Abstract
Background Fingertip injuries with amputation are one of the common hand injury problems. Several reconstructive options are available for fingertip injury. V-Y advancement flap is one of the common flaps. In some cases, their advancement capacities are not sufficient to cover the whole defect, resulting in flexion deformity of the distal interphalangeal (DIP) joint, loss of finger pulp shape, or hooked deformity. The double V-Y flap consists of harvesting two cutaneous flaps on the same neurovascular digital palmar bundle. The first V-Y flap is raised as a neurovascular flap and the second flap is an advancement V-Y plasty.
Objective This article evaluates the outcomes of the double V-Y advancement flap for the fingertip reconstruction.
Materials and Methods This is a prospective study on 19 patients with zone II and III fingertip amputation tip defects between December 2021 and June 2023. The majority were workplace injuries.
Results There were 16 males and 3 females. The average static two-point discrimination was 6 mm. Average advancement of first flap is 8.5 mm and the average advancement of second flap is 4.3 mm. The average total advancement of a double V-Y flap is 12.94 mm (10–15 mm). All of them had “good” total active motion with movement > 210. One patient had flexion deformity at the DIP joint without causing any functional disturbance. All the flaps settled well except for one patient who had superficial partial necrosis of flap which was managed conservatively.
Conclusion This is simple and safe for the reconstruction of zone II and III fingertip amputations with the advantage of like-for-like tissue with near-normal sensation. The second flap increased the advancement of the proximal flap, restoring the pulp shape, and thereby reconstructing a functional and aesthetic fingertip.
Keywords: double V-Y flap, flap-in-flap, fingertip injury, hand injury, fingertip reconstruction
Introduction
Fingertip injuries pose a common problem as the most frequent type of hand injury, 1 with fingertip amputations being a prevalent form of upper extremity amputations. 2 The primary objective of fingertip reconstruction is to achieve a pain-free, sensate, stable palmar skin, and a cosmetically acceptable fingertip. 3 When dealing with fingertip amputations, there is no established gold standard treatment, and various options exist, including conservative approaches, shortening closure, and different flaps, such as homo/hetero digital flaps and toe pulp transfers, for pulp reconstruction. 4 5 The selection of the flap is influenced by considerations such as the level, extent, and orientation of the pulp defect.
The V-Y advancement flap, initially introduced by Tranquilli-Leali 6 in 1935 and subsequently popularized by Atasoy 7 in 1970, continues to be a well-established technique, even though its range of motion is confined to 10 mm. 8 In cases where the defect exceeds 1 cm, anterograde homodigital neurovascular island flaps are proven to be highly beneficial. 9 Nevertheless, these flaps necessitate extensive dissection of the neurovascular pedicle to its common palmar digital artery, and tension on the pedicle during inset may result in stiffness of the proximal interphalangeal joint (PIPJ). 10 11 To overcome these problems, we used the second flap within the Tranquilli-Leali neurovascular island flap to increase the mobility of the flap without causing any interphalangeal (IP) joint stiffness. The aim of our study was to assess the various outcomes of the “flap-in-flap technique”—double V-Y flap in fingertip injury management.
Materials and Method
The study was conducted in the department of plastic surgery at a tertiary care hospital between December 2021 and June 2023 on all the patients who were received in the emergency room or plastic surgery outpatient department with transverse, palmar, and dorsal oblique amputation fingertip injury. Written informed consent was taken from all the patients. Institutional ethical committee clearance was obtained. Evans and Bernardis 12 PNB (pulp, nail, bone) classification system was used for classifying fingertip injuries in our study. Patients who had fingertip injury with doubtful vascularity of the pulp skin, fingers with previous neurovascular bundle (NVB) injury, and injury proximal to the lunula were excluded from the study.
Operative Technique
The technique of “flap-in-flap” (double V-Y flap) entails harvesting two flaps nourished by the same proper palmar digital vessels ( Fig. 1 ). All the cases were done under the digital block. After debridement and wound wash, the proximal or first flap can be marked as a standard V-Y pattern or oblique V-Y pattern depending on the defect orientation and size ( Fig. 4A ). All our cases are elevated as bilateral neurovascular Tranquilli-Leali 13 V-Y flap and if required we extend the apex of the first V-Y flap proximal to the distal IP joint (DIPJ) crease. The flap is raised and islanded, keeping the NVB intact. After elevation of the flap, if there is difficulty in complete inset of the flap without tension at the suture line or requires flexion of IP joints for easy inset, a second flap (V-shaped) is designed within the proximal flap (not exceeding 50% size of the first flap) ( Fig. 2B ). The second flap is elevated through a full-thickness skin incision until the subcutaneous fat tissue pops out, thereby separating the two skin paddles that remain interconnected by fatty tissue containing the neurovascular structures, ensuring their vascularity is preserved ( Fig. 2D ). The inset was given using 3–0 ethilon in such a way that the second flap covers the distal fingertip, while the proximal flap addresses the palmar defect, maintaining the IP joints in full extension ( Fig. 2E ). The resultant raw area due to the advancement of the first flap closed as Y and the resultant raw area between the flap, due to the advancement of the second flap, is allowed to heal by secondary intention. Sterile dressing applied. Sutures were removed after 2 weeks and finger mobilization exercises started once the wound settled well. All the patients were followed up for a minimum period of 6 months.
Fig. 1.
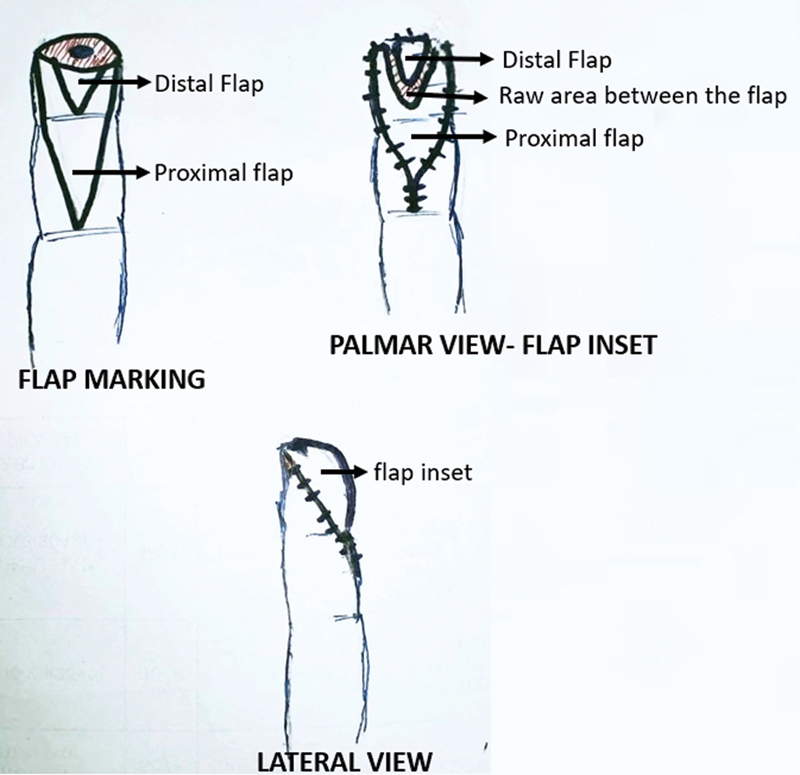
Schematic diagram double V-Y flap.
Fig. 4.
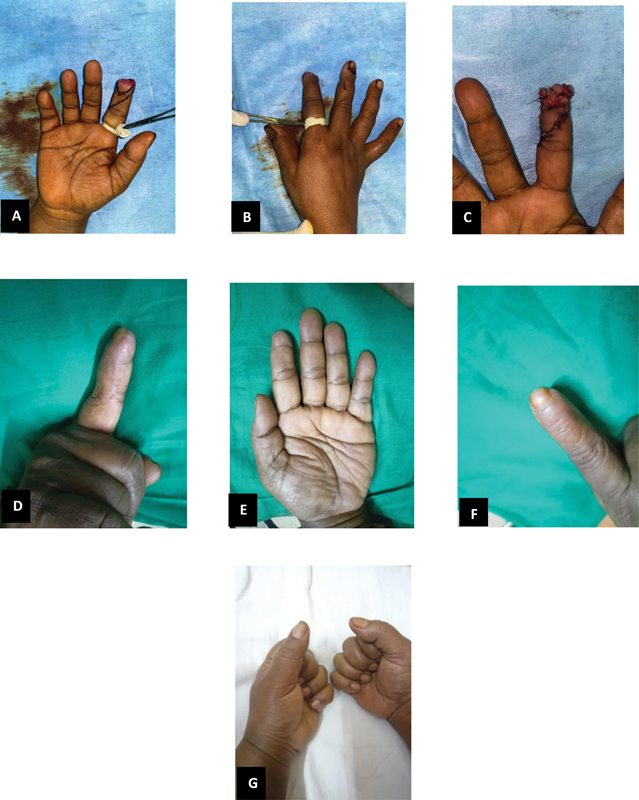
Right index fingertip Injury (P3N5B6) with type II Allen's amputation classification. ( A ) Double V-Y flap marking (palmar view). ( B ) Preop dorsal view. ( C ) Flap inset palmar view. ( D ) Late postop: lateral view showing excellent pulp shape with no distal interphalangeal (DIP) joint flexion deformity. ( E ) Well-settled flap with an inconspicuous flap scar. ( F ) Late postop dorsal view. ( G ) Late postop with a full range of motion of the injured finger.
Fig. 2.
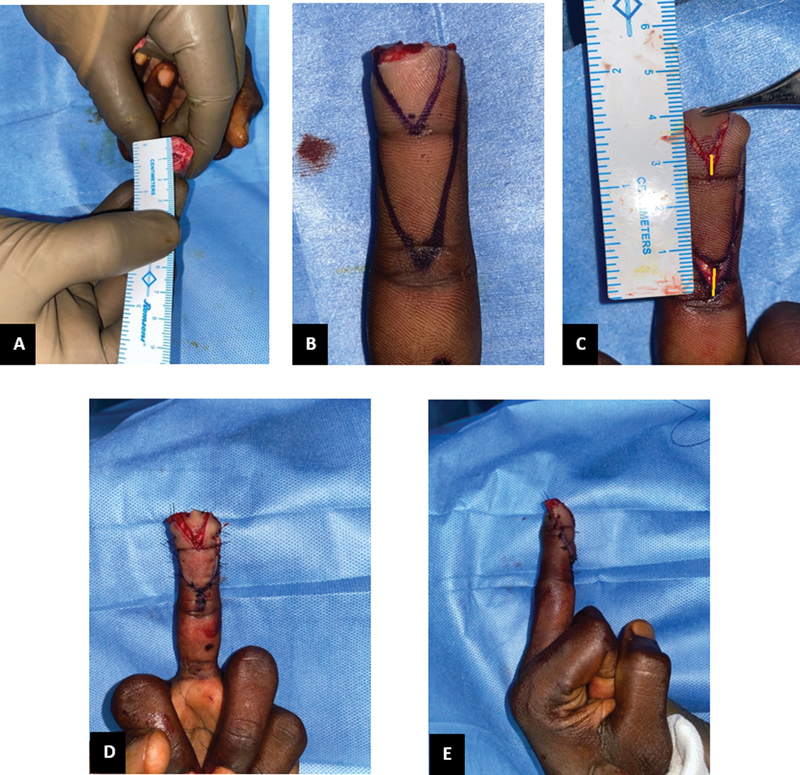
( A ) Transverse amputation raw area measuring 1.5 cm with exposing distal phalanx (DPX) bone stump. ( B ) Double V-Y flap marking. ( C ) Measurement of the advancement produced by both proximal and distal flap (marked as a yellow solid line). ( D ) Flap inset palmar view. ( E ) Flap inset lateral view, the interphalangeal joints are maintained in full extension.
They were assessed for the flexion deformity of the DIPJ, amount of advancement of the flap, static two-point discrimination (S2PD), aesthetically acceptable smooth contouring of pulp shape, and total active motion (TAM) for full functional recovery of an injured finger.
Parameters assessed : The aesthetic evaluation of the fingertip pulp shape was based on Bakhach et al 14 as follows:
Excellent : Characterized by a normal and soft pulp that extends beyond the nail edge.
Good : Involves a retracted and scarred pulp with a typical pulp shape covered by the nail.
Poor : Describes a dystrophic and painful fingertip.
Finger motion was assessed using TAM at the metacarpophalangeal joint, PIPJ, and DIPJ which was calculated, and the results were categorized into three grades using the method of Pun et al 15 as good = > 210 degrees, fair = 180 to 210 degrees, and poor = < 180 degrees.
The amount of advancement of the proximal flap is measured from the length of the Y limb. The amount of advancement of the second flap is measured from the length of the raw area between the flap in the midline ( Fig. 2C ).
The evaluation of fingertip pulp sensation was conducted through S2PD. The S2PD test was performed on the entire skin flaps, including both the proximal and second flaps. The practical difficulty of conducting this test individually on each flap was encountered due to their size limitations.
Results
A total of 19 patients were included, of which 16 (84.2%) were males and 3 (15.7%) were females. The mean age was 32 years (20–50 years). The majority were workplace injuries 17 (89.4%) and 2 (10.6%) were domestic accidents. Index finger was injured in 7 (36.8%), middle finger in 5 (26.3%), ring finger in 3 (15.7%), little finger in 3 (15.7%), and thumb in 1 (5%) patients ( Table 1 ). All our cases were either type II or type III fingertip amputation according to Allen's classification. 16 The results of fingertip injury according to the PNB classification are charted in Table 2 .
Table 1. Summary of patient details.
| Sl. no | Age | Side | Finger | PNB classification | Dominant | Procedure | Mode of injury | Complications |
|---|---|---|---|---|---|---|---|---|
| 1 | 40 | Left | Index | P5N5B5 | Right | B/L NV islanded V-Y advancement flap | Work | Nil |
| 2 | 23 | Left | Middle | P6N5B5 | Right | B/L NV islanded V-Y advancement flap | Work | Nil |
| 3 | 39 | Right | Index | P4N5B5 | Right | B/L NV islanded V-Y advancement flap | Work | Superficial skin necrosis and flexion deformity at DIPJ |
| 4 | 24 | Left | Index | P4N3B5 | Right | B/L NV islanded V-Y advancement flap | Work | Nil |
| 5 | 32 | Left | Ring | P6N5B6 | Right | B/L NV islanded V-Y advancement flap | Work | Nil |
| 6 | 25 | Left | Ring | P4N7B0 | Right | B/L NV islanded V-Y advancement flap | Work | Nil |
| 7 | 26 | Right | Middle | P3N5B5 | Right | B/L NV islanded V-Y advancement flap | Work | Nil |
| 8 | 30 | Right | Middle | P4N5B5 | Right | B/L NV islanded V-Y advancement flap | Work | Nil |
| 9 | 35 | Left | Little | P3N5B5 | Right | B/L NV islanded V-Y advancement flap | Work | Nil |
| 10 | 21 | Right | Little | P3N6B6 | Right | B/L NV islanded V-Y advancement flap | Work | Nil |
| 11 | 42 | Left | Ring | P4N5B5 | Right | B/L NV islanded V-Y advancement flap | Home | Nil |
| 12 | 28 | Right | Index | P3N5B6 | Right | B/L NV islanded V-Y advancement flap | Work | Nil |
| 13 | 34 | Left | Middle | P3N5B6 | Right | B/L NV islanded V-Y advancement flap | Work | Nil |
| 14 | 20 | Right | Index | P5N5B5 | Right | B/L NV islanded V-Y advancement flap | Home | Nil |
| 15 | 50 | Right | Little | P3N5B5 | Right | B/L NV islanded V-Y advancement flap | Work | Nil |
| 16 | 34 | Right | Index | P3N5B5 | Right | B/L NV islanded V-Y advancement flap | Work | Nil |
| 17 | 21 | Right | Middle | P3N6B6 | Right | B/L NV islanded V-Y advancement flap | Work | Nil |
| 18 | 45 | Right | Thumb | P3N5B5 | Right | B/L NV islanded V-Y advancement flap | Work | Nil |
| 19 | 40 | Left | Index | P5N5B5 | Right | B/L NV islanded V-Y advancement flap | Work | Nil |
Abbreviations: B/L, NV, bilateral neurovascular; DIPJ, distal interphalangeal; PNB classification, pulp, nail, and bone classification.
Table 2. PNB classification results.
| PNB | No. of patient |
|---|---|
| P ulp | P3 - 9 (47.3%) |
| P4 - 5 (26.3%) | |
| P5 - 3 (15.7%) | |
| P6 - 2 (10.5%) | |
| N ail | N5 - 15 (78.9%) |
| N6 - 2 (10.5%) | |
| N7 - 1 (5%) | |
| N3 - 1 (5%) | |
| B one | B5 - 13 (68.4%) |
| B6 - 5 (26.3%) | |
| B0 - 1 (5%) |
All the flaps settled well except for one patient, who had superficial necrosis of the distal flap which was managed conservatively without requiring another procedure ( Fig. 4E ). One patient had flexion deformity at DIPJ with no functional disability.
S2PD ranges from 4 to 9 mm with an average of approximately 6.3 mm. This was performed on the whole of the reconstructed flaps (proximal and second flaps). It was difficult to conduct the tests on each flap separately because of their size constraints.
As far as the fingertip pulp shape is concerned, 16 patients (84.2%) had an “excellent” score ( Figs. 3E and 4D ). Three patients (15.7%) had a “good” score.
Fig. 3.
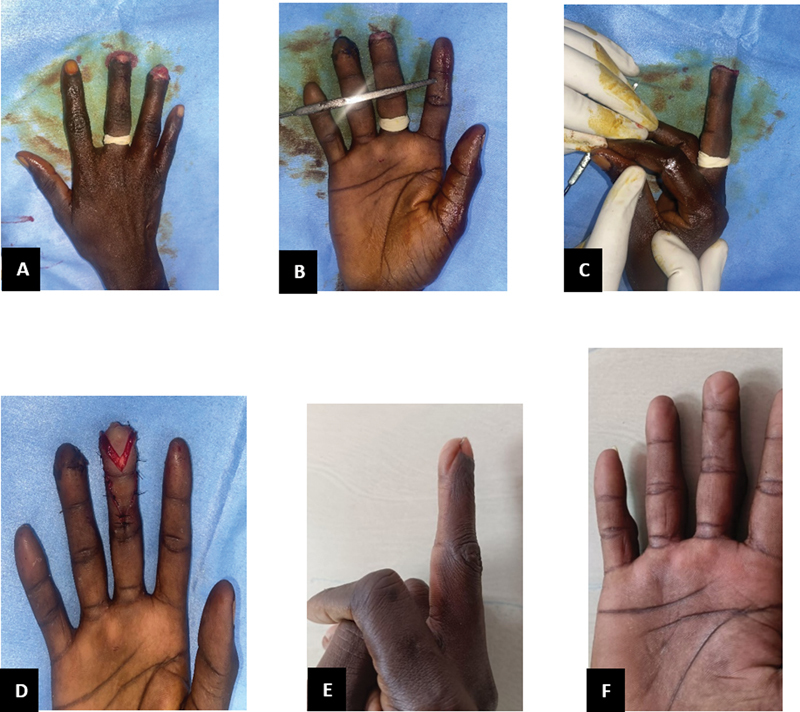
Right middle fingertip injury (P3N5B5) with type II Allen's amputation classification. ( A ) Preop dorsal view. ( B ) Preop palmar view. ( C ) Preop lateral view. ( D ) Flap inset palmar view shows good advancement produced by the second flap. ( E ) Late postop showing excellent pulp shape with no distal interphalangeal (DIP) joint flexion deformity. ( F ) Late postop palmar view showing a well-settled flap.
The average advancement of the first flap was 8.6 mm (range 6–10 mm) and the average advancement of the second flap was 4.3 mm (range 3–5 mm). The average total advancement of a double V-Y flap was 12.94 mm (range 10–15 mm) ( Table 3 ).
Table 3. Results of various parameters assessed.
| Sl. no | Age | Side | Finger | PNB classification |
Static 2 PD (mm) |
Pulp shape and size | Advancement of first flap (mm) | Advancement of second flap (mm) | Total advancement length (mm) |
TAM score (degree) |
TAM grade |
||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MCPJ | PIPJ | DIPJ | |||||||||||
| 1 | 40 | Left | Index | P5N5B5 | 6 | Excellent | 8 | 3 | 11 | 0–90 | 0–98 | 0–65 | Good |
| 2 | 23 | Left | Middle | P6N5B5 | 5 | Excellent | 9 | 5 | 14 | 0–87 | 0–95 | 0–70 | Good |
| 3 | 39 | Right | Index | P4N5B5 | 7 | Excellent | 10 | 5 | 15 | 0–85 | 0–90 | 8–60 | Good |
| 4 | 24 | Left | Index | P4N3B5 | 8 | Excellent | 9 | 4 | 13 | 0–87 | 0–100 | 0–68 | Good |
| 5 | 32 | Left | Ring | P6N5B6 | 7 | Excellent | 8 | 3 | 11 | 0–88 | 0–96 | 0–65 | Good |
| 6 | 25 | Left | Ring | P4N7B0 | 8 | Good | 9 | 4 | 13 | 0–87 | 0–97 | 0–66 | Good |
| 7 | 26 | Right | Middle | P3N5B5 | 5 | Excellent | 10 | 5 | 15 | 0–90 | 0–90 | 0–69 | Good |
| 8 | 30 | Right | Middle | P4N5B5 | 7 | Good | 7 | 5 | 12 | 0–83 | 0–98 | 0–70 | Good |
| 9 | 35 | Left | Little | P3N5B5 | 5 | Excellent | 9 | 4 | 13 | 0–85 | 0–97 | 0–62 | Good |
| 10 | 21 | Right | Little | P3N6B6 | 6 | Excellent | 6 | 4 | 10 | 0–88 | 0–95 | 0–64 | Good |
| 11 | 42 | Left | Ring | P4N5B5 | 8 | Excellent | 9 | 5 | 14 | 0–84 | 0–93 | 0–65 | Good |
| 12 | 28 | Right | Index | P3N5B6 | 7 | Excellent | 10 | 4 | 14 | 0–87 | 0–95 | 0–68 | Good |
| 13 | 34 | Left | Middle | P3N5B6 | 4 | Excellent | 7 | 5 | 12 | 0–85 | 0–98 | 0–63 | Good |
| 14 | 20 | Right | Index | P5N5B5 | 6 | Excellent | 9 | 5 | 14 | 0–88 | 0–99 | 0–66 | Good |
| 15 | 50 | Right | Little | P3N5B5 | 5 | Good | 8 | 4 | 12 | 0–90 | 0–95 | 0–65 | Good |
| 16 | 34 | Right | Index | P3N5B5 | 6 | Excellent | 10 | 5 | 15 | 0–89 | 0–96 | 0–70 | Good |
| 17 | 21 | Right | Middle | P3N6B6 | 5 | Excellent | 9 | 5 | 14 | 0–85 | 0–96 | 0–65 | Good |
| 18 | 45 | Right | Thumb | P3N5B5 | 9 | Excellent | 8 | 4 | 12 | NA | NA | NA | Good |
| 19 | 40 | Left | Index | P5N5B5 | 7 | Excellent | 9 | 3 | 12 | 0–85 | 0–100 | 0–68 | Good |
Abbreviations: DIPJ, distal interphalangeal; MCPJ, metacarpophalangeal joint; PIPJ, proximal interphalangeal joint; PNB classification, pulp, nail, and bone classification; TAM, total active motion.
Concerning the functional movement of fingers, all of them had good TAM grades with movement > 210 degrees ( Fig. 4G ). Though one patient had flexion deformity at the DIPJ of 8 degrees, it did not cause any functional or aesthetically unacceptable fingertip.
Discussion
Fingertip injuries are common hand injuries with various reconstructive options available. When covering defects larger than 1 cm, the reconstructive flap may fail to reach the distal nail bed, especially with an extended finger position. This can result in a tight inset of the flap, impacting flap survival, or causing progressive flexion at the IP joints. To facilitate easier coverage of the defects, IP joints are flexed to advance the flap distally. Despite the application of physiotherapy or orthosis, residual PIPJ stiffness is observed in 15% of cases. 17 To overcome these problems, we used the second (double V-Y) flap harvested from the first flap to cover the distal fingertip which did not require flexion at the IP joint.
In the study by Chakraborty et al 18 in which the Atasoy flap group, the passive range of motion at the DIPJ was affected significantly in comparison to control fingers. However, in our series, the passive range of motion at the DIPJ was not affected. This could be because the second flap helped with the tensionless inset with no IP joint flexion deformity.
A study by Estoppey et al 19 had a mean flexion deformity at the DIPJ of 6.8 degrees with slightly reduced DIPJ mobility but preserved PIPJ mobility with no significant flexion deformity. In another study by Lok et al 20 5 of 11 patients had flexion deformity at the DIPJ. In our study, only one patient had flexion deformity at the DIPJ of 8 degrees ( Fig. 5 ) and none of them had any functional deficit.
Fig. 5.

Flexion deformity at distal interphalangeal (DIP) joint.
In our study, the mean S2PD was 6 mm, comparable to the study conducted by Barbato et al, 21 in which they reported S2PD of 6.5 mm in their series of 20 patients. The S2PD results closely resembled those found in clinical series where only one flap was utilized for pulp reconstruction, as seen in studies. 22 To put it differently, the inclusion of a second V-Y flap on the same neurovascular pedicle did not disrupt the recovery of pulp sensitivity.
The aesthetic outcome in the form of pulp volume and sagittal curved shape of pulp in our series has scored:
_ “Excellent” in 79% of the patients with the majority of them in the transverse amputation group.
_ “Good” in 4 (21%) patients, of which 3 of them belong to palmar oblique amputation (P4). Out of 5 palmar oblique amputations, only 3 of them (60%) had a “good” aesthetic score, indicating cautious use of double V-Y flap in the volar oblique amputation group.
In our series, the mean advancement of the second flap is 4.3 mm (range 3–5 mm), which was comparable with the study conducted by Bakhach et al and Díaz et al 23 in which the average advancement of the second flap was 4.3 and 4.2 mm, respectively. This second flap helped to increase the mobility by 30 to 50% and avoided any IP joint stiffness. This was substantiated by a cadaveric study in which the advancement produced by the single and double V-Y plasty was 15.8 and 18.6 mm, respectively. 24
In our study, one patient had flexion deformity at the DIPJ with no functional deficit. It occurred in a patient who suffered from a large palmar-oblique pulp defect (P4) with an advancement length of 15 mm. This again indicates the cautious use of a double V-Y flap in the palmar oblique amputation fingertip injuries.
Conclusion
The “flap-in-flap” technique uses a double V-Y flap for fingertip reconstruction, maintaining near-normal sensation and aesthetically acceptable pulp shape. It covers defects up to 15 mm, promoting full functional recovery without residual joint stiffness.
Footnotes
Conflict of Interest None declared.
References
- 1.Giesen T, Adani R, Carmes S, Dumontier C, Elliot D, Calcagni M. IFSSH Scientific Committee on skin coverage: 2015 report. Hand Surg Rehabil. 2016;35(05):307–319. doi: 10.1016/j.hansur.2016.07.005. [DOI] [PubMed] [Google Scholar]
- 2.Pomares G, Coudane H, Dap F, Dautel G. Epidemiology of traumatic upper limb amputations. Orthop Traumatol Surg Res. 2018;104(02):273–276. doi: 10.1016/j.otsr.2017.12.014. [DOI] [PubMed] [Google Scholar]
- 3.Martin C, González del Pino J. Controversies in the treatment of fingertip amputations. Conservative versus surgical reconstruction. Clin Orthop Relat Res. 1998;(353):63–73. doi: 10.1097/00003086-199808000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Quell M, Neubauer T, Wagner M. Treatment of fingertip defect injuries with a semi-occlusive dressing [in German] Handchir Mikrochir Plast Chir. 1998;30(01):24–29. [PubMed] [Google Scholar]
- 5.Guelmi K, Barbato B, Maladry D, Mitz V, Lemerle J P. Reconstruction of digital pulp by pulp tissue transfer of the toe. Apropos of 15 cases [in French] Rev Chir Orthop Repar Appar Mot. 1996;82:446–452. [PubMed] [Google Scholar]
- 6.Tranquilli-Leali E. Ricostruzione dell'apice delle falangi ungueali mediante autoplastica volare peduncolata per scormento. Infort Traumatol Lav. 1935;1:186–193. [Google Scholar]
- 7.Atasoy E, Ioakimidis E, Kasdan M L, Kutz J E, Kleinert H E. Reconstruction of the amputated fingertip with a triangular volar flap. J Bone Joint Surg Am. 1970;52(05):921–926. [PubMed] [Google Scholar]
- 8.Lim J X, Chung K C. VY advancement, thenar flap, and cross-finger flaps. Hand Clin. 2020;36(01):19–32. doi: 10.1016/j.hcl.2019.08.003. [DOI] [PubMed] [Google Scholar]
- 9.Evans D M, Martin D L. Step-advancement island flap for fingertip reconstruction. Br J Plast Surg. 1988;41(02):105–111. doi: 10.1016/0007-1226(88)90035-5. [DOI] [PubMed] [Google Scholar]
- 10.Arsalan-Werner A, Brui N, Mehling I, Schlageter M, Sauerbier M. Long-term outcome of fingertip reconstruction with the homodigital neurovascular island flap. Arch Orthop Trauma Surg. 2019;139(08):1171–1178. doi: 10.1007/s00402-019-03198-4. [DOI] [PubMed] [Google Scholar]
- 11.Kayalar M, Bal E, Toros T, Süğün S T, Özaksar K, Gürbüz Y. The outcome of direct-flow neurovascular island flaps in pulp defects. Acta Orthop Traumatol Turc. 2011;45(03):175–184. doi: 10.3944/AOTT.2011.2429. [DOI] [PubMed] [Google Scholar]
- 12.Evans D M, Bernardis C. A new classification for fingertip injuries. J Hand Surg [Br] 2000;25(01):58–60. doi: 10.1054/jhsb.1999.0305. [DOI] [PubMed] [Google Scholar]
- 13.Elliot D, Moiemen N S, Jigjinni V S. The neurovascular Tranquilli-Leali flap. J Hand Surg [Br] 1995;20(06):815–823. doi: 10.1016/s0266-7681(95)80055-7. [DOI] [PubMed] [Google Scholar]
- 14.Bakhach J, Guimberteau J C, Panconi B. The Gigogne flap: an original technique for an optimal pulp reconstruction. J Hand Surg Eur Vol. 2009;34(02):227–234. doi: 10.1177/1753193408098904. [DOI] [PubMed] [Google Scholar]
- 15.Pun W K, Chow S P, So Y C et al. Unstable phalangeal fractures: treatment by A.O. screw and plate fixation. J Hand Surg Am. 1991;16(01):113–117. doi: 10.1016/s0363-5023(10)80023-1. [DOI] [PubMed] [Google Scholar]
- 16.Allen M J. Conservative management of finger tip injuries in adults. Hand. 1980;12(03):257–265. doi: 10.1016/s0072-968x(80)80049-0. [DOI] [PubMed] [Google Scholar]
- 17.Foucher G, Smith D, Pempinello C, Braun F M, Citron N. Homodigital neurovascular island flaps for digital pulp loss. J Hand Surg [Br] 1989;14(02):204–208. doi: 10.1016/0266-7681_89_90127-7. [DOI] [PubMed] [Google Scholar]
- 18.Chakraborty S S, Kala P C, Sahu R K, Dixit P K, Katrolia D, Kotu S. Fingertip amputation reconstruction with VY advancement flap: literature review and comparative analysis of Atasoy and Kutler flaps. World J Plast Surg. 2021;10(03):8–17. doi: 10.29252/wjps.10.3.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Estoppey D, Pomares G, Jager T. Long-term outcome of a “short” anterograde homodigital neurovascular island flap with a simple or double V-Y plasty. Orthop Traumatol Surg Res. 2021;107(05):102981. doi: 10.1016/j.otsr.2021.102981. [DOI] [PubMed] [Google Scholar]
- 20.Lok L-W, Chan W-L, Lau Y-K. Functional outcomes of antegrade homo-digital neurovascular island flaps for fingertip amputation. J Hand Surg Asian Pac Vol. 2017;22(01):39–45. doi: 10.1142/S0218810417500071. [DOI] [PubMed] [Google Scholar]
- 21.Barbato B D, Guelmi K, Romano S J, Mitz V, Lemerle J P. Thenar flap rehabilitated: a review of 20 cases. Ann Plast Surg. 1996;37(02):135–139. doi: 10.1097/00000637-199608000-00003. [DOI] [PubMed] [Google Scholar]
- 22.Tupper J, Miller G. Sensitivity following volar V-Y plasty for fingertip amputations. J Hand Surg [Br] 1985;10(02):183–184. doi: 10.1016/0266-7681(85)90011-7. [DOI] [PubMed] [Google Scholar]
- 23.Díaz L C, Vergara-Amador E, Fuentes Losada L M. Double V-Y flap to cover the fingertip injury: new technique and cases. Tech Hand Up Extrem Surg. 2016;20(04):133–136. doi: 10.1097/BTH.0000000000000132. [DOI] [PubMed] [Google Scholar]
- 24.Jager T, Mussi J-P, Pomares G. Optimization of the homodigital antegrade island flap for fingertip reconstruction: new dissection sequence based on cadaver study findings. Orthop Traumatol Surg Res. 2020;106(02):335–339. doi: 10.1016/j.otsr.2020.01.002. [DOI] [PubMed] [Google Scholar]


