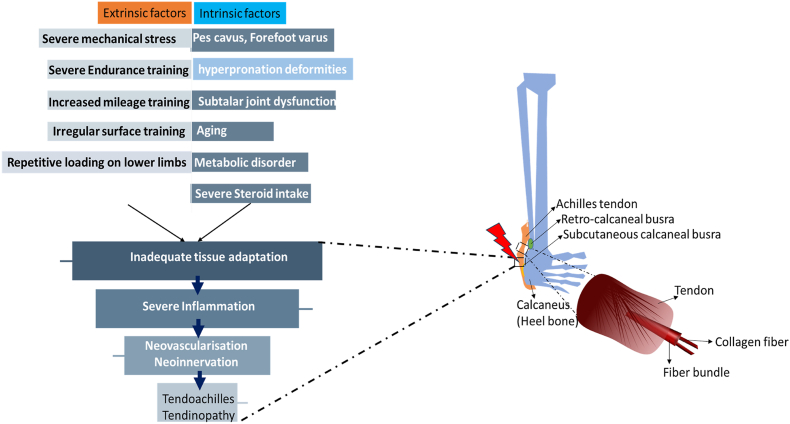
Fig 1.
Achilles tendons are subjected to mechanical forces continuously throughout an individual's life. When these forces are of sufficient intensity, such as during physical activity, they can confer various health benefits not only to the tendons but also to the entire musculoskeletal system. Risk factors for Achilles tendon (AT) injuries can be divided into intrinsic and extrinsic categories, which can occur either in isolation or in combination. Intrinsic factors include biomechanical irregularities of the lower limbs. Examples of these irregularities are indifferent leg length, hyperpronation; other irregularities include pes cavus (high arches), forefoot varus deformity, and limited mobility of the subtalar joint. Additionally, systemic conditions like those associated with advanced age, metabolic syndrome, and the use of specific medications, such as corticosteroids, contribute to intrinsic risk factors. Extrinsic factors involve excessive mechanical stress and poor training practices. These include increased interval training, augmented mileage, training on uneven surfaces, repeated loading, and inadequate shock absorption. Achilles tendinopathy typically features a failed healing response, chronic inflammation, and predominant catabolic activity. This complex interplay of intrinsic and extrinsic factors underscores the importance of a comprehensive approach to understanding and mitigating the risk of Achilles tendon injuries.