Abstract
The objective of this study was to evaluate the incidence of hypoglycemia in patients with diabetic kidney disease (DKD) undergoing maintenance hemodialysis (MHD) and to identify key factors influencing its occurrence. A comprehensive literature search was conducted across databases including CNKI, Wanfang data, VIP, SinoMed, PubMed, Cochrane Library, Web of Science and Embase from their inception to March 31, 2023. The search focused on studies addressing the incidence and influencing factors for hypoglycemia in DKD patients receiving hemodialysis. Eligible studies were selected based on predefined inclusion and exclusion criteria, and data were analyzed using Stata 15.0 software. A total of 24 studies involving 2388 patients were included in this meta-analysis, with 22 studies from China and 2 studies from English-speaking countries. The findings indicated that the incidence of hypoglycemia among hemodialysis patients with DKD was 41.7% (95% confidence interval (CI): 32.6% to 50.9%). Influencing factors associated with hypoglycemia in hemodialysis patients with DKD included age (odds ratio (OR) = 4.507, 95% CI: 3.272 to 6.209), course of DKD (OR = 3.547, 95% CI: 2.523 to 4.988), use of oral hypoglycemic drugs (OR = 4.643, 95% CI: 2.566 to 8.402), fasting plasma glucose (FPG) levels (risk ratio (RR) = 4.033, 95% CI: 2.594 to 6.269), insulin use (OR = 8.242, 95% CI: 4.517 to 15.042), application of glucose-free dialysate (RR = 7.987, 95% CI: 4.605 to 13.855), coefficient of variation in blood glucose (CVBG) (OR = 3.241, 95% CI: 2.071 to 5.071), mean blood glucose (MBG) (OR = 2.930, 95% CI: 1.635 to 5.248), medication compliance (OR = 4.300, 95% CI: 2.047 to 9.031) and self-care ability (OR = 3.543, 95% CI: 1.766 to 7.108). Specifically, risk factors identified were age > 60 years, DKD course > 1 year, use of oral hypoglycemic drugs, FPG < 6.1 mmol/L, insulin administration before dialysis, application of glucose-free dialysate, CVBG ≥ 0.26, MBG < 8.92 mmol/L, poor medication compliance, and poor self-care ability.
Keywords: DKD, hypoglycemic, hypoglycemia, influencing factors, meta-analysis
Introduction
Maintenance hemodialysis (MHD) is the primary modality of renal replacement therapy for patients with diabetic kidney disease (DKD) who progress to chronic renal failure in the uremic stage [1]. Patients with DKD undergoing MHD are at a higher risk of hypoglycemia compared to non-DKD patients due to several factors, including changes in hemodynamics, metabolic disorders, decreased renal clearance of insulin, glucose loss, malnutrition, and impaired gluconeogenesis [2,3]. Hypoglycemia during hemodialysis is associated with various complications, such as inadequate dialysis, irreversible damage to heart and brain cells, and increased incidence and mortality of cardiovascular diseases. Recurrent hypoglycemic episodes can also lower the threshold for the sympathetic adrenal response, thereby increasing the risk of progressive cognitive impairment in elderly patients [4,5]. Current studies on the incidence of hypoglycemia in DKD patients are mostly single-center with small sample sizes, leading to significant differences in incidence rates, ranging from 2.9% to 50.2% [6,7]. Furthermore, there remains a lack of consensus on the factors that influence the development of hypoglycemia in this patient population. Given the clinical importance of managing hypoglycemia in DKD patients on MHD, a comprehensive understanding of its incidence, mechanisms, and influencing factors is crucial. Therefore, we systematically evaluated the incidence and main influencing factors for hypoglycemia in DKD patients undergoing MHD, thereby providing robust evidence to inform effective hypoglycemia management strategies. This study was conducted following the PRISMA statement, and the research protocol was registered on the PROSPERO database (registration number: CRD42023429239).
Materials and methods
Literature retrieval strategy
A comprehensive literature search was performed using the following databases: CNKI, Wanfang Data, VIP, SinoMed, PubMed, the Cochrane Library, Web of Science, and Embase. The search encompassed both subject headings and free-text terms, aiming to identify relevant studies and to trace references for additional pertinent literature. The timeframe for the literature search extended from the establishment of each database to March 31, 2023. Keywords used in the search included “Diabetic Nephropathies”, “Diabetic Nephropathy”, “Diabetic Kidney Disease”, “Diabetic”, “Renal Dialysis”, “Renal Dialyses”, “Hemodialysis”, “Hemodialyses”, “Dialysis”, “Hypoglycemia”, “Glycopenia”, “Glucopenia”, “Low Blood Sugar”, and “Low Blood Glucose”. The detailed retrieval strategy is shown in Table 1.
Table 1.
PubMed retrieval strategy
| Step | Strategy |
|---|---|
| #1 | (Diabetic Nephropathies[MeSH Terms]) OR (Diabetic Nephropathy[Title/Abstract] OR Diabetic Kidney Disease*[Title/Abstract] OR Diabetic[Title/Abstract]) |
| #2 | (Renal Dialysis[MeSH Terms]) OR (Renal Dialyses[Title/Abstract] OR Hemodialysis[Title/Abstract] OR Hemodialyses[Title/Abstract] OR Dialysis[Title/Abstract]) |
| #3 | (Hypoglycemia[MeSH Terms]) OR (Glycopenia[Title/Abstract] OR Glucopenia[Title/Abstract] OR Low Blood Sugar[Title/Abstract] OR Low Blood Glucose[Title/Abstract]) |
| #4 | #1 AND #2 AND #3 |
Inclusion and exclusion criteria of literature
(1) Studies were included if they met the following criteria: ① studies involving DKD patients; ② research focused on the incidence and influencing factors of hypoglycemia during hemodialysis; ③ study designs including randomized controlled trials (RCTs), cohort studies, and case-control studies; ④ literature reporting the occurrence of hypoglycemia (defined as blood glucose ≤ 3.9 mmol/L measured by a blood glucose meter) and its influencing factors, allowing direct extraction or calculation of odds ratios (OR), risk ratios (RRs), and 95% confidence intervals (CI); ⑤ publications in Chinese or English.
(2) The following articles were excluded: ① studies calculating the incidence of hypoglycemia by example; ② studies with insufficient or erroneous data that preclude extraction; ③ duplicate publications; in such cases, only studies with large sample sizes and detailed data were retained; ④ studies for which the full text could not be obtained; ⑤ studies deemed to be of low quality after evaluation; ⑥ review, conference papers, expert comments, and case reports.
Literature screening, data extraction, and quality evaluation
The screening, data extraction, and quality evaluation were independently completed by two researchers (Feifei Jiang and Hang Xu). Discrepancies were resolved through discussion or by consulting a third researcher. Literature management was performed using NoteExpress software. Preliminary literature screening involved a review of titles and abstracts, followed by full-text reading to determine final inclusion. Data extraction included details such as the first author, publication year, country/region, research type, sample size, incidence of hypoglycemia, and influencing factor OR/RR values with corresponding 95% CIs. Another analyst subsequently verified the extracted data independently. The quality of RCTs was assessed using the Jadad evaluation scale [8], which evaluates the generation of random sequences, allocation concealment, blinding, and withdrawals/dropouts, with a score of less than 4 indicating low quality and a score of 4 or higher indicating high quality. For cohort and case-control studies, the Newcastle Ottawa Scale (NOS) [9] was employed, which assesses aspects such as population selection, inter-group comparability, and exposure or outcome measures. A score of ≤ 4 indicates low quality, 5-6 indicates moderate quality, and ≥ 7 indicates high quality.
Statistical analysis
The incidence of hypoglycemia in hemodialysis patients with DKD and the corresponding OR/RR values and 95% CI for influencing factors were analyzed using Stata15.0 software. Effect sizes were pooled using either a fixed-effects or random-effects model based on heterogeneity assessment. Heterogeneity among studies was evaluated using the chi-square (χ2) test (significance level α = 0.10) and the I2 statistic. An I2 value of < 50% and a P value of > 0.10 were considered indicative of moderate homogeneity, in which a fixed-effects model was used for the meta-analysis. Conversely, an I2 value of ≥ 50% or a P value of ≤ 0.10 indicated significant heterogeneity, prompting the use of a random-effects model. In the case of heterogeneity, subgroup analyses and sensitivity analyses were conducted to explore potential sources and assess the stability of the pooled incidence rates and influencing factors. Publication bias was evaluated using funnel plots, Egger’s tests, and Begg’s tests, with a significance level of α = 0.05.
Results
Literature search results
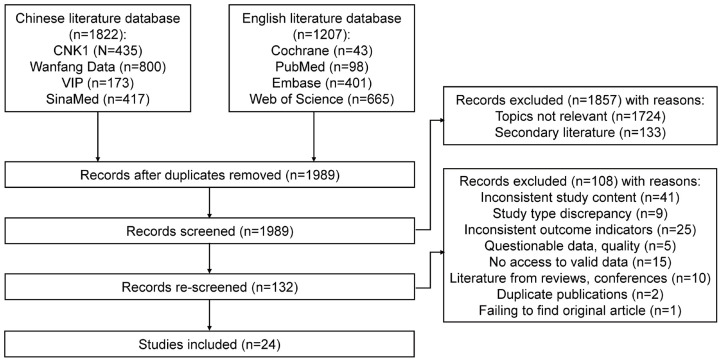
A total of 3029 articles were retrieved from 8 databases following the initial search. After removing duplicates using NoteExpress software, a re-screening was carried out according to the inclusion and exclusion criteria. After excluding ineligible studies, 24 articles were ultimately included (Figure 1).
Figure 1.
Literature selection process.
Basic characteristics and quality evaluation
The characteristics and quality evaluation of the included studies are summarized in Table 2. Among the 24 studies, 22 were published in Chinese and 2 in English. The studies included 8 RCTs, 8 case-control trials, and 8 cohort trials, involving a total of 2388 patients. Table 3 provides detailed information on the distribution of patient numbers, ages, and genders for each study.
Table 2.
Basic information of included literature
| Author | Year of publication | Area | Study type | Sample capacity | The incidence of hypoglycemia (%) | Influencing factor | Literature quality rating | |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Case/Exposure/T | Comparison/C | |||||||
| Chen Li [10] | 2023 | Hainan | Case control | 58 | 62 | 48.33 | ①②③⑦ | 8b |
| Lei Jiandong [11] | 2022 | Leshan | Case control | 112 | 130 | 53.71 | ⑦⑧⑨⑩ | 8b |
| Nian Sujuan [12] | 2021 | Hangzhou | Case control | 46 | 40 | 53.49 | ⑦⑧⑨⑩ | 7b |
| Liu Zipu [13] | 2021 | Hebei | Case control | 46 | 46 | - | ①②③ | 5b |
| Li Lishuang [14] | 2019 | Guangdong | Case control | 40 | 40 | - | ①②③ | 6b |
| Yu Ge [15] | 2018 | Qinghai | Cohort study | 50 | 62 | 44.64 | ①⑤ | 8b |
| Qian Feng [7] | 2018 | Jiangxi | Cohort study | 32 | 64 | 62.50 | - | 6b |
| Gianchandani [16] | 2018 | America | Case control | 76 | 74 | 50.67 | - | 7b |
| Cao Weibo [17] | 2017 | Shandong | RCT | 22 | 24 | - | ⑥ | 5a |
| Aiyitan Ayithazi [18] | 2017 | Xinjiang | RCT | 81 | 81 | - | ⑥ | 4a |
| Sun Yuanbo [19] | 2016 | Heilongjiang | Cohort study | 18 | 48 | 27.27 | ④ | 8b |
| Wu Han [20] | 2016 | Anhui | RCT | 35 | 35 | - | ⑤ | 4a |
| Chen Qingyun [21] | 2015 | Henan | RCT | 20 | 22 | - | ⑥ | 4a |
| Li Yuxia [22] | 2014 | Guangdong | Case control | 56 | 244 | 18.67 | ①②③ | 6b |
| Zhang Shouqing [23] | 2014 | Henan | Cohort study | 59 | 58 | - | ⑥ | 7b |
| Zhang Yanli [24] | 2013 | Hebei | RCT | 68 | 57 | - | ⑤ | 5a |
| Li Xiaoyan [25] | 2013 | Jiangxi | RCT | 40 | 40 | - | ⑥ | 5a |
| He Xiaolan [26] | 2011 | Changsha | Cohort study | 15 | 43 | 29.31 | ④ | 7b |
| Chen Li [27] | 2010 | Henan | Cohort study | 9 | 16 | 44.00 | ⑤ | 6b |
| Liu Jiang [28] | 2009 | Ningbo | Case control | 31 | 31 | 25.81 | - | 6b |
| Sun [29] | 2009 | Taiwan | Cohort study | 54 | 48 | 52.94 | - | 8b |
| Zhang Li [30] | 2008 | Xi’an | RCT | 48 | 46 | - | ⑥ | 4a |
| Huang Yuqing [31] | 2008 | Jiangxi | RCT | 15 | 15 | - | ⑥ | 4a |
| Feng Xuefang [32] | 2007 | Shanghai | Cohort study | 17 | 38 | 32.72 | ④ | 7b |
Note: ① Age; ② DKD course; ③ Oral hypoglycemic drugs; ④ Fasting plasma glucose (FPG); ⑤ Insulin use; ⑥ Sugar free dialysate; ⑦ Coefficient of variation in blood glucose (CVBG = standard deviation of blood glucose/MBG); ⑧ Mean blood glucose (MBG); ⑨ Medication compliance; ⑩ Self-care ability; - indicates no relevant data or inability to perform quantitative synthesis;
is the Jadad score;
is the NOS score.
Table 3.
Total number of patients included in the study, gender distribution, age
| Author | Year of publication | Number of patient cases | Male | Female | Average age (years) |
|---|---|---|---|---|---|
| Chen Li [10] | 2023 | 120 | 76 | 44 | 52.7±8.5 |
| Lei Jiandong [11] | 2022 | 242 | 135 | 107 | NI |
| Nian Sujuan [12] | 2021 | 86 | 55 | 31 | 65.1±11.3 |
| Liu Zipu [13] | 2021 | 46 | NI | NI | NI |
| Li Lishuang [14] | 2019 | 160 | 80 | 80 | NI |
| Yu Ge [15] | 2018 | 112 | 84 | 28 | NI |
| Qian Feng [7] | 2018 | 96 | 56 | 40 | NI |
| Gianchandani [16] | 2018 | 150 | 79 | 71 | 60.4±14.0 |
| Cao Weibo [17] | 2017 | 46 | 32 | 14 | NI |
| Aiyitan Ayithazi [18] | 2017 | 162 | 84 | 29 | 61.5±7.5 |
| Sun Yuanbo [19] | 2016 | 66 | 37 | 29 | 55.0±12.2 |
| Wu Han [20] | 2016 | 70 | 46 | 24 | 54.7±12.0 |
| Chen Qingyun [21] | 2015 | 42 | 27 | 15 | 56.8±6.0 |
| Li Yuxia [22] | 2014 | 300 | 169 | 131 | NI |
| Zhang Shouqing [23] | 2014 | 117 | 72 | 45 | NI |
| Zhang Yanli [24] | 2013 | 125 | 72 | 53 | 60.6±10.7 |
| Li Xiaoyan [25] | 2013 | 80 | 44 | 36 | 66.4±4.9 |
| He Xiaolan [26] | 2011 | 58 | 36 | 22 | NI |
| Chen Li [27] | 2010 | 25 | 13 | 12 | 62.2±12.9 |
| Liu Jiang [28] | 2009 | 31 | 18 | 13 | 61.3±9.5 |
| Sun [29] | 2009 | 102 | 60 | 42 | 64.1±10.9 |
| Zhang Li [30] | 2008 | 94 | 52 | 42 | 65.2±7.4 |
| Huang Yuqing [31] | 2008 | 30 | 15 | 15 | NI |
| Feng Xuefang [32] | 2007 | 55 | 26 | 29 | NI |
Note: NI, no information.
Meta-analysis results
Meta-analysis of the incidence of hypoglycemia in DKD patients undergoing MHD
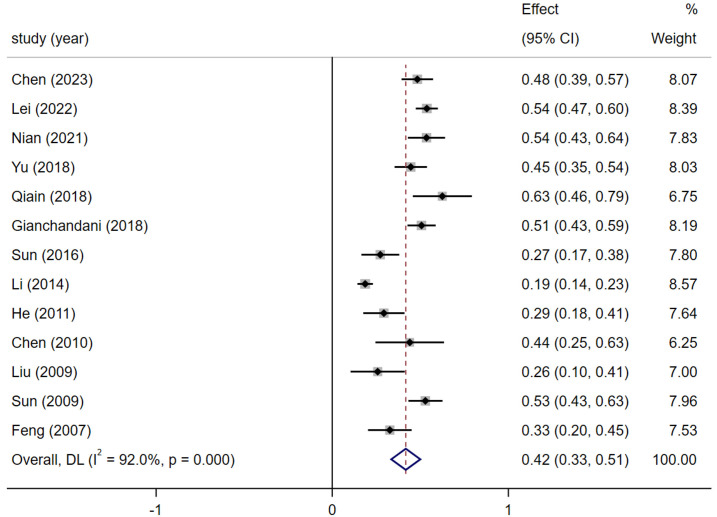
Of the 24 studies, 13 provided data suitable for meta-analysis of the hypoglycemia incidence in DKD patients undergoing MHD. Given the heterogeneity observed among the included studies (I2 = 92%), a random-effects model was used. The results showed that the incidence of hypoglycemia in DKD patients undergoing MHD was 41.7% (95% CI: 32.6% to 50.9%), as shown in Figure 2.
Figure 2.
Forest plot of maintenance hemodialysis (MHD).
Subgroup analysis of the incidence of hypoglycemia in DKD patients undergoing MHD
Subgroup analyses were conducted based on research type and publication year. For cohort studies (n = 7), the heterogeneity was high (I2 = 75.6%, P < 0.001), with a calculated hypoglycemia incidence of 41.3% (95% CI: 32.1-50.6). For case-control studies (n = 6), the heterogeneity was substantial (I2 = 95.9%, P < 0.001), with a calculated hypoglycemia incidence of 41.9% (95% CI: 26.4-57.4). When stratified by publication year, 6 articles published within the last 5 years (I2 = 0.0, P = 0.425) revealed a hypoglycemia incidence of 51.2% (95% CI: 47.6-54.8), whereas 7 articles published over five years ago showed significant heterogeneity (I2 = 86.6, P < 0.001) and an incidence of 32.5% (95% CI: 21.7-43.2) (Table 4).
Table 4.
Subgroup analysis of hypoglycemia incidence in DKD patients undergoing MHD
| Different research types | Number of studies included | Heterogeneity test | Effect model | The incidence of hypoglycemia (%) (95% CI) | |
|---|---|---|---|---|---|
|
| |||||
| I2 (%) | P | ||||
| Study type | |||||
| Cohort study | 7 [7,15,19,26,29,31,32] | 75.6 | < 0.001 | Random | 41.3 (32.1-50.6) |
| Case-control study | 6 [10-12,16,22,28] | 95.9 | < 0.001 | Random | 41.9 (26.4-57.4) |
| Publication year of the paper | |||||
| Over the past 5 years (2018 to present) | 6 [7,10-12,15,16] | 0.0 | 0.425 | Regular | 51.2 (47.6-54.8) |
| 5 years ago (before 2018) | 7 [19,22,26-29,32] | 86.6 | < 0.001 | Random | 32.5 (21.7-43.2) |
Note: MHD, maintenance hemodialysis; DKD, diabetic kidney disease; OR, odds ratio; RR, risk ratio; CI, confidence interval.
Meta-analysis of influencing factors
Among the 24 studies, 20 were eligible for quantitative analysis, identifying 10 extractable influencing factors. These factors were analyzed and their OR/RR values and 95% CI were pooled. The final meta-analysis identified the following risk factors for hypoglycemia in DKD patients undergoing MHD: age ≥ 60 years (I2 = 48.5, P = 0.101; OR/RR: 4.20, 95% CI: 3.00-5.89, Z = 8.334, P < 0.001), DKD course > 1 year (I2 = 0.0, P = 0.464; OR/RR: 3.55, 95% CI: 2.52-4.99, Z = 7.281, P < 0.001), use of oral hypoglycemic drugs (I2 = 67.2, P = 0.028; OR/RR: 4.64, 95% CI: 2.57-8.40, Z = 5.073, P < 0.001), FPG < 6.1 mmol/L (I2 = 0.0, P = 0.986; OR/RR: 4.03, 95% CI: 2.59-6.27, Z = 6.196, P < 0.001), pre-dialysis insulin use (I2 = 0.0, P = 0.714; OR/RR: 8.24, 95% CI: 4.52-15.04), Z = 6.196, P < 0.001), use of glucose-free dialysate (I2 = 18.5, P = 0.289; OR/RR: 7.99, 95% CI: 4.61-13.86, Z = 7.395, P < 0.001), CVBG ≥ 0.26 (I2 = 0.0, P = 0.590; OR/RR: 3.24, 95% CI: 2.07-5.07, Z = 5.147, P < 0.001), MBG < 8.92 mmol/L, poor medication adherence (I2 = 0.0, P = 0.545; OR/RR: 2.93, 95% CI: 1.64-5.25, Z = 5.147, P < 0.001), and poor caring ability (I2 = 0.0, P = 0.810; OR/RR: 3.54, 95% CI: 1.77-7.11, Z = 3.561, P < 0.001) (Table 5).
Table 5.
Meta-analysis of the influencing factors of hypoglycemia in DKD patients undergoing MHD
| Influencing factor | Number of studies included | Heterogeneity test | Effect model | OR/RR (95% CI) | Z | P | |
|---|---|---|---|---|---|---|---|
|
| |||||||
| I2 (%) | P | ||||||
| Age | 5 [10,13-15,22] | 48.5 | 0.101 | Regular | 4.20 (3.00-5.89) | 8.334 | < 0.001 |
| DKD course | 4 [10,13,14,22] | 0.0 | 0.464 | Regular | 3.55 (2.52-4.99) | 7.281 | < 0.001 |
| Oral hypoglycemic drugs | 4 [10,13,14,22] | 67.2 | 0.028 | Random | 4.64 (2.57-8.40) | 5.073 | < 0.001 |
| FPG | 3 [19,26,32] | 0.0 | 0.986 | Regular | 4.03* (2.59-6.27) | 6.196 | < 0.001 |
| Insulin use | 4 [15,20,24,27] | 0.0 | 0.714 | Regular | 8.24 (4.52-15.04) | 6.872 | < 0.001 |
| Sugar free dialysate | 7 [17,18,21,23,25,30,31] | 18.5% | 0.289 | Regular | 7.99* (4.61-13.86) | 7.395 | < 0.001 |
| CVBG | 3 [10-12] | 0.0 | 0.590 | Regular | 3.24 (2.07-5.07) | 5.147 | < 0.001 |
| MBG | 2 [11,12] | 0.0 | 0.545 | Regular | 2.93 (1.64-5.25) | 3.614 | < 0.001 |
| Medication compliance | 2 [11,12] | 48.3 | 0.164 | Regular | 4.30 (2.05-9.03) | 3.852 | < 0.001 |
| Self-care ability | 2 [11,12] | 0.0 | 0.810 | Regular | 3.54 (1.77-7.11) | 3.561 | < 0.001 |
Note: MHD, maintenance hemodialysis; DKD, diabetic kidney disease; OR, odds ratio; RR, risk ratio; CI, confidence interval; FPG, fasting plasma glucose; CVBG, Coefficient of variation in blood glucose; MBG, mean blood glucose;
represents the RR value, while the rest represent the OR value.
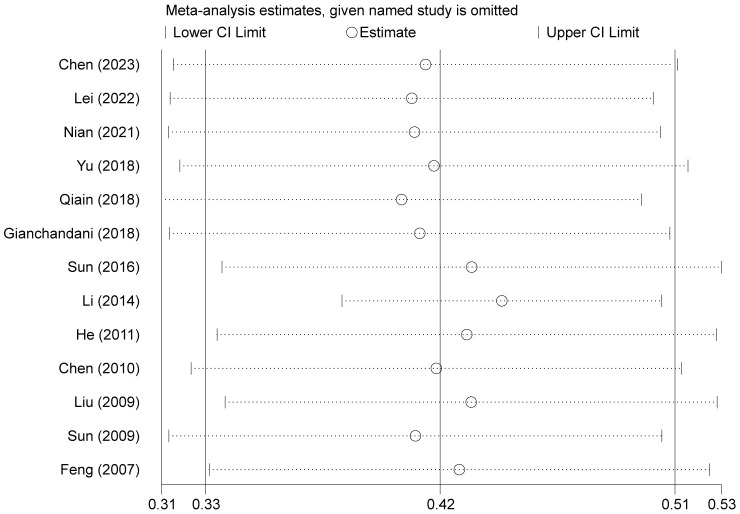
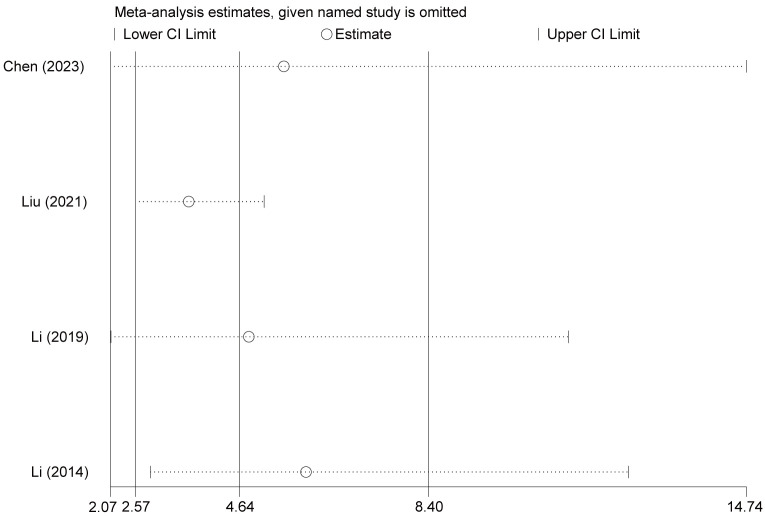
Sensitivity analysis
Due to the significant heterogeneity observed in the incidence of hypoglycemia among DKD patients undergoing MHD, a sequential exclusion method was used for sensitivity analysis. Following the exclusion of certain studies, the results showed that the incidence of hypoglycemia was 40.2% to 42.9%, which was similar to the previously reported figure of 41.7%. This finding indicates that the meta-analysis results are relatively robust. In the analysis of influencing factors, the heterogeneity associated with oral hypoglycemic drugs was found to be 67.2%. A sensitivity analysis was conducted using the same method, and the combined effect values did not show substantial change, further supporting the stability of the meta-analysis results (Figures 3 and 4).
Figure 3.
Sensitivity analysis of the incidence of maintenance hemodialysis (MHD)-associated hypoglycemia in patients with DKD.
Figure 4.
The susceptibility analysis of oral antidiabetic drugs.
Publication bias
Assessment of publication bias using a funnel plot for the incidence of hypoglycemia showed asymmetry among the study points. However, Begg’s test (Z = 1.04, P = 0.300) and Egger’s test (t = 1.50, P = 0.161) did not suggest publication bias (Figure 5).
Figure 5.
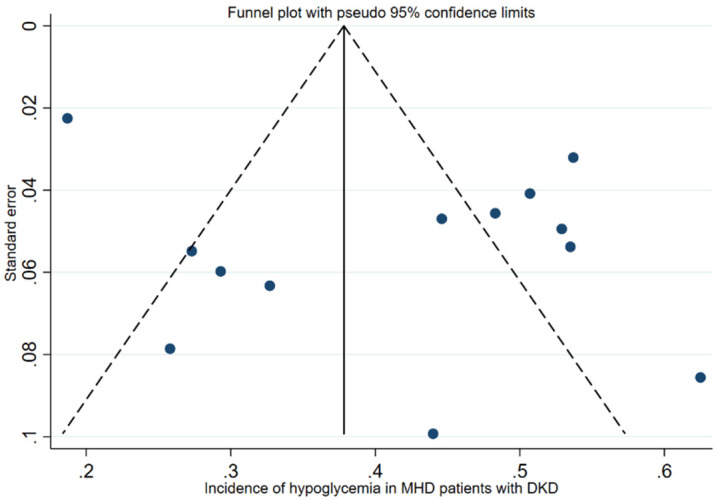
Funnel plot of maintenance hemodialysis (MHD)-associated hypoglycemia incidence rate in DKD patients.
Discussion
Higher incidence of hypoglycemia in DKD patients undergoing MHD
DKD is a leading cause of end-stage kidney disease. Over the past two decades, data on dialysis in China show a rising proportion of DKD as the underlying cause of end-stage kidney disease [33]. Hypoglycemia is a prevalent acute complication in DKD patients undergoing hemodialysis. International studies have reported that the incidence of hypoglycemia during dialysis is 23.8% to 47.6% [6,7], whereas studies from China have shown a significantly higher range of 34.4% to 62.5%, compared to 12.5% to 18.7% in non-DKD hemodialysis patients [7]. Moreover, the incidence of severe hypoglycemia in elderly patients (≥ 60 years) is in one study was alarmingly high at 87.5% [34]. Our meta-analysis revealed that the incidence of hypoglycemia during hemodialysis in DKD patients was 41.7% (95% CI: 32.6-50.9%). Given the heterogeneity across studies, further subgroup analyses were conducted based on the study design. Results showed a combined hypoglycemia incidence of 41.3% (95% CI: 32.1% to 50.6%) for seven cohort studies, with a decrease in heterogeneity (I2 = 75.6%), accounting for some heterogeneity. Additionally, studies published more than five years ago reported a hypoglycemia incidence of 32.5% (95% CI: 21.7% to 43.2%) in DKD patients undergoing dialysis, while recent studies reported a higher incidence of 51.2% (95% CI: 47.6% to 54.8%), with homogeneity among the studies. These findings suggest that variability in reported hypoglycemia incidence could be influenced by factors such as differences in monitoring methods, reporting selections, and the presence of asymptomatic hypoglycemia, which might lead to an underestimation of the true incidence and severity [35]. In addition, hypoglycemia, while often easier to correct than hyperglycemia, receives less preventive attention from patients. The International Hypoglycemia Study Group has pointed out that hypoglycemia is a risk factor for cardiovascular disease and death [36]. In recent years, medical practice has begun to emphasize the importance of hypoglycemia prevention, making it a key research focus.
Factors influencing hypoglycemia in DKD patients undergoing MHD
(1) Age and course of DKD: Epidemiological studies have shown that more than half of MHD patients are elderly. Elderly DKD patients often suffer from peripheral neuropathy, which impairs central nervous system response and reflex regulation to hypoglycemia, increasing the risk of asymptomatic hypoglycemia. This can lead to misdiagnoses such as cerebrovascular diseases, delaying appropriate treatment and resulting in more serious consequences [38,39]. Moreover, a course of DKD exceeding one year can increase the risk of adrenal insufficiency, leading to reduced insulin degradation and glucocorticoid secretion, thereby contributing to lower blood glucose levels. Therefore, patients aged ≥ 60 years and with a DKD course > 1 year need more attention to prevent asymptomatic hypoglycemia.
(2) Oral hypoglycemic drugs: While previous meta-analyses indicated that hypoglycemic drugs have cardio-renal protection effects in patients with type 2 diabetes [40,41], their use may also lead to side effects of hypoglycemia, particularly in DKD patients with impaired renal drug metabolism. Hypoglycemic drugs are mainly metabolized by the kidneys, and this can easily lead to increased hypoglycemia risk during dialysis, especially in elderly patients with renal atrophy and reduced renal blood flow. This study included four original studies, and the results showed that patients who took oral hypoglycemic drugs on dialysis days had a 3.64-fold increased risk of hypoglycemia compared to those who did not. Caution is recommended in using these medications, particularly in light of guidelines [42] that contraindicate most oral hypoglycemic drugs, such as sulfonylureas and biguanides, in dialysis patients. Further research is necessary to explore the use of most traditional and novel oral hypoglycemic drugs in dialysis patients, as these medications often require dose adjustments or lack relevant evidence.
(3) Fasting plasma glucose (FPG): FPG levels are an important factor affecting blood glucose fluctuations. Hemodialysis induces U-shaped glucose fluctuations [43], similar to the FPG variation. Our findings showed that patients with an FPG level of < 6.1 mmol/L had a 4.03 times higher risk of hypoglycemia than those with an FPG of ≥ 6.1mmol/L. However, elevated PFG levels also increased the incidence of complications, such as infection. Thus, maintaining an FPG between 6.1 and 7 mmol/L appears optimal for minimizing the risks of hypoglycemia and other complications.
(4) Insulin use: Hypoglycemia during dialysis is closely related to insulin dosage and insulin resistance [44]. Although insulin resistance tends to improve in DKD patients, insulin’s macromolecular nature makes it difficult to pass through dialysis membranes, extending the half-life of exogenous insulin. If the original insulin dose remain unchanged, there is an increased risk of hypoglycemia [45]. Therefore, insulin regimens for DKD patients on dialysis should be individualized and adjusted on dialysis days to prevent hypoglycemia.
(5) Glucose-free dialysate use: Our analysis revealed a 6.99-fold increased risk of hypoglycemia with the use of glucose-free dialysate. The gradient in glucose concentration between plasma and dialysate during dialysis promotes the diffusion of plasma glucose into the dialysate, leading to continuous glucose loss (15-30 g per session) [2]. With diminished renal gluconeogenesis, the risk of hypoglycemia is greatly increased [46]. Therefore, the use of glucose-free dialysate may cause hypoglycemia.
(6) Coefficient of variation in blood glucose (CVBG) and mean blood glucose (MBG): CVBG (standard deviation/MBG) and MBG can reflect the fluctuation of blood glucose [47]. Fluctuating blood glucose levels indicate poor glycemic control, which leads to poor prognosis. This study showed that patients with CVBG ≥ 0.26 and MBG < 8.92 mmol/L had a 2.24-fold and 1.93-fold increased risk of hypoglycemia, respectively. Elderly diabetic patients exhibited greater blood glucose variability and poorer hypoglycemia awareness [48], possibly leading to poor blood glucose management. Thus, careful monitoring of CVBG and MBG during patient treatment.
(7) Medication compliance and caring ability: Recent research has increasingly recognized the impact of psychosocial factors on hypoglycemia in dialysis patients with diabetes. As a chronic condition, kidney disease demands medication adherence and self-management, which are often intertwined with socio-economic status and self-care ability. DKD patients require adjustment to their hypoglycemic drugs or insulin dosages during hemodialysis. Individuals exhibiting poor medication adherence to prescribed hypoglycemic regimens are at an increased risk of hypoglycemia. Effective care involves both family support and self-management behaviors. A robust social support system is beneficial in fostering self-management behaviors among diabetic patients and enhancing their confidence in preventing hypoglycemia [49]. Conversely, patients with inadequate self-management levels tend to exhibit poor compliance. They struggle to effectively manage physical activity, monitor blood glucose, and adhere to medication and nutrition regimens, which increase their susceptibility to hypoglycemia [50]. Therefore, it is imperative to prioritize clinical evaluations in this context.
This study has several limitations: (1) Most of the studies included in this analysis are in Chinese, which may result in regional bias; (2) Research on the impact of CVBG, MBG, medication adherence, and self-care ability on hypoglycemia is relatively nascent, especially studies on medication adherence and care ability. In addition, the limited number of studies available may introduce bias, necessitating further high-quality investigations.
In summary, the incidence of hypoglycemia in DKD patients during hemodialysis is relatively high, with recent studies indicating an upward trend. Factors such as advanced age, a course of DKD exceeding 1 year, oral hypoglycemic drug use, an FPG level of less than 6.1 mmol/L, pre-dialysis insulin use, use of sugar-free dialysate, large blood glucose fluctuations, and poor medication compliance and caring ability are associated with increased risk of hypoglycemia. Strategies to mitigate these risks include adjusting hypoglycemic or insulin regimens on dialysis days, using sugar-containing dialysate, and implementing educational interventions and social support measures to improve patient compliance and self-care capabilities, ultimately improving patient outcomes.
Acknowledgements
This work was supported by Innovation Project of Guangxi Graduate Education (YCSY2022043) and Guangxi Traditional Chinese Medicine Key Discipline Construction Project (GZXK-Z-20-56).
Disclosure of conflict of interest
None.
References
- 1.Mori K. Maintenance of skeletal muscle to counteract sarcopenia in patients with advanced chronic kidney disease and especially those undergoing hemodialysis. Nutrients. 2021;13:1538. doi: 10.3390/nu13051538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Watha K, Davenport A, Tangvoraphonkchai K. Changes in blood glucose and lactate concentrations with hemodialysis. Artif Organs. 2022;46:138–145. doi: 10.1111/aor.14097. [DOI] [PubMed] [Google Scholar]
- 3.Cao HX, Shao ZH, Yan L, Shao FM. A novel strategy to manage chronic kidney diseases based on a four-level stratified prevention and treatment model. Journal of Chinese Practical Diagnosis and Therapy. 2021;35:1081–1083. [Google Scholar]
- 4.Sun XD, Diao ZL, Liu X. Analysis on death risk factors in patients with diabetic nephropathy undergoing maintenance hemodialysis. Journal of Clinical and Experimental Medicine. 2017;16:633–636. [Google Scholar]
- 5.Hsiao CC, Tu HT, Lin CH, Chen KH, Yeh YH, See LC. Temporal trends of severe hypoglycemia and subsequent mortality in patients with advanced diabetic kidney diseases transitioning to dialysis. J Clin Med. 2019;8:420. doi: 10.3390/jcm8040420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang RT, Liu Y, Lin KK, Jia WN, Wu QY, Wang J, Bai XY. Development of a clinical automatic calculation of hypoglycemia during hemodialysis risk in patients with diabetic nephropathy. Diabetol Metab Syndr. 2023;15:199. doi: 10.1186/s13098-023-01177-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Qian F, Zhang YL, Guo Y. Comparative analysis of complications in hemodialysis patients with end-stage diabetes nephropathy and non diabetes nephropathy. Modern Drug Applications. 2018;12:55–57. [Google Scholar]
- 8.Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: is blinding necessary. Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 9.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 10.Chen L, Wang ZQ, Gu SH. Risk factors analysis and prediction model establishment of hypoglycemia in hemodialysis with glucose free dialysate for patients with diabetes nephropathy. Chinese Journal of Practical Diagnosis and Treatment. 2023;37:179–183. [Google Scholar]
- 11.Lei JD, Wu LJ, Ji S. Establishment of hypoglycemia prediction model and scoring scale for maintenance hemodialysis patients with diabetes nephropathy. Chinese Journal of Nephropathy Research. 2022;11:311–317. [Google Scholar]
- 12.Nian SJ, Li HL, Li E. Study on the occurrence and influencing factors of hypoglycemia in hemodialysis patients with diabetes. Chinese General Medicine. 2021;24:1889–1896. [Google Scholar]
- 13.Liu ZP, Yin BR, Yao M. Analysis of the causes of hypoglycemia in diabetes nephropathy patients caused by hemodialysis. China Health and Nutrition. 2021;31:24–25. [Google Scholar]
- 14.Li LS, Lv WQ, Chen ZT. Analysis of risk factors for hypoglycemia in hemodialysis of patients with diabetes nephropathy. Modern Drug Applications in China. 2019;13:41–43. [Google Scholar]
- 15.Yu G. Analysis of blood glucose fluctuation in maintenance hemodialysis patients with diabetes nephropathy. Qinghai University; 2018. [Google Scholar]
- 16.Gianchandani RY, Neupane S, Heung M. Hypoglycemia in hospitalized hemodialysis patients with diabetes: an observational study. J Diabetes Sci Technol. 2018;12:33–38. doi: 10.1177/1932296817747620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cao WB. Effect of sugar containing dialysate on hemodialysis patients with diabetes nephropathy. Chinese and Foreign Medical. 2017;36:25–27. [Google Scholar]
- 18.Aiyitan A, Qing Q. Study on the effect of sugar free and sugar containing dialysate on blood glucose in patients with diabetes nephropathy. Chinese and Foreign Medical. 2017;36:85–87. [Google Scholar]
- 19.Sun YB, Li GQ, Wang YF. Effect of blood glucose control on complications in maintenance hemodialysis patients with diabetes nephropathy. Lab Med. 2016;31:104–105. [Google Scholar]
- 20.Wu H, Cheng L, Han RD. Intervention of hypoglycemia during dialysis in patients with diabetes nephropathy. Chinese Maternal and Child Health Research. 2016;27:238–239. [Google Scholar]
- 21.Chen QY. Effects of sugar containing dialysate on blood pressure and blood sugar in dialysis patients with diabetes nephropathy. Chinese Practical Medicine. 2015;10:105–106. [Google Scholar]
- 22.Li YX. Analysis of risk factors of hypoglycemia in hemodialysis and nursing care of patients with diabetes nephropathy receiving insulin maintenance therapy. Clinical Medical Engineering. 2014;21:1349–1350. [Google Scholar]
- 23.Zhang SQ. Effects of sugar or sugar free dialysate on mean arterial pressure and heart rate variability in hemodialysis patients with diabetes nephropathy. Journal of Practical Cardiovascular, Cerebrovascular and Pulmonary Vascular Diseases. 2014;22:73–74. [Google Scholar]
- 24.Zhang YL, Ma JJ, Zhang HJ. Observation of hypoglycemic care in hemodialysis with different insulin treatment regimens. Journal of Nurse Continuing Education. 2013;28:1370–1371. [Google Scholar]
- 25.Li XY, Yang G, Zhong SM. Effect of hemodialysis with sugar containing dialysate on incidence of hypoglycemia and hypotension in elderly patients with end-stage diabetes nephropathy. Chinese and Foreign Medical Research. 2013;11:18–19. [Google Scholar]
- 26.He XL. Effect of blood glucose control on complications of maintenance hemodialysis patients with diabetes nephropathy. Clinical Meta. 2011;26:1424–1425. [Google Scholar]
- 27.Chen L, Yang YX. Observation and nursing of hypoglycemia in hemodialysis for patients with diabetes nephropathy. Chinese Practical Medicine. 2010;5:188–189. [Google Scholar]
- 28.Liu J, Xu PF, Yang JG, Yang M, Qiu XH. Clinical analysis of acute and chronic complications in hemodialysis for diabetes nephropathy and non diabetes nephropathy. Journal of Practical Medicine. 2009;25:4172–4173. [Google Scholar]
- 29.Sun CY, Lee CC, Wu MS. Hypoglycemia in diabetic patients undergoing chronic hemodialysis. Ther Apher Dial. 2009;13:95–102. doi: 10.1111/j.1744-9987.2009.00662.x. [DOI] [PubMed] [Google Scholar]
- 30.Zhang L, Qiao BJ, An JM, Meng GQ. Observation on the effect of dialysis solution containing sugar and non sugar on end-stage diabetes nephropathy. Journal of Guangdong Medical College. 2008;3:300–301. [Google Scholar]
- 31.Huang YQ, Liu R, Chen XL. Effects of low glucose dialysate on BS and INS in hemodialysis patients with end-stage diabetes nephropathy. Journal of Gannan Medical College. 2008;3:355–357. [Google Scholar]
- 32.Feng XF, Zhang Y, Zhou R. Effect of blood glucose control on complications in maintenance hemodialysis patients with diabetes nephropathy. China Blood Purification. 2007;6:257–259. [Google Scholar]
- 33.Yang C, Gao B, Zhao X, Su Z, Sun X, Wang HY, Zhang P, Wang R, Liu J, Tang W, Zhang D, Chu H, Wang J, Wang F, Wang S, Zuo L, Wang Y, Yu F, Wang H, Zhang L, Zhang H, Yang L, Chen J, Zhao MH. Executive summary for China kidney disease network (CK-NET) 2016 annual data report. Kidney Int. 2020;98:1419–1423. doi: 10.1016/j.kint.2020.09.003. [DOI] [PubMed] [Google Scholar]
- 34.Ha WC, Oh SJ, Kim JH, Lee JM, Chang SA, Sohn TS, Son HS. Severe hypoglycemia is a serious complication and becoming an economic burden in diabetes. Diabetes Metab J. 2012;36:280–284. doi: 10.4093/dmj.2012.36.4.280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kong YX, Dong AM, Zheng JT. Analysis of hypoglycemia and its influencing factors in outpatients with type 2 diabetes. Chinese General Practitioner. 2019;22:936–941. [Google Scholar]
- 36.International Hypoglycaemia Study Group. Hypoglycaemia, cardiovascular disease, and mortality in diabetes: epidemiology, pathogenesis, and management. Lancet Diabetes Endocrinol. 2019;7:385–396. doi: 10.1016/S2213-8587(18)30315-2. [DOI] [PubMed] [Google Scholar]
- 37.Diao ZL, Guo W, Huang HD. Epidemiological survey of hemodialysis patients in Beijing from 2016 to 2020. J Med Res. 2022;51:114–117. [Google Scholar]
- 38.Freeman J. Management of hypoglycemia in older adults with type 2 diabetes. Postgrad Med. 2019;131:241–250. doi: 10.1080/00325481.2019.1578590. [DOI] [PubMed] [Google Scholar]
- 39.Hoogwerf BJ. Hypoglycemia in older patients. Clin Geriatr Med. 2020;36:395–406. doi: 10.1016/j.cger.2020.04.001. [DOI] [PubMed] [Google Scholar]
- 40.Tsapas A, Avgerinos I, Karagiannis T, Malandris K, Manolopoulos A, Andreadis P, Liakos A, Matthews DR, Bekiari E. Comparative effectiveness of glucose-lowering drugs for type 2 diabetes: a systematic review and network meta-analysis. Ann Intern Med. 2020;173:278–286. doi: 10.7326/M20-0864. [DOI] [PubMed] [Google Scholar]
- 41.Nuffield Department of Population Health Renal Studies Group; SGLT2 inhibitor Meta-Analysis Cardio-Renal Trialists’ Consortium. Impact of diabetes on the effects of sodium glucose co-transporter-2 inhibitors on kidney outcomes: collaborative meta-analysis of large placebo-controlled trials. Lancet. 2022;400:1788–1801. doi: 10.1016/S0140-6736(22)02074-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Expert Group of Nephrology Branch of Chinese Medical Association Chinese guidelines on renal replacement therapy for end-stage diabetes nephropathy. Chinese Journal of Kidney Disease. 2022;38:62–75. [Google Scholar]
- 43.Chen WX, Ju CP, Cui L. Blood glucose changes in regular hemodialysis patients with diabetes during hemodialysis: a multicenter cross-sectional study. Chinese General Medicine. 2020;23:4183–4189. [Google Scholar]
- 44.Li Y. Analysis on the effect of cluster nursing in preventing hypoglycemia in hemodialysis of patients with diabetes nephropathy. Hunan Journal of Traditional Chinese Medicine. 2017;33:121–123. [Google Scholar]
- 45.Amiel SA. The consequences of hypoglycaemia. Diabetologia. 2021;64:963–970. doi: 10.1007/s00125-020-05366-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hayashi A, Shimizu N, Suzuki A, Matoba K, Momozono A, Masaki T, Ogawa A, Moriguchi I, Takano K, Kobayashi N, Shichiri M. Hemodialysis-related glycemic disarray proven by continuous glucose monitoring; glycemic markers and hypoglycemia. Diabetes Care. 2021;44:1647–1656. doi: 10.2337/dc21-0269. [DOI] [PubMed] [Google Scholar]
- 47.Breyton AE, Lambert-Porcheron S, Laville M, Vinoy S, Nazare JA. CGMS and glycemic variability, relevance in clinical research to evaluate interventions in t2d, a literature review. Front Endocrinol (Lausanne) 2021;12:666008. doi: 10.3389/fendo.2021.666008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yan SC, Yang W, Wang JY, Luo HY, Ma YX, Zhao H. The correlation between blood glucose variability, average blood glucose fluctuation and cardiac function in elderly patients with type 2 diabetes. Practical Geriatrics. 2023;37:361–364. [Google Scholar]
- 49.Yang KL, Liu Y, Lu FL. Analysis of hot literature on diabetes nursing research in social network field based on Web of Science. PLA Nursing Journal. 2019;36:42–45. [Google Scholar]
- 50.Yang D, Li SQ. Research progress on the effect of hypoglycemia on cardiovascular disease in patients with type 2 diabetes. Sichuan Medicine. 2020;41:320–322. [Google Scholar]