Abstract
Ganglioneuromas (GN) are benign, slow-growing, non-invasive, and well differentiated neoplasms of neuroblastic origin. We reported a 4 year old girl who presented with a left lateral slow growing cervical neck mass. After surgical excision the tumour was sent for histopathological examination which confirmed ganglioneuroma. Ganglioneuromas should be accounted as the differential diagnosis of pediatric soft tissue tumours of the neck.
Keywords: Ganglioneuroma, Neuroblastoma, Benign cervical masses, Transcervical approach
Introduction
Ganglioneuromas (GN) are rare benign, well differentiated, and non-invasive tumours that arise mainly from neural crest cells of paraspinal sympathetic chain ganglia most commonly occur in the trunk; however,1–5% occur in the head and neck [1]. GNs are usually asymptomatic and in cervical region the symptoms usually stem from mass effect of enlarging size of tumour and nerve dysfunction over a long duration [2, 3].
Complete surgical excision and biopsy is considered the treatment of choice for this benign tumour, which is challenging in the cervical region due to its proximity to neurovascular structures [4]. In this report, we present a case of a 4-year-old girl with a history of enlarging neck mass.
Case Report
A 4 year girl came to the SMGS Hospital Jammu, got admitted in our department with 1 year and 5 month history of enlarging mass in the left lateral side of neck which was gradually increasing in size. There was no history of any discharging sinus, dysphonia, respiratory difficulties, dysphagia, referred otalgia and weight loss. On examination, it was large, well circumscribed single globular mass approximately (5 × 4 × 4 cm) size extending from midline of neck to left anterior border of trapezius, superiorly extending to hyoid bone and inferiorly to clavicle with overlying skin normal. Cranial nerve examination was normal. No lymphadenopathy was found.
Materials and Methods
Routine baseline laboratory investigations were normal. Blood and urine results were negative for by-products of sympathetic response, including vanillylmandelic acid and hydroxymandelic acid. Fine needle aspiration cytology of left cervical swelling was inconclusive.
CECT neck showed large well circumscribed globular heterogeneously enhancing soft tissue density mass lesion 65 × 52 × 46 mm (cc×tr×ap) seen in left supraclavicular region which was extending from C3 to D3 level and was compressing and displacing the left common carotid artery and internal jugular vein suggesting neoplastic lesion.
After all preliminary investigation, wedge biopsy of the cervical swelling was taken and sent for histo-pathological examination which showed Ganglioneuroma. Complete surgical excisional biopsy was planned. Written informed consent was obtained from the parents of the patient. Preoperative counselling regarding nerve injuries was done (See Figs. 1 and 2).
Fig. 1.

Preoperative picture of patient showing extent of neck mass
Fig. 2.

Tumour relations to surrounding structures
Under general anaesthesia, a transcervical approach was used to excise the tumour. A single transverse incision was given in the alignment of skin crease that was extending from the midline of neck to the anterior border of trapezius muscle. The subcutaneous tissue and sub-platysmal flaps were dissected and retracted. On examination, single, large globular, tumour was found beneath the sternocleidomastoid muscle in the left lateral aspect of neck. The careful blunt dissection, the anterior, posterior, and medial margins of the mass were dissected meticulously from the contents of the neck. The vagus nerve, the spinal accessory and hypoglossal nerves were identified and preserved. The internal jugular vein and the common carotid artery which were displaced by the tumour were retracted and also preserved. The excised mass was sent for histopathological examination (See Figs. 3 and 4).
Fig. 3.

Excised tumour specimen
Fig. 4.
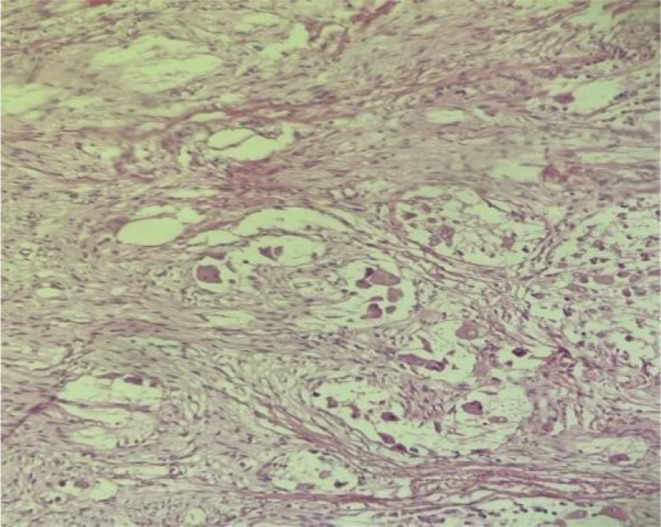
Showing singly scattered as well as nest of mature ganglion cells having abundant granular eosinophilic cytoplasm, eccentric-nuclei and prominent single nucleoli
Histopathological examination confirmed Ganglio-neuroma. The operation was successful, and the postoperative period was uneventful. No other cranial neuropathies were observed. On three consecutive follow-up period which were one month apart, patient was stable and had no significant co-morbidity.
Discussion
The first report of ganglioneuroma located in the neck was made in 1899 by de Quervain. GNs typically occur in the thoracic cavity (60–80%, posterior mediastinum), the cervical region (5%). [5, 6]. Most frequent origin in the neck region is the cervical sympathetic chain, but it can also be located in the larynx, pharynx, and ganglion nodosum of the vagus nerve [7]. Most common extracranial solid tumours of childhood arising from primitive sympathetic ganglion are referred collectively as neuroblastic tumours. Ganglioneuroma, together with ganglioneuroblastomas (intermixed and nodular) and neuroblastomas, are the three recognized types of neuroblastic tumours called peripheral neuroblastic tumours [8, 9].
Imaging is crucial not only in the differential diagnosis of the neck mass but also to plan surgery.
As FNAC was inconclusive therefore wedge biopsy of the neck mass was obtained in our case.
Definite histopathology is required to know the exact nature of tumour and plan regarding the excision of the tumour. The diagnosis of GN was confirmed on histopathological examination of excised specimen. Surgical resection of these tumors is the gold standard treatment. In our case, a transcervical approach was used, however, transoral, transparotid, transcervical-transpharyngeal, and infratemporal fossa approach can also be used depending on the location, size, and pathological type. The relation of tumour to surrounding great vessels and vagus nerve should be carefully evaluated intraoperatively to preserve them. Differential diagnosis usually includes branchial cysts, carotid body tumor, cystic hygroma, tubercular adenitis, pharyngeal diverticulum and lymphoma. Other complications of surgery include vagal nerve paresis/palsy and hypoglossal nerve paresis/palsy. Recurrences have not been reported in the literature following complete excision of the tumour. However, long-term follow-up is required to diagnose delayed recurrences.
Conclusion
Cervical Ganglioneuroma although very rare entity should be accounted as the differential diagnosis of pediatric soft tissue tumours of the neck. Definite histopathology is required to know the exact nature of tumour and plan regarding the excision of the tumour. Complete surgical excision is the gold standard of treatment and histopathological examination of excised specimen is the only way to confirm the diagnosis.
Funding
None.
Declarations
Informed Consent
A written informed consent was taken from the parents of patient in the study.
Conflict of Interest
There are no potential conflicts of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Leeson MC, Hite M (1989) Ganglioneuroma of the sacrum. Clin Orthop Relat Res 246:102–105 [PubMed] [Google Scholar] [PubMed] [Google Scholar]
- 2.Xu T, Zhu W, Wang P (2019) Cervical ganglioneuroma a case report and review of literature. Med (Baltim) 98:e15203 [Crossref] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Helal AA, Badawy R, Mahfouz M, Hussien Tharwat. Adjacent cervical ganglioneuromas. J Pediatr Surg Case Rep 2018 July; 34: 7–9
- 4.Urata S, Yoshida M, Ebihara Y, Asakage T (2013) Surgical management of a giant cervical ganglioneuroma. Auris Nasus Larynx 40:577–580 [DOI] [PubMed] [Google Scholar]
- 5.Califano L, Zupi A, Mangone GM et al (2001) Cervical ganglioneuroma report of a case. Otolaryngol Head Neck Surg 124:115–116 [DOI] [PubMed] [Google Scholar]
- 6.Albonico G, Pellegrino G, Maisano M et al (2001) Ganglioneuroma of parapharyngeal region. Arch Pathol Lab Med 125:1217–1278 [DOI] [PubMed] [Google Scholar]
- 7.Kaufman MR, Rhee JS, Fliegelman LJ, Costantino PD (2001) Ganglioneuroma of the parapharyngeal space in a pediatric patient. Otolaryngol Head Neck Surg 124:702–704 [DOI] [PubMed] [Google Scholar]
- 8.Shimada H, Ambros IM, Dehner LP, Hata J, Joshi VV, Roald B (1999) Terminology and morphologic criteria of neuroblastic tumors: recommendations by the International Neuroblastoma Pathology Committee. Cancer 86(2):349–363 [PubMed] [Google Scholar]
- 9.He WG, Yan Y, Tang W, Cai R, Ren G (2017) Clinical and biological features of neuroblastic tumors: a comparison of neuroblastoma and ganglioneuroblastoma. Oncotarget 8(23):37730–37739. 10.18632/oncotarget.17146 [DOI] [PMC free article] [PubMed] [Google Scholar]


