Abstract
Introduction
The left atrial appendage (LAA) is a distinct structure with unique developmental and structural characteristics. The LAA is involved in the formation of intra-atrial thrombi, particularly in patients with conditions such as atrial fibrillation and mitral valve disease. Left atrial appendage aneurysms (LAAA) are rare abnormal dilations of the LAA that may cause hazardous complications. However, there are limited data on the demographic features, clinical characteristics, management modalities, and prognosis of LAAA patients. This study aimed to conduct a systematic review of the reported cases of LAAA to explore the baseline characteristics, presentation, preferred diagnostic modalities, and optimal management of LAAA.
Methods
A systematic review was conducted following the PRISMA guidelines. We performed a literature search using MEDLINE/PubMed and Google Scholar. Eligible articles published between January 1940 and November 2022 were included. The eligibility criteria included case reports and case series of LAAA in English language articles. The data extracted included information on the authors, publication year, patient characteristics, signs/symptoms, diagnostic procedures, treatments, and outcomes.
Results
We identified 177 patients with LAAA in our study. There was a slight female predominance (50.9%), and the mean age was 29.7 years. Palpitations were the most common symptom reported, followed by shortness of breath and thromboembolic events. Transthoracic and transesophageal echocardiograms were the most common modalities for investigating and diagnosing LAAA, and the mean size of the aneurysm was 7.8 (5.7–9.6) × 5.9 (5.0-6.2) cm. Surgical resection is the treatment of choice for most patients with excellent prognoses. Older age and the presence of arrhythmia were significantly associated with thrombus formation and embolic events.
Conclusion
Left atrial appendage aneurysm is a rare but potentially life-threatening heart pathology that can lead to arrhythmias and thromboembolic events. Surgical resection appears to be the primary treatment option in the current literature, and most patients show improvement or are asymptomatic after treatment. Additionally, alternative approaches, such as transcatheter closure of LAAA, ablation, and medical treatments, have been reported as viable alternatives to surgical intervention.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12872-024-04323-x.
Keywords: Left atrial appendage aneurysm, Atrial fibrillation, Mitral valve disease
Introduction
During the fourth week of embryonic development, the left atrial appendage (LAA) emerges from the left wall of the major atrium [1]. In terms of its development and structure, it differs from the rest of the left atrium. The LAA is located next to the left ventricle’s free wall in the pericardium and it was thought to have a minimal role in cardiac anatomy [2]. However, because of its distinct anatomical and physiological characteristics, it can be used as a decompression chamber when left atrial pressure increases, as it does during left ventricular systole [1]. In addition, the sympathetic and parasympathetic nervous systems both supply a dense network of nerve fibers that innervate the LAA, which is involved in the synthesis of brain natriuretic and atrial peptides [3].
LAA plays a crucial role in the production of thrombi, especially in situations like atrial fibrillation and mitral valve disease. Approximately, 90% of atrial thrombi in nonrheumatic atrial fibrillation are found to be originated from the LAA. Similarly, in patients with rheumatic mitral valve disease, especially mitral stenosis, the LAA is the site of about 60% of atrial thrombi [4].
Rarely, the LAA can dilate abnormally causing left atrial appendage aneurysms (LAAA) [5]. The first reported case of LAAA was published in 1962 [6]. As of the date on which our search was conducted, 177 cases have been reported in literature. Since the first case report of LAAA [7], it has been suggested that patients with LAAA may be more susceptible to thromboembolic events. This potential increased risk is assumed to be associated with hemodynamic changes caused by the greater orifice of the appendage [8].
Despite these findings, there is limited information available about the natural history, clinical course, and effective management strategies for LAAA. The rarity of this condition has led to a lack of standardized diagnostic guidelines and treatment approaches, making it challenging for clinicians to effectively manage patients with LAAA. To address these gaps and enrich the current clinical knowledge, we systematically reviewed all published case reports and case series. This study aims to provide a comprehensive assessment of baseline characteristics, clinical presentations, diagnostic methods, and appropriate treatment strategies for patients with LAAA.
Methods
Study design
This study is a descriptive systematic review aimed at summarizing and analyzing all reported cases of left atrial appendage aneurysms (LAAA). We adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement criteria throughout the review process. This systematic review is registered in the International Platform of Registered Systematic Review and Meta-analysis Protocols (INPLASY) under registration number: INPLASY202470109.
Literature search
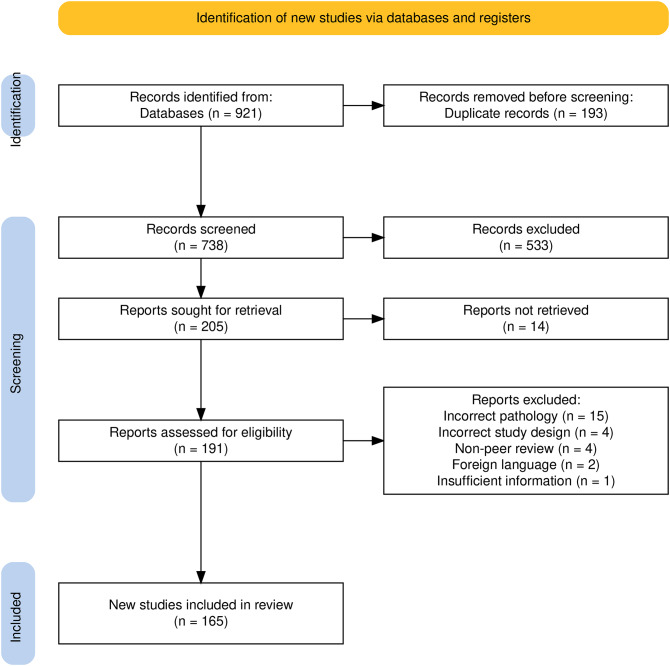
Two separate authors (AO, SA) conducted a literature search for eligible papers published between January 1940 and November 2022 using MEDLINE/PubMed and Google Scholar as secondary sources. Following that, we conducted a search using a combination of the following terms: “left atrium”, “atrial”, “appendage”, “atrial appendage”, “aneurysm”, “congenital”, and “acquired”, as well as the medical topic heading terms “atrial appendage” and “aneurysm” as search terms. The search method generated 931 articles in total. The titles and abstracts of the case reports were used to establish their eligibility. Figure 1 depicts a full PRISMA flow diagram.
Fig. 1.
Search flow diagram
Eligibility criteria
Rayyan AI software was used to remove duplicate articles from the search results. Two independent reviewers used specified eligibility criteria to analyze the retrieved papers. The eligibility screening process was divided into two stages: an initial review of titles and abstracts, followed by a thorough analysis of the whole text. The following criteria were used to choose articles: [1] they had case reports of left atrial appendage aneurysms [2], they contained case series of left atrial appendage aneurysms, and [3] they were published in English exclusively. In vitro research, animal case studies, and non-English literature were all removed.
Quality assessment
The quality of the included case reports and case series was evaluated using a structured assessment tool (Supplementary file 1). We included only peer-reviewed articles to ensure credibility. To assess quality, we utilized a modified version of the Joanna Briggs Institute (JBI) checklist for case reports and case series [9]. Criteria such as clarity of patient history, detailed description of clinical presentation, diagnostic assessment, and intervention details were evaluated to gauge the robustness of each included article.
Data extraction
For the extracted data, the authors employed a standardized data collection sheet. Two authors extracted the intended data separately, and any disputes were discussed and resolved by a third investigator. The retrieved data includes the following: author list, year of publication, baseline patient information, signs/symptoms, diagnostic procedures, therapies, and procedure outcomes.
Data synthesis
IBM SPSS v.21.0 was used to enter and evaluate the data. The continuous variables were correlated using Spearman’s rank correlations because the data did not follow a normal distribution mode. Fisher’s exact test or Pearson’s chi-square were used to compare categorical variables, where applicable. A multivariate logistic regression model was used to generate the odds ratios. Statistical significance was defined as a p-value of < 0.05. The statistical power for the multivariate logistic regression was greater than 0.80, ensuring a robust analysis. The power was calculated using established equations, where the effect size (logarithm of the odds ratio) and standard error were derived from the sample size and variance of predictor variables. The full equations used are provided in the supplementary materials (Supplementary file 2). Non-quantitative data were qualitatively synthesized.
Results
Characteristics of the patients with left atrial appendage aneurysm
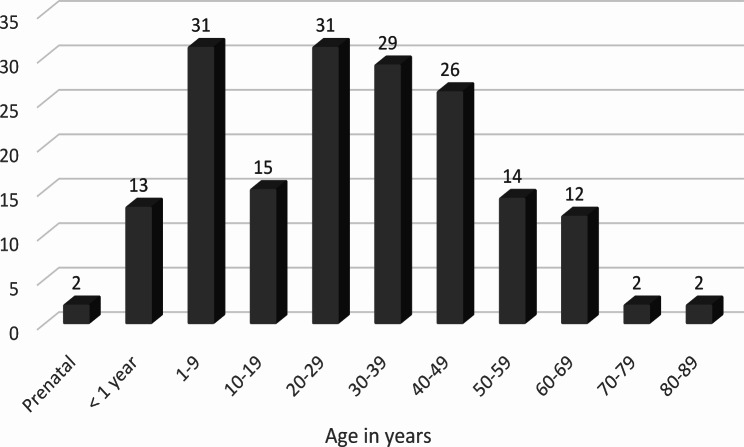
177 patients with LAAA were identified and extracted from 165 case reports and case series for this investigation [10–174]. There were 90 (50.9%) females, 85 (48.0%) males, and 2 (1.1%) patients whose gender was not stated. The patients’ mean age was 29.7 ± 21.2 years (median age was 29.0 [9.0, 44.0] years) (Fig. 2). Two (1.1%) of the documented cases of left atrial appendage aneurysm were prenatal. 59 (33.3%) of the patients were under the age of 18 (pediatrics), 106 (59.9%) were adults, and 12 (6.8%) were over the age of 65 (elderly).
Fig. 2.
Age distribution of patients with LAAA
Symptoms were present in 75.1% (n = 133) of the reported cases. Palpitations were the most frequently reported symptom, affecting 42.9% (n = 76) of symptomatic individuals, followed by shortness of breath, which was stated by 27.1% (n = 48) of the patients. Furthermore, thromboembolic events were detected in 11.3% (n = 20) of patients, while chest discomfort was noted in 10.2% (n = 18) of patients, however, 24.9% (n = 44) of patients remained asymptomatic. Upon thorough physical examination, several noteworthy findings were documented. Systolic murmurs, focal neurological deficits, irregular-irregular pulses, and tachycardia were the main documented findings.
Diagnostic procedures
A chest X-ray (CXR) was performed for 138 (78.0%) of the patients. Among the 138 patients, 136 (98.5%) had abnormalities. A prominent left heart border was found in 76 (55.1%) of the patients. Other abnormalities were described as cardiomegaly in 51 (36.9%) patients and as a “mass” in 9 (6.5%) patients.
Electrocardiography (ECG) was done on 150 patients (84.7%). Among the 150 patients, 96 (64.0%) had abnormalities. The most common ECG abnormalities were atrial fibrillation (52 patients, 29.4%), atrial flutter (12 patients, 6.8%), and supraventricular or atrial tachycardia (12 patients, 6.8%). Other findings that were occasionally documented were right bundle branch block, ischemic changes large notched “P” waves, and conduction anomalies. Of the atrial fibrillation and atrial flutter patients, 14 were diagnosed using a Holter monitor.
Transthoracic echocardiogram (TTE) was performed on 163 patients (92.1%). 106 (65.0%) of the 163 individuals were diagnosed with LAAA. The mass has been described as a cyst, cavity, mass, or echo-free structure. Other abnormalities were found in 77 (43.5%) of the individuals. The most commonly reported anomalies were mitral valve regurgitation and left ventricular compression, which occurred in 29 (16.4%) and 22 (12.4%) patients, respectively. Other documented abnormalities included impaired left ventricular function, a thrombus in the left ventricle, and biatrial enlargement.
Transesophageal echocardiography (TEE) was conducted on 69 individuals (40.0%). LAAA were found in 66 (95.6%) of the patients. In addition to the diagnosis of a left atrial appendage aneurysm, the most frequently reported abnormalities in TEE findings were thrombus materials, left ventricular wall compression, and mitral regurgitation.
Cardiac catheterization was performed on 39 (22.0%) of the patients in the form of left, right, and coronary angiography. Because of advances in echocardiographic procedures and the availability of computed tomography (CT) and magnetic resonance imaging (MRI) scans, angiography is almost never employed in modern medical practice to diagnose LAAA.
CT findings were reported for 82 (46.3%) patients, and radionuclide angiography was reported for 1 (0.6%) patient. Chest and cardiac CT were the most frequently reported imaging methods for 32 (18.1%) and 23 (13.0%) patients, respectively. Other techniques included 3D CT in 9 (5.1%) patients and multiple detectors in 8 (4.5%) patients. Of the 82 patients, 77 (93.9%) were diagnosed with LAAA. Cardiac MRI was performed for 66 (37.3%) patients. Of the 66 patients, 64 (96.9%) were diagnosed with LAAA.
There was a very strong positive correlation between the length of LAAA measured after surgery and MRI (Spearman’s rho = 1.00), TEE (Spearman’s rho = 0.80), and CT (Spearman’s rho = 0.90) data. On the other hand, there was a weak correlation between the length of LAAA measured after surgery and the length of TTE (Spearman’s rho = 0.38). There was a very strong positive correlation between the diameter of LAAA measured after surgery and MRI (Spearman’s rho = 1.0), TEE (Spearman’s rho = 1.0), TTE (Spearman’s rho = 0.83), and CT (Spearman’s rho = 0.80) (Table 1).
Table 1.
Dimensions of left atrial appendage Aneurysms measured by different imaging techniques and correlation with Surgical measurements
| Technique | Dimension | Mean | SD | Median | Q1 | Q3 | Correlation with size by surgery |
|---|---|---|---|---|---|---|---|
| Transthoracic echocardiogram | Length | 6.5 | 2.7 | 6.3 | 4.5 | 8.4 | 0.38 |
| Width | 5.3 | 3.0 | 5.1 | 3.1 | 6.7 | 0.83 | |
| Transesophageal echocardiogram | Length | 7.8 | 3.1 | 7.0 | 5.7 | 9.6 | 0.80 |
| Width | 5.9 | 1.9 | 5.3 | 5.0 | 6.2 | 1.00 | |
| CT scan | Length | 7.2 | 2.5 | 7.0 | 5.1 | 9.0 | 0.90 |
| Width | 5.9 | 2.0 | 5.6 | 4.2 | 7.0 | 0.80 | |
| MRI | Length | 6.6 | 2.5 | 6.7 | 4.6 | 8.5 | 1.00 |
| Width | 5.2 | 2.0 | 4.3 | 3.4 | 6.9 | 1.00 | |
| Surgery | Length | 9.2 | 4.3 | 8.0 | 6.6 | 11.6 | - |
| Width | 7.8 | 3.9 | 7.0 | 5.6 | 10.0 | - |
SD = standard deviation; Q1: first quartile; Q3: third quartile, CT: Computed Tomography,
MRI: Magnetic resonance imaging
Associated congenital anomalies
In this study, associated congenital anomalies were reported in 22 (12.4%) of the patients. Of the 22 patients, 5 (22.7%) had more than one congenital anomaly. Atrial septal defects were reported in 4 (2.2%) patients, and 2 other patients had defects combined with other congenital anomalies (1.1%). Mitral regurgitation was reported in another 4 (2.2%) patients. Ventricular septal defects were reported as single or combined with other congenital anomalies in 4 (2.2%) patients.
Treatment and prognosis
For the 177 patients analyzed, treatment information was available for 165 (93.2%) patients. Among the treatment modalities employed, LAAA resection was performed in 132 (74.5%) patients. The majority of LAAA resections (108 patients, 61.0%) were conducted via median sternotomy, 7 (3.9%) patients underwent lateral thoracotomy, 6 (3.4%) patients underwent mini-thoracotomy, and one patient (0.5%) underwent endoscopic resection. Notably, 13 (7.3%) patients underwent LAAA resection, but the specific method utilized was not specified in the available data. LAAA resection was accompanied by the Maze procedure in 13 (7.3%) patients, mitral valve repair/replacement in 6 (3.4%) patients, and radiofrequency ablation in 6 (3.4%) patients.
Of those patients who underwent LAAA resection and follow-up, 94 (94.9%) reported being asymptomatic, experiencing improved symptoms, or returning to sinus rhythm. However, 4 (4%) patients exhibited persistent or recurrent symptoms, and unfortunately, 1 (0.5%) patient died during the surgical procedure. In 33 (18.6%) patients, the treatment response was not mentioned.
In terms of additional procedures, ablation served as the sole treatment for three patients, one of whom experienced arrhythmia recurrence. Two (1.1%) patients opted for transcatheter closure of the LAAA, which reported clinical improvement and suggested an alternative approach to conventional surgical methods. Furthermore, 24 (13.5%) patients were managed solely with medical treatments such as antiarrhythmic and/or anticoagulant therapies. Unfortunately, the treatment response was not mentioned for 11 (6.2%) patients, either due to loss to follow-up or pending follow-up appointments. Of the remaining patients, 10 (5.6%) reported improved symptoms, one (0.5%) experienced a recurrence of arrhythmia, and 2 (1.1%) patients passed away—one after 4 weeks and the other after 10 years due to a cerebrovascular accident complicated by septicemia during hospitalization.
Histopathological findings and thrombus size
Histopathological findings were reported for 47 (26.5%) of the patients. Fibrosis was the most commonly reported histopathological finding in 34 (72.3%) patients. Other reported histopathological findings included hypertrophy in 9 (5.1%) patients, fatty infiltration in 2 (1.1%) patients, and dysplasia in 2 (1.1%) patients. The thrombus size was mentioned for 13 (7.3%) patients. The mean length was 3.3 ± 2.0 cm (the median was 3.0 [1.8, 4.9] cm), and the mean width was 3.8 ± 2.0 cm (the median was 3.1 [2.5, 4.8] cm).
Summary of case series of LAAAs case report
A summary of the LAAA case report’s case series is shown in Table 2. Patients reported a variety of symptoms, including dyspnea, palpitations, and CVA. CXR, TTE, TEE, CT, MRI, and catheterization were among the imaging modalities used for diagnosis. The aneurysms varied in size from 2.5 cm to 9.0 cm, and some of them had clots inside of them. The majority of patients underwent surgical resection, although some required further procedures and few denied therapies. While some patients’ symptoms subsided and their cardiac rhythms returned to normal, others’ symptoms persisted.
Table 2.
Table Summary of Case series of LAAAs
| Author(s) | Year | Age (years) | Gender (M/F) | Symptoms | Imaging Techniques | Key Findings | Treatment | Outcomes |
|---|---|---|---|---|---|---|---|---|
| Foale, R A et al. (55) | 1982 | 43 | F | CVA | CXR, TTE, Cath | 4.0 cm LAA aneurysm | Surgical resection | Not mentioned |
| Foale, R A et al. (55) | 1982 | 39 | F | Asymptomatic | CXR, TTE | 6.0 cm LAA aneurysm | Surgical resection | Not mentioned |
| Foale, R A et al. (55) | 1982 | 47 | F | Palpitations | CXR, TTE | 2.5 cm LAA aneurysm | Declined treatment | - |
| Burke, RP et al. (120) | 1992 | 37 | M | CVA, AFib | CXR, TTE, Cath | 9.0 × 6.0 cm LAA aneurysm | Surgical resection | Normal rhythm |
| Burke, RP et al. (120) | 1992 | 29 | M | Dyspnea, chest pain | CXR, TEE | 4.0 × 6.0 cm LAA aneurysm | Surgical resection | Asymptomatic |
| Gajjar T, Desai N (88) | 2011 | 29 | M | Dyspnea | CXR, CT | LAA aneurysm | Not mentioned | - |
| Gajjar T, Desai N (88) | 2011 | 48 | M | Dyspnea | CXR, CT | LAA aneurysm | Not mentioned | - |
| Mirmohammadsadeghi M et al. (84) | 2013 | 30 | F | Fatigue | CXR, TTE, TEE, CT angio | 5.0 × 4.0 cm LAA aneurysm filled with clots | Surgical resection | Not mentioned |
| Mirmohammadsadeghi M et al. (84) | 2013 | 46 | M | CVA | TTE | 5.0 × 4.0 cm LAA aneurysm filled with clots | Surgical resection | Not mentioned |
| Kuiten W et al. (114) | 2013 | 69 | M | Dyspnea, AFib | CT, TTE | 7.0 × 5.5 cm LAA aneurysm | Surgical resection, electrical cardioversion and amiodarone | Persistent AFib |
| Kuiten W et al. (114) | 2013 | 39 | M | CVA, palpitations | CXR, TTE, TEE, CT MRI | 7.0 × 7.0 cm LAA aneurysm | Surgical resection | Normal rhythm |
| Zhang X et al. (138) | 2020 | 4 | F | Abnormal CXR | CXR, TTE | 3.8 × 1.8 cm LAA aneurysm | Declined treatment | - |
| Zhang X et al. (138) | 2020 | 3 | M | Abnormal CXR | CXR, TTE, TEE, MRI | 4.5 × 3.2 cm LAA aneurysm | Surgical resection | Correction of LAAA |
| Zhang X et al. (138) | 2020 | 0.3 | F | Abnormal CXR | CXR, TTE | 3.8 × 2.2 cm LAA aneurysm | Declined treatment | - |
| Zhang X et al. (138) | 2020 | 9 | F | Abnormal TTE after mitral valvuloplasty | TTE | 3.3 × 1.9 cm LAA aneurysm | Surgical resection | Not mentioned |
| Zhang X et al. (138) | 2020 | 1 | F | Rapid heart rate | TTE | 2.9 × 1.1 cm LAA aneurysm | Surgical resection | Correction of LAAA |
| Sharifuzzaman M et al. (27) | 2021 | 18 | F | Palpitation, chest pain | CXR, TTE | 6.0 × 9.9 cm LAA aneurysm | Surgical resection | Asymptomatic |
| Sharifuzzaman M et al. (27) | 2021 | 5 | M | Palpitations | CXR, TTE | LAA aneurysm | Surgical resection | Not mentioned |
M: Male, F: Female, CVA: Cerebrovascular accident, CXR: Chest X-ray, TTE: Transthoracic Echocardiogram, TEE: Transesophageal Echocardiography, Afib: Atrial Fibrillation, CT: Computed Tomography, MRI: Magnetic Resonance Imaging
Factors associated with presence of arrythmia and thrombus in left atrial appendage aneurysm
The chi-square test and Fisher’s exact test showed that the presence of arrythmia was significantly associated with older age, male sex, and the presence of thrombus in LAAA (Table 3).
Table 3.
Associations between the presence of arrhythmia and demographic and clinical variables
| Absence of arrhythmia | Presence of arrhythmia | |||||
|---|---|---|---|---|---|---|
| Variable | n | % | n | % | Chi-square/Fisher’s exact test | p value |
| Age category | ||||||
| Pediatric | 42 | 23.8 | 17 | 9.6 | 20.4 | < 0.001 |
| Adult | 42 | 23.8 | 64 | 36.1 | ||
| Elderly | 2 | 1.1 | 10 | 5.6 | ||
| Gender | ||||||
| Male | 30 | 9.8 | 55 | 31.1 | 11.7 | 0.003 |
| Female | 55 | 17.2 | 35 | 19.8 | ||
| Not Mentioned | 1 | 0.6 | 1 | 0.6 | ||
| Presence of thrombus in left atrial appendage aneurysm | ||||||
| Yes | 11 | 6.2 | 28 | 15.8 | 8.1 | 0.006 |
| No | 76 | 43 | 62 | 35 | ||
P < 0.05 was considered to indicate statistical significance
When these variables were retained in a multivariate logistic model (Table 4), older patients were 5.1-fold (95% CI: 2.3–11.4) more likely to have arrythmia compared to younger patients, male patients were 4.4-fold (95% CI: 2.1–9.1) more likely to have arrythmia compared to female patients, and patients who had thrombus in the LAAA were 3.0-fold (95% CI: 1.3–6.9) more likely to have arrythmia compared to the patients who did not have thrombus in the LAAA. The patients who received anticoagulants were less likely to have thrombus in LAAA (Fisher’s exact test = 11.6, p = 0.001). The chi-square test and Fisher’s exact test showed that the presence of thrombus in LAAA was significantly associated with mortality, older age, and the presence of arrythmia (Table 5).
Table 4.
Multivariate logistic model for identifying the predictors of arrhythmia
| 95% CI for OR | |||||||
|---|---|---|---|---|---|---|---|
| Variable | β | SE | Wald | p value | OR | Lower | Upper |
| Age | 1.63 | 0.41 | 15.67 | < 0.001 | 5.1 | 2.3 | 11.4 |
| Gender | 1.48 | 0.37 | 16.29 | < 0.001 | 4.4 | 2.1 | 9.1 |
| Presence of thrombus in left atrial appendage aneurysm (n = 39) | 1.10 | 0.42 | 6.73 | 0.009 | 3.0 | 1.3 | 6.9 |
SE = standard error; CI = confidence interval; OR = odds ratio
Table 5.
Associations between the presence of thrombus in left atrial appendage aneurysms and demographic and clinical variables
| Absence thrombus in left atrial appendage aneurysm | Presence of thrombus in left atrial appendage aneurysm | |||||
|---|---|---|---|---|---|---|
| Variable | n | % | n | % | Chi-square/Fisher’s exact test | p value |
| Mortality | ||||||
| No | 138 | 78 | 36 | 20.3 | 10.4 | 0.011 |
| Yes | 0 | 0.0 | 3 | 1.7 | ||
| Age category | ||||||
| Pediatric | 51 | 28.8 | 8 | 4.5 | 4.8 | 0.091 |
| Adult | 80 | 45.2 | 26 | 14.7 | ||
| Elderly | 7 | 4 | 5 | 2.8 | ||
| Presence of arrythmia | ||||||
| No | 76 | 43 | 11 | 6.2 | 8.1 | 0.006 |
| Yes | 62 | 35 | 28 | 15.8 | ||
We observed a significant association between the presence of tachyarrhythmias and various clinical outcomes. Specifically, patients with tachyarrhythmias were more likely to experience adverse outcomes such as recurrent atrial flutter and persistent atrial fibrillation, compared to those without arrhythmias. For example, of the patients with tachyarrhythmias, 33.3% showed persistent arrhythmias or recurrence of atrial flutter, while 50% experienced stable sinus rhythm post-treatment. In contrast, patients without tachyarrhythmias more frequently achieved asymptomatic states and stable sinus rhythms following treatment, with 62.5% showing complete resolution of symptoms.
Discussion
This systematic review provides a comprehensive assessment of 177 cases of LAAA, a rare condition characterized by localized or diffuse dilation of the left atrial appendage. We found a slight predominance in female patients (50.9%), with a mean age of 29.7 years. The most common presenting symptoms were palpitations, shortness of breath, and thromboembolic events. Transthoracic and transesophageal echocardiograms were the preferred diagnostic modalities, and surgical resection emerged as the most frequently utilized treatment, with favorable prognoses. Older age and the presence of arrhythmia were significantly associated with thrombus formation and embolic events. There was a role of tachyarrhythmias in shaping clinical outcomes for patients with LAAA. Patients with tachyarrhythmias were more likely to experience recurrent atrial flutter or persistent atrial fibrillation, suggesting that the presence of arrhythmias in LAAA patients may indicate a more severe disease course or complications such as thrombus formation. Furthermore, our results indicate that achieving stable sinus rhythm is a key determinant of favorable outcomes, with patients without tachyarrhythmias showing higher rates of symptom resolution and overall improvement.
LAAA is a rare condition with significant clinical implications, yet knowledge regarding its etiology, presentation, and management remains limited. The first documented case of LAAA dates back to 1962 by Parmley LF Jr. [6], and only 177 cases have been reported in the literature since then. LAAA can either be congenital or acquired, with congenital LAAA arising from abnormalities such as pectinate muscle dysplasia, whereas acquired LAAA is associated with left atrial enlargement due to mitral valve diseases or other myocardial pathologies [158].
Depending on where it occurs, LAAA can alternatively be categorized as extrapericardial or intrapericardial. Left atrial appendage weakening leads to the intrapericardial form, and the following diagnostic requirements have been proposed: origination from an apparently healthy atrial chamber, clear connection to the atrial cavity, situated inside the pericardium, and aneurysm disruption of the left ventricle [44]. The extrapericardial kind is connected to a pericardial defect that can herniate and develop into aneurysmal dilatation. It is well recognized that the extrapericardial variant has a better prognosis [175]. Despite these criteria for categorizing LAAA types, it is usually difficult to distinguish them clearly in many cases.
Our findings indicated that LAAA can present at any age, although the majority of cases occur in the second or third decade of life. The introduction of fetal echocardiography has made it possible to diagnose LAAA prenatally, emphasizing the importance of early detection to prevent complications. Despite a slight female predominance, the risk factors for the development of LAAA are not well understood, and more extensive studies are needed to identify predisposing factors for this condition.
The clinical presentation of LAAA is heterogeneous, with a significant number of patients remaining asymptomatic. When symptoms occur, palpitations, shortness of breath, and thromboembolic events are most common. Determining whether these symptoms are directly caused by LAAA or related to underlying cardiac disorders can be challenging, as LAAA may serve as a substrate for atrial tachyarrhythmias or contribute to arrhythmias through abnormalities in the conduction system. However, no study has definitively established the role of LAAA in the origin of atrial arrhythmias using electrophysiological investigations, leaving a gap in the understanding of the arrhythmogenic potential of LAAA [171].
Additionally, associated abnormalities in the conduction system can contribute to the development of arrhythmias. However, no study has definitively established the origin of atrial arrhythmias specifically from LAAA using electrophysiological investigations. Less commonly, it can irritate the left phrenic nerve, which causes hiccups [116], and push the left recurrent laryngeal nerve, creating a persistent cough [176]. In the majority of cases, the physical examination results appear normal or may reveal certain findings, such as systolic murmurs (most commonly), focal neurological deficits, irregular-irregular pulses, or tachycardia.
Diagnosing LAAA can be challenging due to the nonspecific nature of most symptoms. Initial diagnostic tests commonly used include CXR and ECG analyses. While these tests lack specificity, they can show certain abnormalities that are often observed in the majority of patients, such as a prominent left heart border on CXR and the presence of atrial fibrillation and/or flutter on ECG. In patients with LAAA, chest X-ray revealed a mass-like enlargement in 98.5% of patients. This finding indicates that CXR is an excellent initial workup for these patients. Furthermore, such findings on CXR and ECG should prompt physicians to perform a more specific form of imaging.
In the cases documented in the literature, TTE, TEE, CT scan, cardiac MRI, and cardiac catheterization were the most frequently used cardiac imaging modalities. With 65% sensitivity, TTEs can be somewhat useful for diagnosis. However, TTE results frequently characterize LAAA as echo-free structures, cysts, cavities, or masses, requiring additional diagnostic testing. Since cardiac catheterization is invasive and has been superseded by safer alternatives, it is the least commonly used diagnostic technique. With their high sensitivity (93.9%) and ability to perform enhanced anatomical detail imaging, CT scans enable the investigation of congenital anomalies and the relationship between LAAA and surrounding tissues. TEE and cardiac MRI had the highest sensitivities for diagnosing LAAA (95.6% and 96.9%, respectively). These parameters are useful for detecting thrombi and are strongly correlated with the length and diameter of the LAAA, as measured post-surgery.
Surgery is the main treatment modality for LAAA, whether symptomatic or not. Various effective techniques, including median sternotomy, left thoracotomy, mini-thoracotomy, and minimally invasive endoscopic approaches, have been reported for aneurysmectomy. Recently, a unique noninvasive method of transcatheter closure for LAAA was described [156]. In our study, surgical resection was performed in more than 75% of the patients. Histopathologic examination of LAAA tissue revealed fibrosis in most patients. Less commonly, hypertrophy, fatty infiltration, or dysplasia can be observed. Generally, the prognosis following surgical resection is favorable, with a success rate of 94.9% and minimal complications in patients with a reported follow-up. Only 4% of patients experienced persistent or recurrent symptoms, and one patient died during the surgical procedure [59].
We found that mortality due to LAAA is significantly associated with the presence of a thrombus. The presence of a thrombus is associated with the presence of arrhythmia, older age, and male sex. For individuals who are not suitable for surgery, medical management should focus on treating atrial tachyarrhythmia and thromboembolic complications. Mortality was reported in two patients treated with medical therapy [48, 107]. However, it is not possible to compare the outcomes of surgical and medical management, as most patients treated medically are either lost to follow-up or pending follow-up appointments.
In cases where a preoperative or intraoperative echocardiogram detects a thrombus or a large LAAA, cardiopulmonary bypass is used to minimize the risk of thrombus dislodgement during aneurysm manipulation. Minimally invasive endoscopic techniques can safely remove LAAAs without left atrial or appendage thrombi, effectively eliminating the risk of thromboembolism and tachyarrhythmia. However, resection of giant LAAAs may result in dysmorphic atrial tissue, increasing the likelihood of atrial tachyarrhythmia. Therefore, for patients with large LAAAs, atrial fibrillation, or biatrial enlargement, concurrent consideration of Cox-Maze III type or other ablative procedures during LAAA resection is recommended [177].
Limitations
We must acknowledge several constraints in our research. Our review was limited to studies available in the English language. Moreover, this review was based on a retrospective analysis of cases reported in the existing literature, which introduces an inherently high risk of bias associated with case reports and case series. These types of studies often have limited sample sizes, a lack of control groups, and are subject to publication bias, where more unusual or positive outcomes are preferentially reported. Additionally, the statistical analysis conducted in this review involved data pooled from different reports. The variability in data suggests potential heterogeneity, which may be due to differences in performed interventions and outcome measures. As such, the results reported in this review should be interpreted cautiously, considering the presence of this heterogeneity. Another important limitation is the limited number of reports on large LAAA. The accumulation of more data in the future could allow for a comprehensive meta-analysis. It is also important to note that asymptomatic cases of LAAA may go unnoticed, resulting in an underrepresentation of the broader patient population with LAAA. Furthermore, the absence of a universally accepted definition for LAAA adds to the complexity and potential inconsistencies in our findings.
Conclusion
LAAA is a rare condition characterized by the expansion of the left atrial appendage. It can be congenital or acquired, gradually increasing in size and posing a risk of thromboembolism. Surgical intervention is crucial for managing LAAA, for which favorable outcomes have been reported. LAAA may coexist with other congenital anomalies. Currently, diagnostic imaging, such as echocardiography and MRI, can play a key role in the evaluation of LAAAs. Based on the pooled data, MRI and TEE showed an excellent degree of correlation to post-surgical LAAA dimensions when compared to other modalities. More data are still needed to allow drawing more solid conclusions on the best ways to evaluate LAAA and optimize treatment strategies.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
Not applicable.
Abbreviations
- LAA
Left Atrial Appendage
- LAAA
Left Atrial Appendage Aneurysm
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- INPLASY
International Platform of Registered Systematic Review and Meta-Analysis Protocols
- SPSS
Statistical Package for the Social Sciences
- CXR
Chest X-ray
- ECG
Electrocardiography
- TTE
Transthoracic Echocardiogram
- TEE
Transesophageal Echocardiography
- CT
Computed Tomography
- MRI
Magnetic Resonance Imaging
- CVA
Cerebrovascular accident
Author contributions
All authors contributed to the study’s conception and design. SA, AO, and MA were involved in literature review, screening, and data extraction. RS conducted the statistical analysis. The initial draft of the manuscript was written by AO/SA, and all authors provided comments on previous versions. YD oversaw each stage of the study and provided the required comments when needed. All authors read, reviewed, and approved the final manuscript.
Funding
The authors declare that they did not receive any financial support for the conduct of this research.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Al-Saady NM, Obel OA, Camm AJ. Left atrial appendage: structure, function, and role in thromboembolism. Heart. 1999;82(5):547–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Blackshear JL, Odell JA. Appendage obliteration to reduce stroke in cardiac surgical patients with atrial fibrillation. Ann Thorac Surg. 1996;61(2):755–9. [DOI] [PubMed] [Google Scholar]
- 3.Wilber DJ. Neurohormonal Regulation and the left atrial appendage: still more to learn. J Am Coll Cardiol. 2018;71(2):145–7. [DOI] [PubMed] [Google Scholar]
- 4.Odell JA, Blackshear JL, Davies E, Byrne WJ, Kollmorgen CF, Edwards WD, et al. Thoracoscopic obliteration of the left atrial appendage: potential for stroke reduction? Ann Thorac Surg. 1996;61(2):565–9. [DOI] [PubMed] [Google Scholar]
- 5.Beigel R, Wunderlich NC, Ho SY, Arsanjani R, Siegel RJ. The left atrial appendage: anatomy, function, and noninvasive evaluation. JACC Cardiovasc Imaging. 2014;7(12):1251–65. [DOI] [PubMed] [Google Scholar]
- 6.Parmley LF. Congenital atriomegaly. Circulation. 1962;25:553–8. [DOI] [PubMed] [Google Scholar]
- 7.Beinart R, Heist EK, Newell JB, Holmvang G, Ruskin JN, Mansour M. Left atrial appendage dimensions predict the risk of stroke/TIA in patients with atrial fibrillation. J Cardiovasc Electrophysiol. 2011;22(1):10–5. [DOI] [PubMed] [Google Scholar]
- 8.Lee JM, Shim J, Uhm JS, Kim YJ, Lee HJ, Pak HN, et al. Impact of increased orifice size and decreased flow velocity of left atrial appendage on stroke in nonvalvular atrial fibrillation. Am J Cardiol. 2014;113(6):963–9. [DOI] [PubMed] [Google Scholar]
- 9.JBI Critical Appraisal Tools | JBI [Internet]. [cited 2024 Oct 5]. https://jbi.global/critical-appraisal-tools
- 10.Sbarouni E, Kogerakis N, Stavridis G. 68-year-old woman with paroxysmal atrial fibrillation. Heart. 2018. heartjnl-2018-314143. [DOI] [PubMed]
- 11.Coraducci F, Belleggia S, Torselletti L, Coretti F, Valeri Y, Maiorino F, et al. 510 Giant left atrial appendage aneurysm in a 47 years old male: a case report. Eur Heart J Suppl. 2021;23(SupplementG):suab133008. [Google Scholar]
- 12.Das N, Tadros SS, DeBrunner M. A case of a left atrial appendage disguised as a coronary artery aneurysm. CASE Cardiovasc Imaging Case Rep. 2021;5(5):305–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ford C, O’Brien JM, Irvin D, Chow J, Chandrasekhar J, A CASE OF, GIANT LEFT ATRIAL APPENDAGE WITH ATRIAL FIBRILLATION MASQUERADING AS SYMPTOMATIC PERICARDIAL EFFUSION. J Am Coll Cardiol. 2021;77(18):2689. [Google Scholar]
- 14.Haydin S. A giant aneurysm of the left atrial appendage in childhood. Turk J Thorac Cardiovasc Surg. 2014;22:171–3. [Google Scholar]
- 15.Sarin SS, Bindra T, Chhabra GS. A giant left atrial appendage aneurysm with a large pinball-like thrombus in a 2 year old. Ann Pediatr Cardiol. 2012;5(2):215–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang HQ, Zhang Z, Yang H, Wu S, Fu YH, Song ZM, et al. A huge congenital left atrial appendage Aneurysm. Chin Med J (Engl). 2017;130(24):3011–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Di Salvo G, Al-Sehly A, Fadley FA, Bulbul ZA, Fadel BM, Fayyadh MA, et al. A rare case of giant congenital left atrial appendage aneurysm in a 4-month-old child. J Cardiovasc Med. 2017;18(9):723. [DOI] [PubMed] [Google Scholar]
- 18.Dye L, Freed JK, Leschke JR, Pagel PS. A Rare cause of intermittent Dyspnea, Occasional palpitations, and atypical chest discomfort. J Cardiothorac Vasc Anesth. 2018;32(4):2031–3. [DOI] [PubMed] [Google Scholar]
- 19.Sevimli S, Gundogdu F, Aksakal E, Arslan S, Gurlertop Y, Senocak H. A rare congenital anomaly: biatrial appendage aneurysm with atrial and ventricular septal defect. Echocardiogr Mt Kisco N. 2007;24(9):987–90. [DOI] [PubMed] [Google Scholar]
- 20.Aydin Sahin D, Vefa Yildirim S, Ozkan M. A rare giant congenital left atrial appendage aneurysm in a 1-day-old newborn. Echocardiography. 2018;35(5):757–9. [DOI] [PubMed] [Google Scholar]
- 21.Evangeliou AP, Sotiroglou E, Charitakis N, Loufopoulos G, Varassas C, Papadopoulos S, et al. An asymptomatic patient with an additional Cardiac Chamber Giant Left Atrial Appendage. Case Rep Cardiol. 2020;2020:6519089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yıldırım I. An incidentally diagnosed asymptomatic congenital left atrial appendage aneurysm. Turk J Thorac Cardiovasc Surg. 2014;22(2):407–9. [Google Scholar]
- 23.DeSena HC, Niyazov DM, Parrino PE, Lucas VW, Shah SB, Moodie DS. An unusual Cardiac defect in a patient with clinical features overlapping between Cardiofaciocutaneous and Noonan syndromes. Congenit Heart Dis. 2010;5(1):70–5. [DOI] [PubMed] [Google Scholar]
- 24.Sauza-Sosa JC, De la Cruz-Reyna EL, Velazquez-Gutierrez CN. An unusual congenital heart disease: Giant Left Atrial Appendage. Methodist DeBakey Cardiovasc J 18(2):106–7. [DOI] [PMC free article] [PubMed]
- 25.Yao R, Hunsaker RP, Gelman B. An unusual echocardiogram. J Cardiothorac Vasc Anesth. 2008;22(4):636–8. [DOI] [PubMed] [Google Scholar]
- 26.Guignan C, Guerra Marcano F, Ramírez C. Aneurysm left atrial appendage. Cardiometry. 2017;77–9.
- 27.Mak MS, Biswas A, Nah PKAM. Aneurysm of left atrial appendage: report of two repaired cases. Bangladesh Heart J. 2021;36(2):158–63. [Google Scholar]
- 28.Krishnamoorthy KM. Aneurysm of the Left Atrial Appendage. Cardiology. 2002;97(4):233–4. [DOI] [PubMed] [Google Scholar]
- 29.Pomerantzeff PMA, Freyre HM, de Almeida Brandão CM, Pereira Barreto AC, Almeida de Oliveira S. Aneurysm of the left atrial appendage. Ann Thorac Surg. 2002;73(6):1981–3. [DOI] [PubMed] [Google Scholar]
- 30.van der Hauwaert LG, Dumoulin M, Daenen W, Stalpaert G. Aneurysm of the left atrial appendage. Clin Cardiol. 1979;2(1):49–51. [DOI] [PubMed] [Google Scholar]
- 31.Victor S, Nayak VM. Aneurysm of the Left Atrial Appendage. Tex Heart Inst J. 2001;28(2):111–8. [PMC free article] [PubMed] [Google Scholar]
- 32.Lipkin D, Colli A, Somerville J. Aneurysmal dilatation of left atrial appendage diagnosed by cross sectional echocardiography and surgically removed. Br Heart J. 1985;53(1):69–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Parker JO, Gonnell WF. Aneurysmal dilatation of the left atrial appendage. Am J Cardiol. 1965;16(3):438–41. [DOI] [PubMed] [Google Scholar]
- 34.Yakut K, Varan B, Erdoğan İ. Asymptomatic giant congenital left atrial aneurysm. Turk J Pediatr. 2019;61(1):117–9. [DOI] [PubMed] [Google Scholar]
- 35.Othman N, Yunus A, Mahmod M. Asymptomatic left atrial appendage Aneurysm. Int J Clin Cardiol. 2015;2.
- 36.Ota C, Kimura M, Kitami M, Kure S. Asymptomatic left atrial appendage aneurysm (LAAA) with pericardial defect in a 1-year-old girl. BMJ Case Rep. 2018;2018:bcr2018224573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hof IE, Wildbergh TX, van Driel VJ, Wittkampf FH, Cramer MJ, Meine M, et al. Atrial fibrillation with a giant left atrial appendage can be successfully treated with pulmonary vein antrum isolation. Neth Heart J. 2012;20(4):179–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wagshal AB, Applebaum A, Crystal P, Goldfarb B, Erez A, Tager S, et al. Atrial Tachycardia as the Presenting sign of a left atrial appendage Aneurysm. Pacing Clin Electrophysiol. 2000;23(2):283–5. [DOI] [PubMed] [Google Scholar]
- 39.Nagai T, Higaki J, Okayama H. Atrial tachycardia in congenital left atrial appendage aneurysm: three-dimensional computed tomography imaging with electro-anatomical mapping. Eur Heart J. 2010;31(13):1590–1590. [DOI] [PubMed] [Google Scholar]
- 40.Nakahara T, Minakata K, Yamazaki K, Funamoto M, Sakata R. Bilateral atrial appendage aneurysms associated with atrial fibrillation. Asian Cardiovasc Thorac Ann. 2014;22(3):347–9. [DOI] [PubMed] [Google Scholar]
- 41.Pradella M, Mozer AB, Baraboo JJ, Narang A, Gong FF, Budd AN, et al. Blood Flow Dynamics in a Giant Left Atrial Appendage Aneurysm visualized by 4D-Flow CMR. JACC Case Rep. 2021;3(18):1924–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gan GCH, Bhat A, Desai H, Eshoo S. Cardiac Vignette: Giant Left Atrial Appendage Aneurysm. Heart Lung Circ. 2015;24(7):e81–5. [DOI] [PubMed] [Google Scholar]
- 43.Ozmen CA, Alyan O, Altintaş B, Karahan Z. Case images: visualization of a giant left atrial aneurysm by multidetector computed tomography and echocardiography. Turk Kardiyol Dernegi Arsivi Turk Kardiyol Derneginin Yayin Organidir. 2009;37(1):76. [PubMed] [Google Scholar]
- 44.Li R, Ma F, Guan HX, Pan YY, Liu LG, Wang DW, et al. Case Report: giant congenital left atrial appendage Aneurysm presenting with Acute massive cerebral infarction and refractory atrial fibrillation: a Case Report and Literature Review. Front Cardiovasc Med. 2022;9:888825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yoshihara S, Yaegashi T, Matsunaga M, Naito M. Chicken-wing type congenital left atrial appendage aneurysm. Kardiol Pol. 2021;79(2):199–200. [DOI] [PubMed] [Google Scholar]
- 46.Saygi M, Ergul Y, Guzeltas A. Combination of congenital left atrial appendage aneurysm in an infant with transposition of the great arteries: a previously unreported association. Cardiol Young. 2015;25(7):1377–8. [DOI] [PubMed] [Google Scholar]
- 47.Halas RF, Schmehil CJ, Ten Eyck GR, Loker JL. Congenital aneurysm of both left ventricle and left atrium. Ann Pediatr Cardiol. 2018;11(1):97–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bramlet DA, Edwards JE. Congenital aneurysm of left atrial appendage. Br Heart J. 1981;45(1):97–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shaheen F, Gojwari T, Ahmad N. Congenital aneurysm of left atrial appendage presenting as young stroke: CT &MR findings. Eur J Radiol Extra. 2008;68(3):e107–9. [Google Scholar]
- 50.Gupta S, Agarwal S, Pratap H, Datt V, Banerjee A. Congenital aneurysm of left atrial appendage: a case report. J Card Surg. 2010;25(1):37–40. [DOI] [PubMed] [Google Scholar]
- 51.de la Fuente A, Urchaga A, Sánchez R, Fernández JL, Moriones I. Congenital aneurysm of the left atrial appendage. Ann Thorac Surg. 2008;85(6):2139–40. [DOI] [PubMed] [Google Scholar]
- 52.Munárriz A, Escribano E, Urchaga A, Olaz F, Beunza M, de La Fuente A, et al. Congenital aneurysm of the left atrial appendage. Eur J Echocardiogr J Work Group Echocardiogr Eur Soc Cardiol. 2008;9(1):152–4. [DOI] [PubMed] [Google Scholar]
- 53.Zokaei AH, Sabzi F. Congenital aneurysm of the Left Atrial Appendage with Left superior Vena Cava. Clin Med Insights Ther. 2011;3:CMT.S7558.
- 54.Robinson PJ, Neutze JM, Brandt PW, Hill DG, Anderson RJ, Rutland MD. Congenital aneurysm of the left atrium: diagnosis and management. Aust N Z J Med. 1984;14(3):267–9. [DOI] [PubMed] [Google Scholar]
- 55.Foale RA, Gibson TC, Guyer DE, Gillam L, King ME, Weyman AE. Congenital aneurysms of the left atrium: recognition by cross-sectional echocardiography. Circulation. 1982;66(5):1065–9. [DOI] [PubMed] [Google Scholar]
- 56.Lekkerkerker JC, Jaarsma W, Cramer MJM. Congenital giant aneurysm of the left atrial appendage. Heart. 2005;91(3):e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bhattarai A, Padalino MA, Stellin G. Congenital giant aneurysm of the left atrial appendage in an infant. Cardiol Young. 2011;21(6):697–9. [DOI] [PubMed] [Google Scholar]
- 58.Kunishima T, Musha H, Yamamoto T, Aoyagi H, Kongoji K, Imai M, et al. Congenital Giant Aneurysm of the Left Atrial Appendage Mimicking Pericardial absence. Jpn Circ J. 2001;65(1):56–9. [DOI] [PubMed] [Google Scholar]
- 59.Akhtar P, Habib S, Hussain M, Tasneem H, Hussain A, Rasool I, CONGENITAL GIANT ANEURYSM OF THE LEFT ATRIAL APPENDAGE: DIAGNOSIS AND MANAGEMENT. Pak Heart J [Internet]. 2007 [cited 2023 Jun 24];40(1–2). https://pakheartjournal.com/index.php/pk/article/view/44
- 60.Rafighdoust AA, Hamedanchi A, Mirzaei A, CONGENITAL GIANT INTRAPERICARDIAL ANEURYSM OF LEFT. ATRIAL APPENDAGE: A VERY RARE BUT POTENTIALLY DANGEROUS ENTITY. Iran Heart J. 2003;4(4):75–8. [Google Scholar]
- 61.Chen Y, Mou Y, Jiang LJ, Hu SJ. Congenital giant left atrial appendage aneurysm: a case report. J Cardiothorac Surg. 2017;12:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Pomé G, Pelenghi S, Grassi M, Vignati G, Pellegrini A. Congenital intrapericardial aneurysm of the left atrial appendage. Ann Thorac Surg. 2000;69(5):1569–71. [DOI] [PubMed] [Google Scholar]
- 63.Ganeshakrishnan KI, Khandeparkar JM, Natrajan VM, Agrawal NB, Oswal DH, Magotra RA. Congenital intrapericardial aneurysm of the left-atrial appendage. Thorac Cardiovasc Surg. 1992;40(6):382–4. [DOI] [PubMed] [Google Scholar]
- 64.Coselli JS, Beall AC, Ziaddi GM. Congenital intrapericardial aneurysmal dilatation of the left atrial appendage. Ann Thorac Surg. 1985;39(5):466–7. [DOI] [PubMed] [Google Scholar]
- 65.Atchison FW, Rehfeldt KH. Congenital left atrial appendage Aneurysm. Anesth Analg. 2011;112(6):1303. [DOI] [PubMed] [Google Scholar]
- 66.Selvaraj T, Kapoor PM, Krishna M, Kiran U, Chowdhury U, Seth S. Congenital left atrial appendage aneurysm. Ann Card Anaesth. 2008;11(1). [DOI] [PubMed]
- 67.Tidake A, Gangurde P, Mahajan A. Congenital left atrial appendage aneurysm associated with a systemic embolism. Cardiol Young. 2015;25(3):597–9. [DOI] [PubMed] [Google Scholar]
- 68.Cho MJ, Park JA, Lee HD, Choo KS, Sung SC. Congenital left atrial appendage aneurysm diagnosed by fetal echocardiography. J Clin Ultrasound JCU. 2010;38(2):94–6. [DOI] [PubMed] [Google Scholar]
- 69.Kühn A, Schreiber C, Vogt M. Congenital left atrial appendage aneurysm in a 2-year-old boy. Eur Heart J. 2006;27(8):959. [DOI] [PubMed] [Google Scholar]
- 70.Comess KA, Labate DP, Winter JA, Hill AC, Miller DC. Congenital left atrial appendage aneurysm with intact pericardium: diagnosis by transesophageal echocardiography. Am Heart J. 1990;120(4):992–6. [DOI] [PubMed] [Google Scholar]
- 71.Kwan CM, Tsai LM, Lin LJ, Yang YJ, Chen JH. Congenital left atrial appendage aneurysm with thrombus formation: diagnosis by transesophageal echocardiography. J Clin Ultrasound. 1993;21(7):480–3. [DOI] [PubMed] [Google Scholar]
- 72.Low ZK, Yap KH, Fortier MV, Nakao M. Congenital left atrial appendage aneurysm with unexpected course of left anterior descending coronary artery. Interact Cardiovasc Thorac Surg. 2020;32(3):495–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Chowdhury UK, Seth S, Govindappa R, Jagia P, Malhotra P. Congenital left atrial appendage aneurysm: a case report and brief review of literature. Heart Lung Circ. 2009;18(6):412–6. [DOI] [PubMed] [Google Scholar]
- 74.Wang B, Li H, Zhang L, He L, Zhang J, Liu C, et al. Congenital left atrial appendage aneurysm: a rare case report and literature review. Med (Baltim). 2018;97(2):e9344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Goyal K, Kayakkal S, Muneer K, Nair R, Sajeev C. Congenital left atrial appendage aneurysm: a treacherous extra chamber. Heart India. 2017;5(2):96–8. [Google Scholar]
- 76.Bamous M, Aithoussa M, Abetti A, Boulahya A. Congenital left atrial appendage aneurysm: atypical presentation. Ann Pediatr Cardiol. 2017;10(3):293–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Su X, Yang F, Yu D, He X. Congenital left atrial appendage aneurysm: prenatal diagnosis and outcome of a rare cardiac abnormality. Echocardiography. 2021;38(3):480–3. [DOI] [PubMed] [Google Scholar]
- 78.Marla J, Marla NJ, Tantri G, Jayaprakash C. Congenital-left atrial appendage Aneurysm in an 8-Year-old girl. J Clin Diagn Res. 2012;6(6):1073–5. [Google Scholar]
- 79.Gold JP, Afifi HY, Ko W, Horner N, Hahn R. Congential giant aneurysms of the left atrial appendage: diagnosis and management. J Card Surg. 1996;11(2):147–50. [DOI] [PubMed] [Google Scholar]
- 80.Yanli Z, Xiaocong W, Liping P, Yan M, Wei Y, Shu J. Diagnosis of a giant left atrial appendage aneurysm by contrast-enhanced echocardiography: case report and literature review. J Clin Ultrasound. 2021;49(3):293–7. [DOI] [PubMed] [Google Scholar]
- 81.Ruttkay T, Scheid M, Gotte J, Doll N. Endoscopic resection of a Giant Left Atrial Appendage. Innovations. 2015;10(4):282–4. [DOI] [PubMed] [Google Scholar]
- 82.Vagefi PA, Choudhry M, Hilgenberg AD. Excision of an aneurysm of the left atrial appendage. J Thorac Cardiovasc Surg. 2007;133(3):822–e8231. [DOI] [PubMed] [Google Scholar]
- 83.Oda S, Nakano T, Kado H. Expansion of a huge Compressive Left Atrial Appendage Aneurysm in a 29-Day-old infant. Ann Thorac Surg. 2020;110(6):e521–3. [DOI] [PubMed] [Google Scholar]
- 84.Mirmohammadsadeghi M, Kiani Y, Nasr A, Zavvar R, Behjati M, Rabbani M, et al. Five chambered heart or large atrial appendage aneurysm: a report of two cases. ARYA Atheroscler. 2013;9(3):213–5. [PMC free article] [PubMed] [Google Scholar]
- 85.Nezafati MH, Nazari Hayanou H, Kahrom M, Khooei A, Nezafati P. Five chambered heart: case of a huge left atrial appendage aneurysm. Cardiovasc Pathol. 2018;34:43–5. [DOI] [PubMed] [Google Scholar]
- 86.Plonska-Gosciniak E, Larysz B, Jurczyk K, Kasprzak JD. Five-chambered heart: a 20-year story of left atrial appendage aneurysm. Eur Heart J. 2009;30(8):1014. [DOI] [PubMed] [Google Scholar]
- 87.Sawicki KT, Mehta CK, Silverberg RA. Five-Chambered Heart: palpitations and Syncope due to a left atrial appendage Aneurysm. Circ Cardiovasc Imaging. 2021;14(12):1147–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Gajjar T, Desai N. Giant aneurysm of left atrial appendage — a rare anomaly. Eur J Cardiothorac Surg. 2011;40(5):1270. [DOI] [PubMed] [Google Scholar]
- 89.Zhang PF, Zhang M, Zhang W, Yao GH, Wu SM, Zhang Y. Giant aneurysm of the Left Atrial Appendage detected by real-time 3-Dimensional Echocardiography. Tex Heart Inst J. 2010;37(1):129–30. [PMC free article] [PubMed] [Google Scholar]
- 90.Kissami I, El Ouazzani G, El Bekkaoui M, Skiker I, Elouafi N, Bazid Z. Giant aneurysm of the left atrial appendage: a case report of a rare cause of dyspnea in a 55-year old woman. Ann Med Surg. 2021;71:102905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Killinger G, Brandani LM, Bianco R, Dulbecco E, Rodriguez Correa CA. Giant Congenital Aneurysm of the Left Atrial Appendage. Rev Argent Cardiol. 2013;81(5):417–9. [Google Scholar]
- 92.Zhari B, Bellamlih H, Boumdine H, Amil T, Bamous M, En-Nouali H. [Giant congenital intrapericardial left atrial appendage aneurysm: about a case and review of the literature]. Pan Afr Med J. 2016;24:225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Hassan M, Said K, El-Hamamsy I, Abdelsalam S, Afifi A, Hosny H, et al. Giant congenital left atrial appendage Aneurysm. J Am Coll Cardiol. 2013;61(4):478. [DOI] [PubMed] [Google Scholar]
- 94.Hui C, Luo S, An Q. Giant congenital left atrial appendage aneurysm. Cardiol Young. 2017;27(3):577–9. [DOI] [PubMed] [Google Scholar]
- 95.Zeng H, Yu J, Xu Z, Luo Y, Chen H, Zhu H. Giant congenital left atrial appendage aneurysm. J Card Surg. 2015;30(8):646–7. [DOI] [PubMed] [Google Scholar]
- 96.Harland DR, Suma V, Muthukumar L, Port SC, Werner PH, Tajik AJ. Giant congenital left atrial appendage Aneurysm presenting with recurrent supraventricular tachycardia and chest Pain. CASE Cardiovasc Imaging Case Rep. 2019;3(3):129–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Frambach PJ, Geskes GG, Cheriex EC, Wellens HJ, Penn OC. Giant intrapericardial aneurysm of the left atrial appendage. Eur Heart J. 1990;11(9):848–53. [DOI] [PubMed] [Google Scholar]
- 98.Bouallouche SA, Bouziane A, Laali M, Safar B, Milleron O. Giant left atrial appendage aneurysm. Eur Heart J Cardiovasc Imaging. 2014;15(8):862. [DOI] [PubMed] [Google Scholar]
- 99.Yong HS, Kim EJ, Choi CU. Giant left atrial appendage aneurysm. Eur Heart J. 2007;28(18):2207. [DOI] [PubMed] [Google Scholar]
- 100.Khanra D, Tiwari P, Kodliwadmath A, Duggal B. Giant left atrial appendage aneurysm and atrial fibrillation: chicken or the egg? BMJ Case Rep. 2019;12(8):e231300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Wagdy K, Samaan A, Romeih S, Simry W, Afifi A, Hassan M. Giant left atrial appendage aneurysm compressing the left anterior descending coronary artery. Echocardiogr Mt Kisco N. 2016;33(11):1790–2. [DOI] [PubMed] [Google Scholar]
- 102.Li M, Wang Y, Liu S, Yang J, Ma C. Giant left atrial appendage aneurysm compressing the left ventricular wall diagnosed by multiple imaging technology. Cardiol J. 2019;26(4):416–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Clarke JR, Zvaigzne CG, Disler D, Giuffre RM, Rebeyka IM, Patton DJ. Giant left atrial appendage aneurysm in a neonate. World J Pediatr Congenit Heart Surg. 2012;3(3):392–5. [DOI] [PubMed] [Google Scholar]
- 104.Rawtani S. Giant Left Atrial Appendage Aneurysm in an infant. World J Pediatr Congenit Heart Surg. 2021;12(1):131–2. [DOI] [PubMed] [Google Scholar]
- 105.Pawar R, Patel S, V S K PVS, Rao S. Giant left atrial appendage aneurysm in association with tricuspid atresia. Eur Heart J Cardiovasc Imaging. 2016;17(3):352. [DOI] [PubMed] [Google Scholar]
- 106.Morin J, Cantin L, Pasian S, Philippon F, Beaudoin J. Giant Left Atrial Appendage Aneurysm mimicking Mediastinal Mass and Associated with Incessant Atrial Arrhythmias. J Atr Fibrillation. 2017;9(6):1539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Bolt L, Studer Brüngger A, Huber LC, Arrigo M. Giant left atrial appendage aneurysm with thrombus: a challenging management. Cardiovasc Med [Internet]. 2022 Jul 1 [cited 2023 Jun 24];25(04). https://cardiovascmed.ch/article/doi/cvm.2022.02213
- 108.Valentino MA, Al Danaf J, Morris R, Tecce MA. Giant left atrial appendage aneurysm: a case of mistaken identity. J Cardiol Cases. 2017;15(4):129–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Sawalha W, Badaineh Y, Samara Y. Giant left atrial appendage aneurysm: a case report. JRMS June. 2005;12:41–4. [Google Scholar]
- 110.Das R, Kapoor L, Ganguly S, Maity A, RoyChowdhury S, Narayan P. Giant Left Atrial Appendage Aneurysm: a rare entity. Ann Thorac Surg. 2018;106(6):e323–4. [DOI] [PubMed] [Google Scholar]
- 111.Teng P, Ni Y, Sun Q, Zhao H. Giant Left Atrial Appendage Aneurysm: Surgical Treatment to prevent potential complications. Heart Surg Forum. 2018;21(6):E464–5. [DOI] [PubMed] [Google Scholar]
- 112.Ulucam M, Muderrisoglu H, Sezgin A. Giant left atrial appendage aneurysm: the third ventricle! Int J Cardiovasc Imaging. 2005;21(2–3):225–30. [DOI] [PubMed] [Google Scholar]
- 113.Dumitrescu A, Walsh KP, Wood AE. Giant left atrial appendage with a common ventricular-appendicular wall and an abnormal course of the circumflex coronary artery in an asymptomatic 18-month-old girl. Pediatr Cardiol. 2008;29(2):431–3. [DOI] [PubMed] [Google Scholar]
- 114.Kuiten WMM, de Heer LM, van Aarnhem EEHL, Onsea K, van Herwerden LA. Giant left atrial appendage: a rare anomaly. Ann Thorac Surg. 2013;96(4):1478–80. [DOI] [PubMed] [Google Scholar]
- 115.Akgün T, Kahveci G, Güler A, Andaçoğlu O. Huge intrapericardial aneurysm of the left atrial appendage. Turk Kardiyol Dernegi Arsivi Turk Kardiyol Derneginin Yayin Organidir. 2009;37(3):212. [PubMed] [Google Scholar]
- 116.Asfalou I, Boumaaz M, Raissouni M, Sabry M, Benyass A, Zbir EM. Huge left atrial appendage aneurysm revealed by chronic hiccups. J Saudi Heart Assoc. 2017;29(4):293–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Momtahen M, Abdi S, Mohebbi B, Hosseini S, Mohammadzadeh A. Huge left atrial appendage aneurysm, the five-chamber heart. Res Cardiovasc Med. 2018;7(2):103. [Google Scholar]
- 118.Hammad AMM, Abdel-Aziz O, Alsheikh RGh, Wahby EA. Idiopathic giant aneurysm of left atrial appendage. Indian J Thorac Cardiovasc Surg. 2004;20(4):186–8. [Google Scholar]
- 119.Smeglin A, Merchan J, Maysky M, Johnstone M, Pastore JO. Images in cardiovascular medicine: Giant left atrial appendage aneurysm. Circulation. 2008;118(23):2393–4. [DOI] [PubMed] [Google Scholar]
- 120.Burke RP, Mark JB, Collins JJ, Cohn LH. Improved Surgical Approach to Left Atrial Appendage Aneurysm. J Card Surg. 1992;7(2):104–7. [DOI] [PubMed] [Google Scholar]
- 121.Oz A, Oguz B, Karcaaltincaba M, Yilmaz M, Haliloglu M. Incidentally detected congenital giant left atrial appendage aneurysm in a child: MRI findings. JBR-BTR Organe Soc R Belge Radiol SRBR Orgaan Van K Belg Ver Voor Radiol KBVR. 2014;97(1):30–2. [DOI] [PubMed]
- 122.Yeung DF, Miu W, Turaga M, Tsang MYC, Tsang TSM, Jue J, et al. Incidentally discovered left atrial appendage Aneurysm Managed conservatively. Heart Lung Circ. 2020;29(5):e53–5. [DOI] [PubMed] [Google Scholar]
- 123.Park JS, Lee DH, Han SS, Kim MJ, Shin DG, Kim YJ, et al. Incidentally found, growing congenital aneurysm of the left atrium. J Korean Med Sci. 2003;18(2):262–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Tandon R, Arisha MJ, Nanda NC, Kumar S, Wander GS, Srialluri S, et al. Incremental benefit of three-dimensional transthoracic echocardiography in the assessment of left atrial appendage aneurysm leading to severe extrinsic compression of a coronary artery. Echocardiography. 2018;35(5):685–91. [DOI] [PubMed] [Google Scholar]
- 125.Tanabe T, Ishizaka M, Ohta S, Sugie S. Intrapericardial aneurysm of the left atrial appendage. Thorax. 1980;35(2):151–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Thomas E, Salmon AP, Vettukattil JJ. Intrapericardial giant left atrial appendage. Cardiol Young. 2004;14(3):338–40. [DOI] [PubMed] [Google Scholar]
- 127.Hosseini S, Hashemi A, Saedi S, Jalili F, Maleki M, Jalalian R, et al. Left atrial appendage Aneurysm. Ann Thorac Surg. 2016;102(3):e207–9. [DOI] [PubMed] [Google Scholar]
- 128.Jiang B, Wang X, Liu F, Song L. Left atrial appendage aneurysm. Interact Cardiovasc Thorac Surg. 2020;30(3):495–6. [DOI] [PubMed] [Google Scholar]
- 129.Li YH, Lin WY. Left atrial appendage aneurysm. Am J Med Sci. 2015;350(2):129. [DOI] [PubMed] [Google Scholar]
- 130.Mathur A, Zehr KJ, Sinak LJ, Rea RF. Left atrial appendage aneurysm. Ann Thorac Surg. 2005;79(4):1392–3. [DOI] [PubMed] [Google Scholar]
- 131.Salih AF, Milhoan KA, Cicek S. LEFT ATRIAL APPENDAGE ANEURYSM. J Sulaimani Med Coll. 2011;1(1):79–82. [Google Scholar]
- 132.Vázquez Antona CA, Cruz-Reyes OA, Ruiz-Esparza Dueñas E. Left atrial appendage aneurysm and atrial septal defect. Rev Esp Cardiol Engl Ed. 2014;67(1):61. [DOI] [PubMed] [Google Scholar]
- 133.Kawata M, Imanaka K, Matsuoka T, Yamabi H. Left atrial appendage aneurysm causes severe mitral regurgitation and heart failure: report of a successfully treated case. J Thorac Cardiovasc Surg. 2012;143(2):e17–18. [DOI] [PubMed] [Google Scholar]
- 134.Brenneman DJ, Pitkin AD, Gupta D, Bleiweis MS, Reyes KM, Chandran A. Left atrial appendage Aneurysm characterized by Multimodal Imaging. World J Pediatr Congenit Heart Surg. 2020;11(4):NP161–3. [DOI] [PubMed] [Google Scholar]
- 135.Nakamura M, Takemoto K, Terada K, Fujita S, Tanimoto T, Tanaka A. Left atrial appendage Aneurysm diagnosed by Transthoracic Echocardiography. Circ J off J Jpn Circ Soc. 2022;86(7):1147. [DOI] [PubMed] [Google Scholar]
- 136.Tanoue Y, Kado H, Shiokawa Y, Sagawa K. Left atrial appendage aneurysm in a child. Ann Thorac Surg. 2004;77(2):721–3. [DOI] [PubMed] [Google Scholar]
- 137.Ayed, Shati A, Asseri A, Mohammed A, Al-Gathradi, Sadeq K et al. Left Atrial Appendage Aneurysm in a Two Month Old Infant: A Case report. 2014;11.
- 138.Zhang X, Li P, Cao Y, Li X, Duan X, Bai S, et al. Left atrial appendage aneurysm in pediatrics. Echocardiography. 2020;37(6):917–21. [DOI] [PubMed] [Google Scholar]
- 139.Acartürk E, Kanadaşi M, Yerdelen VD, Akpinar O, Ozeren A, Saygili OB. Left atrial appendage aneurysm presenting with recurrent embolic strokes. Int J Cardiovasc Imaging. 2003;19(6):495–7. [DOI] [PubMed] [Google Scholar]
- 140.Bilge M, Yasar AS, Bozkurt M, Karakas F, Bilen E, Yuksel IO. Left atrial appendage aneurysm secondary to eccentric severe ischemic mitral regurgitation. Echocardiogr Mt Kisco N. 2009;26(10):1225–7. [DOI] [PubMed] [Google Scholar]
- 141.LaBarre TR, Stamato NJ, Hwang MH, Jacobs WR, Stephanides L, Scanlon PJ. Left atrial appendage aneurysm with associated anomalous pulmonary venous drainage. Am Heart J. 1987;114(5):1243–5. [DOI] [PubMed] [Google Scholar]
- 142.Shih YJ, Lin YC, Tsai YT, Lin CY, Lee CY, Yang HY, et al. Left Atrial Appendage Aneurysm with Paroxysmal Atrial Fibrillation. Heart Surg Forum. 2012;15(1):1. [DOI] [PubMed] [Google Scholar]
- 143.Wilson D, Kalra N, Brody EA, Van Dyk H, Sorrell VL. Left atrial appendage Aneurysm—A rare anomaly with an atypical presentation. Congenit Heart Dis. 2009;4(6):489–93. [DOI] [PubMed] [Google Scholar]
- 144.Ashish, Abhijit. Sahil. LEFT ATRIAL APPENDAGE ANEURYSM: a CASE REPORT. J Evol Med Dent Sci. 2014;3.
- 145.Belov DV, Moskalev VI, Garbuzenko DV, Arefyev NO. Left atrial appendage aneurysm: a case report. World J Clin Cases. 2020;8(19):4443–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Soleimani A, Sattarzadeh R. Left atrial appendage aneurysm: a rare cause of paroxysmal supraventricular tachycardia. Heart Lung Circ. 2008;17(3):246–7. [DOI] [PubMed] [Google Scholar]
- 147.Kapoor S, Ghosh VB, Dublish S, Prakash A. Left atrial appendage Aneurysm: An Unusual cause of Hematuria with Stroke. Indian J Pediatr. 2013;80(7):609–10. [DOI] [PubMed] [Google Scholar]
- 148.Krueger SK, Ferlic RM, Mooring PK. Left atrial appendage aneurysm: correlation of noninvasive with clinical and surgical findings: report of a case. Circulation. 1975;52(4):732–8. [DOI] [PubMed] [Google Scholar]
- 149.Veiga VC, Rojas SSO, Silva Junior A, Patrício ML, Marum ECH, Abensur H. Left atrial appendage aneurysm: echocardiographic diagnostic. Arq Bras Cardiol. 2008;90(5):e36–38. [DOI] [PubMed] [Google Scholar]
- 150.Hossain MA, Badruzzaman M, Kabir MM, Islam MJ, Masud MR. Left Atrial Appendage Giant Aneurysm- A Case Report. Bangladesh Heart J. 2022;37(1):81–3. [Google Scholar]
- 151.Youssef AA, Wilbring M, Laniado M, Kappert U. Like a dented bumper: a heart impressed by a giant left atrial appendage in a 22-year-old patient. Eur Heart J. 2014;35(31):2057. [DOI] [PubMed] [Google Scholar]
- 152.Kiaii B, Doll N, Kuehl M, Mohr FW. Minimal invasive endoscopic resection of a giant left atrial appendage aneurysm. Ann Thorac Surg. 2004;77(4):1437–8. [DOI] [PubMed] [Google Scholar]
- 153.Baburaj AK, Rameshwara T, Vellachamy KA, Vettath MP. Off-pump excision of left atrial appendage aneurysm: a case report. Heart Surg Forum. 2006;9(1):E478–479. [DOI] [PubMed] [Google Scholar]
- 154.DiBardino DJ, Aggarwal A, Knudson JD. Off-pump snare technique for congenital left atrial appendage aneurysm. Cardiol Young. 2014;24(3):555–8. [DOI] [PubMed] [Google Scholar]
- 155.Chung JW, Shim J, Shim WJ, Kim YH, Hwang SH. Paradoxical Response of Giant Left Atrial Appendage Aneurysm after Catheter ablation of Atrial Fibrillation. Investig Magn Reson Imaging. 2016;20(2):132. [Google Scholar]
- 156.Kothandam S, Ramasamy R. Planning and execution of catheter closure of a giant left atrial appendage aneurysm causing recurrent cardioembolism. Ann Pediatr Cardiol. 2020;13(4):353–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Sasaki T, Kawasaki Y, Murakami Y, Fujino M, Nakamura K, Yoshida Y, et al. Prenatally diagnosed left atrial appendage aneurysm with various postnatal imaging investigations: a case report. Echocardiography. 2021;38(10):1809–12. [DOI] [PubMed] [Google Scholar]
- 158.Hoffmann U, Hamed N, Herold C, Globits S. Radiological signs of a left atrial aneurysm. Eur Radiol. 2000;10(8):1332–4. [DOI] [PubMed] [Google Scholar]
- 159.de Feyter PJ, Zienkowicz BS, Heidendal GA, Majid PA, Roos JP. Radionuclide Angiography in the diagnosis of congenital intrapericardial aneurysm of the left atrial appendage. Thorax. 1980;35(2):154–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Clark JB, Ting JG, Polinsky RJ, Wolfe LT. Resection of a Giant Left Atrial Appendage Aneurysm via Limited Thoracotomy. World J Pediatr Congenit Heart Surg. 2014;5(3):475–7. [DOI] [PubMed] [Google Scholar]
- 161.Itaya H, Aoki C, Hatanaka R, Fukuda I. Resection of left atrial appendage aneurysm and full maze procedure as curative management for stroke recurrence. Gen Thorac Cardiovasc Surg. 2020;68(3):295–7. [DOI] [PubMed] [Google Scholar]
- 162.Karatasakis GT, Beldekos DI, Makos GS, Sfirakis PD, Cokkinos DV. Resolution of Thrombi in Left Atrial Appendage Aneurysm. Echocardiogr Mt Kisco N. 1997;14(2):161–2. [DOI] [PubMed] [Google Scholar]
- 163.Fan F, Bai S, Tong F, Zheng J, Li Q, Guo Z, et al. Safe treatment of congenital left atrial appendage aneurysm using lateral thoracotomy on a 3-year-old patient. Cardiol Young. 2021;31(1):144–7. [DOI] [PubMed] [Google Scholar]
- 164.Ergül Y, Öztürk E, Özgür S. Successful radiofrequency ablation of accessory pathway associated with left atrial appendage aneurysm in a low birthweight premature patient. Turk J Pediatr. 2019;61(1):142–6. [DOI] [PubMed] [Google Scholar]
- 165.Nakai Y, Asano M, Nomura N, Mishima A. Surgical management of an aneurysm of the left atrial appendage to prevent potential sequelae. Interact Cardiovasc Thorac Surg. 2013;17(3):586–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Bharati A, Merhcant S, Nagesh C, Bansal A. The giant dog ear sign of left atrial appendage aneurysm—revisited on 3 T cardiac MRI (free-breathing, non-contrast). BJR Case Rep. 2016;2(1):20150292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Sharma J, Kapoor A. The fifth cardiac chamber: case of a huge left atrial appendage aneurysm. Indian J Med Res. 2015;142(6):770–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Kim YW, Kim HJ, Ju MH, Lee JW. The treatment of Left Atrial Appendage Aneurysm by a minimally invasive Approach. Korean J Thorac Cardiovasc Surg. 2018;51(2):146–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Rengifo LM, Hazle MA, Kincaid EH, Ootaki Y. Thoracoscopic Resection of Left Atrial Appendage Aneurysm in a 16-Year-old boy. Ann Thorac Surg. 2021;112(6):e451–3. [DOI] [PubMed] [Google Scholar]
- 170.Culver DL, Bezante GP, Schwarz KQ, Meltzer RS. Transesophageal echocardiography in the diagnosis of acquired aneurysms of the left atrial appendage. Clin Cardiol. 1993;16(2):149–51. [DOI] [PubMed] [Google Scholar]
- 171.Cujec B, Bharadwaj B, Orchard RC, Lopez JF. Transesophageal echocardiography in the diagnosis of left atrial appendage aneurysm. J Am Soc Echocardiogr off Publ Am Soc Echocardiogr. 1990;3(5):408–11. [DOI] [PubMed] [Google Scholar]
- 172.Zhao J, Ge Y, Yan H, Pan Y, Liao Y. Treatment of congenital aneurysms of the left atrium and left atrial appendage. Tex Heart Inst J. 1999;26(2):136–9. [PMC free article] [PubMed] [Google Scholar]
- 173.Brazier A, Hasan R, Jenkins P, Hoschtitzky A. Urgent resection of a giant left atrial appendage aneurysm and mitral valve replacement in a complex case of Hurler-Scheie syndrome. BMJ Case Rep. 2015;2015:bcr2015211551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Vedula GB, Aggarwal K. Young female with palpitations. Ann Emerg Med. 2019;74(2):303–4. [DOI] [PubMed] [Google Scholar]
- 175.Renner U, Busch UW, Sebening H, Fischer M, Bauer R, Hagl S, et al. [Slow increase in the size of the left atrium with atrial fibrillation–a congenital pericardial defect or aneurysm of the left atrium?]. Z Kardiol. 1987;76(9):581–4. [PubMed] [Google Scholar]
- 176.Toufan M, Pourafkari L, Afrasiabi A, Sohrabi M, Nader ND. Left atrial appendage aneurysm presenting with chronic cough. Neth Heart J Mon J Neth Soc Cardiol Neth Heart Found. 2017;25(9):526–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Aryal MR, Hakim FA, Ghimire S, Ghimire S, Giri S, Pandit A, et al. Left atrial appendage aneurysm: a systematic review of 82 cases. Echocardiogr Mt Kisco N. 2014;31(10):1312–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.