Abstract
Purpose: To describe a unique finding in ocular syphilis using multimodal imaging. Methods: A single case was analyzed. Results: A 52-year-old man presented with chronic syphilitic posterior uveitis and was treated with intravenous and intramuscular penicillin for systemic manifestations, topical steroids, and unilateral bevacizumab for secondary macular neovascularization. Bilateral transitory outer retinal microcysts were subsequently seen on optical coherence tomography, with an appearance distinct from outer retinal lesions found in other degenerative retinal diseases. Conclusions: Longstanding smoldering inflammation in this patient resulted in retinal pigment epithelial disruption and subsequent overlying photoreceptor rearrangement with microcyst formation. The spontaneous resolution and reappearance of these lesions elsewhere, despite previous treatment, may offer further insight into localized retinal tissue response from treponemal disease.
Keywords: ocular syphilis, uveitis, macular neovascularization (MNV), optical coherence tomography (OCT), fundus autofluorescence
Introduction
A well-documented masquerade syndrome, ocular syphilis can present as chorioretinitis, necrotizing retinitis, retinal vasculitis, neuroretinitis, retinal artery and vein occlusion, exudative retinal detachments, or otherwise. 1 We report a case of syphilitic posterior uveitis, secondary inflammatory macular neovascularization (MNV) formation, and transitory microcystic outer retinal lesions that appeared after the completion of systemic antibiotic therapy.
Case Report
A 52-year-old man presented with 1 to 2 years of gradual blurring and dimming of vision in the left eye that had acutely worsened in the previous 3 months. He also had intermittent tinnitus in the left ear, rare numbness of the left-sided upper extremity, migratory rashes, and remote painful oral ulcers. The patient’s visual acuity (VA) was 20/25 OD and 20/80 OS. The funduscopic examination showed bilateral low-grade posterior vitreous cells, subtle disc edema, mottling of the retinal pigment epithelium (RPE), and a macular hemorrhage in the left eye. Optical coherence tomography (OCT) showed an epiretinal membrane, subretinal hyperreflective material and subretinal fluid with increased overlying retinal thickness consistent with active MNV in the left eye, and areas of extrafoveal ellipsoid attenuation (Figure 1). Fluorescein angiography (FA) was significant for mild late disc leakage, leakage from an MNV complex in the left eye, peripheral vascular sheathing, and window defects.
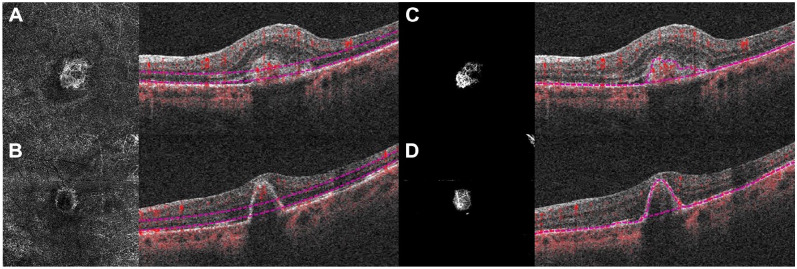
Figure 1.
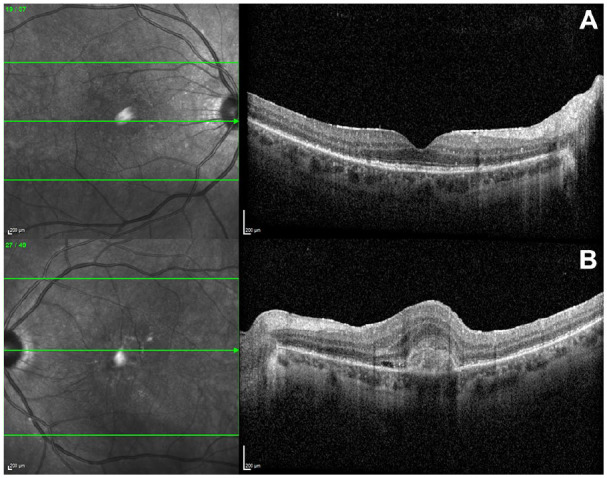
Initial foveal optical coherence tomography scans. (A) The right eye has scant vitreous cells, a trace epiretinal membrane (ERM), outer retinal/retinal pigment epithelium (RPE) atrophy, and no intraretinal fluid. (B) The left eye has scant vitreous cells, an ERM, outer retinal/RPE atrophy, macular neovascularization complex with subretinal hyperreflective material, subretinal fluid, and overlying increased retinal thickening.
The laboratory workup returned a highly positive rapid plasmid reagin titer (1:128) and reactive Treponema pallidum antibody consistent with syphilitic posterior uveitis. The patient was admitted for cerebrospinal fluid studies, which were negative, and ultimately received a 2-week course of daily intravenous penicillin.
After being discharged, he was followed closely on an outpatient basis by ophthalmology and infectious diseases. Two weeks after treatment with penicillin, the patient began monthly intravitreal antivascular endothelial growth factor (anti-VEGF) injections, initially with 2 doses of ranibizumab and thereafter with bevacizumab. At the 4-week timepoint, the patient received a single dose of intramuscular penicillin. Clinically evident intraocular inflammation resolved within 2 months, and the VA improved to 20/30+ OS. The MNV showed gradual improvement, with exudation eventually resolving in the setting of monthly bevacizumab (Figure 2).
Figure 2.
Optical coherence tomography angiography of the left eye shows a subretinal vascularized complex. (A) En face and transverse raster scans highlight the outer retina to choriocapillaris slab and (B) the retinal pigment epithelium (RPE)–RPE fit slab 1 day after administration of intravenous penicillin. (C) En face and transverse raster scans highlight the outer retina to choriocapillaris slab and (D) the RPE–RPE fit slab 29 weeks after administration of intravenous penicillin. Segmentation incorporates (B) the macular neovascularization complex with regression of the vascular network, leaving (D) residual pigment epithelial detachment and fibrosis without flow.
However, 2 to 3 months after the initiation of penicillin and the patient’s first anti-VEGF injection, the onset of transitory cystic outer retinal lesions that regressed and reappeared in new areas was seen in both eyes (Figure 3). An increased signal transmission suggestive of RPE disruption was noted in the choroid underlying these lesions, each of which had relative improvement in residual atrophy by monthly follow-up (Figure 4). No chorioretinal, vascular, or disc leakage suggestive of ongoing inflammation was seen at 7 months on repeat FA and indocyanine green angiography.
Figure 3.
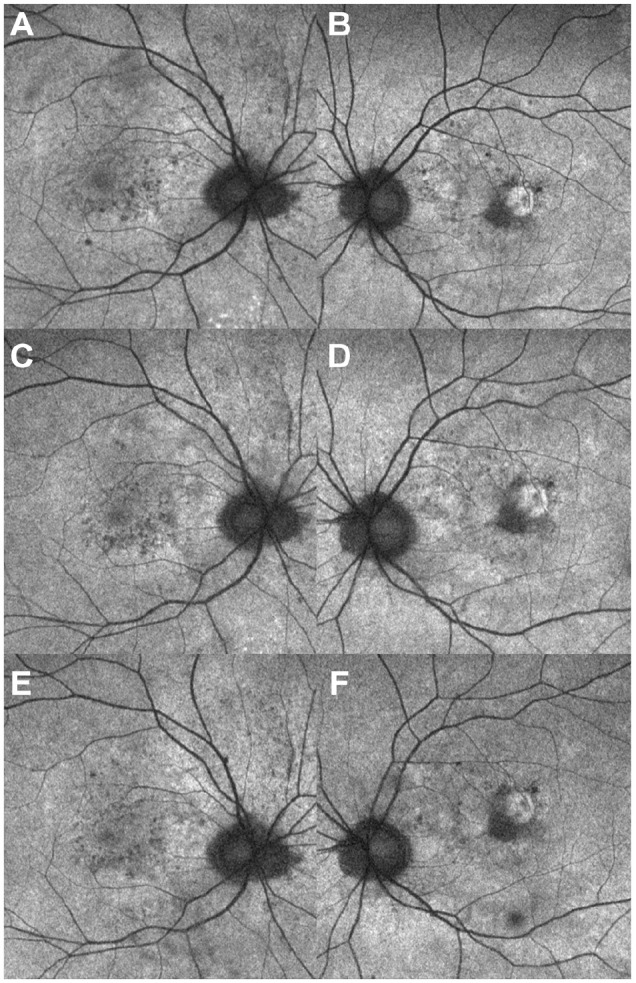
Serial fundus autofluorescence of both eyes shows transient, percolating areas of hyperautofluorescence and hypoautofluorescence in the macula (A and B) 13 weeks, (C and D) 18 weeks, and (E and F) 23 weeks after administration of intravenous penicillin.
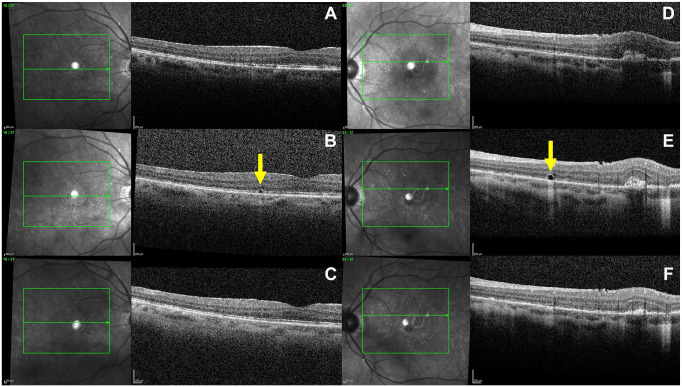
Figure 4.
Serial registered optical coherence tomography rasters of the right eye (A) 23 weeks, (B) 29 weeks, and (C) 36 weeks after administration of intravenous penicillin. Left eye (D) 2 weeks, (E) 5 weeks, and (F) 9 weeks after administration of intravenous penicillin. Photographs show both regression of the macular neovascularization (MNV) complex in the left eye and the spontaneous appearance and disappearance of an outer retinal microcyst in each eye (arrows). Note the increased transmission into the choroid in the area of the microcyst, similar to the areas of retinal pigment epithelial atrophy adjacent to the MNV complex temporally.
Conclusions
In this case, secondary MNV arose theoretically in the setting of disruption of Bruch membrane by treponemal disease or inflammation-mediated angiogenic factors. Inflammatory MNV, while rare in the setting of ocular syphilis, has been reported both at initial presentation and in a delayed fashion.2,3 Specifically, type 2 subretinal neovascular membranes were seen, as is typical with both infectious uveitis and noninfectious uveitis. 4 Anecdotally, syphilitic MNV responds well to a combination of intravenous penicillin and oral corticosteroids. 5 We also believe that this patient’s syphilis was adequately treated given his adherence to standard of care, declining titers, and otherwise systemically unremarkable findings. To our knowledge, the transitory microcysts of the outer retina have not been previously reported in the setting of syphilitic posterior uveitis after treatment. Although components of the patient’s history and the appearance of the microcysts en face or on OCT are reminiscent of other retinal conditions (particularly “comet” lesions and outer retinal tubulations), there are distinct differences.
As early as 2003, comet lesions were described as a unique feature of pseudoxanthoma elasticum. The small, round, whitish areas of hyperfluorescent RPE atrophy, often with tapered tails oriented toward the optic disc, may present alongside peau d’orange fundus mottling before angioid streaks develop, 6 hence conferring significant diagnostic value early in the disease course. 7 The first depictions of such lesions on OCT described “irregular hyporeflective spaces with hyperreflective inner border and focal debris-like deposits above the RPE” with occasional coalescence and variable chorioretinal extension from the RPE–Bruch complex, surrounding a sparing of retinal layers, and a transmission effect. The lesions’ characteristics and the timing of their appearance led the authors to postulate their role as a sign of disease chronicity, perhaps secondary to calcification of Bruch membrane with subsequent chorioretinal degeneration. 8
The largest series to date of peripapillary comet lesions in patients with pseudoxanthoma elasticum described heterogenous lesions ranging from punctate hyperreflective areas at the level of the outer retinal segment and RPE–Bruch complex to larger ovoid structures with hyperreflective borders in the outer nuclear level. 9 Despite important differences, mechanistic parallels were drawn to less specific outer retinal tubulations, usually characterized on OCT as ovoid hyporeflective spaces with hyperreflective borders in the outer nuclear layer. These tubulations are known to arise in the setting of retinal injury (in particular in neovascular age-related macular degeneration and other chronic degenerative disorders), causing loss of photoreceptor tight junctions, outward folding of photoreceptors, and formation of new lateral connections by direct contact of opposite aspects of the fold. 10 It was further speculated that a similar process was occurring in comet lesions by which outer retinal hyperreflective bands had invaginated on a focal disruption of the RPE–Bruch complex to form a cystic cavity in an attempt to preserve photoreceptors. 9
In 2018, Battaglia Parodi et al 11 presented a case of retinitis pigmentosa with white, hyperautofluorescent subretinal bodies along the vascular arcades. OCT showed corresponding hyporeflective spaces distinct from the RPE enclosed entirely by an irregular hyperreflective lining, which the authors theorized arose from the oxidative and related accumulation of calcific and proteinaceous material at the underlying Bruch membrane. The idea that multiple conditions involving RPE disruption can produce variable but similar cystic lesions lends credence to a similar process occurring in our patient’s case.
Furthermore, in 2016 Sridhar et al 12 presented findings of hyperreflective outer retinal dots in a case of active syphilitic chorioretinitis that could also exist on a similar spectrum, albeit without a cystic component or MNV, and that resolved within 1 week of treatment. Here, we postulate that particularly longstanding smoldering inflammation and an initially high burden of disease led to the persistent disruption of the RPE–Bruch complex, even after treatment. This in turn resulted in the formation of not only transitory punctate hyperreflective spots but also more uniquely appearing underlying microcysts on OCT, possibly as a result of a rearrangement process not unlike that involved in the formation of outer retinal tubulations but resulting in a distinct, smaller lesion. Again, it is notable that such lesions appeared in both eyes while only a single eye was observed with and treated for MNV.
Our findings may have constituted a late, localized Jarish-Herxheimer–like reaction occurring 2 to 3 months after administration of antibiotics. In 2003, Fathilah and Choo 13 described a case of rapid-onset visual decline hours after administration of penicillin. More recently, Forouzan et al 14 recounted a case of presumed ocular syphilis with worsening optic nerve edema, new-onset macular edema, and deteriorating vision a few days into the treatment course, without more typical systemic symptoms (ie, fever, hypotension, tachycardia, or hyperventilation). Last, Abd Manan et al 15 reported a patient with neuroretinitis whose increasing macular edema contributed to worsening vision 2 days after oral doxycycline was initiated, again without systemic symptoms, with syphilis infection confirmed on subsequent cultures. Our case is distinct from those cases in the onset, duration, and symptomatology in that they occurred during or quite soon after treatment, then quickly improved with the administration of systemic steroids.
This case highlights a unique imaging finding of transitory outer retinal microcysts in the context of syphilitic posterior uveitis with inflammatory MNV. The presumed underlying etiology involving RPE disruption and resulting cystic appearance evoke pathophysiologic aspects of comet lesions and outer retinal tubulations. However, the smaller size, resolution, and migratory reappearance of these microcysts may offer insight into the effect of longstanding low-grade inflammation at the RPE and the resulting photoreceptor rearrangement and spontaneous recovery, the clinical significance of which is not yet entirely known.
Footnotes
Ethical Approval: Institutional review board approval was not required because this was a single retrospective case report that does not meet the definition of research.
Statement of Informed Consent: Consent was obtained from the patient for clinical care. No identifiable features, images, or clinical information were used in this manuscript; thus, consent was not required.
Dr. Papakostas is on the advisory board of Alimera Sciences, Roche, EyePoint, and Pharmaceuticals. Dr. Kovacs is a consultant to Intergalactic Therapeutics. Neither of the other authors declared potential conflicts of interest with respect to the research, authorship, and/or publication of the article.
Funding: Support was provided via an unrestricted departmental grant from Research to Prevent Blindness.
Authorship: All authors attest that they meet the current ICMJE criteria for authorship.
ORCID iDs: James P. Winebrake  https://orcid.org/0000-0001-9158-6438
https://orcid.org/0000-0001-9158-6438
Kyle D. Kovacs  https://orcid.org/0000-0001-7568-6703
https://orcid.org/0000-0001-7568-6703
References
- 1. Furtado JM, Simões M, Vasconcelos-Santos D, et al. Ocular syphilis. Surv Ophthalmol. 2022;67(2):440-462. doi: 10.1016/j.survophthal.2021.06.003 [DOI] [PubMed] [Google Scholar]
- 2. Halperin LS, Lewis H, Blumenkranz MS, Gass JD, Olk RJ, Fine SL. Choroidal neovascular membrane and other chorioretinal complications of acquired syphilis. Am J Ophthalmol. 1989;108(5):554-562. doi: 10.1016/0002-9394(89)90433-9 [DOI] [PubMed] [Google Scholar]
- 3. Balaskas K, Spencer S, D’Souza Y. Peripapillary choroidal neovascularisation in the context of ocular syphilis is sensitive to combination antibiotic and corticosteroid treatment. Int Ophthalmol. 2013;33(2):159-162. doi: 10.1007/s10792-012-9641-2 [DOI] [PubMed] [Google Scholar]
- 4. Agarwal A, Invernizzi A, Singh RB, et al. An update on inflammatory choroidal neovascularization: epidemiology, multimodal imaging, and management. J Ophthalmic Inflamm Infect. 2018;8(1):13. Published online September 12, 2018. doi: 10.1186/s12348-018-0155-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Giuffrè C, Marchese A, Cicinelli MV, et al. Multimodal imaging and treatment of syphilitic choroidal neovascularization. Retin Cases Brief Rep. 2022;16(1):85-88. doi: 10.1097/ICB.0000000000000912 [DOI] [PubMed] [Google Scholar]
- 6. Gass JD. “Comet” lesion: an ocular sign of pseudoxanthoma elasticum. Retina. 2003;23(5):729-730. doi: 10.1097/00006982-200310000-00029 [DOI] [PubMed] [Google Scholar]
- 7. Gliem M, Zaeytijd JD, Finger RP, Holz FG, Leroy BP, Charbel Issa P. An update on the ocular phenotype in patients with pseudoxanthoma elasticum. Front Genet. 2013;4:14. Published online April 4, 2013. doi: 10.3389/fgene.2013.00014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Barteselli G, Viola F. Comet lesions in pseudoxanthoma elasticum: a spectral domain optical coherence tomography analysis. Retina. 2015;35(5):1051-1053. doi: 10.1097/IAE.0000000000000396 [DOI] [PubMed] [Google Scholar]
- 9. Murro V, Mucciolo DP, Sodi A, et al. Peripapillary comet lesions and comet rain in PXE-related retinopathy. Graefes Arch Clin Exp Ophthalmol. 2018;256(9):1605-1614. doi: 10.1007/s00417-018-4037-2 [DOI] [PubMed] [Google Scholar]
- 10. Zweifel SA, Engelbert M, Laud K, Margolis R, Spaide RF, Freund KB. Outer retinal tubulation: a novel optical coherence tomography finding [published correction appears in Arch Ophthalmol. 2012 Jul 1;130(7):856]. Arch Ophthalmol. 2009;127(12):1596-1602. doi: 10.1001/archophthalmol.2009.326 [DOI] [PubMed] [Google Scholar]
- 11. Battaglia Parodi M, Romano F, Bandello F. Comet lesions in retinitis pigmentosa. Retina. 2018;38(7):e46-e47. doi: 10.1097/IAE.0000000000002119 [DOI] [PubMed] [Google Scholar]
- 12. Sridhar J, Shahlaee A, Sharma P. En face: disappearing outer retinal dots in treated syphilitic chorioretinitis. Ophthalmology. 2016;123(3):557. doi: 10.1016/j.ophtha.2016.01.001 [DOI] [PubMed] [Google Scholar]
- 13. Fathilah J, Choo MM. The Jarisch-Herxheimer reaction in ocular syphilis. Med J Malaysia. 2003;58(3):437-439. [PubMed] [Google Scholar]
- 14. Forouzan P, Fell D, Jones FR. Ocular syphilis as a cause of chronic postoperative uveitis followed by a localized ocular jarisch-herxheimer-like reaction. Ocul Immunol Inflamm. 2023;31(3):649-652. doi: 10.1080/09273948.2022.2042321 [DOI] [PubMed] [Google Scholar]
- 15. Abd Manan N, Musa AA, Lott PW, Zahari M, Tajunisah I. Ocular jarisch-herxheimer reaction in the treatment of ocular syphilis: a case report and review of the literature. Cureus. 2023;15(1):e33696. Published online January 12, 2023. doi: 10.7759/cureus.33696 [DOI] [PMC free article] [PubMed] [Google Scholar]