Abstract
Background
Distal radial fractures are common forearm injuries. A key rehabilitation objective is achieving adequate wrist palmar and dorsal flexion range-of-motion (ROM). However, few studies have explored this relationship, with even lesser number of studies investigating the impact of distal radius alignment on wrist ROM limitation due to fractures. We aimed to determine the effect of radial alignment on wrist palmar and dorsal flexion ROM after conservative treatment for distal radial fractures.
Patients and methods
This retrospective, cohort study, included 82 patients with distal radial fractures (11 men, 71 women, mean age: 65.9 ± 16.6 years) who underwent examination at an orthopedic clinic. Wrist ROM limitation was defined as ˂60° of dorsal flexion and ˂55° of palmar flexion. The palmar tilt (PT), radial length (RL), and radial inclination (RI) were radiographically measured. The patient’s age, residual symptoms, and rehabilitation period were extracted from medical records. Univariate and multivariate analyses were conducted with the presence/absence of wrist ROM limitation as the objective variable, with the PT, RL, and RI as explanatory variables. A comparison of age, and rehabilitation period between the groups with and without wrist ROM limitation was performed using the Mann–Whitney U test. The presence/absence of residual symptoms were compared between two groups using the chi-squared test.
Results
Univariate analysis revealed that PT, RL and RI were associated with palmar flexion ROM limitation. Multivariate analysis showed that PT was the only factor associated with palmar flexion ROM limitation (odds ratio: 0.85, 95% confidence interval: 0.78–0.91, p < 0.001), while dorsal flexion ROM limitation was not associated with any of the three measurements. The group with palmar flexion ROM limitation presented older age (73.1 vs. 59.6 years), higher residual symptom frequency (23 vs. 12 patients), and longer rehabilitation period (159.2 vs. 73.9 days) compared to the group without the limitation (p < 0.01).
Conclusion
Dorsal displacement of the distal radius induces alterations in the wrist joint motion axis, potentially affecting limitation in palmar flexion ROM. Patients with palmar flexion ROM limitation had more residual symptoms and longer rehabilitation period than those without. These findings may contribute to the development of evidence-based joint ROM exercises, risk management, goal setting, and rehabilitation programs for patients with distal radial fractures.
Keywords: Distal radial fractures, palmar flexion ROM limitation, palmar tilt
KEY MESSAGES
Dorsal displacement of the distal radius may limit palmar flexion ROM.
Palmar tilt is an important aspect of joint mobilization exercises, goal setting, and treatment planning in distal radial fractures.
Introduction
Distal radial fractures, including radial and ulnar diaphyseal fractures, are common forearm injuries; they mostly occur in low-energy traumas in older adults and women [1–9]. Dorsal displacement of distal radius fractures, known as Colles’ fractures, results from the position of the injured limb and anatomic factors. In traction repair, these anatomical factors include a thick long axis along the palmar aspect and a thin Z-shaped radial interosseous ligament along the dorsal aspect, resulting in a palmar dominance of traction transmission and difficulty in repositioning the bone fragments into palmar flexion position [10]. Therefore, many studies have focused on bone malunion and subjective and functional outcomes after distal radius fractures [11–23]. External fixation with plaster casts or splinting is the preferred conservative treatment for these distal radial fractures; this treatment has shown good outcomes even in the presence of radial malunion [12–14].
Meanwhile, several studies have reported an association between radial malunion and functional outcomes [15–23]. Palmar tilt (PT), radial length (RL), and radial inclination (RI) are key measures for assessing distal radius alignment, closely associated with symptomatic outcomes [16]. A PT of ≥ −10° has been associated with a poor prognosis for alignment changes, arm-related disability lasting 2 years [17,18], and increased difficulty in daily life activities and work-related tasks [19]. In addition, loss of PT and radial shortening are associated with joint space narrowing and intra-articular injury [20] and long-term wrist pain, as measured using the pain subscale of the patient-rated wrist evaluation (PRWE), including patient-rated levels of pain at rest, during various activities, and pain intensity and frequency [21]. Moreover, previous studies have reported a correlation between the loss of PT and decreased wrist range of motion (ROM) and functional outcomes [22,23].
An important rehabilitation objective is achieving adequate wrist palmar and dorsal flexion ROM, typically reported at ∼60° of dorsal flexion for standing from a chair with armrests and 55° of palmar flexion for personal care of daily life activities [24]. Understanding the relationship between radiographic parameters and wrist ROM is crucial for predicting prognosis and determining the efficacy of conservative treatment and rehabilitation [25]. However, few studies have explored this relationship, with even lesser number of studies investigating the impact of distal radius alignment on wrist ROM limitation due to fractures. We hypothesized that the loss of PT in distal radial fractures could lead to limitations in wrist palmar ROM by altering the axis of wrist joint motion in the sagittal plane toward dorsiflexion.
Therefore, in this study, we aimed to determine the effect of distal radius alignment on wrist palmar and dorsal flexion ROM in distal radial fractures. By identifying the relationship between wrist join ROM limitation and distal radius alignment during daily life activities, this research sought to facilitate evidence-based rehabilitation goal setting and program planning for patients with distal radius fractures.
Patients and methods
The research team for this retrospective cohort study was formed in 2023. We collected data from patients who visited a single orthopedic clinic between 2009 and 2024. Participants were diagnosed with distal radial fracture by one orthopedic surgeon using radiography, pain testing, and physical examination. The study population comprised 106 patients (16 [15%] men and 90 [85%] women) who underwent rehabilitation. Patients were excluded if (1) measurements of the Anterior-Posterior view and lateral view were difficult to obtain due to pain; (2) they discontinued rehabilitation; (3) they presented with complex regional pain syndrome: (4) they had a history of surgery; and (5) they intended to undergo rehabilitation for other conditions, such as knee osteoarthritis and periarthritis of the shoulder joints, and not for distal radius fractures, because of the effects on the frequency and period of rehabilitation.
The patient’s age, sex, presence/absence of wrist ROM limitation and residual symptoms, initial treatment, fixation period (from injury to initiation of rehabilitation), rehabilitation frequency and period, and overall treatment period and ROM measurement date (from injury to completion of rehabilitation) were extracted from medical records.
Wrist range-of-motion limitation
Wrist ROM was measured on the completion of rehabilitation implementation. According to previous studies on activities of daily living and functional wrist ROM [24], wrist ROM limitation was defined as ˂60° of dorsal flexion and ˂55° of palmar flexion, as measured by the physician and physical therapist. Patients were categorized into two groups: the wrist ROM limitation group and the non-ROM limitation group.
Radiographic findings
PT, RL, and RI were measured using the RADspeed Pro radiography system (Shimadzu Corp, Kyoto, Japan). These outcomes were obtained from the findings of radiographs, in which the physician diagnosed bone union.
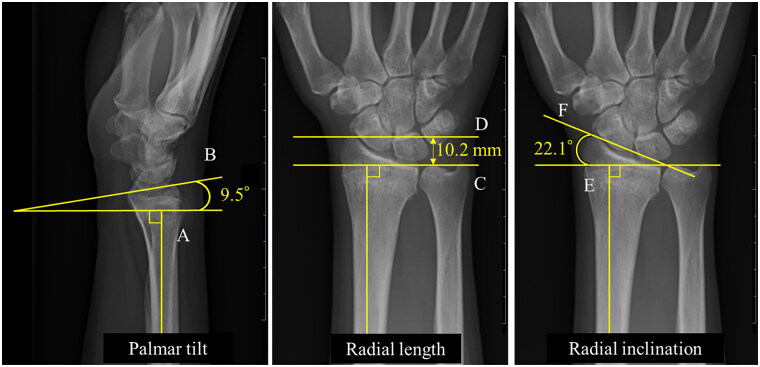
PT [26,27] was defined as the angle between the perpendicular drawn to the long axis of the radius and the line connecting the dorsal and palmar rims of the radius, with a reference value of 10°. RL [27] was defined as the distance between two lines drawn perpendicular to the long axis of the radius, and the apex of the radial styloid and the ulnar aspect of the articular surface, with a reference value of 11 mm. RI [27] was defined as the angle between the perpendicular line to the long axis of the radius and the line connecting the radial styloid and ulnar border of the distal radius, with a reference value of 22° (Figure 1). The first and second intraclass correlation coefficients for the same examiner for PT, RL, and RI were 0.965 (95% confidence interval [CI]: 0.903–0.988), 0.822 (95% CI: 0.485–0.940), and 0.926 (95% CI: 0.786–0.975), respectively.
Figure 1.
Method of measurement of distal radius alignment (representative case). Palmar tilt (PT): (1) Draw a line perpendicular to the long axis of the radius (A); (2) draw a line connecting the dorsal and palmar rims of the radius (B); and (3) measure the angle between lines A and B. Radial length (RL): (1) Draw a line on the distal ulnar articular surface (C); (2) draw a line on the radial styloid process (D); and (3) measure the distance between lines C and D. Radial inclination (RI): (1) Draw a perpendicular line to the long axis of the radius (E); (2) draw a line connecting the radial styloid process and ulnar border of the distal radius (F); and (3) measure the angle between lines E and F.
Statistical analysis
The objective variable was the presence or absence of wrist palmar and dorsal flexion ROM limitation, while the PT, RL, and RI were chosen as explanatory variables for both univariate and multivariate analyses. Receiver operating characteristic (ROC) curves of the radiographic parameters were plotted to determine the presence or absence of wrist ROM limitation, and the sensitivity and specificity of the area under the curve (AUC) and cutoff values were analyzed.
The sex distribution and presence or absence of residual symptoms were compared between groups with and without wrist ROM limitation using the chi-squared test. Pearson’s chi-squared test was used if <20% of the cells had expected frequencies of <5, and Fisher’s exact probability test was conducted if this value was >20%. A comparison of age, fixation period, rehabilitation frequency and period, and treatment period between the two groups was performed using the Mann–Whitney U test. Statistical analysis was performed using R4.4.1 (R Software for Statistical Computing, Vienna, Austria), with the significance level set at <5%.
Ethical considerations
This study was approved by the Ethics Committee of Hitachino Orthopedic Clinic (protocol number: 202301). As this was a retrospective study and no adverse events were observed in the patients, the need for informed consent was waived.
Results
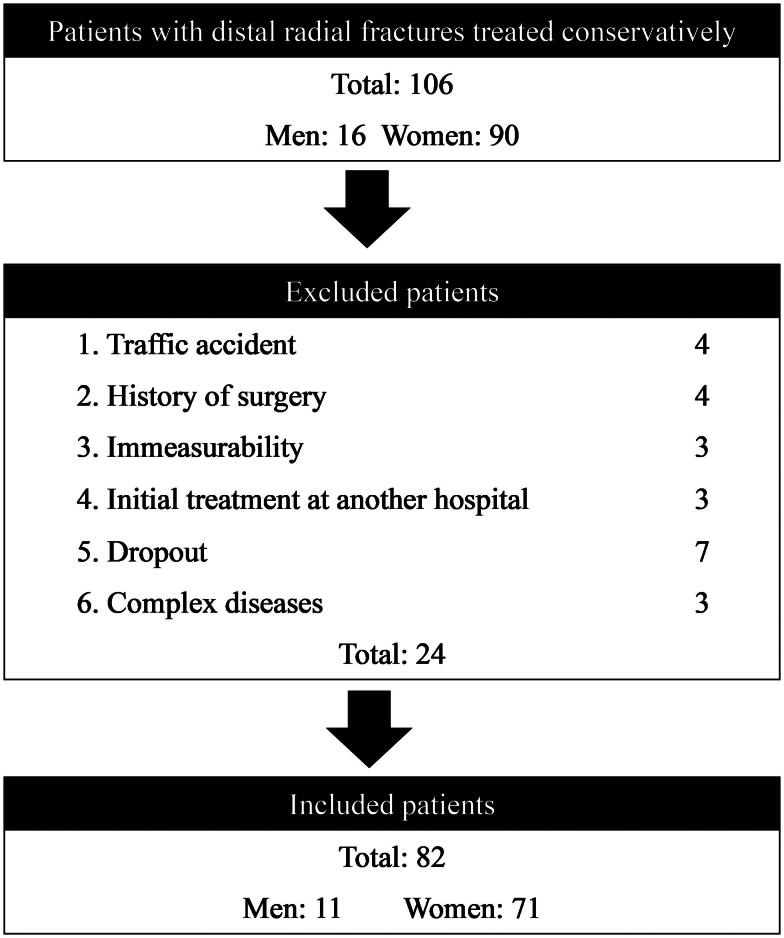
Among 106 patients with distal radial fractures treated at our institution, 82 patients (11 [13%] men, 71 [87%] women; mean age, 65.9 ± 16.6 years; fracture side, 37 [45%] right hand and 45 [55%] left hand) were included in the study (Figure 2). Among the included patients, 38 presented palmar flexion ROM limitation, 10 had dorsal flexion ROM limitation, and 35 had residual symptoms. The mean period of bone union and radiographic assessment was 64.7 ± 18.3 days, and the mean PT, RL, and RI were −1.9 ± 12.1°, 6.4 ± 2.8 mm, and 11.0 ± 4.7°, respectively. Initial treatments included splinting in 57 patients (70%), plaster cast in 11 patients (13%), bracing and splinting in six patients (7%), splinting and triangular bandage in two patients (2%), palmar splinting in two patients (2%), above elbow splinting in two patients (2%), local anesthesia and bilateral splinting in one patient (1%), and wrist support in one patient (1%). The rehabilitation sessions frequency averaged 16.4 ± 17.6 times, with fixation period of 33.7 ± 10.5 days, rehabilitation period of 113.0 ± 108.2 days, and treatment period and ROM measurement date of 146.7 ± 106.3 days. Finally, residual symptoms, such as limitations in squeezing, daily life activities, and weightlifting, were observed in 43% of included patients (Table 1).
Figure 2.
Patient inclusion criteria.
Table 1.
Distribution of residual symptoms.
| Details | Frequency | Proportion among the residual symptom group (%) | Overall percentage (%) |
|---|---|---|---|
| Squeezing | 10 | 29 | 12 |
| Daily living | 8 | 23 | 10 |
| Lifting weights | 6 | 17 | 7 |
| Motion pain | 4 | 11 | 5 |
| Weight pain | 2 | 6 | 2 |
| Numbness | 1 | 3 | 1 |
| Wrist pain | 1 | 3 | 1 |
| Housework | 1 | 3 | 1 |
| Job | 1 | 3 | 1 |
| Gardening | 1 | 3 | 1 |
| Total | 35 | 43 |
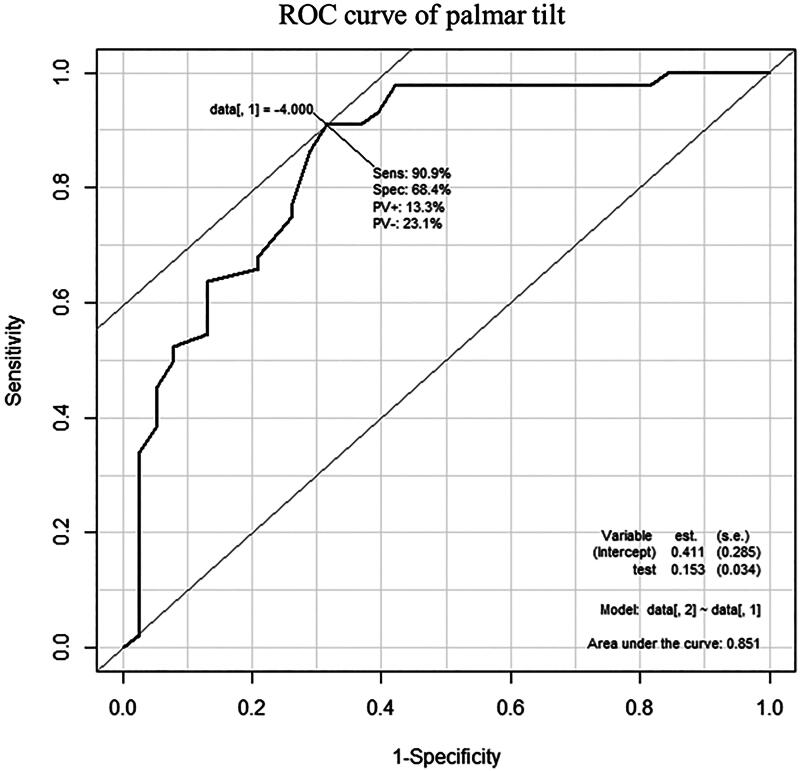
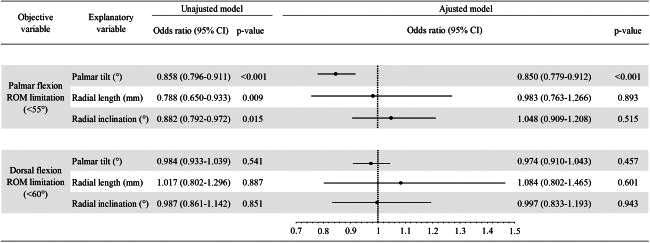
Univariate analysis revealed that PT (odds ratio [OR]: 0.858, 95% CI: 0.796–0.911), RL (OR: 0.788, 95% CI: 0.650–0.933), and RI (OR: 0.882, 95% CI: 0.792–0.972) were associated with palmar flexion ROM limitation. Furthermore, multivariate analysis showed that PT was the only factor associated with palmar flexion ROM limitation (OR: 0.850, 95% CI: 0.779–0.912, Table 2). In contrast, dorsal flexion ROM limitation was not associated with any of the three measurements. The ROC curve for PT in predicting the presence of palmar flexion ROM limitation yielded an AUC of 0.851, with a cutoff value of −4°, 90.9% sensitivity, and 68.4% specificity (Figure 3).
Table 2.
Univariate and multivariate analyses with palmar and dorsal flexion ROM limitation as the objective variables.
|
CI: confidence interval; ROM: range of motion.
Figure 3.
ROC curve of palmar tilt with and without palmar flexion range-of-motion limitation. ROC: receiver operating characteristic.
The comparison of age, sex, residual symptoms, fixation period, rehabilitation frequency and period, and treatment period between the groups with and without palmar flexion ROM limitation (Table 3) revealed older age (73.1 ± 10.0 vs. 59.6 ± 18.7 years, p < 0.001), higher residual symptom frequency (23 vs. 12 patients, p = 0.002), and higher rehabilitation frequency (23.2 ± 23.1 vs. 10.5 ± 7.4 times, p < 0.001) in the wrist ROM limitation group. Additionally, significantly longer rehabilitation and treatment periods were observed in the wrist ROM limitation group (159.2 ± 140.2 and 196.5 ± 143.6 days, respectively, vs. 73.9 ± 45.1 and 111.7 ± 45.1 days, respectively, p < 0.001). No significant differences were found in sex distribution and fixation period between the groups.
Table 3.
Comparison of sex, residual symptoms, fixation period, rehabilitation period, and treatment period in the palmar flexion ROM limitation and non-ROM limitation groups.
| Variables | Palmar flexion ROM limitation |
p-Value | Effect size, r | |
|---|---|---|---|---|
| Present | Absent | |||
| Age, years | 73.1 (10.0) | 59.6 (18.7) | <0.001 | 0.37 |
| Sex (men/women), number of patients | 3/35 | 8/36 | 0.173 | |
| Residual symptoms (presence/absence), number of patients | 23/15 | 12/32 | 0.002 | |
| Fixation period, days | 37.4 (16.1) | 37.8 (7.3) | 0.343 | 0.10 |
| Rehabilitation frequency, times | 23.2 (23.1) | 10.5 (7.4) | <0.001 | 0.40 |
| Rehabilitation period, days | 159.2 (140.2) | 73.9 (45.1) | <0.001 | 0.44 |
| Treatment period, days | 196.5 (143.6) | 111.7 (45.1) | <0.001 | 0.41 |
Fixation period: number of days from the onset of injury to the commencement of rehabilitation; treatment period: number of days from the onset of injury to the end of rehabilitation; ROM: range-of-motion; Palmar flexion ROM limitation: <55°, as identified by a physician and physical therapist.
Discussion
Previous studies have measured the outcomes of distal radial fractures using the PRWE and Disabilities of Arm, Shoulder, and Hand (DASH) scores [16,18,20,21,28]. The present study clarified the effect of distal radius alignment on wrist ROM, which may provide useful findings for rehabilitation implementation.
The results of univariate analysis showed that the PT, RL, and RI were significantly associated with palmar flexion ROM limitation, consistent with previous studies linking distal radius malunion and malalignment to prognosis [19,21–23,29,30]. Moreover, multivariate analysis identified PT as the only factor associated with palmar flexion ROM limitation, which may be attributed to the dorsal displacement of the distal radius, known as Colles’ fracture, altering the axis of motion of the wrist joint. According to the results of this study, dorsal flexion ROM limitation showed no association with PT, suggesting that the change in the wrist joint motion axis primarily affects palmar flexion ROM limitation rather than dorsal flexion ROM limitation. Therefore, even with adequate intra-articular motion of the flexor carpal joint, such as sliding or rolling of the carpal bone in the radial articular plane, the change in the articular plane in the dorsal direction may result in palmar flexion ROM limitation. As the complication rate of dorsal capsular injuries in intra-articular distal radial fractures is ∼70% [29], excessive palmar flexion joint ROM without considering dorsal displacement of the distal radius may result in extensional stress not only on the capsular wrist ligaments but also on the dorsal radial interphalangeal ligament and extensor tendon. Moreover, the present study determined the cutoff value of PT for the presence of palmar flexion ROM limitation using an ROC curve, suggesting that a loss of PT of ≥ −4° may result in palmar flexion ROM limitation. Despite its relatively low specificity of 68% [31], the high sensitivity of 91% underscores the importance of PT as an important parameter in guiding rehabilitation strategies and joint ROM exercises.
The present study found no significant difference in the fixation period between the groups with and without palmar flexion ROM limitation. This implies that rehabilitation was chosen regardless of the degree of displacement of distal radius fractures and bone union to prevent contracture due to edema and fibrosis caused by plaster casts and splints [32]. However, in this study, the rehabilitation and treatment periods were significantly longer in the group with palmar flexion ROM limitation than in the group without ROM limitation, and many patients experienced difficulty with the treatment. Furthermore, the higher prevalence of residual symptoms among older patients with palmar flexion ROM limitation, compared to those without, corresponds to findings from a previous study [30]; this study indicated that rehabilitating distal radial fractures in older patients is often challenging. These residual symptoms affected activities related to wrist palmar ROM, such as squeezing motion, potentially contributing to wrist palmar flexion ROM limitation. Additionally, no significant differences between surgical treatment with a volar locking plate and conservative treatment after >1 year of follow-up have been previously revealed [32,33]. These findings suggest the need for a comprehensive approach, incorporating rehabilitation of daily life activities, movement guidance, and joint ROM exercises while considering radiographic findings.
This study has various limitations. First, unlike previous studies that used the PRWE ,and DASH to evaluate the treatment outcomes [16,18,20,21,28] , our evaluation relied solely on data extracted from medical records to ascertain the presence of residual symptoms. Therefore, compared to previous studies [28] that reported a good prognosis of 72%, the proportion of patients with non-residual symptoms was lower at 57%, potentially encompassing patients with relatively mild disability in performing daily life activities and work-related tasks. Additionally, the outcome of wrist ROM limitation in this study was assessed in a mildly defined setting. Although we conducted a multivariate analysis using the presence or absence of wrist ROM limitation as the objective variable (obtained from the medical records), future studies should consider using multiple linear regression analysis using detailed joint ROM measurements, such as radial and ulnar deviation, pronation, and supination, as outcomes to obtain more useful findings for rehabilitation. Finally, although this study used quantitative assessments, such as PT, RL, and RI to determine their relationship with wrist ROM, the relationship between wrist ROM and qualitative assessments, such as AO/OTA classification and Fernandez classification system, should also be clarified [34].
Conclusions
This study elucidated the relationship between radiographic parameters and wrist ROM following conservative treatment for distal radial fractures. Univariate analysis revealed associations between the PT, RL, and RI and palmar flexion ROM limitation (set as the objective variable). Multivariate analysis further identified that the PT was the only factor associated with palmar flexion ROM limitation. Patients with palmar flexion ROM limitation had more residual symptoms and longer treatment periods than those without. These findings may contribute to the development of evidence-based joint ROM exercises, risk management, goal setting, and rehabilitation programs for patients with distal radial fractures.
Acknowledgements
The authors would like to thank Inami H. for their assistance in data collection.
Funding Statement
No funding was received.
Authors contributions
Takahashi M. conducted the writing of the original draft. Takahashi M., Iwamoto K., Fukaya T., and Igawa T. conducted the conceptualization, methodology, investigation methods, and formal analysis of this study. Miyauchi Y., Mutsuzaki H., and Tomita K. conducted the review and editing. Miyauchi Y. conducted the supervision and the project administration. All authors agree to be accountable for all aspects of the work.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The datasets generated and/or analyzed during the current study are not publicly available due to the protection of the study participants’ personal information but are available from the corresponding author on reasonable request.
References
- 1.Diamantopoulos AP, Rohde G, Johnsrud I, et al. The epidemiology of low- and high-energy distal radius fracture in middle-aged and elderly men and women in Southern Norway. PLOS One. 2012;7(8):e43367. doi: 10.1371/journal.pone.0043367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Flinkkilä T, Sirniö K, Hippi M, et al. Epidemiology and seasonal variation of distal radius fractures in Oulu, Finland. Osteoporos Int. 2011;22(8):2307–2312. doi: 10.1007/s00198-010-1463-3. [DOI] [PubMed] [Google Scholar]
- 3.Mellstrand-Navarro C, Pettersson HJ, Tornqvist H, et al. The operative treatment of fractures of the distal radius is increasing: results from a nationwide Swedish study. Bone Joint J. 2014;96-B(7):963–969. doi: 10.1302/0301-620X.96B7.33149. [DOI] [PubMed] [Google Scholar]
- 4.Sigurdardottir K, Halldorsson S, Robertsson J.. Epidemiology and treatment of distal radius fractures in Reykjavik, Iceland, in 2004. Comparison with an Icelandic study from 1985. Acta Orthop. 2011;82(4):494–498. doi: 10.3109/17453674.2011.606074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tsai CH, Muo CH, Fong YC, et al. A population-based study on trend in incidence of distal radial fractures in adults in Taiwan in 2000–2007. Osteoporos Int. 2011;22(11):2809–2815. doi: 10.1007/s00198-010-1489-6. [DOI] [PubMed] [Google Scholar]
- 6.Wilcke MK, Hammarberg H, Adolphson PY.. Epidemiology and changed surgical treatment methods for fractures of the distal radius: a registry analysis of 42,583 patients in Stockholm County, Sweden, 2004–2010. Acta Orthop. 2013;84(3):292–296. doi: 10.3109/17453674.2013.792035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sakuma M, Endo N, Oinuma T, et al. Incidence and outcome of osteoporotic fractures in 2004 in Sado City, Niigata Prefecture, Japan. J Bone Miner Metab. 2008;26(4):373–378. doi: 10.1007/s00774-007-0841-1. [DOI] [PubMed] [Google Scholar]
- 8.Ando J, Takahashi T, Ae R, et al. Epidemiology of distal radius fracture: a regional population-based study in Japan. BMC Musculoskelet Disord. 2023;24(1):478. doi: 10.1186/s12891-023-06608-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.MacIntyre NJ, Dewan N.. Epidemiology of distal radius fractures and factors predicting risk and prognosis. J Hand Ther. 2016;29(2):136–145. doi: 10.1016/j.jht.2016.03.003. [DOI] [PubMed] [Google Scholar]
- 10.Rockwood CA, Bucholz RW, Court-Brown CM, et al. Rockwood and Green’s fractures in adults. 6th ed. Philadelphia: Lippincott Williams & Wilkins; 2010. p. 2059. [Google Scholar]
- 11.Lucas B, Lippisch R, Pliske G, et al. Conservative management of distal radius fractures. Unfallchirurgie. 2023;126(3):227–237. doi: 10.1007/s00113-023-01293-1. [DOI] [PubMed] [Google Scholar]
- 12.Ranjan V, Agrawal U, Chatterji G, et al. Assessing the radiological and functional outcomes of Colles’ cast versus functional position cast immobilization in the conservative treatment of distal end of radius fractures. Cureus. 2024;16(6):e63492. doi: 10.7759/cureus.63492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Südow H, Severin S, Wilcke M, et al. Non-operative treatment or volar locking plate fixation for dorsally displaced distal radius fractures in patients over 70 years – a three year follow-up of a randomized controlled trial. BMC Musculoskelet Disord. 2022;23(1):447. doi: 10.1186/s12891-022-05394-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Young BT, Rayan GM.. Outcome following nonoperative treatment of displaced distal radius fractures in low-demand patients older than 60 years. J Hand Surg Am. 2000;25(1):19–28. doi: 10.1053/jhsu.2000.jhsu025a0019. [DOI] [PubMed] [Google Scholar]
- 15.Kong L, Kou N, Wang Y, et al. The necessity of restoration of radiologic parameters by closed reduction in elderly patients with distal radius fractures. Med Sci Monit. 2019;25:6598–6604. doi: 10.12659/MSM.915824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Grewal R, , MacDermid JC. The risk of adverse outcomes in extra-articular distal radius fractures is increased with malalignment in patients of all ages but mitigated in older patients. J Hand Surg Am. 2007;32(7):962–970. doi: 10.1016/j.jhsa.2007.05.009 17826547 [DOI] [PubMed] [Google Scholar]
- 17.Lichtman DM, Bindra RR, Boyer MI, et al. American Academy of Orthopaedic Surgeons clinical practice guideline on: the treatment of distal radius fractures. J Bone Joint Surg Am. 2011;93(8):775–778. doi: 10.2106/JBJS.938ebo. [DOI] [PubMed] [Google Scholar]
- 18.Brogren E, Wagner P, Petranek M, et al. Distal radius malunion increases risk of persistent disability 2 years after fracture: a prospective cohort study. Clin Orthop Relat Res. 2013;471(5):1691–1697. doi: 10.1007/s11999-012-2767-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gliatis JD, Plessas SJ, Davis TR.. Outcome of distal radial fractures in young adults. J Hand Surg Br. 2000;25(6):535–543. doi: 10.1054/jhsb.2000.0373. [DOI] [PubMed] [Google Scholar]
- 20.Forward DP, Davis TR, Sithole JS.. Do young patients with malunited fractures of the distal radius inevitably develop symptomatic post-traumatic osteoarthritis? J Bone Joint Surg Br. 2008;90(5):629–637. doi: 10.1302/0301-620X.90B5.19448. [DOI] [PubMed] [Google Scholar]
- 21.Karnezis IA, Panagiotopoulos E, Tyllianakis M, et al. Correlation between radiological parameters and patient-rated wrist dysfunction following fractures of the distal radius. Injury. 2005;36(12):1435–1439. doi: 10.1016/j.injury.2005.09.005. [DOI] [PubMed] [Google Scholar]
- 22.Kodama N, Takemura Y, Ueba H, et al. Acceptable parameters for alignment of distal radius fracture with conservative treatment in elderly patients. J Orthop Sci. 2014;19(2):292–297. doi: 10.1007/s00776-013-0514-y. [DOI] [PubMed] [Google Scholar]
- 23.Perugia D, Guzzini M, Civitenga C, et al. Is it really necessary to restore radial anatomic parameters after distal radius fractures? Injury. 2014;45:S21–S26. doi: 10.1016/j.injury.2014.10.018. [DOI] [PubMed] [Google Scholar]
- 24.Ryu JY, Cooney WP III, Askew LJ, et al. Functional ranges of motion of the wrist joint. J Hand Surg Am. 1991;16(3):409–419. doi: 10.1016/0363-5023(91)90006-w. [DOI] [PubMed] [Google Scholar]
- 25.Handoll HHG, Elliott J.. Rehabilitation for distal radial fractures in adults. Cochrane Database Syst Rev. 2015;2015(9):CD003324. doi: 10.1002/14651858.CD003324.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mann FA, Kang SW, Gilula LA.. Normal palmar tilt: is dorsal tilting really normal? J Hand Surg Br. 1992;17(3):315–317. doi: 10.1016/0266-7681(92)90120-q. [DOI] [PubMed] [Google Scholar]
- 27.van Eerten PV, Lindeboom R, Oosterkamp AE, et al. An X-ray template assessment for distal radial fractures. Arch Orthop Trauma Surg. 2008;128(2):217–221. doi: 10.1007/s00402-007-0391-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jaremko JL, Lambert RG, Rowe BH, et al. Do radiographic indices of distal radius fracture reduction predict outcomes in older adults receiving conservative treatment? Clin Radiol. 2007;62(1):65–72. doi: 10.1016/j.crad.2006.08.013. [DOI] [PubMed] [Google Scholar]
- 29.Hanker GJ. Radius fractures in the athlete. Clin Sports Med. 2001;20(1):189–201. doi: 10.1016/s0278-5919(05)70255-6. [DOI] [PubMed] [Google Scholar]
- 30.Stewart HD, Innes AR, Burke FD.. Factors affecting the outcome of Colles’ fracture: an anatomical and functional study. Injury. 1985;16(5):289–295. doi: 10.1016/0020-1383(85)90126-3. [DOI] [PubMed] [Google Scholar]
- 31.Yatsuya H, Li Y, Hirakawa Y, et al. A point system for predicting 10-year risk of developing type 2 diabetes mellitus in Japanese men: Aichi Workers’ Cohort Study. J Epidemiol. 2018;28(8):347–352. doi: 10.2188/jea.JE20170048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Moromizato K, Kimura R, Fukase H, et al. Whole-body patterns of the range of joint motion in young adults: masculine type and feminine type. J Physiol Anthropol. 2016;35(1):23. doi: 10.1186/s40101-016-0112-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Arora R, Lutz M, Deml C, et al. A prospective randomized trial comparing nonoperative treatment with volar locking plate fixation for displaced and unstable distal radial fractures in patients sixty-five years of age and older. J Bone Joint Surg Am. 2011;93(23):2146–2153. doi: 10.2106/JBJS.J.01597. [DOI] [PubMed] [Google Scholar]
- 34.Carula BC, Giostri GS, Bebber F, et al. Evaluation of intra- and interobserver reproducibility of the new AO/OTA classification for distal radius fractures compared with the Fernandez classification. Rev Bras Ortop. 2022;57(6):917–923. doi: 10.1055/s-0041-1740471. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analyzed during the current study are not publicly available due to the protection of the study participants’ personal information but are available from the corresponding author on reasonable request.