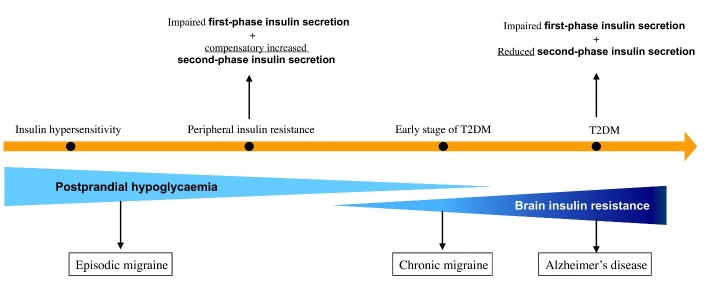
Figure 1.
The “Neuroenergetic hypothesis”: a metabolic bridge between migraine and Alzheimer’s disease (AD). This illustrates the Neuroenergetic Hypothesis that we first described elsewhere [15]. Herein we focused on the “extended Neuroenergetic Hypothesis” as to there being a metabolic bridge between chronic migraine and AD. Conditions that are connected by a continuum of time and pathophysiology are marked by an orange arrow, i.e., insulin hypersensitivity, insulin resistance, early stage of T2DM and T2DM. Both insulin hypersensitivity and peripheral insulin resistance can lead to postprandial hypoglycaemia through different mechanisms. Postprandial hypoglycaemia has been identified as a major contributor to cerebral energy deficiency that underlies episodic migraine. The worsening of glucose metabolism, evidenced by the orange arrow, may extend to the brain over time, leading to brain insulin resistance. Brain insulin resistance generates a chronic mismatch between the energy reserve of the brain and functional expenditure, which is involved in the chronification of migraine and, in the long run, at least in certain subsets of patients, in the prodromic phase of AD, along a putative metabolic physiopathological continuum. T2DM, type 2 diabetes mellitus.