Abstract
Background
Measles, a highly contagious and potentially fatal disease, remains a significant public health concern, particularly in low- and middle-income countries. Vaccination is the most effective way to prevent measles and achieving high immunization coverage is crucial for protecting children and communities. This study investigated the trends and inequalities in measles immunization coverage among two-year-olds in Sierra Leone between 2008 and 2019.
Methods
The study utilized data from the Sierra Leone Demographic Health Surveys conducted in 2008, 2013, and 2019. The World Health Organisation Health Equity Assessment Toolkit was used to calculate various inequality measures, including Difference (D), Ratio (R), Population Attributable Risk (PAR), and Population Attributable Fraction (PAF). An inequality assessment was conducted for six stratifiers: age, economic status, level of education, place of residence, sex of the child, and sub-national province.
Results
In Sierra Leone, measles immunization coverage increased between 2008 and 2013 and decreased slightly in 2019. In 2008, 66.2% of two-year-olds were immunized, which increased to 86.2% in 2013 and then fell slightly to 82.2% in 2019. There was a decrease in inequality for age from 4.2 percentage points in 2008 to 3.0 percentage points in 2019 (D = 4.2 in 2008 and 3.0 in 2019). Economic-related inequality decreased from 8.1 percentage points in 2008 to 7.5 percentage points in 2019 (D = 8.1 in 2008 and 7.5 in 2019). Inequality in education decreased from 10.3 percentage points in 2008 to 7.4 percentage points in 2019 based on results from the inequality measure D. For place of residence, inequality decreased from 6.0 percentage points in 2008 to 4.0 percentage points in 2019. For the child’s sex, the inequality increased from 1.9 percentage points in 2008 to 4.5 percentage points in 2019. The PAF revealed that the setting average could have been 1.4% higher in 2008 and 2.7% higher in 2019 without the child’s sex inequality. Provincial inequality decreased from 19.4 percentage points in 2008 to 16.9 percentage points in 2019 (D = 19.4 in 2008 and 16.9 in 2019).
Conclusion
The observed fluctuations in national measles immunization coverage for children under two underscore the need for sustained efforts in vaccination programs. While improvements in access based on age, socioeconomic status, education level, and place of residence suggest progress in reducing inequalities, the persistent provincial disparities, with a significant gap in 2019, highlight ongoing challenges that must be addressed to ensure equitable health outcomes. Additionally, the increase in inequalities based on the child’s sex during the study period raises concerns about targeted interventions that may inadvertently neglect specific groups. These findings imply that policymakers must prioritize strategies that maintain high vaccination rates and focus on closing the geographical and sex-based gaps, particularly in underserved provinces and among vulnerable populations.
Keywords: Children, Immunization, Measles, Public health, Sierra Leone
Introduction
Measles, a highly contagious viral disease, can cause severe complications like pneumonia, encephalitis, and even death [1–3]. Fortunately, measles immunization offers a powerful shield against this devastating illness. Immunisation coverage refers to the percentage of children who have received the measles vaccine by a specific age, typically by their second birthday [4, 5]. High immunization coverage is essential to achieve herd immunity, a phenomenon where widespread vaccination indirectly protects those who cannot vaccinate for medical reasons. This collective protection is crucial for preventing outbreaks and safeguarding vulnerable populations [6–8].
Immunisation plays a vital role in child health and survival, especially in low-resource settings with limited access to healthcare infrastructure [3, 6, 8]. By preventing measles and its associated complications, immunization programs contribute significantly to a healthier childhood and a brighter future for children [7]. Despite significant progress in recent decades, global measles immunization coverage remains uneven [3, 7, 9]. While global coverage for the first dose of the measles vaccine (MCV1) stands at approximately 86%, there remains a substantial gap for the second dose (MCV2), with coverage hovering around 71% in 2019 [10]. In comparison, the coverage for the third dose of the diphtheria-tetanus-pertussis vaccine (DTP3) is also crucial to consider. DTP3 coverage has consistently outperformed MCV1 in many regions, highlighting a disparity in vaccination uptake. Notably, some countries, especially in the African region, have yet to introduce MCV1. This absence may contribute to the continued low global coverage rates for measles vaccinations and underscores the need for targeted interventions to improve access and uptake of both MCV1 and MCV2 [11–13].
Sierra Leone’s journey with measles immunization coverage reflects a commendable effort towards improvement, yet challenges remain. Demographic and Health Surveys (DHS) data indicate that coverage rates have improved over time but haven’t reached the desired 6th threshold. Furthermore, significant disparities exist across different regions and socioeconomic groups. In response to this situation, the Government of Sierra Leone, in collaboration with international organizations like WHO and UNICEF, has implemented various interventions and policies. These efforts include mass immunization campaigns, routine immunization services, and community outreach programs. Despite these initiatives, various obstacles continue to hinder progress [14]. Logistical hurdles, inadequate healthcare infrastructure, disruptions in vaccine supply chains, and socio-cultural barriers pose significant challenges [15]. Additionally, the Ebola and COVID-19 pandemic further strained the healthcare system, impacting routine immunization services [15]. Addressing these challenges requires sustained commitment from stakeholders and innovative strategies to ensure timely and complete immunization for all children.
Previous national studies have explored immunization coverage in Sierra Leone [14, 15]. However, a critical knowledge gap exists regarding the specific socioeconomic and geographical inequalities in measles immunization coverage among two-year-olds. Existing research [14] focuses on overall immunization coverage without dissecting the disparities between different population groups and provinces. This study addresses this knowledge gap by examining the inequalities in measles immunization coverage among two-year olds in Sierra Leone. By identifying socioeconomic and geographical disparities in measles immunization coverage among two-year-olds in Sierra Leone from 2008 to 2019, we aim to provide valuable insights that inform targeted interventions to improve immunization rates and achieve more equitable health outcomes. This research holds significant value for multiple stakeholders: it will offer policymakers evidence-based recommendations to strengthen immunization programs and address existing disparities in coverage; researchers will gain insights into socioeconomic and geographic inequalities, paving the way for further investigation; and international partners and donors will access critical data to guide funding decisions aimed at improving child health and immunization rates in Sierra Leone.
Methods
Study design and source
We used data from the 2008, 2013, and 2019 Sierra Leone Demographic Health Surveys (SLDHS). The SLDHS is a nationwide survey that aims to discover consistent trends and variations in demographic indicators, health indicators, and social issues across all genders and age groups. The study utilized a cross-sectional design, where participants were chosen using a stratified multi-stage cluster sampling technique. The SLDHS report thoroughly explains the sampling process [16]. This study involved mothers who submitted measles immunization data on their children who were two years old as many national immunization schedules recommend measles vaccinations at around 12 months and 18 months of age. Therefore, two-year-olds would have received both doses of the measles vaccine, making them a representative group to assess immunization coverage. The 2008, 2013, and 2019 SLDHS data were available via the WHO HEAT online platform [17]. The study was done in accordance with the guidelines outlined in the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines [18].
Variables
Measles vaccination coverage among children aged two years was the outcome variable in this study. It was calculated in the toolkit for children aged two years. The variable represents the proportion of children between the ages of 12 and 23 months who have had at least one dose of the measles vaccine before the survey. This information is based on the vaccination card presented to the interviewer, as reported by the mother. In instances when the interviewee did not present a card (i.e., this choice was absent), the mother’s report served as the source of information regarding the child’s measles vaccination status. If the mother’s vaccination report was absent, it was recorded as an indication that no measles vaccine had been administered. The variables used as stratifiers were age of the mother, economic status, education, places of residence, sex of the child, and sub-national province. Age was categorized into 15–19 and 20–49. The economic status was classified into five groups: the poorest, poor, middle, rich, and richest. The maternal education status was categorized into three groups: no, primary, and secondary or higher education. The place of residence was either urban or rural. The sex of the child was recorded as male or female. The sub-national province consisted of five areas.
Data analysis
The analysis was performed via the web-based version of the WHO Health Equity Assessment Toolkit (HEAT) programme [17]. This software contains the variable of interest (measles immunization coverage) disaggregated by six dimensions of inequality, allowing for a comprehensive examination of measles immunization coverage. Additionally, HEAT provides estimates, confidence intervals, and summary measures of inequality, enabling us to effectively assess inequalities in immunization coverage and make informed conclusions based on the data. The analysis began with data selection, where relevant datasets on measles immunization coverage, socioeconomic status, and geographical distribution were gathered from the SLDHS. We used the software’s visualization tools to explore our data and identify potential patterns or disparities. We applied the HEAT software’s analytical tools to assess health inequalities. This includes calculating summary measures of health inequality. Using the designated stratifiers, estimates and confidence intervals (CIs) for measles immunization coverage among two-year-olds were calculated within the HEAT software. Four metrics were utilized to compute inequality: Difference (D), Population Attributable Risk (PAR), Population Attributable Fraction (PAF), and Ratio (R). D measures the absolute gap in measles immunization coverage between two subgroups (usually sub-groups with higher and lower coverage), comparing their respective rates. A higher D value indicates greater inequality. R compares the measles immunization coverage of two subgroups by dividing the coverage of the subgroup with the highest coverage by the one with the lowest coverage, offering a relative measure of inequality. An R value greater than 1 indicates lower measles immunization coverage in the disadvantaged group. Both D and R are unweighted measures, meaning they do not account for the population sizes of the subgroups and focus solely on the two groups being compared. On the other hand, PAR estimates the proportion of a health outcome that can be attributed to a specific risk factor within the population, while PAF indicates the percentage of the total health outcome that would be eliminated if the risk factor were removed. A positive PAF suggests that reducing inequalities would lead to a decrease in overall measles immunization coverage and a higher PAR indicates a greater impact of inequalities on measles immunization coverage. These measures provide insights into the potential impact of reducing inequalities on overall health outcomes. R and PAF are relative measures of inequality used to evaluate and compare the differences between various elements in relation to one another. In contrast, D and PAR are absolute measures, providing clear-cut values indicating the gap in vaccination coverage or the proportion of health outcomes attributable to a specific risk factor. This distinction is important, as absolute measures like D and PAR offer straightforward insights into the magnitude of inequality, while relative measures like R and PAF contextualize these differences within the broader population dynamics. The inclusion of summary measures is predicated on the recognition by the World Health Organisation that both absolute and relative summary metrics are essential for deriving policy-relevant findings. The literature extensively elucidates the summary measures and calculations of the World Health Organisation metrics [19, 20].
Results
Trends of measles immunization coverage among two-year-olds in Sierra Leone by different inequality stratifiers
Table 1 shows measles immunization coverage trends among two-year-olds in Sierra Leone by different inequality stratifiers. The data is presented as the number of individuals (N), percentage (%), and confidence intervals (Lower Bound [LB] and Upper Bound [UB]). Overall, measles immunization coverage increased between 2008 and 2013, then decreased slightly in 2019. In 2008, 66.2% of two-year-olds were immunized, which increased to 86.2% in 2013 and then fell to 82.2% in 2019. Coverage was generally higher among mothers aged 20–49 compared to younger mothers (15–19 years old). Coverage increased as economic status increased. In all survey years, the richest quintile (Quintile 5) had the highest coverage, while the poorest quintile (Quintile 1) had the lowest coverage. Coverage was generally higher among mothers with more education. No education resulted in the lowest coverage, while secondary or higher education resulted in the highest coverage. While coverage was generally higher in urban areas compared to rural areas, it is important to note that this may not fully reflect the situation for all urban residents. In many sub-Saharan African countries, including Sierra Leone, there may be disparities in access and utilization of social services, such as vaccination, between the urban core and more peripheral or suburban areas. These disparities can lead to gaps in coverage among urban populations, particularly those with lower socioeconomic status. There was not a significant difference in coverage between male and female children. In 2019, coverage was highest in the Northern province (87.7%) and lowest in the northwestern province (70.8%).
Table 1.
Trends in the prevalence of measles immunization coverage among two-year-olds by different inequality dimensions in Sierra Leone, 2008–2019
| 2008(66.2%) | 2013 (86.2%) | 2019 (82.2%) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Dimension | N | %. | LB | UB | N | %. | LB | UB | N | %. | LB | UB |
| Age | ||||||||||||
| 15–19 years | 57 | 62.2 | 46.0 | 76.1 | 129 | 88.7 | 80.8 | 93.7 | 85 | 79.3 | 67.1 | 87.7 |
| 20–49 years | 881 | 66.4 | 62.4 | 70.2 | 1881 | 86.0 | 83.4 | 88.3 | 1580 | 82.3 | 79.9 | 84.5 |
| Economic status | ||||||||||||
| Quintile 1 (poorest) | 196 | 63.1 | 54.5 | 71.0 | 480 | 85.8 | 81.3 | 89.3 | 378 | 76.9 | 71.2 | 81.7 |
| Quintile 2 | 197 | 61.4 | 52.3 | 69.7 | 470 | 84.3 | 79.0 | 88.5 | 370 | 81.3 | 76.0 | 85.6 |
| Quintile 3 | 233 | 62.8 | 55.8 | 69.3 | 392 | 86.1 | 81.8 | 89.5 | 343 | 84.7 | 79.5 | 88.8 |
| Quintile 4 | 176 | 75.5 | 67.3 | 82.2 | 393 | 88.3 | 83.8 | 91.6 | 309 | 84.9 | 80.3 | 88.6 |
| Quintile 5 (richest) | 134 | 71.3 | 61.8 | 79.2 | 275 | 87.4 | 77.7 | 93.2 | 264 | 84.4 | 77.4 | 89.5 |
| Education | ||||||||||||
| No education | 731 | 62.9 | 58.2 | 67.4 | 1431 | 85.3 | 82.3 | 87.9 | 889 | 80.0 | 76.6 | 83.0 |
| Primary education | 107 | 81.9 | 71.6 | 89.0 | 276 | 84.3 | 77.5 | 89.3 | 240 | 78.3 | 71.5 | 83.9 |
| Secondary or higher education | 99 | 73.3 | 61.5 | 82.5 | 303 | 92.1 | 87.6 | 95.1 | 535 | 87.5 | 83.7 | 90.5 |
| Residence | ||||||||||||
| Rural | 686 | 64.5 | 59.6 | 69.2 | 1543 | 85.9 | 83.0 | 88.4 | 1076 | 80.7 | 77.4 | 83.6 |
| Urban | 252 | 70.6 | 64.5 | 76.1 | 467 | 87.1 | 81.5 | 91.2 | 589 | 84.8 | 80.7 | 88.2 |
| Sex of child | ||||||||||||
| Female | 462 | 65.2 | 59.5 | 70.5 | 1035 | 85.9 | 82.4 | 88.9 | 843 | 79.9 | 75.9 | 83.4 |
| Male | 476 | 67.1 | 62.0 | 71.9 | 975 | 86.5 | 83.6 | 88.9 | 821 | 84.4 | 81.4 | 87.0 |
| Province | ||||||||||||
| Eastern | 195 | 71.5 | 64.0 | 78.0 | 494 | 88.0 | 82.9 | 91.7 | 355 | 82.5 | 76.2 | 87.4 |
| Northern | 415 | 56.6 | 50.5 | 62.6 | 745 | 83.5 | 79.3 | 87.0 | 289 | 87.7 | 82.7 | 91.4 |
| Northwestern | NA | NA | NA | NA | NA | NA | NA | NA | 320 | 70.8 | 63.7 | 77.0 |
| Southern | 199 | 74.6 | 65.4 | 82.0 | 540 | 90.2 | 85.4 | 93.6 | 394 | 84.2 | 80.0 | 87.6 |
| Western | 128 | 76.1 | 67.3 | 83.1 | 230 | 81.6 | 71.0 | 88.9 | 305 | 85.9 | 79.6 | 90.4 |
N-Sample size; NA-Not available as between 2008 and 2013, Sierra Leone had four regions: LB-Lower Bound; UB-Upper Bound
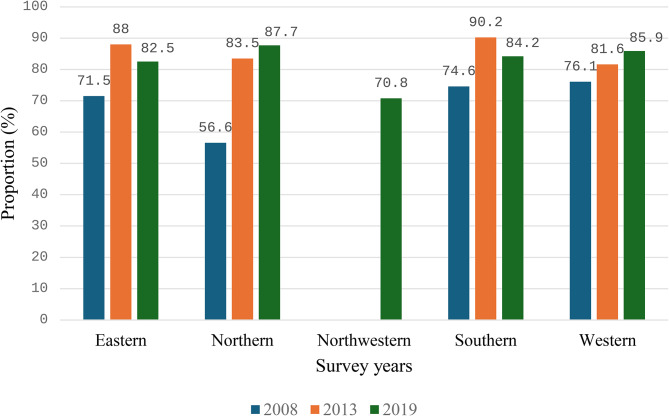
Provincial prevalence of measles immunization coverage among two-year-olds in Sierra Leone in 2008, 2013 and 2019
Figure 1 shows the provincial prevalence of measles immunization coverage among two-year-olds in Sierra Leone in 2008, 2013 and 2019. Each bar represents the percentage of immunization coverage, illustrating trends over time across different subnational province in this particular order in 2019 (Eastern, Northern, Northwest, Southern, and Western). Between 2008 and 2013 Sierra Leone had four subnational provinces (Eastern, Northern, Southern, and Western). Approximately 76.1% of children of mothers in the Western province had measles immunization in 2008, whilst in the coverage was only 56.6% in the Northern province. In 2013, 90.2% of children of mothers in the Southern province had measles immunization whilst 81.6% of children of mothers in the Western province were immunized against measles. In 2019, measles vaccination coverage was 87.7% in the Northern province and 70.8% in the Northwestern province.
Fig. 1.
Provincial prevalence of measles immunization coverage among two-year-olds in Sierra Leone in 2008, 2013 and 2019
Trends in inequality indices for measles immunization coverage in Sierra Leone (2008–2019)
Table 2 shows inequality indices for measles immunization coverage in Sierra Leone from 2008 to 2019. Here, we present the results for one absolute measure (D) and one relative measure (PAF). One of them (D) is a simple measure and PAF is a complex measure. There was a decrease in inequality for age from 4.2 percentage points in 2008 to 3.0 percentage points in 2019 (D = 4.2 in 2008 and 3.0 in 2019). The PAF reveal that the setting average could have been 0.3% higher in 2008 and 0.1% higher in 2019 without age inequality. Economic disparity decreased from 8.1 percentage points in 2008 to 7.5 percentage points in 2019 (D = 8.1 in 2008 and 7.5 in 2019). PAF in 2008 was 7.6 and 2.7 in 2019, indicating that the setting average in measles vaccination coverage could have increased by almost 8% in 2008 and 3% in 2019 without economic inequality. Inequality in education decreased from 10.3 percentage points in 2008 to 7.4 percentage points in 2019 (D = 10.3 in 2008 and 7.4 in 2019). For place of residence, inequality decreased from a D of 6.0 percentage points in 2008 to 4.0 percentage points in 2019. For the child’s sex, the inequality increased from a D of 1.9 percentage points in 2008 to 4.5 percentage points in 2019. The PAF revealed that the setting average could have been 1.4% higher in 2008 and 2.7% higher in 2019 without the child’s sex inequality. Provincial inequality decreased from a D of 19.4 percentage points in 2008 to 16.9 percentage points in 2019. The PAF revealed that the setting average could have been 15% higher in 2008, 5% higher in 2013, and 7% higher in 2019 without provincial inequality.
Table 2.
Inequality indices of estimates of factors associated with measles immunization coverage among two-year-olds in Sierra Leone, 2008–2019
| 2008 | 2013 | 2019 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Dimension | Est. | LB | UB | Est. | LB | UB | Est. | LB | UB |
| Age | |||||||||
| D | 4.2 | -11.6 | 20.0 | -2.6 | -9.4 | 4.0 | 3.0 | -7.4 | 13.5 |
| PAF | 0.3 | 0.3 | 0.4 | 0 | -0.0 | 0.0 | 0.1 | 0.1 | 0.1 |
| PAR | 0.2 | -0.5 | 1.0 | 0 | -0.3 | 0.3 | 0.1 | -0.2 | 0.6 |
| R | 1.0 | 0.8 | 1.3 | 0.9 | 0.8 | 1.0 | 1.0 | 0.9 | 1.1 |
| Economic status | |||||||||
| D | 8.1 | -3.8 | 20.1 | 1.5 | -6.9 | 10.1 | 7.5 | -0.4 | 15.4 |
| PAF | 7.6 | 7.5 | 7.7 | 1.3 | 1.3 | 1.4 | 2.7 | 2.6 | 2.7 |
| PAR | 5.0 | -2.0 | 12.2 | 1.1 | -2.4 | 4.8 | 2.2 | -1.8 | 6.2 |
| R | 1.1 | 0.9 | 1.3 | 1.0 | 0.9 | 1.1 | 1.0 | 0.9 | 1.2 |
| Education | |||||||||
| D | 10.3 | -1.0 | 21.8 | 6.8 | 2.2 | 11.4 | 7.4 | 2.8 | 12.1 |
| PAF | 10.7 | 10.6 | 10.8 | 6.8 | 6.8 | 6.9 | 6.4 | 6.4 | 6.4 |
| PAR | 7.1 | -1.1 | 15.4 | 5.9 | 2.9 | 8.8 | 5.3 | 2.8 | 7.8 |
| R | 1.1 | 0.9 | 1.3 | 1.0 | 1.0 | 1.1 | 1.0 | 1.0 | 1.1 |
| Residence | |||||||||
| D | 6.0 | -1.4 | 13.6 | 1.2 | -4.3 | 6.7 | 4.0 | -0.7 | 8.9 |
| PAF | 6.7 | 6.6 | 6.8 | 1.0 | 1.0 | 1.1 | 3.2 | 3.1 | 3.2 |
| PAR | 4.4 | -0.4 | 9.3 | 0.9 | -1.7 | 3.6 | 2.6 | 0.2 | 5.0 |
| R | 1.0 | 0.9 | 1.2 | 1.0 | 0.9 | 1.0 | 1.0 | 0.9 | 1.1 |
| Sex of child | |||||||||
| D | 1.9 | -5.4 | 9.3 | 0.5 | -3.6 | 4.7 | 4.5 | -0.1 | 9.1 |
| PAF | 1.4 | 1.3 | 1.4 | 0.3 | 0.3 | 0.3 | 2.7 | 2.7 | 2.8 |
| PAR | 0.9 | -2.0 | 3.9 | 0.2 | -1.2 | 1.8 | 2.2 | 0.4 | 4.1 |
| R | 1.0 | 0.9 | 1.1 | 1.0 | 0.9 | 1.0 | 1.0 | 0.9 | 1.1 |
| Province | |||||||||
| D | 19.4 | 9.5 | 29.4 | 8.6 | -1.0 | 18.3 | 16.9 | 8.9 | 24.8 |
| PAF | 14.9 | 14.8 | 15.0 | 4.6 | 4.6 | 4.7 | 6.7 | 6.6 | 6.7 |
| PAR | 9.8 | 2.8 | 16.9 | 4.0 | 1.7 | 6.3 | 5.5 | 1.9 | 9.1 |
| R | 1.3 | 1.1 | 1.5 | 1.1 | 0.9 | 1.2 | 1.2 | 1.1 | 1.3 |
Est-Estimate; LB-Lower Bound; UB-Upper Bound
Discussion
This study examines the socioeconomic and geographical inequalities in measles immunization coverage among two-year-olds in Sierra Leone from 2008, 2013 and 2019. Coverage increased between 2008 and 2013, but declined slightly in 2019. The decline in 2019 may be attributed to several factors, including the impact of the Ebola outbreak between 2013 and 2014. The outbreak likely disrupted healthcare services, including immunization programs, leading to a temporary decline in coverage. Additionally, other factors such as economic instability, population displacement, and changes in immunization policies or implementation may have contributed to the decline. Addressing these underlying issues and implementing strategies to improve immunization coverage is crucial to protect the health of the population and prevent measles outbreaks in Sierra Leone. A study on measles incidence trends in Nigeria found fluctuating MCV coverage, as there was a slight decrease in immunization coverage from 2010 to 2017 and a slight increase in 2018 and 2019 [21]. Additionally, a scorecard on progress for immunization elimination in fifteen African countries found a slight increase in MCV-1 coverage from 2001 to 2009 in most African countries for this study. However, there was a decline by 2015, followed by an increase in 2017, before declining again. However, Sierra Leone experienced a rise in measles immunization coverage over the years; recent studies on measles immunization in Sierra Leone have shown similar trends, indicating improvements in immunization efforts and highlighting challenges in maintaining high coverage rates [22–25]. Possible reasons for the observed trends include enhanced efforts by the government and international organizations, implementation of immunization campaigns, improvements in healthcare infrastructure, and increased public awareness about the importance of measles vaccination. For instance, introducing the Measles and Rubella Initiative and intensifying the Expanded Programme on Immunization services likely contributed to the increased coverage observed in the earlier years of the study period.
Additionally, the study found a decrease in maternal age-related inequalities in measles immunization coverage between 2008 and 2019. This suggests that efforts to reach children of mothers of younger age groups may have been successful. Comparisons with previous studies in other African countries indicate similar patterns of reduced age-related disparities despite the difference in the study length. The mother’s age was shown to be strongly correlated with vaccination status in a study carried out in the Eastern Province of Zambia [26]. The study evaluated characteristics associated with measles-rubella vaccination among children aged 9-179 months following a statewide immunization programme post-2016. Interestingly, children born to mothers younger than 30 or older than 49 were less likely to be vaccinated than those born to mothers between 30 and 39. Younger children were also more likely to have had the measles-rubella immunization than older children within the target age range [26]. Possible reasons for these improvements in Sierra Leone include targeted immunization campaigns and policies prioritizing children of younger mothers. The successful reduction in maternal age-related disparities could also be linked to community health worker programs targeting children of younger mothers for vaccination, ensuring they receive the necessary immunizations on time. Additionally, public health education campaigns might have played a role in increasing awareness among parents about the importance of early childhood immunizations. This finding highlights the effectiveness of focused strategies in improving health outcomes and suggests that ongoing efforts are necessary to maintain and build upon these successes.
Findings on inequalities based on education and economic status showed reduced disparities between 2008 and 2019. A study conducted between 2000 and 2014 on trends in socioeconomic disparities in Vietnamese children aged 12 to 23 months who received full vaccination coverage, evidence for reducing vaccination-related inequality shows that the full vaccination coverage concentration index dropped during the period, indicating a gradual decline in socioeconomic disparities [27]. Again, there was a decrease in vaccination coverage between children from wealthy and low-income families as the concentration curve approached the equality line [27]. According to the study, children from wealthier homes and mothers with better educational attainment had higher chances of receiving all recommended vaccinations. Full vaccination coverage was far more likely in children whose mothers had completed upper secondary and university education and belonged to higher socioeconomic groups. The general level of socioeconomic inequality decreased, but discrepancies persisted. Similar findings were also observed in findings written in a book on child immunization by WHO [28]. Compared to their peers, children from ethnic minority groups, those living in rural regions, and those whose mothers had only completed elementary school or less had lower full immunization rates [27]. Additionally, a study on unequal immunization rates against measles in the WHO’s “big six” nations in the Southeast Asian region revealed that except Thailand, there were notable socioeconomic differences in every country concerning maternal education levels, wealth quintiles, antenatal care use, and nutritional status [29]. Wealth-related inequalities are prevalent in measles immunization coverage. Across low- and middle-income countries, children from wealthier households consistently have higher immunization coverage than those from poorer households [28]. This trend is observed in various countries, including Nigeria and Pakistan, where coverage among the richest quintile is notably higher than among the poorest [29]. Possible reasons for these reductions in Sierra Leone include government policies aimed at increasing access to education and economic development and targeted interventions by partner organizations to address these disparities. Initiatives such as school-based vaccination campaigns might have contributed to reducing economic and educational barriers to immunization. Additionally, improvements in healthcare access and quality in underserved areas could have played a crucial role in narrowing these gaps. Future research should explore the long-term sustainability of these interventions and their effectiveness in maintaining high vaccination rates across different socioeconomic groups.
Our study findings indicated an increase in sex-related inequalities in measles immunization coverage. According to the study titled “Inequalities in full immunization coverage: trends in low- and middle-income countries,” some countries exhibit slight disparities favoring boys in immunization coverage, while most do not show significant differences between boys and girls [29]. This suggests that female children were increasingly less likely to be immunized than their male counterparts. Countries such as Azerbaijan, Belize, India, Mali, and Somalia have highlighted similar sex-related disparities, though in many instances, these variations are typically negligible and not statistically significant [29]. However, research on sex and gender differences in immunization coverage among children under two years old has found notable differences in immune responses, with a higher number of females observed to have better responses compared to males [30]. In Sierra Leone, several factors may contribute to these inequalities. Cultural preferences and biases often lead to differential access to healthcare based on the child’s sex. In some communities, male children are prioritized for healthcare services, including immunization, due to entrenched cultural norms and gender biases. For instance, studies from Nigeria [31] and Tanzania [32] have documented similar trends, indicating that families may allocate resources preferentially to male children, reflecting societal beliefs about gender roles and future economic contributions. Moreover, the increasing sex-related disparities in immunization coverage may be exacerbated by systemic barriers that limit access to healthcare for female children. These barriers can include logistical challenges in reaching healthcare facilities, societal attitudes that undervalue female health, and insufficient gender-sensitive policies that address the unique needs of girls in healthcare systems. To address these disparities, there is a pressing need for gender-sensitive interventions and policies that ensure equal access to immunization services for both male and female children. Future studies should investigate the underlying cultural factors contributing to these disparities, as well as assess the impact of gender-focused interventions in improving immunization coverage. By understanding these dynamics, public health initiatives can be better tailored to promote equity in immunization services.
Our findings revealed that significant provincial disparities persist. Notably, the Northern province exhibited the highest immunization coverage, whereas the newly formed Northwestern province reported the lowest. The challenges faced by the Northwestern province may be multifaceted and contribute to these lower vaccination rates. Key factors include potential disruptions in healthcare infrastructure, which can hinder the delivery of immunization services [33]. For instance, areas with limited healthcare facilities may struggle to provide consistent vaccine access, leading to gaps in coverage [34]. Additionally, logistical challenges, such as inadequate transportation networks, can impede the ability of families to reach vaccination sites, particularly in rural areas where distances are greater. Moreover, insufficient outreach efforts in the Northwestern province may further exacerbate these disparities. Community awareness campaigns are crucial for informing families about the importance of immunization and available services. In contrast, urban areas often benefit from better healthcare infrastructure and more effective outreach programs, resulting in higher vaccination rates. For instance, countries like Ethiopia show a substantial difference, with urban areas having significantly higher coverage than rural areas [28, 29]. To address these geographical inequalities, targeted interventions are essential. Strengthening healthcare infrastructure in underserved provinces, improving transportation and logistics for vaccine delivery, and implementing community-based outreach programs could significantly enhance access to immunization services. Future research should focus on evaluating the effectiveness of these interventions and understanding the specific barriers faced by communities in the Northwestern province, ensuring that all children have equitable access to vaccinations.
Policy and practice implications
Our study on measles immunization coverage in Sierra Leone highlights several areas for policy and practice improvements. The decrease in provincial inequality suggests policy changes targeting these areas can have a substantial impact. Policies could include allocating resources to provinces with lower coverage, improving vaccine access through mobile clinics, and partnering with local communities to address vaccine hesitancy. The increasing gender disparity requires an investigation into the reasons behind it. This could involve studies to understand socio-cultural factors or access barriers for boys. Based on the findings, policies can target mothers of boys through targeted communication campaigns or ensuring healthcare worker availability preferred by men. The study shows progress in reducing inequalities based on socioeconomic status, education, and place of residence. Policies such as financial assistance programs or community outreach in disadvantaged areas should ensure these successful strategies continue. The study emphasizes the importance of integrating equity lens into all aspects of immunization programs. This could involve setting clear targets to reduce disparities, allocating resources based on need, and monitoring progress towards achieving equitable coverage. Regularly monitoring coverage rates and identifying areas with declining rates or persistent inequalities could help address some of these challenges. This allows for timely adjustments to policies and interventions. The government should partner with community leaders, healthcare workers, and local NGOs to address vaccine hesitancy and raise awareness about the importance of measles immunization. By implementing these policy and practice changes, Sierra Leone can improve measles immunization coverage, ensure equitable access for all children, and prevent outbreaks of this dangerous disease.
Strengths and limitations
There are some strengths of the study that need to be acknowledged. First, the DHS data covers a large sample size and provides information representative of the entire country, allowing for generalizable findings. Again, the DHS collects data using consistent methods across countries and over time, facilitating comparisons within Sierra Leone and potentially with other countries. Also, DHS includes information on socioeconomic status, education level, place of residence, and child’s sex, all relevant factors for analyzing inequalities in immunization coverage. Moreover, HEAT offers tools for analyzing complex datasets like DHS, allowing you to calculate proportions, assess trends, and estimate the contribution of different factors to inequalities. In terms of limitations, some information in DHS relies on self-reporting, which can be prone to errors due to recall or social desirability bias. Again, while DHS covers relevant factors, it does not capture all potential reasons for vaccine hesitancy or missed vaccinations. Finally, the DHS uses a cross-sectional study design, limiting the ability to establish causal relationships between factors and immunization coverage.
Conclusion
There was a positive trend in national measles immunization coverage for children under two. Despite the progress, coverage dropped slightly in 2019. Inequalities in access to immunization based on age, socioeconomic status, education level, and place of residence decreased between 2008 and 2019. Provincial inequality remains a significant challenge, with a decrease but still a substantial gap in 2019. Disparities based on the child’s sex increased during the study period. Continued efforts are needed to ensure consistent progress in national coverage rates and prevent further decline. Addressing the provincial disparities by focusing resources and outreach programs on areas with lower coverage could be useful. Again, investigating the reasons behind the increasing gender gap and developing strategies to improve immunization rates among boys should be given attention. There is also the need to integrate considerations of socioeconomic status, education level, and place of residence into program design and implementation to reduce inequalities further. Regularly monitoring coverage rates and inequalities to identify areas needing improvement and assessing the effectiveness of interventions should be a priority of governmental and non-governmental organizations.
Acknowledgements
We are grateful to MEASURE DHS and the World Health Organization for making the dataset and the HEAT software accessible.
Author contributions
AO and BOA contributed to the study design and conceptualisation. AO and BOA performed the analysis. AO, AUBS, US, AT, CB, and BOA developed the initial draft. All the authors critically reviewed the manuscript for its intellectual content. All authors read and amended drafts of the paper and approved the final version. AO had the final responsibility of submitting it for publication.
Funding
This study received no funding.
Data availability
The dataset used can be accessed at https://whoequity.shinyapps.io/heat/.
Declarations
Ethics approval and consent to participate
This study did not seek ethical clearance since the WHO HEAT software and the dataset are freely available in the public domain.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Clinical trial number
Not applicable.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.WHO, Measles. https://www.who.int/news-room/fact-sheets/detail/measles. 2024. Accessed 13 July 2024.
- 2.CDC US. Measles symptoms and complications | Measles (Rubeola) | CDC. https://www.cdc.gov/measles/signs-symptoms/index.html. 2024. Accessed 13 July 2024.
- 3.Bester JC. Measles and measles vaccination: a review. JAMA Pediatr. 2016;170(12):1209–1215. 10.1001/jamapediatrics.2016.1787. PMID: 27695849. [DOI] [PubMed]
- 4.Plans-Rubió P. Vaccination coverage for routine vaccines and herd immunity levels against measles and pertussis in the world in 2019. Vaccines (Basel). 2021;9(3):256. 10.3390/vaccines9030256. PMID: 33805681; PMCID: PMC7999208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fu H, Abbas K, Klepac P, et al. Effect of evidence updates on key determinants of measles vaccination impact: a DynaMICE modelling study in ten high-burden countries. BMC Med. 2021;19:281. 10.1186/s12916-021-02157-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bester JC. Measles vaccination is best for children: the argument for relying on herd immunity fails. J Bioeth Inq. 2017;14(3):375–84. 10.1007/s11673-017-9799-4. Epub 2017 Aug 16. PMID: 28815434. [DOI] [PubMed] [Google Scholar]
- 7.Cutts FT, Ferrari MJ, Krause LK, et al. Vaccination strategies for measles control and elimination: time to strengthen local initiatives. BMC Med. 2021;19:2. 10.1186/s12916-020-01843-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Robert A, Kucharski AJ, Funk S. The impact of local vaccine coverage and recent incidence on measles transmission in France between 2009 and 2018. BMC Med. 2022;20:77. 10.1186/s12916-022-02277-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sudfeld CR, Navar AM, Halsey NA. Effectiveness of measles vaccination and vitamin A treatment. Int J Epidemiol. 2010;39(1):i48–55. 10.1093/ije/dyq021. PMID: 20348126; PMCID: PMC2845860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Minta AA, Ferrari M, Antoni S, et al. Progress toward measles elimination — worldwide, 2000–2022. MMWR Morb Mortal Wkly Rep. 2023;72:1262–8. 10.15585/mmwr.mm7246a311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.CDC US. Measles (Rubeola). Questions About Measles. https://www.cdc.gov/measles/about/questions.html. 2024. Accessed 13 July 2024.
- 12.CDC US. Global measles vaccination. Fast Facts: Global Measles. https://www.cdc.gov/global-measles-vaccination/data-research/index.html. 2024. Accessed 13 July 2024.
- 13.Wang R, Jing W, Liu M, Liu J. Trends of the global, regional, and national incidence of measles, vaccine coverage, and risk factors in 204 countries from 1990 to 2019. Front Med (Lausanne). 2022;8:798031. 10.3389/fmed.2021.798031. PMID: 35127753; PMCID: PMC8810814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jalloh MF, Sengeh P, Ibrahim N, Kulkarni S, Sesay T, Eboh V, Jalloh MB, Abu Pratt S, Webber N, Thomas H, Kaiser R, Singh T, Prybylski D, Omer SB, Brewer NT, Wallace AS. Association of community engagement with vaccination confidence and uptake: a cross-sectional survey in Sierra Leone, 2019. J Glob Health. 2022;12:04006. 10.7189/jogh.12.04006. PMID: 35265325; PMCID: PMC8876869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wassenaar M, Fombah AE, Chen H, et al. Immunisation coverage and factors associated with incomplete immunisation in children under two during the COVID-19 pandemic in Sierra Leone. BMC Public Health. 2024;24:143. 10.1186/s12889-023-17534-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Statistics Sierra Leone - StatsSL, ICF. Sierra Leone Demographic and Health Survey 2019. StatsSL/ICF. 2020. https://dhsprogram.com/pubs/pdf/FR365/FR365.pdf. Accessed 13 July 2024.
- 17.Health Equity Assessment Toolkit (HEAT). Software for exploring and comparing health inequalities in countries. In: Built-in database edition. Version 6.0. Geneva: World Health Organization. 2024. https://www.who.int/data/inequality-monitor/assessment_toolkit. Accessed 5 July 2024.
- 18.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, STROBE Initiative. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495–9. Epub 2014 Jul 18. PMID: 25046131. [DOI] [PubMed] [Google Scholar]
- 19.WHO. Handbook on health inequality monitoring with a special focus on low and middle-income countries. Geneva World Health Organization 2013. https://www.who.int/docs/default-source/gho-documents/health-equity/handbook-on-health-inequality-monitoring/handbook-on-health-inequality-monitoring.pdf. Accessed 13 July 2024.
- 20.Hosseinpoor AR, Nambiar D, Schlotheuber A, et al. Health Equity Assessment Toolkit (HEAT): software for exploring and comparing health inequalities in countries. BMC Med Res Methodol. 2016;16:141. 10.1186/s12874-016-0229-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jean Baptiste AE, Masresha B, Wagai J, Luce R, Oteri J, Dieng B, Bawa S, Ikeonu OC, Chukwuji M, Braka F, Sanders EAM, Hahné S, Hak E. Trends in measles incidence and measles vaccination coverage in Nigeria, 2008–2018. Vaccine. 2021;39(Suppl 3):C89–95. 10.1016/j.vaccine.2021.03.095. Epub 2021 Apr 17. PMID: 33875267. [DOI] [PubMed] [Google Scholar]
- 22.Wariri O, Nkereuwem E, Erondu NA, Edem B, Nkereuwem OO, Idoko OT, Agogo E, Enegela JE, Sesay T, Conde IS, Kaucley L, Awuah AA, Abdullahi S, Luce RR Jr, Banda R, Nomhwange T, Kampmann B. A scorecard of progress towards measles elimination in 15 west African countries, 2001-19: a retrospective, multicountry analysis of national immunisation coverage and surveillance data. Lancet Glob Health. 2021;9(3):e280–90. 10.1016/S2214-109X(20)30481-2. PMID: 33607028; PMCID: PMC7900524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sesay FF, Hodges MH, Kamara HI, Turay M, Wolfe A, Samba TT, Koroma AS, Kamara W, Fall A, Mitula P, Conteh I, Maksha N, Jambai A. High coverage of vitamin A supplementation and measles vaccination during an integrated maternal and child health week in Sierra Leone. Int Health. 2015;7(1):26–31. 10.1093/inthealth/ihu073. Epub 2014 Oct 14. PMID: 25316706. [DOI] [PubMed]
- 24.Masresha BG, Luce R Jr, Weldegebriel G, Katsande R, Gasasira A, Mihigo R. The impact of a prolonged Ebola outbreak on measles elimination activities in Guinea, Liberia and Sierra Leone, 2014–2015. Pan Afr Med J. 2020;35(Suppl 1):8. 10.11604/pamj.supp.2020.35.1.19059. PMID: 32373259; PMCID: PMC7196330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sesay U, Serna-Chavez HM, Gebru GN, et al. Assessing the impact of COVID-19 on routine immunization in Sierra Leone. BMC Public Health. 2024;24:1795. 10.1186/s12889-024-19221-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Carcelen AC, Mutembo S, Matakala KH, Chilumba I, Mulundu G, Monze M, Mwansa FD, Moss WJ, Hayford K. Impact of a measles and rubella vaccination campaign on seroprevalence in Southern Province, Zambia. Am J Trop Med Hyg. 2021;104(6):2229–32. 10.4269/ajtmh.20-1669. PMID: 33939639; PMCID: PMC8176503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vo HL, Huynh LT, Anh HNS, Do DA, Doan TN, Nguyen TH, Nguyen Van H. Trends in socioeconomic inequalities in full vaccination coverage among Vietnamese children aged 12–23 months, 2000–2014: evidence for mitigating disparities in vaccination. Vaccines (Basel). 2019;7(4):188. 10.3390/vaccines7040188. PMID: 31752228; PMCID: PMC6963749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.World Health Organization. State of inequality: childhood immunisation. https://iris.who.int/handle/10665/252541. 2024. Accessed 13 July 2024.
- 29.Restrepo-Méndez MC, Barros AJ, Wong KL, Johnson HL, Pariyo G, França GV, Wehrmeister FC, Victora CG. Inequalities in full immunization coverage: trends in low- and middle-income countries. Bull World Health Organ. 2016;94(11):794–805. 10.2471/BLT.15.162172. Epub 2016 Aug 31. PMID: 27821882; PMCID: PMC5096343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Flanagan KL, Fink AL, Plebanski M, Klein SL. Sex and gender differences in the outcomes of vaccination over the life course. Annu Rev Cell Dev Biol. 2017;33:577–599. 10.1146/annurev-cellbio-100616-060718. PMID: 28992436. [DOI] [PubMed]
- 31.Milazzo A. Son preference, fertility and family structure: evidence from reproductive behavior among Nigerian women. Policy Research Working Paper; No. 6869. © World Bank, Washington, DC. 2014. http://hdl.handle.net/10986/18805
- 32.Hassan A, Schaffnit SB, Sear R, Urassa M, Lawson DW. Fathers favour sons, mothers don’t discriminate: sex-biased parental care in northwestern Tanzania. Evol Hum Sci. 2019;1:e13. 10.1017/ehs.2019.14. PMID: 37588395; PMCID: PMC10427269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Causey K, Fullman N, Sorensen RJD, Galles NC, Zheng P, Aravkin A, Danovaro-Holliday MC, Martinez-Piedra R, Sodha SV, Velandia-González MP, Gacic-Dobo M, Castro E, He J, Schipp M, Deen A, Hay SI, Lim SS, Mosser JF. Estimating global and regional disruptions to routine childhood vaccine coverage during the COVID-19 pandemic in 2020: a modelling study. Lancet. 2021;398(10299):522–34. 10.1016/S0140-6736(21)01337-4. Epub 2021 Jul 17. PMID: 34273292; PMCID: PMC8285122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hardt K, Bonanni P, King S, Santos JI, El-Hodhod M, Zimet GD, Preiss S. Vaccine strategies: optimising outcomes. Vaccine. 2016;34(52):6691–9. 10.1016/j.vaccine.2016.10.078. Epub 2016 Nov 23. PMID: 27887796. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset used can be accessed at https://whoequity.shinyapps.io/heat/.