Abstract
Aims
We aimed to investigate the anxiolytic effect of darbepoetin alpha (DEPO), an erythropoietin derivative, in a neuroinflammation model regarding different behaviors and biological pathways.
Methods
Forty adult male Wistar albino rats were divided into four groups (control, LPS, DEPO, and DEPO + LPS). The rats were treated with 5 µg /kg DEPO once a week for four weeks, after which neuroinflammation was induced with 2 mg/kg lipopolysaccharide (LPS). The elevated plus maze, open-field, and light‒dark box tests were conducted to assess anxiety levels. Harderian gland secretions were scored via observation. Tumor necrosis factor alpha (TNF-α), Interleukin-1-beta (IL-1β), brain-derived growth factor (BDNF), serotonin, cortisol, total antioxidant/oxidant (TAS/TOS), and total/free thiol levels were measured in the prefrontal cortex, striatum, and serum.
Results
DEPO had a potent anxiolytic effect on both DEPO and DEPO + LPS groups. Compared to the control group, DEPO administration caused an increase in serotonin and BDNF levels and decreased basal cortisol and TNF-α levels in naive rats. IL-1β did not alter after DEPO administration in naive rats. Prophylactic DEPO treatment remarkably downregulated cortisol, IL-1β, and TNF-α in the DEPO + LPS group. In addition, prophylactic DEPO administration significantly attenuated the decrease in serotonin and BDNF levels in the DEPO + LPS group. Furthermore, DEPO ameliorated excessive harderian gland secretion in the DEPO + LPS group. Compared with those in the control group, the free thiol content in the serum increased after DEPO administration. No similar effect was seen in the DEPO + LPS group receiving prophylactic DEPO. TAS showed no difference among all experimental groups. DEPO administration increased TOS and OSI in the serum and prefrontal cortex but not in the striatum. This effect was not seen in the DEPO + LPS group.
Conclusion
Darbepoetin alpha had an anxiolytic effect on many physiological mechanisms in a neuroinflammation model and naive rats.
Keywords: Anxiety, Darbepoetin alpha, Erythropoietin, Neuroinflammation
Introduction
Anxiety, in its most general definition, is an uncertain-unpleasant emotional state that covers different conditions, such as fear, distress, and restlessness [1]. Approximately 264 million people suffer from anxiety disorders, with an estimated global prevalence of 3.6% [2]. Different pathways and molecular groups, such as neurotransmitters, neurotrophic factors, oxidative stress, cytokines, and hormones, play a role in the physiopathology of anxiety [3]. In recent years, neuroinflammation in the central nervous system has been thought to contribute to the physiopathology of mental disorders. Inflammation markers are highly expressed in patients’ serum and cerebrospinal fluid [4, 5]. Postmortem studies have also reported that inflammation is associated with mental disorders [6]. Furthermore, preclinical studies revealed that anxiety-like behavior (ALB) was increased in rodents in a model of neuroinflammation [7, 8]. The hypothalamic-pituitary-adrenal (HPA) axis is a crucial mediator of stress-immune pathway communication in neuroinflammation. Inflammation leads to hyperactivity and dysfunction of the HPA axis. Preclinical studies have shown that systemic administration of pro-inflammatory cytokines such as IL-1 and TNF-α induces hyperactivity of the HPA axis in animals. Furthermore, inflammation affects other biological factors and contributes to the pathophysiology of anxiety [9].
Erythropoietin (EPO) is a glycoprotein hormone and growth factor. EPOR, the receptor for EPO, has two subtypes with different variations: homodimeric and heterodimeric [10]. The heterodimeric subunit exerts a protective effect on the cell [11]. Because of its protective effect on cells, EPO has been used in various experimental models, such as myocardial infarction, acute liver injury, ischemic skin wounds, and diabetes [12–15].EPO has been shown in animal studies to cross the blood-brain barrier [16]. Subsequent research has examined its effects on central nervous system diseases in both preclinical and clinical studies [17]. EPO increases neuron density, decreases the number of necrotic neurons, reduces brain edema and infarct volume, and increases neuron survival [18].
Erythropoietin studies have focused mainly on its protective effects in neurological models [17]. This study aims to study darbepoetin alpha (EPO derivation), which has never been studied in psychiatric models, and ensure that EPO, in general, is enlightening in physiopathological anxiety processes. This study aimed to investigate the anxiolytic effect of darbepoetin alpha, an erythropoietin derivative, in rats, both in healthy and neuroinflammation models.
Methods
Animals
Adult male Wistar albino rats (n = 40) aged 12 weeks were used in this study. The rats were purchased from Ankara University Experimental Animals Breeding and Research Laboratory. The subjects were sheltered under a 12 h light/dark cycle at a constant temperature (22–25 °C) and humidity (50 ± 5%) and had access to ad libitum chow and tap water. 3–4 rats were housed in the same cage. All procedures were carried out under the approval of the Ankara University Experimental Animals Ethics Committee, and the approval reference number is 2020-2-10. After adaptation, the animals were divided into four groups (n = 10 for each group): the control (C), darbepoetin alpha (DEPO), lipopolysaccharide (LPS), and DEPO + LPS groups.
Drug treatment and experimental protocol
Darbepoetin alpha, an erythropoietin derivative, was administered intraperitoneally at 5 µg/kg for four consecutive weeks. Darbepoetin alpha (DEPO) was used from Aranesp (Manufactured by AMGEN). The dose of 5 μg/kg chosen in this study is a modified version of the drug administration schedule performed by Coccia et al. for chronic inflammatory disease in the rodent model [19]. After four weeks of prophylactic DEPO administration, a single dose of 2 mg/kg LPS was intraperitoneally administered to induce neuroinflammation (Sigma Aldrich, Escherichia coli O111:B4) [20]. The control group was administered saline (1 ml/kg). The DEPO group was administered 5 µg /kg weekly for four consecutive weeks. The LPS group was administered a single dose of 2 mg/kg LPS. After four weeks of prophylactic DEPO administration, a single dose of 2 mg/kg LPS was intraperitoneally in the DEPO + LPS group. The rats were euthanized using sodium thiopental (50 mg/kg) and exsanguinated by cardiac puncture, and the prefrontal cortex and striatum were removed for subsequent analysis. The experimental protocol is detailed in Table 1.
Table 1.
Drug treatment and experimental protocol. *: LPS group participated in behavioral test (n = 10). Two animals from the LPS group died before euthanization (n = 8). OFT: open field test, EPM: elevated plus maze, LDB: light-dark box. X: no implementation was carried out
| Experimental Schedule | ||||||||
|---|---|---|---|---|---|---|---|---|
| Experimental Groups | 1–28 Days | 28th Day | 35th Day | 42th Day | 49th Day | 56th Day | 57th Day |
|
|
Control (C) (n = 10) |
Adaptation | Saline 1 ml/kg | Saline 1 ml/kg | Saline 1 ml/kg | Saline 1 ml/kg | Saline 1 ml/kg | Euthanization (12 pm) | |
|
Darbepoetin alpha (DEPO) (n = 10) |
DEPO 5 µg/kg | DEPO 5 µg/kg | DEPO 5 µg/kg | DEPO 5 µg/kg | Saline 1 ml/kg | Euthanization (12 pm) | ||
|
Lipopolysaccharides (LPS) (n = 10) |
X | X | X | X | LPS 2 mg/kg |
Euthanization (12 pm) (n = 8)* |
||
|
Darbepoetin alpha + Lipopolysaccharides (DEPO + LPS) (n = 10) |
DEPO 5 µg/kg | DEPO 5 µg/kg | DEPO 5 µg/kg | DEPO 5 µg/kg | LPS 2 mg/kg | Euthanization (12 pm) | ||
| Injection Schedule | X | X | 12 pm | 12 pm | 12 pm | 12 pm | 12 pm | |
| Behavioral Test Schedule | X | X | X | X | X | X |
6 pm: OFT + EPM 8 pm: LDB |
|
Behavioral tests
In all anxiety tests, animal behavior was recorded by a camera for 5 min. The test apparatuses were cleaned with 70% alcohol in each experiment. The open field test and elevated plus maze were conducted between 6.00 and 8.00 p.m., and the light-dark box was carried out between 8.00 and 12.00 p.m.
Open-Field Test (OFT)
The OFT was conducted to investigate locomotor activity and anxiety-like behaviors (ALB) [21]. The apparatus included a hypethral box of 100 × 100 × 40 cm whiteboards. The base of the box was divided into 25 equal squares. The squares adjacent to the edges of the apparatus wall are defined as the peripheral zone, and the squares in the middle of the box are defined as the central zone. First, the subjects were placed in the central zone for the experiment. Central zone time, central zone entrance number, unsupported rearing number, and rearing latency were used to assess the ALB. Furthermore, we analyzed locomotor activity parameters, including total distance traveled and total rearing number.
Elevated plus maze (EPM)
Elevated plus maze (EPM) is one of the most widely used and validated behavioral tests for assessing anxiety-like behaviors in rodents [21]. A 50 cm × 10 cm open arm, a 50 × 50 × 10 cm closed arm, and a test apparatus made of white odorless wood with a height of 70 cm from the floor were used. Each experiment was performed once for 5 min. The time spent in the open arms, number of entries into the open arms, frequency of head dipping, and stretching posture were recorded.
Light dark box (LDB)
The light-dark box (LDB) was conducted to investigate anxiety-like behaviors [22]. The apparatus (40 cm width and 110 cm length) consisted of two equal compartments: a light zone (850 lx illumination intensity) and a dark zone. A wall with a hole (7.5 × 7.5 cm2) was placed on the floor between the light and dark zones. The rats were individually placed in the apparatus for 5 min, beginning from the light zone. The time spent in the light zone, the number of entries between the light/dark zone, and the latency of the entrance to the dark zone were recorded and analyzed.
Harderian gland secretion
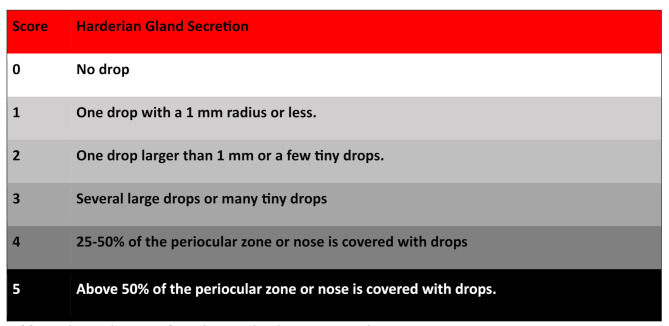
The Harderian gland is located in the orbit of the eye in land mammals, including rodents. Under stress, red-black staining around the eye and nose (aka chromodacryorrhoea) is seen due to increased Harderian gland secretion. Harderian gland secretion increases with stress and is considered a marker of stress and animal welfare [21, 23]. Harderian gland function was analyzed 24 h after LPS application, the time before sacrifice. A score of 0–5 points was given to each animal according to the Choromodacryorrhoea scale [23].
This scale ranges from 0 to 5, with 0 indicating no spotting and 5 indicating severe spotting (See Table 2).
Table 2.
The evaluation of harderian gland secretion scale
Molecular analysis
Brain tissue (striatum and prefrontal cortex) was dissected under the guidance of the Paxinos Rat brain atlas [79] roughly in less than 2 min on a flat plastic kept cold on ice. Tissue samples were immediately frozen in liquid nitrogen and kept at − 80 °C until analysis. The tissues were then homogenized for molecular studies.
ELISA kits were used following the manufacturer’s instructions (serotonin (BT Lab, no: E0866Ra), TNF-α (BT Lab, no: E0764Ra), BDNF (BT Lab, no: E0476Ra), cortisol (BT Lab E0828Ra), and IL-1β (Cloud Clone Lab: SEA563Ra). Ten samples from the control, DEPO, and DEPO + LPS groups and eight samples from the LPS group were studied in the ELISA kits.
Total antioxidant status (TAS) and total oxidant status (TOS) were also measured using colorimetric kits (Rel Assay no: RL0017 and Rel Assay no: RL0024, respectively). TAS and TOS levels were used to calculate the oxidative index (OSI). OSI = TOS (µmol H2O2 equivalent/L)/TAS (µmol Trolox equivalent/L). Thiol/disulfite balance values were determined automatically and spectrophotometrically according to commercial instructions (colorimetric kit, Rel Assay Diagnostics, Gaziantep, Turkey). In Colorimetric kits, eight samples from the control, LPS, and DEPO groups and eight samples from the DEPO + LPS group were studied (Due to a technical problem in one serum of the DEPO + LPS group, we could not make measurements; therefore, the serum data of the DEPO + LPS group are shown as 7 in the dot plot graphs).
Physiological measurements
The subjects’ body weights were measured 24 h prior to and immediately before the end of the experiment. Water and food consumption were recorded for the animals during the last 24 h. Blood glucose levels (via a Call Plus glucometer) and the hemoglobin (HB)/hematocrit (HCT) ratio (via hemoglobin Mission Ultra) were measured using blood collected from the tail vein of the rats under anesthesia. The duration during which the animals could not maintain their initial posture after the anesthetic was administered, as well as the time until the paw withdrawal reflex disappeared following a painful stimulus, were recorded to determine the onset of deep anesthesia.
Statistical analysis
Shapiro‒Wilk test was conducted as a normality test. One-way analysis of variance (ANOVA) was performed. The Tukey’s test was used to examine the differences between the groups. P values < 0.05 were considered statistically significant. If there was no normal distribution, the nonparametric test was conducted as Kruskal Wallis performed; afterward, Dunn was conducted as a post hoc test (Median values and interquartile range of parameters that did not show normal distribution were also given). The behavioral and molecular findings are presented as the mean (X) ± standard errors of the mean (SEM) in the dot plot graphs. Basic physiological parameters are presented as the mean (X) ± standard error of the mean (SEM) in the table. p-value less than 0.05 was accepted for statistical significance. Whether there is a relationship between molecular findings and deep anesthesia time was tested with Pearson correlation analysis. Further, the relationship between hemoglobin values and TOS/OSI was also analyzed by using the Pearson correlation test.
Results
Behavioral results
We observed anxiety-like behaviors (ALB) and locomotor activity in the OFT, the results of which are shown in Fig. 1. According to the time spent in the central zone and central zone entrance number parameters, darbepoetin alpha has a potent anxiolytic effect on both DEPO and DEPO + LPS groups (“one-way ANOVA”, p < 0.0001). Darbepoetin alpha similarly increased unsupported rearing behavior, indicative of reduced anxiety, in both the DEPO (“one-way ANOVA”, p < 0.0001) and DEPO + LPS groups (“one-way ANOVA”, p < 0.05). Prophylactic DEPO administration led to earlier rearing behavior in the DEPO + LPS group; thus, rearing latency was significantly decreased (“one-way ANOVA”, p < 0.0001). DEPO administration did not affect locomotor activity, including the total number of rearings or the total distance traveled compared to the control group (“one-way ANOVA”, p > 0.05). Prophylactic DEPO administration attenuated the hypolocomotor picture associated with inflammation in both the vertical and horizontal direction, and thus, the DEPO + LPS group displayed a higher value vs. the LPS group (“one-way ANOVA”, p < 0.0001).
Fig. 1.
Behavioral findings in the open field test in the experimental groups (A) Central zone time, (B) central zone entrance number, (C) unsupported rearing number, (D) rearing latency, (E) total rearing number, (F) total distance traveled. Figure 1 Behavioral findings in the light-dark box for the experimental groups (G) light zone time, (H) light‒dark zone entrance number, (I) dark zone latency; values in the graphs are presented as the means ± SEMs (*p < 0.05, ** p < 0.01, **** p < 0.0001)
We observed the time spent in the open arms, number of open arm entries, head dipping behavior, and stretch-attend posture in the EPM test, the results of which are shown in Fig. 2. Darbepoetin alpha had a powerful anxiolytic effect both in the DEPO and DEPO + LPS groups. The time spent in the open arms and the number of open-arm entries were significantly greater in DEPO and DEPO + LPS groups (“one-way ANOVA”, p < 0.0001). Head dipping behavior, an exploratory behavior associated with decreased anxiety, increased in both DEPO and DEPO + LPS groups (“one-way ANOVA”, p < 0.0001). We also examined stress-related stretch-attend posture, which was significantly lower in the DEPO group than in the control group and the DEPO + LPS group than in the LPS group (“one-way ANOVA”, p < 0.0001).
Fig. 2.
Behavioral findings in the elevated plus-maze test for the experimental groups: (A) time spent in open arm, (B) number of open arm entrance, (C) number of head dips, (D) stretch-attend posture. Furthermore, the harderian gland secretion score is shown in Fig. 1-E. Results are presented as mean ± SEMs (**p < 0.01, **** p < 0.0001)
We observed light zone time, light-dark zone entrance number, and dark zone entrance latency in the LDB test, the results of which are shown in Fig. 1. Although a slight increase was observed in healthy subjects after darbepoetin alpha administration, there was no significant difference in light zone time, light-dark zone entrance number, or dark zone entrance latency DEPO vs. control groups (“Kruskal Wallis”, p > 0.05). According to DEPO + LPS vs. LPS, Prophylactically administered darbepoetin alpha had a significant anxiolytic-like effect on the light-dark box test parameters, including light zone time (“Kruskal Wallis”, DEPO + LPS; median 45, interquartile range 30,75 and LPS; median 10, interquartile range 8.25: p < 0.0001) and light dark zone entrance number (“Kruskal Wallis”, DEPO + LPS; median 3, interquartile range2.25 and LPS; median 1, interquartile range 0: p < 0.01).
Harderian gland scale
We observed the harderian gland scale score, the results of which are shown in Fig. 3. The secretion of the Harderian gland, whose secretion increases in the context of stress and disease, increased in the LPS group. Prophylactic darbepoetin alpha attenuated this deterioration in the DEPO + LPS group (“one-way ANOVA”, p < 0.0001).
Fig. 3.
Behavioral findings Harderian gland secretion score for the experimental groups. Results are presented as mean ± SEMs (**** p < 0.0001). LPS labeled photo: Black spots around the face of the rat with increased secretion of Harderian’s gland. DEPO + LPS labeled photo: Black spots reduced by prophylactic DEPO application. DEPO labeled photo: Black spots are almost non-existent. Control labeled photo: Black spots are almost non-existent
Molecular results
We measured levels of TNF alpha and IL-1beta serotonin and BDNF, which were shown in Fig. 4. The levels of the proinflammatory cytokines TNF alpha and IL-1 beta in the striatum and prefrontal cortex (PFC) were examined. Prophylactic darbepoetin alpha administration had anti-inflammatory effects on both the striatum and PFC in the DEPO + LPS group. According to DEPO + LPS vs. LPS group, TNF alpha levels were significantly decreased in the PFC and striatum (“one-way ANOVA”, p < 0.0001). Furthermore, DEPO treatment decreased TNF-alpha levels in the PFC and striatum in the DEPO group vs. control group (“one-way ANOVA”, p < 0.05). Similar results were observed for IL-1beta in the DEPO + LPS group. Prophylactic DEPO treatment had anti-inflammatory effects on both the PFC and the striatum, and the level of this cytokine was significantly reduced in the DEPO + LPS group (“one-way ANOVA”, p < 0.0001). Unlike TNF alpha, the DEPO group had no anti-inflammatory effect on basal IL-1beta inflammatory responses compared to the control group (“one-way ANOVA”, p > 0.05).
Fig. 4.
Molecular findings for the experimental groups: (A) PFC-TNF-𝛼, (B) striatum-TNF-𝛼, (C) PFC-IL-β, (D) striatum-IL-1β, (E) PFC-BDNF, (F) striatum-BDNF, (G) PFC-serotonin, (H) striatum-serotonin, (I) PFC-cortisol, (J) stratum-cortisol, and (K) serum-cortisol. Results are presented as mean ± SEMs (*p < 0.05, **p < 0.01, **** p < 0.0001)
Serotonin was significantly greater in the PFC and striatum of the DEPO group than in the control group (“one-way ANOVA”, p < 0.0001). Inflammation severely suppresses serotonin production. This suppression was significantly alleviated by prophylactic DEPO administration. Serotonin was considerably higher in the PFC and striatum of the DEPO + LPS group than in the LPS group (“one-way ANOVA”, p < 0.05). BDNF was significantly greater in the PFC and striatum of the DEPO group than in the control group (“one-way ANOVA”, p < 0.0001). Neuroinflammation suppressed and damaged BDNF. This damage and suppression were alleviated by prophylactic DEPO administration in both the PFC and striatum. BDNF had a higher value in the PFC and striatum of the DEPO + LPS group than in the LPS group (“one-way ANOVA”, p < 0.01). Cortisol levels were markedly lower in the PFC (“one-way ANOVA”, p < 0.005), striatum (“one-way ANOVA”, p < 0.0001), and serum (“one-way ANOVA”, p < 0.05) of the DEPO group than in the control group. Similarly, cortisol levels were significantly lower in the PFC, striatum, and serum of the DEPO + LPS group compared to the LPS group (“one-way ANOVA”, p < 0.0001).
TAS, TOS, and OSI were measured in both the prefrontal cortex, striatum, and serum, the results of which are shown in Fig. 5. DEPO did not exhibit antioxidant activity in DEPO or DEPO + LPS groups. There was no significant difference in the TAS parameters among the groups for the PFC, striatum, or serum (“Kruskal Wallis”, p > 0.05). TOS levels increased in the PFC, (control; median 10.62, interquartile range 3.87 and DEPO; median 21, interquartile range 5.88, “Kruskal Wallis”, p < 0.001) and serum (control; median 5.27, interquartile range 8.19 and DEPO; median 24.66, interquartile range 20.47, “Kruskal Wallis”, p < 0.01) in the DEPO group vs. the control group. Similarly, the OSI values increased in the PFC (control; median 1.004, interquartile range 0.436 and DEPO; median 3.35, interquartile range 2.11, “Kruskal Wallis”, p < 0.001) and serum (control; median 0.38, interquartile range 0.16 and DEPO; median 1.76, interquartile range 1.07, “Kruskal Wallis”, p < 0.05) for the DEPO group compared with those in the control group.
Fig. 5.
Molecular findings for the experimental groups: (A) PFC-TAS, (B) PFC-TOS, (C) PFC-OSI, (C) Striatum-TaS, (D) Striatum-TOS, (F) Striatum-OSI, (G) serum-TAS, (H) serum-TOS, (I) serum-OSI, (J) serum-native thiol, (K) serum-total thiol, and (L) serum-Thiol/disulfide balance. Results are presented as the means ± SEMs (*p < 0.05, ** p < 0.01, *** p < 0.001
According to DEPO vs. control groups, the TOS and OSI parameters did not significantly change in the striatum region (“Kruskal Wallis”, p > 0.05). A similar effect was not observed in the DEPO + LPS vs. LPS groups (“Kruskal Wallis”, p > 0.05). Furthermore, we measured different antioxidant systems, including native thiol, total thiol, and disulfide balance, in serum. Native thiol increased significantly in the DEPO group compared with the control group (control; median 132, interquartile range 240.3 and DEPO; median 780, interquartile range 777.2, “Kruskal Wallis”, p < 0.05). A similar effect was not observed in the DEPO + LPS vs. LPS groups (“Kruskal Wallis”, p > 0.05). The total thiol content and disulfide balance did not differ among all the groups (“Kruskal Wallis”, p > 0.05).
In naive rats receiving DEPO treatment, a statistically significant correlation was found between PFC TOS levels and hemoglobin values (“Pearson Correlation”, r = 0,74, p < 0.05). Similarly, in naive rats receiving DEPO treatment a statistically significant correlation was found between PFC OSI levels and hemoglobin values (“Pearson Correlation”, r = − 0,74, p < 0.05). Another correlation between proinflammatory cytokines and deep anesthesia duration was analyzed. A statistically significant correlation was found between TNF-alpha levels in the PFC (“Pearson Correlation”, r = − 0,76, p < 0.05) and striatum (“Pearson Correlation”, r = -0,75, p < 0.05) and the duration of deep anesthesia in the LPS group. Similarly, a statistically significant correlation was found between IL-1beta levels in the PFC (“Pearson Correlation”, r = -0,73, p < 0.05) and striatum (“Pearson Correlation”, r= -0,91, p < 0.05) and the duration of deep anesthesia in the LPS group.
Furthermore, we analyzed other physiological parameters, such as hemoglobin, hematocrit, blood glucose, weight loss, weight loss ratio, water/feed consumed, loss of posture latency during anesthesia, and deep anesthesia time. All the parameters are given in Table 3 as arithmetic mean and standard errors of the means. Significant differences are marked and explained below the table.
Table 3.
Results are presented as the means ± SEMs. *: control vs. DEPO, (“one-way ANOVA”, p < 0.01), #: DEPO + LPS vs. LPS, (“one-way ANOVA”, p < 0.001), ☆: DEPO + LPS vs. LPS, (“one-way ANOVA”, p < 0.05), ♦: control vs. LPS, (“one-way ANOVA”, p < 0.001)
| GROUPS | Control | DEPO | LPS | DEPO + LPS |
|---|---|---|---|---|
| HB (g/dl) | 17,85 ± 0,72 | 21,85 ± 0,71 * | 16,26 ± 0,81 | 20,61 ± 1,02# |
| HCT (%) | 54,38 ± 1,92 | 67,88 ± 1,63 * | 50,88 ± 2,62 | 60,50 ± 2,33# |
| Glucose (mg/dl) | 106 ± 4,21 | 105 ± 4,73 | 114 ± 3,76 | 105,8 ± 5,11 |
| Weight loss (g) | 0,62 ± 0,26 | 0,50 ± 0,80 | 34 ± 4,06♦ | 17,25 ± 1,74# |
| Weight loss % | 0,23 ± 0,09 | 0,25 ± 0,09 | 9,77 ± 0,90♦ | 4,99 ± 0,43# |
| Loss of posture latency (sec) | 81,13 ± 4,65 | 90,13 ± 5,24 | 43,13 ± 3,19♦ | 65,13 ± 6,84☆ |
| Deep anesthesia latency (sec) | 170, 4 ± 6,23 | 264,3 ± 21, 86 * | 81,13 ± 6,69♦ | 163,9 ± 17,61☆ |
Discussion
In the present study, DEPO demonstrated a potent anxiolytic effect. In the OFT, both the time spent in the central zone, which is the risk zone, and the number of entries into the central zone significantly increased in both the DEPO and DEPO + LPS groups. This increase suggests a reduction in ALB [21]. Unsupported rearing -where animals stand on both feet without touching the walls of the OFT- reflects exploratory behavior and reduced anxiety sensitivity. In this study, DEPO also enhanced unsupported rearing behavior in both DEPO and DEPO + LPS groups. Khairallah et al. reported improvements in locomotor activity and ALB following EPO treatment in rats with neuroinflammation induced by LPS [7]. Similarly, another rodent study found that recombinant human erythropoietin (RhuEPO) treatment increased the frequency of unsupported rearing behaviors, indicating decreased anxiety [24]. In this study, locomotor activity was also assessed in the OFT. In the present study, DEPO administration did not affect locomotor activity in the vertical (total rearing number) or horizontal (total distance traveled) directions, which is consistent with findings from other researchers [25, 26]. According to our result in the LPS group, hypolocomotion was observed, aligning with other literature reports [27, 28]. Prophylactic administration of DEPO also improved the hypolocomotor symptoms in the DEPO + LPS group.
According to the results of the EPM test, DEPO exhibited a potent anxiolytic effect in both DEPO and DEPO + LPS groups. The number of entries into the open arms, which represents a risky area of the experimental setup, as well as the time spent in the open arms, increased in all the DEPO-treated rats. In other rodent studies, RhuEPO reduced the ALB symptoms in a sleep apnea model [29]. Additionally, Beta-hydroxybutyrate, a hematopoietic agent, has demonstrated an anxiolytic effect in rats subjected to chronic stress [30]. According to Osborn et al., rhuEPO treatment did not produce an anxiolytic effect in the EPM [25]. Furthermore, we analyzed head dipping, where subjects looked down from the open arm and tried to estimate height, and found that this behavior increased with DEPO administration. In addition, stretch-attend posture decreased with DEPO application.
In the LDB test, another anxiety test, we observed potent anxiolytic effects in the DEPO + LPS group compared to the LPS group. No such strong effect was observed in the DEPO group. DEPO moderately increased anxiolytic behaviors in the DEPO group, although it did not produce a significant or potent anxiolytic effect. In this study, we administered the 5mcg dose of DEPO. The desired anxiolytic impact can be observed in a dose-dependent manner. Leconte et al. reported an anxiolytic effect with carbamylated erythropoietin in LDB, while EPO treatment was found to be insufficient [31]. Imaging and clinical studies have indicated that EPO can improve working memory, exhibit antidepressant effects, and reduce fear responses, as well as mitigate side effects of electroconvulsive therapy [32–36]. serum EPO levels have been found to decrease in patients diagnosed with generalized anxiety disorder, with a negative correlation observed between reduced EPO levels and increased anxiety scores [37].
In the present study, we investigated harderian gland function, which has not been examined in LPS-induced studies before. Notably, black spots were observed in the eyes, nose, and nasal fur of rats treated with LPS, corresponding to scores of 4 to 5 on the harderian gland secretion scale. Significantly, prophylactic DEPO treatment mitigated this effect, resulting in a decrease of the harderian gland scale to approximately 2 in the DEPO + LPS group.
Tnf-𝛼 and IL-1β were analyzed in the PFC and striatum as inflammatory markers. DEPO exhibited anti-inflammatory effects, significantly decreasing TNF-𝛼 levels in both regions for the DEPO and DEPO + LPS groups. Similarly, prophylactic DEPO administration decreased IL-1beta levels in the DEPO + LPS. However, in naive rats, DEPO did not exert an anti-inflammatory effect on IL-1beta. There is no consensus on the impact of EPO on basal inflammatory levels in the absence of disease models. One study has shown that TNF-α and IL-1β levels are decreased in the hippocampus of old rats receiving recombinant EPO treatment every other day, while a similar effect was not observed in the healthy young rats [38]. EPO administration did not significantly change TNF-α or IL-1β levels in neuron cultures [39]. Experimental studies have focused on the effects of EPO and its derivatives on inflammation in neurological and neuropsychiatric animal models. EPO has shown anti-inflammatory effects in these disease models [40, 41]. In summary, it appears to generally suppress inflammation in disease states.
Serotonin is an important neurotransmitter involved in the neurobiology of anxiety. Serotonin and its receptors in the PFC play critical roles in mood regulation, particularly anxiety [42]. Serotonin in the striatum also plays a role in the control of movement and mood [43]. In the present study, chronic DEPO treatment significantly increased serotonin levels in both the PFC and striatum compared to the control group. In addition, prophylactic DEPO administration also produced a similar effect on the DEPO + LPS group. There is a well-defined pathway related to inflammation known as the serotonin pathway. In this pathway, increases in TNF-α and IL-1β stimulate the endogenous enzyme indoleamine 2,3-dioxygenase (IDO). As the abundance of this enzyme increases, kynurenine and its metabolites are formed from tryptophan, a precursor of serotonin. Finally, neuroinflammation may cause a decrease in serotonin levels [44, 45]. In our study, 24 h after high-dose LPS administration, serotonin levels decreased in both the PFC and striatum, consistent with previous studies [44, 45].
BDNF is a growth factor involved in neuronal survival, neurotransmitter secretion, and the regulation of dendritic growth. The relationship between BDNF levels and anxiety disorders has been shown in clinical studies and animal models of anxiety. It has been reported that BDNF plays a role in ALB in animal models and that various stress factors can lead to decreased BDNF expression [46]. In the present study, DEPO treatment significantly increased BDNF levels in naive rats’ PFC and striatum. In aged rats, BDNF levels increased, especially in the PFC, following recombinant EPO administration [47]. Similar effects have been shown in naive animals treated with various EPO forms. In adult male rodents, BDNF gene expression increased in the dorsal dentate gyrus after CEPO administration without hematopoiesis [48]. After four weeks of recombinant EPO administration, BDNF levels were elevated in aged rats. The same study observed with a moderate increase in BDNF levels in young adult rats [38]. In the present neuroinflammation model with LPS, BDNF levels were severely reduced in both the PFC and striatum. DEPO + LPS group’s rats, the BDNF profile showed recovery. A review by Said et al. reported the positive effect of EPO on BDNF in various neurological injury models [17].
An imbalance between oxidants and antioxidants in favor of oxidants can potentially lead to damage, a condition described as “oxidative stress”. In the present study, TAS was not significantly affected in serum or brain tissue in any group. After DEPO administration, TOS did not change in the striatum but increased in PFC and serum. Furthermore, DEPO administration resulted in increased hemoglobin levels which correlated positively with increased total oxidant levels and a heightened oxidative stress index in the PFC. Oxidation occurs due to increased hemoglobin and autooxygenation mechanisms [49, 50]. This study revealed that the increase in oxidation was positively correlated with the increase in hemoglobin through the autooxidation mechanism. In the present study, different antioxidant mechanisms were also investigated. Thiol, which is an organic compound containing a sulfhydryl group, plays a critical role in preventing the formation of any oxidative stress state in cells. Free thiol, total thiol, and disulfide balance are frequently measured [51]. In the present study, the level of free thiol, an antioxidant marker, was significantly higher in healthy rats after DEPO administration compared to control rats. Our study is an essential preclinical study showing the antioxidant activity of DEPO via free thiol. Supporting our results, Sedriep et al. reported that an increase of total thiol was compatible with elevated EPO and EPO receptor levels in the brain [52]. rHuEPO administration increased total thiol levels in hemodialysis patients [53].
Dysfunction of the HPA axis has been implicated in both anxiety and neuroinflammation There is increased glucorticoid secretion due to dysfunction of the HPA axis. Cortisol, often referred to as a stress hormone, is a vital hormone used to fight the threat caused by anxiety [54]. Although corticosterone is the principal glucocorticoid in rodents, cortisol levels are also frequently analyzed. Gong et al. reported that rodents adapt to acute severe stress with a rapid increase in cortisol response, while they adapt to chronic stress with an increasing corticosteroid response [55]. For this reason, cortisol secretion was examined in serum in the present study. LPS was used as an acute and severe stress to induce neuroinflammation. Our findings indicate that DEPO treatment significantly reduced cortisol levels in the serum, prefrontal cortex (PFC), and striatum of both DEPO and DEPO + LPS groups. Supporting these data, the literature indicates that EPO reduces the secretion of cortisol-secreting factors and corticosteroids. These studies emphasize that EPO attenuates hyperactivity of the HPA axis through its protective effect on the nervous system [56, 57]. After LPS administration, high mortality rates can be observed in the neuroinflammatory model [58]. In the present study, the mortality rate in the group with LPS-induced neuroinflammation was 20%. In the rats that received DEPO treatment before LPS, the survival rate after LPS administration was 100% with no fatalities occurred. Furthermore, prophylactic DEPO treatment ameliorated weight loss.
LPS impairs the function of the blood-brain barrier, and increased levels of TNF-α following LPS administration are associated with this impairment [59]. Our results revealed a negative correlation between elevated levels of proinflammatory cytokines (TNF-α and IL-1β) in both the PFC and the striatum and a reduced duration of anesthesia. Prophylactic DEPO application prolonged loss of posture latency and deep anesthesia latency. Although we could not directly measure the function and permeability of the blood-brain barrier, these results suggest that DEPO may have contributed to maintaining the function and stability of the blood-brain barrier.
DEPO significantly increased hemoglobin, suggesting DEPO treatment may have increased oxygenation. Therefore, DEPO may also have caused similar anxiolytic effects seen with hyperbaric oxygen therapy. The ameliorative effects of hyperbaric oxygen treatment on the brain have been shown by different mechanisms [60]. In support of the present study, Peng et al. reported that prophylactic hyperbaric oxygen treatment produced an anxiolytic effect in rats [61]. EPO binding and EPO-receptor expression have been identified in different tissues, including the heart, blood vessels, kidneys, liver, gastrointestinal tissues, pancreatic islands, testis, female reproductive tract, placenta, prostate, and skeletal muscle [62–64]. DEPO may bind to EPO receptors in these tissues, resulting in a general improvement in systemic inflammation. Furthermore, DEPO may bind to the EPOR receptor in these tissues, releasing some factors into circulation crossing the blood-brain barrier and mediating some effects in the brain.
Prophylactic effects of Darbepoetin alpha or EPO derivatives on anxiety have not yet been demonstrated. Acute mountain sickness (AMS) is a disease affecting individuals who climb high altitudes. AMS is characterized by a headache, gastrointestinal symptoms, weakness, dizziness or lightheadedness, and difficulty sleeping [65]. People exposed to high altitudes often experience somatic symptoms triggered by hypoxia, such as breathlessness, palpitations, dizziness, headache, and insomnia. High altitude might cause anxiety and panic symptoms [66]. Erythropoietin has been identified an effective candidate prophylactic treatment for AMS [65, 67]. Preterm birth is a significant risk factor for psychiatric disorders, including anxiety [68]. Meta-analyses show low-dose prophylactic early erythropoietin might prevent several neonatal complications in preterm infants [69, 70]. Therefore, there is a need for studies showing the possible effects of prophylactic EPO administration against anxiety and psychiatric disorders that may rise in preterm infants as they reach school age. Lippert and Borlongan reported that hyperbaric oxygen treatment (HBOT) preconditioning displayed a prophylactic treatment for neuroinflammation [71]. EPO can reduce inflammation with effects similar to those of HBOT. Some researchers think that prophylactic HBOT can be applied to soldiers at risk of traumatic brain injury and neuroinflammation [60]. Soldiers at risk of traumatic brain injury and neuroinflammation can benefit from prophylactic HBOT.
The interaction between the prefrontal cortex (PFC) and the striatum plays an essential role in cognitive processes [72]. The information coming from the prefrontal cortex is processed in the striatum. In the striatum, the funneling information is processed as a result of being re-integrated by the cortex. With the excessive increase of connections, funneling integration is being disrupted, and anxiety is rising [73]. Brain-derived neurotrophic factor (BDNF) has been shown to be transported from the prefrontal cortex to the striatum via anterograde transport [74]. Therefore, altering BDNF gene expression in the prefrontal cortex may also have consequences in other brain regions, such as the striatum [75]. Anxiety is associated with elevated pro-inflammatory cytokines in the prefrontal cortex and the striatum. It has been reported that increased levels of pro-inflammatory cytokines in both regions are associated with an increase in anxiety-like behaviors [76]. Chemical changes occurring in the prefrontal cortex and the increased activation through the reciprocal projections of both brain regions show that the prefrontal cortex and striatum are target brain areas in anxiety pathology [77, 78]. The presented study supports the idea that the chemical changes observed in the PFK and striatum, such as BDNF and pro-inflammatory cytokines, along with increased anxiety-like behaviors, may indicate that these two brain regions could be target areas for anxiety.
There were several limitations in the present study. First, some basic physiological measurements, such as blood pressure and rectal temperature, were not included, as these parameters may influence anxiety-like behavior (ALB). Additionally, the study was conducted using only male rats due to budgetary and time constraints. We would also like to emphasize that the female ovarian cycle is no longer a fundamental limitation in preclinical studies. Responses to behavioral tests may differ in male and female rats. These differences can be overcome with the experimental protocol and appropriate behavioral tests. We plan to study both male and female rats by considering these differences.
Conclusion
In summary, both darbepoetin alpha applied to DEPO and DEPO + LPS groups showed potent anxiolytic effects. Darbepoetin alpha demonstrated neuroprotective effects on both behavior and molecular pathways in the neuroinflammation model inducing LPS. Our results provide the prophylactic effects of Darbepoetin alpha or EPO derivatives on anxiety, the first evidence in the literature. The use of EPO may serve as a valuable prophylactic option for individuals such as mountain climbers, professionals working at high altitudes, athletes, soldiers, and preterm infants who are at risk for psychiatric disorders. More research is needed to clarify the physiological functions of erythropoietin and its protective healing effects in nervous system diseases.
Acknowledgements
This research was supported by Ankara University Scientific Research Projects Directorate with project number 19L0230011.The presented work received the second prize at the Turkish Physiology Congress in 2023 and congress abstracts were published in Wiley Acta Physiologica.
Author contributions
E.N. and H.Ç. designed and supervised the project. H.Ç. performed the animal experiments and analyzed the data. H.Ç and D.O. performed molecular biology experiments. All authors wrote the manuscript.
Funding
This research was supported by the Ankara University Scientific Research Projects Directorate with project number 19L0230011.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
All procedures were carried out under the approval of the Ankara University Experimental Animals Ethics Committee, and the approval reference number is 2020-2-10.
Consent to publication
Not applicable.
Conflict of interest
The authors declare that they have no conflicts of interest.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Reber AS. The Penguin dictionary of psychology. penguin; 1995.
- 2.Depression W. Other common mental disorders: global health estimates. Geneva: World Health Organization; 2017. p. 24. [Google Scholar]
- 3.Vismara M, et al. Peripheral biomarkers in DSM-5 anxiety disorders: an updated overview. Brain Sci. 2020;10(8):564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zou Z, et al. Differences in cytokines between patients with generalised anxiety disorder and panic disorder. J Psychosom Res. 2020;133:109975. [DOI] [PubMed] [Google Scholar]
- 5.Levine J, et al. Cerebrospinal cytokine levels in patients with acute depression. Neuropsychobiology. 1999;40(4):171–6. [DOI] [PubMed] [Google Scholar]
- 6.Dean B, et al. Different changes in cortical tumor necrosis factor-α-related pathways in schizophrenia and mood disorders. Mol Psychiatry. 2013;18(7):767–73. [DOI] [PubMed] [Google Scholar]
- 7.Khairallah M, et al. Activation of migration of endogenous stem cells by erythropoietin as potential rescue for neurodegenerative diseases. Brain Res Bull. 2016;121:148–57. [DOI] [PubMed] [Google Scholar]
- 8.Rubab S, et al. Enhanced neuroprotective and antidepressant activity of curcumin-loaded nanostructured lipid carriers in lipopolysaccharide-induced depression and anxiety rat model. Int J Pharm. 2021;603:120670. [DOI] [PubMed] [Google Scholar]
- 9.Rhie SJ, Jung E-Y, Shim I. The role of neuroinflammation on pathogenesis of affective disorders. J Exerc Rehabilitation. 2020;16(1):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chateauvieux S, et al. Erythropoietin, erythropoiesis and beyond. Biochem Pharmacol. 2011;82(10):1291–303. [DOI] [PubMed] [Google Scholar]
- 11.Wang RL, et al. Erythropoietin-derived peptide ARA290 mediates brain tissue protection through the β‐common receptor in mice with cerebral ischemic stroke. CNS Neurosci Ther. 2024;30(3):e14676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moon C, et al. Erythropoietin reduces myocardial infarction and left ventricular functional decline after coronary artery ligation in rats. Proc Natl Acad Sci. 2003;100(20):11612–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gilboa D, et al. Erythropoietin enhances Kupffer cell number and activity in the challenged liver. Sci Rep. 2017;7(1):10379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Buemi M, et al. Recombinant human erythropoietin stimulates angiogenesis and healing of ischemic skin wounds. Shock. 2004;22(2):169–73. [DOI] [PubMed] [Google Scholar]
- 15.Chen LN, et al. Erythropoietin improves glucose metabolism and pancreatic β-cell damage in experimental diabetic rats. Mol Med Rep. 2015;12(4):5391–8. [DOI] [PubMed] [Google Scholar]
- 16.Brines ML, et al. Erythropoietin crosses the blood–brain barrier to protect against experimental brain injury. Proc Natl Acad Sci. 2000;97(19):p10526–10531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Said MF, Islam AA, Massi MN. Effect of erythropoietin administration on the expression of brain-derived neurotrophic factor, stromal cell-derived Factor-1, and neuron-specific enolase in traumatic brain injury: a literature review. Annals Med Surg. 2021;69:102666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chong ZZ, Kang J-Q, Maiese K. Hematopoietic factor erythropoietin fosters neuroprotection through novel signal transduction cascades. J Cereb Blood Flow Metabolism. 2002;22(5):503–14. [DOI] [PubMed] [Google Scholar]
- 19.Coccia MA, et al. Novel erythropoiesis stimulating protein (darbepoetin alfa) alleviates anemia associated with chronic inflammatory disease in a rodent model. Exp Hematol. 2001;29(10):1201–9. [DOI] [PubMed] [Google Scholar]
- 20.Cazareth J, et al. Molecular and cellular neuroinflammatory status of mouse brain after systemic lipopolysaccharide challenge: importance of CCR2/CCL2 signaling. J Neuroinflamm. 2014;11:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Caliskan H, et al. Effects of exercise training on anxiety in diabetic rats. Behav Brain Res. 2019;376:112084. [DOI] [PubMed] [Google Scholar]
- 22.Çalışkan H, et al. Duloxetine alleviates high light-induced anxiety-related behaviors in Wistar rats. Trop J Pharm Res. 2019;18(11):2319–23. [Google Scholar]
- 23.Burn CC, et al. Long-term effects of cage-cleaning frequency and bedding type on laboratory rat health, welfare, and handleability: a cross-laboratory study. Lab Anim. 2006;40(4):353–70. [DOI] [PubMed] [Google Scholar]
- 24.Poveshchenko A, et al. Cytokine gene expression in cerebral hemispheres and behavioral reactions of (CBA× C57Bl) F1 mice. Bull Exp Biol Med. 2002;133:65–7. [DOI] [PubMed] [Google Scholar]
- 25.Osborn M, et al. Antidepressant-like effects of erythropoietin: a focus on behavioural and hippocampal processes. PLoS ONE. 2013;8(9):e72813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Köllensperger M, et al. Erythropoietin is neuroprotective in a transgenic mouse model of multiple system atrophy. Mov Disord. 2011;26(3):507–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gao Y, et al. Dihydroartemisinin ameliorates LPS-induced neuroinflammation by inhibiting the PI3K/AKT pathway. Metab Brain Dis. 2020;35:661–72. [DOI] [PubMed] [Google Scholar]
- 28.Arab Z, et al. Zataria multiflora extract reverses lipopolysaccharide-induced anxiety and depression behaviors in rats. Avicenna J Phytomedicine. 2020;10(1):78. [PMC free article] [PubMed] [Google Scholar]
- 29.Dayyat EA, et al. Exogenous erythropoietin administration attenuates intermittent hypoxia-induced cognitive deficits in a murine model of sleep apnea. BMC Neurosci. 2012;13:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yamanashi T, et al. Beta-hydroxybutyrate, an endogenic NLRP3 inflammasome inhibitor, attenuates stress-induced behavioral and inflammatory responses. Sci Rep. 2017;7(1):7677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Leconte C, et al. Comparison of the effects of erythropoietin and its carbamylated derivative on behaviour and hippocampal neurogenesis in mice. Neuropharmacology. 2011;60(2–3):354–64. [DOI] [PubMed] [Google Scholar]
- 32.Miskowiak K, O’Sullivan U, Harmer CJ. Erythropoietin enhances hippocampal response during memory retrieval in humans. J Neurosci. 2007;27(11):2788–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Miskowiak K, O’Sullivan U, Harmer CJ. Erythropoietin reduces neural and cognitive processing of fear in human models of antidepressant drug action. Biol Psychiatry. 2007;62(11):1244–50. [DOI] [PubMed] [Google Scholar]
- 34.Miskowiak KW, et al. Erythropoietin modulates neural and cognitive processing of emotional information in biomarker models of antidepressant drug action in depressed patients. Psychopharmacology. 2010;210:419–28. [DOI] [PubMed] [Google Scholar]
- 35.Miskowiak KW, et al. Neural correlates of improved executive function following erythropoietin treatment in mood disorders. Psychol Med. 2016;46(8):1679–91. [DOI] [PubMed] [Google Scholar]
- 36.Schmidt LS, et al. Erythropoietin as an add-on treatment for cognitive side effects of electroconvulsive therapy: a study protocol for a randomized controlled trial. Trials. 2018;19:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kurutas EB. Erythropoietin and erythropoietin receptor levels and their diagnostic values in Drug- naïve patients with generalized anxiety disorder. Clin Psychopharmacol Neurosci. 2023;21(2):288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jia Z, et al. Erythropoietin attenuates the memory deficits in aging rats by rescuing the oxidative stress and inflammation and promoting BDNF releasing. Mol Neurobiol. 2016;53:5664–70. [DOI] [PubMed] [Google Scholar]
- 39.Zhang C-y, et al. Erythropoietin attenuates propofol-induced hippocampal neuronal cell injury in developing rats by inhibiting toll-like receptor 4 expression. Neurosci Lett. 2020;716:134647. [DOI] [PubMed] [Google Scholar]
- 40.Kumral A, et al. Erythropoietin attenuates lipopolysaccharide-induced white matter injury in the neonatal rat brain. Neonatology. 2007;92(4):269–78. [DOI] [PubMed] [Google Scholar]
- 41.Maurice T, et al. Intranasal formulation of erythropoietin (EPO) showed potent protective activity against amyloid toxicity in the Aβ25–35 non-transgenic mouse model of Alzheimer’s disease. J Psychopharmacol. 2013;27(11):1044–57. [DOI] [PubMed] [Google Scholar]
- 42.Lambe EK, et al. Serotonin receptor expression in human prefrontal cortex: balancing excitation and inhibition across postnatal development. PLoS ONE. 2011;6(7):e22799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Virk MS et al. Opposing roles for serotonin in cholinergic neurons of the ventral and dorsal striatum. Proceedings of the National Academy of Sciences, 2016. 113(3): pp. 734–739. [DOI] [PMC free article] [PubMed]
- 44.Zhao X, et al. Behavioral, inflammatory and neurochemical disturbances in LPS and UCMS-induced mouse models of depression. Behav Brain Res. 2019;364:494–502. [DOI] [PubMed] [Google Scholar]
- 45.Miura H, et al. Shifting the balance of brain tryptophan metabolism elicited by isolation housing and systemic administration of lipopolysaccharide in mice. Stress. 2009;12(3):206–14. [DOI] [PubMed] [Google Scholar]
- 46.Suliman S, Hemmings SM, Seedat S. Brain-derived neurotrophic factor (BDNF) protein levels in anxiety disorders: systematic review and meta-regression analysis. Front Integr Nuerosci. 2013;7:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wang H-Q, et al. Effects of recombinant human erythropoietin on brain-derived neurotrophic factor expression in different brain regions of aging rats. Nan Fang Yi Ke da xue xue bao = J South Med Univ. 2016;37(4):551–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sathyanesan M, et al. Carbamoylated erythropoietin modulates cognitive outcomes of social defeat and differentially regulates gene expression in the dorsal and ventral hippocampus. Translational Psychiatry. 2018;8(1):113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rifkind JM, Mohanty JG, Nagababu E. The pathophysiology of extracellular hemoglobin associated with enhanced oxidative reactions. Front Physiol. 2015;5:117808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pandey KB, Rizvi SI. Markers of oxidative stress in erythrocytes and plasma during aging in humans. Oxidative Med Cell Longev. 2010;3:2–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Yazar H, et al. An analysis of plasma thiol/disulphide homeostasis in patients with stable angina. Online Türk Sağlık Bilimleri Dergisi. 2020;5(2):318–23. [Google Scholar]
- 52.Sedriep S, et al. Beneficial nutraceutical modulation of cerebral erythropoietin expression and oxidative stress: an experimental study. J Biol Regul Homeost Agents. 2011;25(2):187. [PubMed] [Google Scholar]
- 53.Usberti M, et al. Effects of erythropoietin and vitamin E-modified membrane on plasma oxidative stress markers and anemia of hemodialyzed patients. Am J Kidney Dis. 2002;40(3):590–9. [DOI] [PubMed] [Google Scholar]
- 54.Stahl SM. Stahl’s essential psychopharmacology: neuroscientific basis and practical applications. Cambridge University Press; 2021.
- 55.Gong S, et al. Dynamics and correlation of serum cortisol and corticosterone under different physiological or stressful conditions in mice. PLoS ONE. 2015;10(2):e0117503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dey S, Scullen T, Noguchi CT. Erythropoietin negatively regulates pituitary ACTH secretion. Brain Res. 2015;1608:14–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tringali G, et al. Erythropoietin inhibits basal and stimulated corticotropin-releasing hormone release from the rat hypothalamus via a nontranscriptional mechanism. Endocrinology. 2007;148(10):4711–5. [DOI] [PubMed] [Google Scholar]
- 58.An N, et al. Pretreatment of mice with rifampicin prolongs survival of endotoxic shock by modulating the levels of inflammatory cytokines. Immunopharmacol Immunotoxicol. 2008;30(3):437–46. [DOI] [PubMed] [Google Scholar]
- 59.Ghosh A, et al. Assessment of blood-brain barrier function and the neuroinflammatory response in the rat brain by using cerebral open flow microperfusion (cOFM). PLoS ONE. 2014;9(5):e98143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Eve DJ et al. Hyperbaric oxygen therapy as a potential treatment for post-traumatic stress disorder associated with traumatic brain injury. Neuropsychiatr Dis Treat, 2016. pp. 2689–705. [DOI] [PMC free article] [PubMed]
- 61.Peng Y, et al. Hyperbaric oxygen preconditioning ameliorates anxiety-like behavior and cognitive impairments via upregulation of thioredoxin reductases in stressed rats. Prog Neuropsychopharmacol Biol Psychiatry. 2010;34(6):1018–25. [DOI] [PubMed] [Google Scholar]
- 62.Jelkmann W. The erythropoietin receptor in normal and cancer tissues. Crit Rev Oncol Hematol. 2008;67(1):39–61. [DOI] [PubMed] [Google Scholar]
- 63.Maiese K, et al. New avenues of exploration for erythropoietin. JAMA. 2005;293(1):90–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Nijholt KT, et al. The erythropoietin receptor expressed in skeletal muscle is essential for mitochondrial biogenesis and physiological exercise. Pflugers Arch. 2021;473(8):1301–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Heo K, et al. Prophylactic effect of erythropoietin injection to prevent acute mountain sickness: an open-label randomized controlled trial. J Korean Med Sci. 2014;29(3):416–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wang YH, et al. Acute Mountain sickness and the risk of subsequent Psychiatric Disorders—A Nationwide Cohort Study in Taiwan. Int J Environ Res Public Health. 2023;20:2868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Heldeweg MLA, et al. Altitude Pre-acclimatization with an erythropoiesis-stimulating Agent. Eur J Case Rep Intern Med. 2023;10(4):003792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Johnson S, Marlow NP. Birth and Childhood Psychiatric disorders. Pediatr Res. 2011;69:11–8. [DOI] [PubMed] [Google Scholar]
- 69.Liang L, et al. Sustained low-dose prophylactic early erythropoietin for improvement of neurological outcomes in preterm infants: a systematic review and meta-analysis. J Affect Disord. 2021;282:1187–92. [DOI] [PubMed] [Google Scholar]
- 70.Fischer HS, et al. Prophylactic erythropoietin for neuroprotection in very preterm infants: a meta-analysis update. Front Pead. 2021;9:657228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lippert T, Borlongan CV. Prophylactic treatment of hyperbaric oxygen treatment mitigates inflammatory response via mitochondria transfer. CNS Neurosci Ther. 2019;25(8):815–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zhang Y, et al. Functional connectivity between prefrontal cortex and striatum estimated by phase locking value. Cogn Neurodyn. 2016;10(3):245–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Marchand WR. Cortico-basal ganglia circuitry: a review of key research and implications for functional connectivity studies of mood and anxiety disorders. Brain Struct Funct. 2010;215:73–96. [DOI] [PubMed] [Google Scholar]
- 74.Altar CA, et al. Anterograde transport of brain-derived neurotrophic factor and its role in the brain. Nature. 1997;389(6653):856–60. [DOI] [PubMed] [Google Scholar]
- 75.Roceri M, et al. Postnatal repeated maternal deprivation produces age-dependent changes of brain-derived neurotrophic factor expression in selected rat brain regions. Biol Psychiatry. 2004;55(7):708–14. [DOI] [PubMed] [Google Scholar]
- 76.Yu H, et al. Suppressive effects of Gelsemine on anxiety-like behaviors Induced by Chronic unpredictable mild stress in mice. Brain Sci. 2022;12(2):191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Macpherson T, Hikida T. Role of basal ganglia neurocircuitry in the pathology of psychiatric disorders. J Neuropsychiatry Clin Neurosci. 2019;73(6):289–301. [DOI] [PubMed] [Google Scholar]
- 78.Sgambato-Faure V, Tremblay L. Dopamine and serotonin modulation of motor and non-motor functions of the non-human primate striato-pallidal circuits in normal and pathological states. J Neural Transm. 2018;125(3):485–500. [DOI] [PubMed] [Google Scholar]
- 79.Paxinos G, Watson C. The rat brain in stereotaxic coordinates: hard cover edition. Elsevier; 2006.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.