Abstract
Rheumatic fever is the most common cause of mitral stenosis worldwide. Embolic events represent severe complications of mitral stenosis. We describe the case of a 45-year-old women who had an ischemic stroke as the initial manifestation of previously unrecognized mitral stenosis in the absence of atrial fibrillation.
Key Words: mitral valve, rheumatic heart disease, stroke
Graphical abstract
History of Presentation
A 45-year-old woman was referred for evaluation at our institution (National Institute of Cardiology, Rio de Janeiro, Brazil) 2 years after the diagnosis of severe mitral stenosis (MS). MS was diagnosed after an ischemic stroke (IS) episode in the left temporoparietal region when she was 43 years old. The patient did not receive anticoagulant agents or antiplatelet drugs after the cerebral event. She reported the onset of dyspnea (NYHA functional class III) 6 months after the cerebral event. Cardiac auscultation revealed a regular rhythm and a heart murmur suggestive of severe MS, with a diastolic rumbling quality +3/4 at the mitral focus with presystolic accentuation, an opening snap of the mitral valve close to the second heart sound (S2 short snap), and increased intensity of S2 at the pulmonary focus (hyperphonetic P2). Neurologic examination revealed Broca's aphasia. The patient’s vital signs were as follows: blood pressure, 120/85 mm Hg; heart rate, 76 beats/min; and oxygen saturation, 99% on ambient air.
Take-Home Messages
-
•
MS should be considered a possible cause of IS in a young patient, especially in countries where RF is endemic.
-
•
This case highlights the need and importance to identify patients with MS who are in sinus rhythm and have a high risk of embolic events and who may have indications for the use of anticoagulation.
Past Medical History
The diagnosis of rheumatic fever (RF) had not been established before the clinical manifestation of the IS. She had no history of oral contraceptive use, thrombotic events, or known thrombophilia. She did not smoke or use illicit drugs.
Differential Diagnosis
Investigation of IS in a young patient without preexisting conditions requires a search for collagen vascular diseases, thrombophilia, vasculitis, and infective endocarditis. Rheumatic MS and embolic complications should be considered in countries where RF is endemic.
Investigations
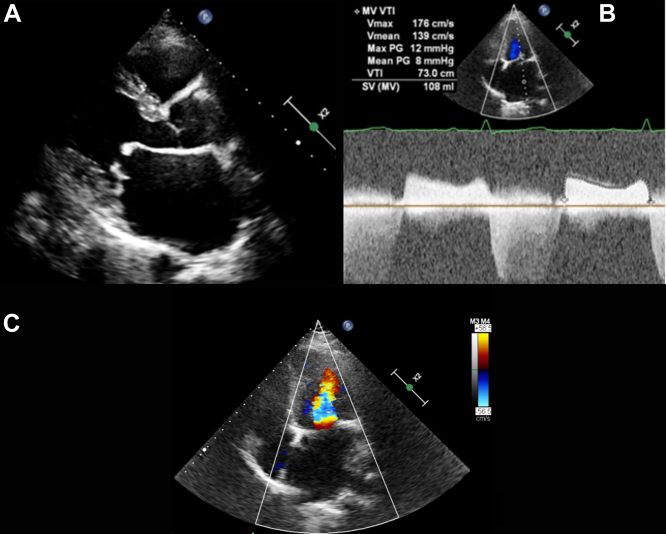
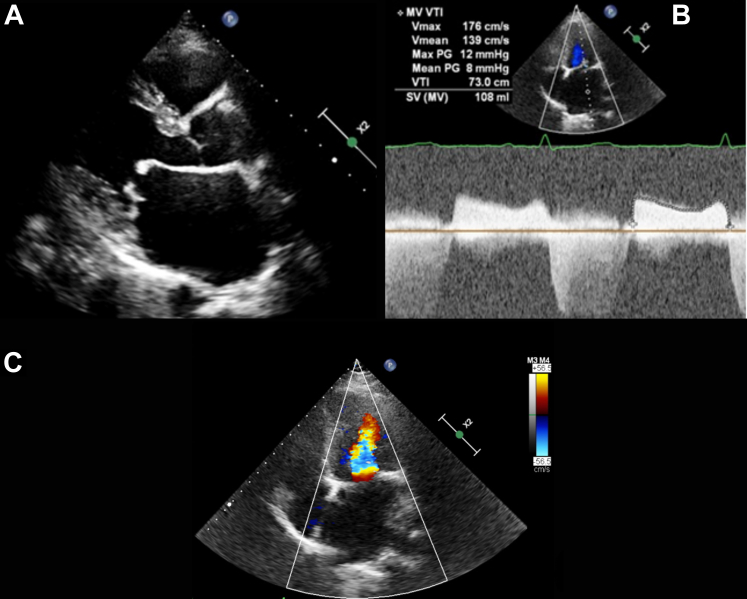
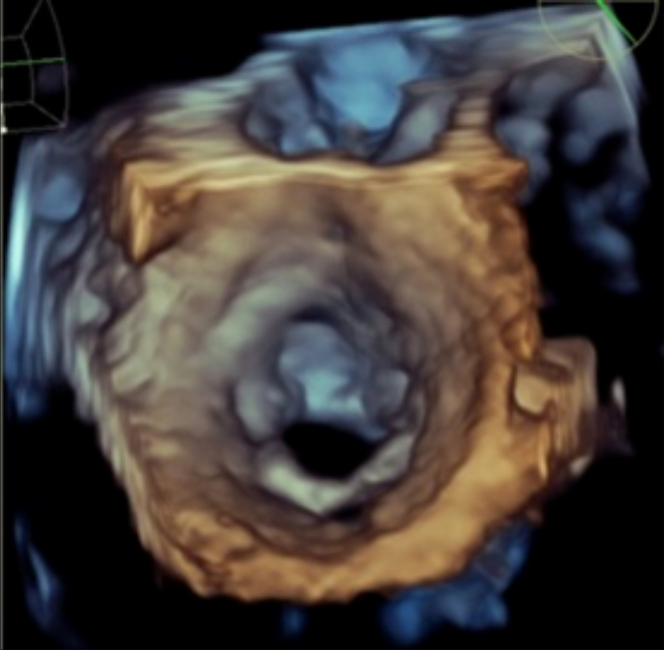
The patient was referred to our institution after confirmation of severe MS on transthoracic echocardiography. This imaging revealed left atrial (LA) enlargement with a volume of 98 mL/m2. The maximal diastolic gradient between the left atrium and the left ventricle was estimated at 12 mm Hg and medium 8 mm Hg (Figures 1A to 1C). The Wilkins-Block valve score was estimated as >8. Three-dimensional transesophageal echocardiography (TEE) showed MS in view of left atrium (Figure 2). Spontaneous echocardiographic contrast in the left atrium and low flow in the LA appendage (0.1 cm/s) were noted on TEE. Sinus rhythm with mild supraventricular instability was observed on 24-hour Holter monitoring, and results of laboratory tests for collagen disorders and thrombophilia were normal A recent brain computed tomography scan revealed temporoparietal capsular encephalomalacia on the left side with a retractile effect on the left lateral ventricle and a small area indicative of vascular sequelae in the right parietal area (Figure 3).
Figure 1.
Transthoracic Echocardiography
(A) A 2-dimensional parasternal long-axis view showing severe mitral stenosis. (B) Continuous Doppler showing high values of flow and valvular gradients. (C) A 2-dimensional image with apical 4-chamber color Doppler showing “candle flame” diastolic flow compatible with severe mitral stenosis. max = maximum; MV = mitral valve; PG = pressure gradient; SV = stroke volume; VTI = velocity-time integral.
Figure 2.
Transesophageal Echocardiography
A 3-dimensional short-axis view showing severe mitral stenosis.
Figure 3.
Brain Computed Tomography
Cerebral infarct in the right temporoparietal region and capsular encephalomalacia on the left temporoparietal area.
Management
The patient was treated with diuretic agents, beta-blockers, and vitamin K antagonists (VKAs). Valve replacement was indicated because of the presence of symptoms and significant MS. The patient underwent mechanical mitral valve prosthesis implantation. Intraoperative echocardiography demonstrated appropriate disc opening and normal transvalvular gradients of the valvular prosthesis.
Follow-Up
After intervention, the patient returned to NYHA functional class I and is under regular follow-up at our institution. She is receiving warfarin anticoagulation therapy and has not had a recurrence of cardioembolic events.
Discussion
RF is the leading cause of MS in the world. The prevalence of MS remains high in low-income countries and usually affects young individuals.1 RF is often underdiagnosed and recognized late, when there is already irreversible valve damage and associated complications.
In this case, the patient had an IS as the initial manifestation of previously unrecognized MS. Systemic embolism in MS results from thrombus formation in the left atrium, and one-half of all clinically apparent emboli are found in the cerebral vessels. The risk of embolic events correlates directly with the patient’s age and LA size and inversely with cardiac output.2
Approximately 20% of patients with MS and embolic events are in sinus rhythm.2 Most young patients remain in sinus rhythm even in the presence of significant MS. A clinical history of palpitations should alert clinicians to the possibility of paroxysmal atrial fibrillation in patients who experience embolic events in sinus rhythm. Holter monitoring should be considered in these cases.
The increased LA volume and spontaneous contrast are associated with a high risk of embolic events in MS,3 and one-half of the patients with MS and sinus rhythm demonstrate spontaneous contrast in the left atrium. These findings probably caused the embolic event in this patient.
In the presence of severe MS complicated by an embolic event, anticoagulation was indicated in this case. The American College of Cardiology, American Heart Association, and European Society of Cardiology (ESC) guidelines recommend anticoagulation with VKAs for patients with rheumatic MS and 1 of the following: atrial fibrillation, a previous embolic event, or thrombus.4 Direct oral anticoagulant agents provide an alternative to VKAs in patients with native valve heart disease excluding rheumatic MS. In the INVICTUS (INVestIgation of rheumatiC Atrial Fibrillation Treatment Using Vitamin K Antagonists, Rivaroxaban or Aspirin Studies) trial, VKAs led to a lower rate of a composite outcome of cardiovascular events or death compared with rivaroxaban therapy.5 The use of oral anticoagulation in patients with MS and sinus rhythm is controversial in the literature. The ESC guidelines advocate the use of oral anticoagulation when patients are in sinus rhythm and TEE shows spontaneous contrast or an enlarged left atrium (M-mode diameter >50 mm/LA volume >60 mL/m2).6
Mitral valve replacement was indicated in this patient as a result of severe symptomatic MS (mitral valve area <1.5 cm2) with unfavorable anatomical characteristics for percutaneous intervention. In this case, surgery is a Class 1 indication according to current guidelines.4 The indication for valve intervention in asymptomatic patients and a history of embolic events is controversial in the literature. The ESC guidelines recommend percutaneous mitral comissurotomy in asymptomatic patients with a high embolic risk such as a history of systemic embolism, spontaneous contrast in the left atrium, and recent onset atrial fibrillation (Class 2a indication).6 Further studies are needed to define more precisely which patients will benefit from valve intervention to prevent embolic events in the presence of MS.
Conclusions
RF is prevalent in low-income countries and affects young adults. The diagnosis of rheumatic heart disease often occurs late in the presence of severe valvular involvement. Embolic events constitute a significant concern in rheumatic MS, and in one-half of cases, these events occur in the cerebral circulation. Patients with rheumatic MS and sinus rhythm may experience embolic events. VKAs are recommended for patients in sinus rhythm who are at high embolic risk.
Funding Support and Author Disclosures
Funding was provided by Fundação Pró Coração (FUNDACOR), Rio de Janeiro, Brazil. The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
References
- 1.Tarasoutchi F., Montera M.W., Ramos A.I.O., et al. Update of the Brazilian guidelines for valvular heart disease: 2020. Arq Bras Cardiol. 2020;115(4):720–775. doi: 10.36660/abc.20201047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thomas J.D., Bonow R.O. In: Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine. 11th ed. Zipes D.P., Libby P., Bonow R.O., Mann D.L., Tomaselli G.F., editors. Elsevier; 2019. Mitral valve disease; pp. 1415–1424. [Google Scholar]
- 3.Otto C.M., Nishimura R.A., Bonow R.O., et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2021;77(4):e25–e197. doi: 10.1016/j.jacc.2020.11.018. [DOI] [PubMed] [Google Scholar]
- 4.Galusko V., Ionescu A., Edwards A., et al. Management of mitral stenosis: a systematic review of clinical practice guidelines and recommendations. Eur Heart J Qual Care Clin Outcomes. 2022;8(6):602–618. doi: 10.1093/ehjqcco/qcab083. [DOI] [PubMed] [Google Scholar]
- 5.Connolly S.J., Karthikeyan G., Ntsekhe M., et al. Rivaroxaban in rheumatic heart disease-associated atrial fibrillation. N Engl J Med. 2022;387(11):978–988. doi: 10.1056/NEJMoa2209051. [DOI] [PubMed] [Google Scholar]
- 6.Vahanian A., Beyersdorf F., Praz F., et al. 2021 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. 2022;43(7):561–632. doi: 10.1093/eurheartj/ehab395. [DOI] [PubMed] [Google Scholar]