Abstract
Screening for food insecurity and other social determinants of health is being integrated into oncology practice. We performed a pilot randomized trial to investigate whether an unconditional cash transfer (UCT) could be used to address food insecurity among female breast and gynecological cancer survivors. Food-insecure cancer survivors completed a baseline survey and were randomly assigned to receive $100/month for 3 months (UCT) or usual care (UC). Participants (n = 14) completed a follow-up survey after 3 months, and we compared changes in health-related quality of life, indicators of food insecurity, diet quality, and whether a participant had to forgo, delay, or make changes to medical care because of cost. The UCT was associated with higher physical health scores, fewer indicators of food insecurity, better diet quality, and a lower likelihood of forgoing medical care than those who received UC. Our results suggest that UCTs can improve outcomes for food-insecure cancer survivors.
Brief communication
Screening for food insecurity and other social determinants of health is increasingly recommended as part of oncology practice.1,2 As many as 36% of cancer survivors report experiencing food insecurity,3 defined as a household-level economic and social condition of limited or uncertain access to adequate food.4 However, few interventions addressing food insecurity among cancer survivors have been tested. Most of the current food insecurity interventions provide food assistance in the form of food vouchers or prescriptions, food pantries, or meal delivery services. These food assistance interventions play a critical role in keeping patients and families from going hungry, but providing food directly to patients removes their ability to buy and prepare nutritious, culturally sustaining meals. Furthermore, these interventions do not address related financial and social needs of cancer patients, such as housing instability, transportation challenges, or unpaid utility bills. We sought to overcome these limitations by piloting an unconditional cash transfer (UCT) intervention to address financial and social needs among female breast and gynecological cancer survivors receiving care at the University of New Mexico Comprehensive Cancer Center (UNMCCC).
UCTs are a direct investment of money given to patients, without any conditions or rules about financial use.5 UCTs have been shown to confer sustainable, long-term health benefits in other settings, but their use to improve cancer outcomes remains untested. In our prior research, UCTs emerged as the preferred solution for addressing food insecurity among cancer survivors and their caregivers in New Mexico.6 Here we report the results from a prospective, randomized pilot trial of patients with female breast or gynecological cancer who were receiving care at the UNMCCC.
The trial randomly assigned participants to receive either a mailed $100 VISA merchandise card each month for 3 months and usual care (UC) or UC alone per routine clinical practice. For this initial pilot, the amount of financial assistance ($100 per month) was approximately equivalent to one-third of the Supplemental Nutrition Assistance Program maximum benefit amount for one person.7 UC included access to all patient support services and resources available at UNMCCC, including patient navigation, social work, financial counselors, and dieticians for assistance with social and dietary needs. In our formative intervention development work, we learned that referrals are made to these services when social or dietary needs are identified by providers. Although we did not specify how these referrals needed to be made for patients enrolled in this study, we did standardize the receipt of nutritional and cancer survivorship information by providing printed pamphlets on Nutrition During Cancer Treatment and Nutrition and the Cancer Survivor developed by the American Institute for Cancer Research.8 Pamphlets were mailed to all participants after completion of the baseline survey. At the conclusion of the 3-month study follow-up period, participants in the UC arm received a one-time payment in VISA merchandise cards of $300. The rationale for this delayed payment was to ensure that all participants, who by study design were identified as food insecure, received monetary assistance independent of their study arm assignment. All study procedures were approved by the Institutional Review Board of the University of New Mexico Health Sciences Center. The trial is registered at ClinicalTrials.gov, identifier NCT05176743.
Participant recruitment occurred between September 2021 and March 2022. Eligible participants included UNMCCC patients diagnosed within the past 24 months with stage I-III female breast, ovarian, endometrial, cervical, or vulvar cancer who had completed their initial course of cancer-directed therapy. All participants had to be at least 18 years of age and able to speak English or Spanish. Study staff identified potentially eligible participants from clinic lists and screened for food insecurity using the 2-item Hunger VitalSignTM screening tool.9 The target sample size for this pilot study was initially 44 patients, selected based on the UNMCCC clinic volume of breast and gynecological patients in 2019 and an anticipated recruitment of 50% of eligible, food-insecure patients. However, health-care service disruptions throughout the coronavirus pandemic reduced both the total volume of patients and the capacity of study staff to screen for eligible patients.
Participants completed a baseline survey, administered as a web-based survey or computer-assisted telephone interview, depending on patient preference. The survey measured health-related quality of life (HRQoL) using the PROMIS Global Health Scale10 as well as sociodemographic characteristics. After completion of the baseline survey, participants were randomly assigned using a permuted block randomization block size of 10, with a 1:1 distribution to either the UCT or UC arm of the study. Three months after the baseline survey, all participants were asked to complete a follow-up survey that assessed HRQoL,10 indicators of adult food insecurity,4 diet quality (≥2.5 cups of fruits and vegetables daily), and whether a participant had to forgo, delay, or make changes to medical care because of cost.3
Out of 42 patients screened for food insecurity by our study team, 19 (45%) were found to be food insecure and eligible for participation. Seventeen patients (89%) consented to participate in the study, completed the baseline survey, and were randomly assigned to the UCT intervention arm (n = 7) or UC (n = 10). Fourteen (82%) participants went on to complete the 3-month follow-up survey. Despite excellent recruitment and retention among eligible, invited patients, staffing shortages and a drop in anticipated clinic volume during the coronavirus pandemic resulted in a sample size (n = 14) that was only 32% of our intended 44 participants.
Of the 14 participants completing all study activities, 70% had an annual household income of less than $30 000, and 50% had a bachelor’s degree or higher level of education. Six (43%) participants reported working at least part-time. We observed a difference in the proportion of participants in the UCT (n = 5) and UC (n = 9) arms reporting a disability at baseline (0% vs 67%).
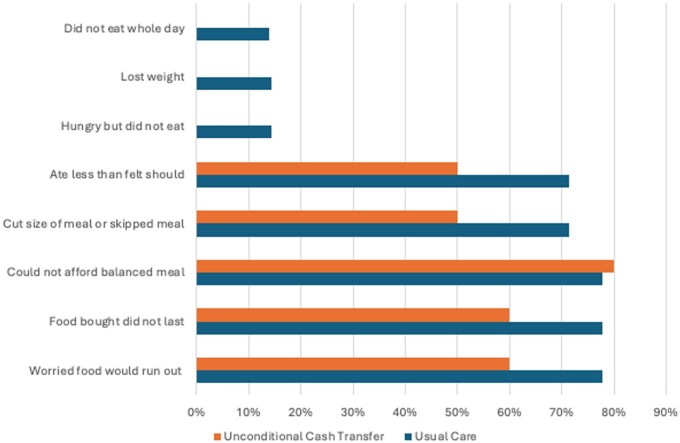
HRQoL scores at baseline and follow-up are shown in Table 1. The UCT was associated with a 4.4 point higher physical health score (SD = 6.4) over the 3-month follow-up period, whereas the physical health score in the UC arm appeared to decline by 1 point (SD = 5.0). No difference in mental health was observed in either arm over time. Figure 1 displays the proportion of participants reporting indicators of adult food insecurity at 3 months in each study arm. None of the participants who received the UCT reported that they did not eat for a whole day, lost weight, or felt hungry but did not eat. In comparison, there was at least 1 participant in the UC arm who reported experiencing these indicators of food insecurity.
Table 1.
Change in health-related quality of life.
| Usual care | Unconditional cash transfer | |||
|---|---|---|---|---|
| (n = 9) |
(n = 5) |
|||
| Mental health | Physical health | Mental health | Physical health | |
| Baseline mean (SD) | 40.8 (8.0) | 40.0 (5.1) | 45.7 (5.4) | 39.3 (4.4) |
| Follow-up mean (SD) | 42.1 (6.4) | 39.0 (5.4) | 46.2 (8.4) | 43.7 (2.6) |
| Change mean (SD) | 1.3 (8.1) | −1.0 (5.0) | 0.5 (5.5) | 4.4 (6.4) |
Figure 1.
Percentage of participants reporting indicators of adult food insecurity at 3 months, by study arm, N = 14.
In the follow-up survey, 80% of patients in the UCT arm reported consuming at least 2.5 cups of fruits and vegetables daily compared with just 22% in the UC arm, whereas no substantial difference was seen between arms in terms of participants reporting regular physical activity. Moreover, fewer patients who received the UCT (40%) reported having to forgo, delay, or make changes to medical care because of cost than those who received UC (56%). In contrast, when asked at baseline, approximately 40% of participants in both the UCT and UC arms reported ever having to forgo, delay, or make changes to medical care because of cost.
In this small, randomized pilot trial, we found that food-insecure patients who received a UCT of $100 per month for 3 months reported higher HRQoL scores, fewer indicators of adult food insecurity, and better diet quality. Importantly, patients receiving the UCT were also less likely to report forgoing, delaying, or making changes to medical care because of cost. This suggests that the cost of a modest investment in patients with identified social needs may be offset by better patient outcomes and better adherence to care. Prior studies document higher medical costs among food-insecure patients,11-13 highlighting the potential value of developing effective interventions to address social needs.14,15
Forty-five percent of patients screened in this study were food insecure. This exceeded our earlier estimate of the prevalence of food insecurity of 36% from our prior, population-based study of food insecurity in New Mexico.3 This may be due to a particularly high prevalence of food insecurity among female breast and gynecological oncology patients and to a willingness of food-insecure patients to disclose food insecurity to our research team. National data find that food insecurity disproportionately affects women and households with children.16 Our experience supports other studies highlighting the feasibility and acceptability of food insecurity screening in clinical practice.17-19
As screening for social needs continues to be implemented and is expanding in use in clinical practice, interventions addressing multiple, related needs must be developed and tested. In this study, we did not have access to information about other coexisting social needs or additional assistance provided. However, our results suggest that even modest investments in patients in the form of UCTs can improve outcomes. Future trials and economic evaluations of UCTs as a strategy for addressing social needs are warranted.
Acknowledgments
The funder was not involved in the design of the study; the collection, analysis, and interpretation of the data; the writing of the manuscript; or the decision to submit the manuscript for publication.
Contributor Information
Jean A McDougall, Office of Community Outreach and Engagement, Fred Hutchinson Cancer Center, Seattle, WA, United States; Department of Internal Medicine, University of New Mexico, Albuquerque, NM, United States.
Shoshana Adler Jaffe, University of New Mexico Comprehensive Cancer Center, Albuquerque, NM, United States.
Kendal Jacobson, University of New Mexico Comprehensive Cancer Center, Albuquerque, NM, United States.
Tori L Shaver, School of Medicine, University of New Mexico, Albuquerque, NM, United States.
Jennifer L F Wilson, University of New Mexico Comprehensive Cancer Center, Albuquerque, NM, United States.
Tawny Boyce, University of New Mexico Comprehensive Cancer Center, Albuquerque, NM, United States.
Bernard Tawfik, Department of Internal Medicine, University of New Mexico, Albuquerque, NM, United States; University of New Mexico Comprehensive Cancer Center, Albuquerque, NM, United States.
Janet Page-Reeves, Office for Community Health, Department of Family and Community Medicine, University of New Mexico, Albuquerque, NM, United States.
Author contributions
Jean Alison McDougall, PhD, MPH (Conceptualization; Formal analysis; Funding acquisition; Investigation; Methodology; Writing—original draft; Writing—review & editing), Shoshana Adler Jaffe, MPH (Conceptualization; Investigation; Methodology; Writing—review & editing), Kendal Jacobson, BA (Investigation; Project administration; Writing—review & editing), Tori L. Shaver, MS (Data curation; Writing—review & editing), Jennifer L.F. Wilson, MS (Data curation; Writing—review & editing), Katrina Baca, MD (Data curation; Writing—review & editing), Tawny Boyce, MS, MPH (Formal analysis; Methodology; Writing—review & editing), Bernard Tawfik, MD (Investigation; Writing—review & editing), Janet M. Page-Reeves, PhD (Conceptualization; Investigation; Methodology; Writing—review & editing).
Funding
This study used funding from the Wake Forest NCI Community Oncology Research Program (NCORP) Research Base (2UG1CA189824, MPIs: Lesser & Weaver). This research also used services provided by the Behavioral Measurement and Population Science Shared Resource and the Biostatistics Shared Resource, facilities supported by the State of New Mexico, and a University of New Mexico Comprehensive Cancer Center NCI-funded grant, P30CA118100.
Conflicts of interest
All authors, Jean A. McDougall, Shoshana Adler Jaffe, Kendal Jacobson, Tori L. Shaver, Jennifer L.F. Wilson, Katrina Baca, Tawny Boyce, Bernard Tawfik, and Janet Page-Reeves, declare that they have no conflicts of interest to disclose.
Data availability
The data underlying this article cannot be shared due to the privacy of individuals who participated in the study.
References
- 1. National Comprehensive Cancer Network. Measuring and addressing health-related social needs in cancer: working group recommendations. Accessed November 13, 2024. https://www.nccn.org/docs/default-source/oncology-policy-program/HRSN-WG-Recommendations.pdf
- 2. American Cancer Society. Increasing food security efforts across the cancer continuum: a toolkit for comprehensive cancer control coalitions. Accessed November 13, 2024. https://acs4ccc.org/wp-content/uploads/2023/06/ACS-FI-Toolkit_GSCN-2023-1.pdf
- 3. McDougall JA, Anderson J, Adler Jaffe S, et al. Food insecurity and forgone medical care among cancer survivors. J Clin Oncol Oncol Pract. 2020;16:e922-e932. 10.1200/JOP.19.00736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. United States Department of Agriculture Economic Research Service. Definitions of food security. Accessed April 11, 2024. https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-u-s/definitions-of-food-security/
- 5. Yoshino CA, Sidney-Annerstedt K, Wingfield T, et al. Experiences of conditional and unconditional cash transfers intended for improving health outcomes and health service use: a qualitative evidence synthesis. Cochrane Database Syst Rev. 2023;3:CD013635. 10.1002/14651858.CD013635.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. McDougall JA, Jaffe SA, Guest DD, Sussman AL.. The balance between food and medical care: experiences of food insecurity among cancer survivors and informal caregivers. J Hunger Environ Nutr. 2022;17:380-396. 10.1080/19320248.2021.1892295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. New Mexico Health Care Authority. Looking for assistance. Accessed November 13, 2024. https://www.hca.nm.gov/lookingforassistance/supplemental_nutrition_assistance_program__snap/
- 8. American Institute for Cancer Research. Survivorship. Accessed April 11, 2024. https://store.aicr.org/collections/survivorship
- 9. Hager ER, Quigg AM, Black MM, et al. Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics. 2010;126:e26-e32. 10.1542/peds.2009-3146 [DOI] [PubMed] [Google Scholar]
- 10. Hays RD, Bjorner JB, Revicki DA, Spritzer KL, Cella D.. Development of physical and mental health summary scores from the patient-reported outcomes measurement information system (PROMIS) global items. Qual Life Res. 2009;18:873-880. 10.1007/s11136-009-9496-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Berkowitz SA, Basu S, Meigs JB, Seligman HK.. Food insecurity and health care expenditures in the United States, 2011-2013. Health Serv Res. 2018;53:1600-1620. 10.1111/1475-6773.12730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Berkowitz SA, Seligman HK, Meigs JB, Basu S.. Food insecurity, healthcare utilization, and high cost: a longitudinal cohort study. Am J Manag Care. 2018;24:399-404. [PMC free article] [PubMed] [Google Scholar]
- 13. Men F, Gundersen C, Urquia ML, Tarasuk V.. Food insecurity is associated with higher health care use and costs among Canadian adults. Health Aff (Millwood). 2020;39:1377-1385. 10.1377/hlthaff.2019.01637 [DOI] [PubMed] [Google Scholar]
- 14. Basu S, Berkowitz SA, Davis C, Drake C, Phillips RL, Landon BE.. Estimated costs of intervening in health-related social needs detected in primary care. JAMA Intern Med. 2023;183:762-774. 10.1001/jamainternmed.2023.1964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Yan AF, Chen Z, Wang Y, et al. Effectiveness of social needs screening and interventions in clinical settings on utilization, cost, and clinical outcomes: a systematic review. Health Equity. 2022;6:454-475. 10.1089/heq.2022.0010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rabbitt MP, Hales LJ, Burke MP, Coleman-Jensen A. Household Food Insecurity in the United States in 2022. Economic Research Report No. (ERR-325). 2024:53. Accessed November 13, 2024. https://www.ers.usda.gov/publications/pub-details/?pubid=107702
- 17. Alvis CE, Mosha M, Amankwah EK, Hernandez RG, Morrison JM.. Comparison of caregiver and provider food insecurity screening preferences within a health system. Clin Pediatr (Phila). 2024;63:650-658. 10.1177/00099228231191926 [DOI] [PubMed] [Google Scholar]
- 18. Frost K, Stafos A, Metcalf AL, et al. Knowledge and barriers related to food insecurity screening in healthcare settings. Public Health Nurs. 2022;39:770-777. 10.1111/phn.13040 [DOI] [PubMed] [Google Scholar]
- 19. Patel KG, Borno HT, Seligman HK.. Food insecurity screening: a missing piece in cancer management. Cancer. 2019;125:3494-3501. 10.1002/cncr.32291 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article cannot be shared due to the privacy of individuals who participated in the study.