Abstract
Introduction:
Riedel’s thyroiditis is a rare inflammatory disease of the thyroid with non-specific and varied presentations. A typical presentation and ultrasound findings are reported in this case.
Case Report:
A 68-year-old male is referred to Ear, Nose and Throat for a neck lump that varied in size over 2 years. An ultrasound scan identified a suspicious nodule on the left thyroid that was biopsied confirming the diagnosis of Riedel’s thyroiditis.
Discussion:
The aetiology, presentation and management of Riedel’s thyroiditis are explored. The use of ultrasound and the utility of other imaging and biochemical tests are discussed.
Conclusion:
Riedel’s thyroiditis is a difficult condition to diagnose due to rarity, varied presentation, with non-specific clinical, biochemical and radiographic findings which often mimic thyroid cancers. Definitive diagnosis of Riedel’s thyroiditis requires histological analysis, and while fine-needle aspirations are typically insufficient, diagnostic samples can be taken with ultrasound-guided core biopsies.
Keywords: Ultrasound, CT, head and neck, ultrasound appearances, clinical
Introduction
Riedel’s thyroiditis (RT) is a rare inflammatory condition resulting in fibrosis of the thyroid and adjacent structures. It has a potential relationship with IgG4-mediated spectrum of fibrosclerotic disease. Presentations vary from a small, non-tender, firm neck nodule, to a diffuse, firm and painful goitre causing dysphagia and dyspnoea. 1
Ultrasonography in RT typically reveals poorly defined, hypoechoic and hypovascular areas that mimic thyroid malignancy. 1 As a result, biopsy sampling is required, either via core biopsy using ultrasound guidance or surgical excision.
The computed tomography (CT) or magnetic resonance imaging (MRI) allows further assessment of extra-thyroid invasion and lymph node involvement. Treatment depends upon disease extent and patient choice, with options including active surveillance, steroidal treatment or other immunotherapy (e.g. tamoxifen) or surgical intervention.
Case history
A 68-year-old male was referred to Ear, Nose and Throat (ENT) with a 1-year history of an evolving palpable nodule at the level of the left thyroid with no signs of recent infection, thyroid disease or compressive symptoms. Clinical examination confirmed a fixed, non-tender and firm nodule in relation to the left lobe, with no associated lymphadenopathy. Nasendoscopy determined no pharyngeal or laryngeal abnormalities.
Initial blood tests showed normal serum anti-thyroid peroxidase (TPO) antibodies (6 IU/mL) and was negative for: anti-nuclear antibodies (ANAs), anti-DNA antibodies (1.8 IU/mL), anti-myeloperoxidase antibodies (<0.2 IU/mL) and anti-proteinase 3 (<0.2 IU/mL). Full blood count and electrolytes were normal across the board (cCa: 2.43 mmol/L). His C-reactive protein (CRP) was <1 mg/L, and erythrocyte sedimentation rate (ESR) was mildly raised at 25 mm/h.
Thyroid function tests were suggestive of subclinical hypothyroidism (thyroid-stimulating hormone (TSH) = 6.28, Free T4 = 13), and serum immunoglobulins showed no abnormalities (IgG = 12.9 g/L, IgA = 2.09 g/L, IgM = 0.7 g/L). Serum IgG4 was normal (0.53 g/L).
The patient proceeded to have an ultrasound assessment of the thyroid and neck which demonstrated an ill-defined, avascular, hypoechoic solid nodule measuring 17 × 13 × 13 mm in the left lobe with no associated lymphadenopathy, but extrathyroid extension into adjacent strap muscle was observed anteriorly (see Figure 1). Thyroid malignancy was the initial sonographic diagnosis, with a BTA grading of U5. Ultrasound was used to guide two 18G core biopsy samples with no complications.
Figure 1.
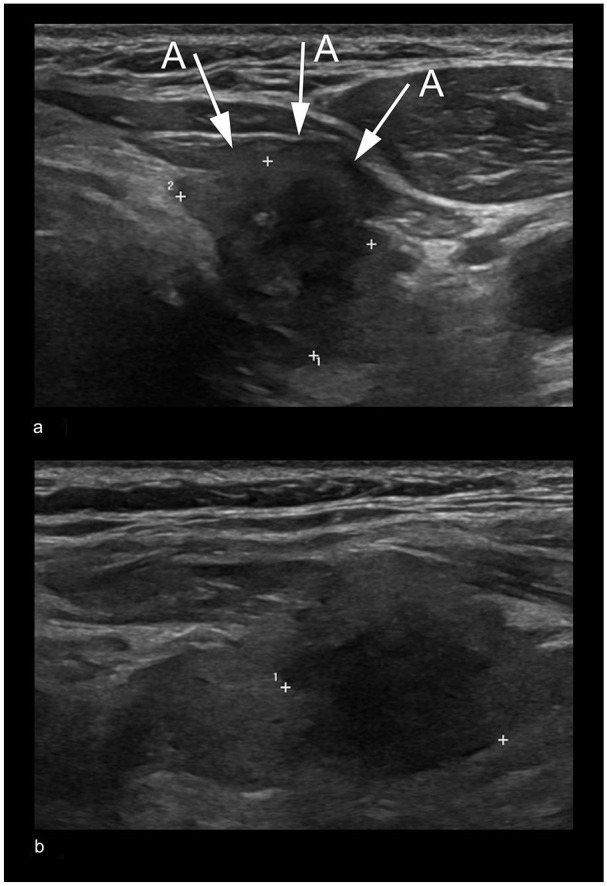
Axial (a) and sagittal (b) sonograms through the left thyroid lobe confirm a poorly defined, heterogeneous, hypoechoic left thyroid (callipers). On the axial image (a), extra-thyroid extent to involve over-lying strap muscle is demonstrated (arrows; A).
CT neck and chest with contrast showed a non-enlarged thyroid, with a poorly defined soft tissue mass within the left lobe, confirming extra-thyroid extension and infiltration of the overlying strap muscle (see Figure 2). The scan was otherwise unremarkable.
Figure 2.
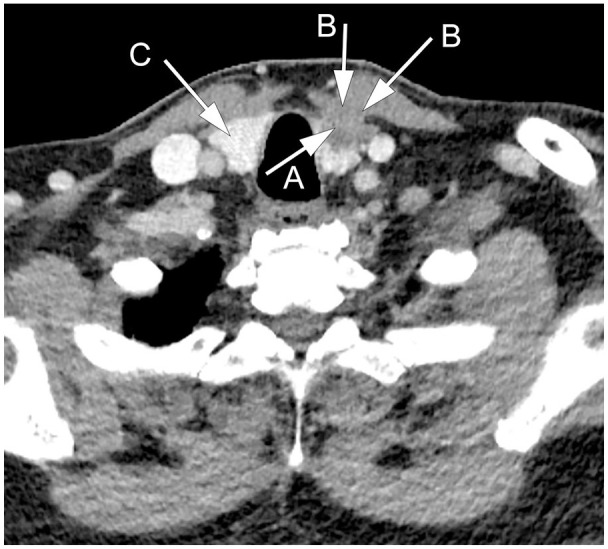
Axial post-contrast CT image at the left of the thyroid demonstrates an ill-defined, low attenuation lesion within the thyroid left lobe (A). This extends outside of the thyroid involving strap muscle (B). Normal thyroid right lobe (C).
Histology of the core sample showed largely fibrotic and sclerotic connective tissue interspersed with hemosiderin laden macrophages and eosinophils (see Figure 3). No cells of obvious malignant or granulomatous morphology were identified. Further special stains were performed which determined an absence of amyloid and calcitonin. Through this process of elimination, a diagnosis of RT was made. The patient declined surgical hemithyroidectomy, and a follow-up CT scan after 5 months showed stable appearances of the nodule; hence, a shared decision with the patient was made to avoid further intervention and to monitor him using active surveillance.
Figure 3.
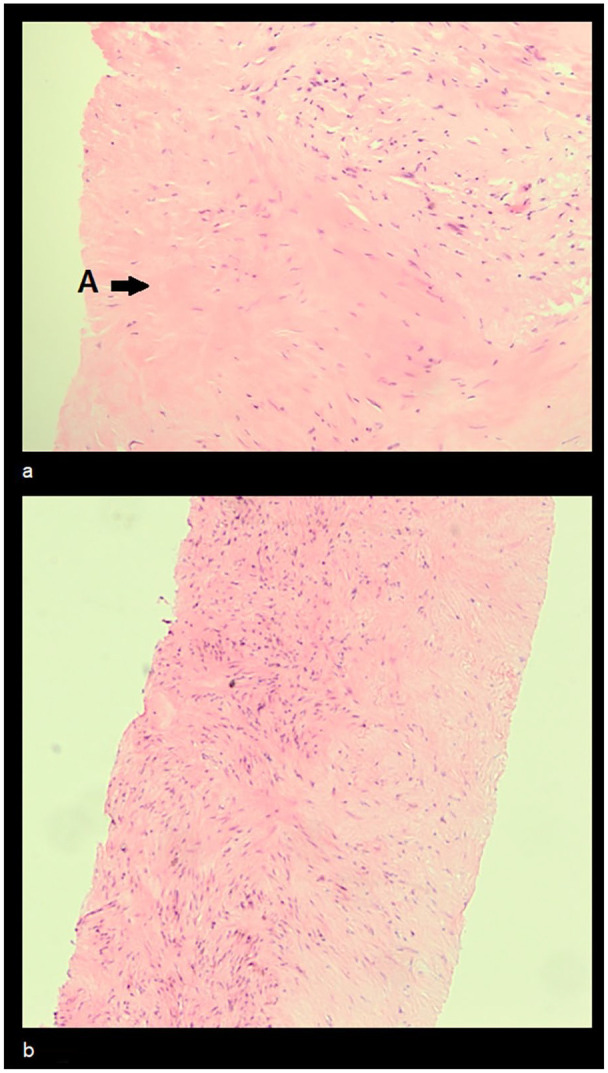
(a) (×20 magnification) and (b) (×10 magnification) core thyroid samples stained with hematoxylin and eosin under light microscopy. Dense, abnormal connective tissue (arrow A) interspersed with inflammatory cells can be seen.
Discussion
RT is a rare inflammatory condition characterised by dense fibrosis of the thyroid parenchyma, with infiltration of adjacent organs, muscles and neurovascular structures. 1 The exact aetiology is unclear with recent studies suggesting an association with IgG-4 and IgG-4-related systemic disease.1–3 It has an estimated prevalence of 1.06 in 100,000 people and affects women more frequently (1:4), most commonly aged between 30 and 50. 4
Presentations vary but include neck swelling with or without pain, hoarseness of voice and occasionally with obstructive signs such as stridor or dysphagia. 1
Biochemical pictures are mixed and non-specific, with some patients testing positive for anti-thyroglobulin (27%), anti-TPO (43%) and thyrotropin receptor stimulating antibody (20%). Thyroid function tests are also non-specific, with patients presenting primarily euthyroid, but can present with hyper- or hypothyroidism. Some cases of RT also mention parathyroid involvement with hypoparathyroidism and hypocalcemia. Inflammatory markers, such as CRP and ESR, are often raised (>90%). 5 IgG4 has been increasingly associated with RT, with raised levels being described on immunohistochemical staining of histology samples. 2 Raised serum IgG4 levels in RT, however, have not yet been reported.
Imaging alone cannot diagnose RT as its radiological appearance can mimic primary thyroid malignancy and lymphoma. Sonographic findings are those of an ill-defined, hypoechoic and heterogeneous mass with lack of internal vascularity. Extra-thyroid extension to involve adjacent structures (including vessels and the recurrent laryngeal nerve) has also been described, with CT and MRI having utility in further evaluating the local extent of the lesion1 These imaging appearances mimic those of papillary thyroid carcinoma, anaplastic thyroid carcinoma, fibrosing variants of Hashimoto’s thyroiditis, sarcoma and non-Hodgkin’s lymphoma, 1 and will require a core or surgical biopsy for a histological diagnosis. Fine needle aspiration cytology is typically insufficient, due to lack of thyroid follicular cells.1,5 The most common histological finding is fibrous tissue with lymphocyte infiltration, and occasionally occlusive phlebitis, 5 but should importantly contain no giant cells, lymphoid follicles, granulomas or obviously malignant cells. 1 The role of immunohistochemical staining for IgG4 has not yet been established.1,2
The clinical course of RT varies, with some lesions expanding rapidly, or regressing without any intervention. Complications of RT include venous thrombosis, recurrent laryngeal nerve injury, Horner’s syndrome, parathyroid and tracheal invasion, 1 and pseudotumours within the lung, lacrimal gland and orbit, exophthalmos and cholangitis. 2 Some studies postulate RT as part of a spectrum of fibrosclerotic conditions mediated by IgG4; other conditions within this spectrum include (but not limited to) retroperitoneal, pancreatic or mediastinal fibrosis. 3
Treatment is non-standardised and tailored to the patient; options include surgical removal (total or hemithyroidectomy) or medical active (tamoxifen, rituximab or glucocorticoids, typically prednisolone 40 mg for 3 months) or symptomatic treatment (alfacalcidol, levothyroxine).1,5 Surgery is preferably avoided due to technical complexity, as a result of irregular spread, infiltration and extension as mentioned above which can risk substantial postoperative morbidity. RT has a low mortality rate (approximately 1%), with good response to surgical and medical intervention (90% improvement). 5
Conclusion
RT is a difficult condition to diagnose due to rarity, varied presentation and non-specific clinical, biochemical and radiographic findings, and will require a definitive histological diagnosis. It mimics thyroid malignancy, and careful steps are needed not to misdiagnose RT. Fine needle aspiration sampling is often insufficient to diagnose RT, yet ultrasound-guided core biopsy sampling can be a less invasive alternative to open thyroid surgery for the diagnosis and treatment of RT.
Acknowledgments
The authors thank Emily Appleby, the Clinical photography Team, Radiology and ENT department, Eastbourne District General Hospital, for their support and help.
Footnotes
Contributors: Dr Kevin Michell contributed to Criteria 1, 2 and 3. Dr Suzannah Hall contributed to Criteria 1, 2 and 3. Miss Zainab Alshiekh Ali contributed to Criteria 2 and 3. Mr Muhannah Al-Hashim contributed to Criteria 2 and 3. Professor David C Howlett contributed to Criteria 1, 2 and 3.
The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article.
Ethics Approval: This manuscript has been produced in accordance with ethical standards, including written informed consent obtained from the patient for publication of this case report and accompanying images.
Permission from Patient(s) or Subject(s) Obtained in Writing for Publishing Their Case Report: Yes.
Permission Obtained in Writing from Patient or Any Person Whose Photo Is Included for Publishing Their Photographs and Images: Yes.
Confirm that You Are Aware that Permission from a Previous Publisher for Reproducing Any Previously Published Material Will be Required Should Your Article be Accepted for Publication and that You Will be Responsible for Obtaining that Permission: Yes.
Guarantor: Kevin Michell is guarantor of this article.
ORCID iD: Kevin Michell  https://orcid.org/0000-0002-5397-260X
https://orcid.org/0000-0002-5397-260X
References
- 1. Czarnywojtek A, Pietrończyk K, Thompson LDR, et al. IgG4-related sclerosing thyroiditis (Riedel-Struma): a review of clinicopathological features and management. Virchows Archiv 2023; 483: 133–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Dahlgren M, Khosroshahi A, Nielsen GP, et al. Riedel’s thyroiditis and multifocal fibrosclerosis are part of the IgG4-related systemic disease spectrum. Arthritis Care Res 2010; 62: 1312–1318. [DOI] [PubMed] [Google Scholar]
- 3. Katz G, Stone JH. Clinical perspectives on IgG4-related disease and its classification. Ann Rev Med 2022; 73: 545–562. [DOI] [PubMed] [Google Scholar]
- 4. Hay ID. Thyroiditis: a clinical update. Inmayo Clinic Proceedings 1985; 60: 836–843. [DOI] [PubMed] [Google Scholar]
- 5. Zala A, Berhane T, Juhlin CC, et al. Riedel thyroiditis. J Clin Endocrinol Metab 2020; 105: e3469–e3481. [DOI] [PubMed] [Google Scholar]


