- Martinez A, Israelski D, Walker C, & Koopman C (2002). Posttraumatic stress disorder in women attending human immunodeficiency virus outpatient clinics. AIDS Patient Care and STDs, 16, 283–291. [DOI] [PubMed] [Google Scholar]
- Mickelson KD, Kessler RC, & Shaver PR (1997). Adult attachment in a nationally representative sample. Journal of Personality and Social Psychology, 73, 1092–1106. [DOI] [PubMed] [Google Scholar]
- Nightingale VR, Sher TG, Mattson M, Thilges S, & Hansen NB (2011). The effects of traumatic stressors and HIV-related trauma symptoms on health and health related quality of life. AIDS and Behavior, 15, 1870–1878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olson DH (1986). Circumplex model VII: Validation studies and FACES-III. Family Process, 25, 337–351. [DOI] [PubMed] [Google Scholar]
- Prager K (1995). The psychology of intimacy. New York: Guilford Press. [Google Scholar]
- Repetti RL, Taylor SE, & Seeman TE (2002). Risky families: Family social environments and the mental and physical health of offspring. Psychological Bulletin, 128, 330–366. [PubMed] [Google Scholar]
- Riggs SA, Vosvick M, & Stallings S (2007). Attachment styles, stigma and psychological distress among HIV + adults. Journal of Health Psychology, 12, 922–936. [DOI] [PubMed] [Google Scholar]
- Schmidt S, Fischer T, Chren MM, Strauss B, & Elsner P (2001). Strategies of coping and quality of life in women with alopecia. British Journal of Dermatology, 144, 1038–1044. [DOI] [PubMed] [Google Scholar]
- Spiegel D, Bloom JR, Kraemer HC, & Gottheil E (1989). Effect of psychosocial treatment on survival of patients with metastatic breast cancer. The Lancet, 2, 888–891. [DOI] [PubMed] [Google Scholar]
- Turner-Cobb JM, Gore-Felton C, Marouf F, Koopman C, Kim P, Israelski D, et al. (2002). Coping, social support and attachment style as psychosocial correlates of adjustment in men and women with HIV/AIDS. Journal of Behavioral Medicine, 25, 337–353. [DOI] [PubMed] [Google Scholar]
- van der Kolk BA, McFarlane AC, & van der Hart O (1996). A general approach to treatment of posttraumatic stress disorder. In van der Kolk BA, McFarlane AC, & Weisaeth L (Eds.), Traumatic stress: The effects of overwhelming experience on mind, body and society (pp. 417–440). New York, NY: The Guilford Press. [Google Scholar]
- Weathers FW, Huska JA, & Keane TM (1991). The PTSD checklist-civilian version (PCL-C). (Available from F.W. Weathers, National Center for PTSD, Boston Veterans Affairs Medical Center, 150 S. Huntington Avenue, Boston, MA 02130).
- West M, Livesley WJ, Reiffer L, & Sheldon A (1986). The place of attachment in the life events model of stress and illness. Canadian Journal of Psychiatry, 31, 202–207. [DOI] [PubMed] [Google Scholar]
- Wyatt GE, Myers HF, Williams JK, Kitchen CR, Loeb T, Carmona JV, et al. (2002). Does a history of trauma contribute to HIV risk for women of color? Implications for prevention and policy. American Journal of Public Health, 92, 660–665. [DOI] [PMC free article] [PubMed] [Google Scholar]


