Abstract
Introduction
Maternal and child mortality remains a major public health concern in Ethiopia. Improving the practice of short inter-pregnancy intervals is a key strategy to reduce neonatal and maternal mortality. Several primary studies conducted in Ethiopia have revealed the practice short inter-pregnancy interval. However, inconsistencies among these studies have been observed, and no review has been conducted to report the combined magnitude, determinants, and complications. Therefore, this review aims to estimate the national magnitude, determinants, and complications of short inter-pregnancy intervals among pregnant mothers in Ethiopia.
Methods
Following the PRISMA standards, we systematically reviewed and meta-analyzed articles from PubMed, Cochrane Library, and Google Scholar that investigated the magnitude, determinants, and complications of a short inter-pregnancy interval. The Q and I2 tests were used to assess heterogeneity across studies. We utilized a weighted inverse variance random effects model to evaluate the national magnitude and effect size of linked covariates. To examine publication bias, we employed a funnel plot and Egger's regression test. A sensitivity analysis was also performed to determine the impact of the studies.
Results
The analysis included a total of twenty-six studies. The pooled magnitude of a short inter-pregnancy interval in Ethiopia was found to be 44.054% (95% CI 32.735–55.372; I2 = 100%; P < 0.001). no formal education (AOR = 1.889; 95% CI 1.261–2.517; I2 = 3.42%; P = 0.41), never used contraceptive methods (AOR = 3.38; 95% CI 2.41–4.35; I2 = 44.9%; P = 0.027), breastfeeding duration of less than 24 months (AOR = 6.69; 95% CI 4.77–8.52; I2 = 95.5%; P = 0.00), having a preceding female child (AOR = 1.45; 95% CI 0.88–2.015; I2 = 16.4%; P = 0.301), and experiencing fetal complication (AOR = 3.55; 95% CI 1.986–5.122; I2 = 0%; P = 0.482).
Conclusion
A substantial number of women in Ethiopia continue to have a short inter-pregnancy interval. To address this issue, it is crucial to focus on empowering women through education and raising awareness about the importance of spacing pregnancies adequately. Efforts should be made to improve breastfeeding practices, promoting the recommended duration of at least 24 months.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12978-024-01893-z.
Keywords: Inter pregnancy interval, Pregnancy interval, Short pregnancy interval, Ethiopia
Background
The World Health Organization (WHO) defines the inter pregnancy interval as the time period between a live birth and a subsequent pregnancy [1, 2]. According to WHO, it is recommended that there should be a minimum of 2 years between a woman's previous delivery and her subsequent conception [2]. The WHO's recommendation for a minimum inter pregnancy interval of 2 years is supported by research findings. Studies have shown that both short inter pregnancy intervals (less than 24 months) and long intervals (greater than 59 months) are associated with heightened risks of various adverse outcomes. These include preterm birth; low birth weight; small-for-gestational-age birth; and an increased risk of preeclampsia [3–7].
Maternal and neonatal mortality rates remain significant public health concerns globally, with low-income countries facing disproportionately higher rates compared to high-income countries [6, 8–10]. The 2017 WHO report highlights the significant burden of maternal and neonatal mortality in Sub-Saharan Africa (SSA) and South Asia. According to the report, SSA and South Asia together contribute to 87% of the estimated 358,000 maternal deaths and over three-quarters of the 3.6 million neonatal deaths that occur annually worldwide. Moreover, Sub-Saharan Africa specifically faces a high maternal mortality ratio, with approximately 533 maternal deaths per 100,000 live births [11, 12]. Ethiopia has faced a higher number of infant and neonatal deaths compared to the average rates of infant and neonatal mortality reported in Africa. This disparity highlights the urgent need for targeted interventions and improvements in maternal and child healthcare in Ethiopia [13].
A short birth interval has been associated with a range of adverse perinatal, neonatal, and child health outcomes, as well as negative effects on maternal health. Some of these adverse outcomes include: Preterm birth, Low birth weight, perinatal death and stillbirth Antepartum haemorrhage and Eclampsia [7, 14–16]. Moreover, closely spaced birth intervals can contribute to accelerated population growth, which can pose challenges to development efforts [17]. Moreover, when a new baby arrives, the family is likely to invest more of its limited resources in the care of the new-born, leaving the other children with an inadequate share of resources [17, 18].
In a study conducted in several African countries, including Rwanda, Uganda, Cameroon, and Ethiopia, the magnitude of short inter pregnancy intervals ranged from 20 to 59% [19–22]. Closely spaced births can indeed have a potentially devastating impact on both individuals and society. Conversely, optimal birth spacing offers significant health, social, and economic benefits for families [23]. Currently, in developing countries, over 200 million women desire to either space or limit their pregnancies but lack access to appropriate family planning (FP) options [24]. Demographic Health Survey (DHS) studies show a substantial body of literature indicating that factors such as maternal education, maternal age, early marriage, inability to breastfeed, and inadequate knowledge, attitude, and practice towards modern contraceptive use serve as determinants for the occurrence of short inter-pregnancy intervals [17].
Moreover, the progress made in reducing under-5 mortality has stagnated in comparison to the reduction in neonatal mortality [25]. Optimal child birth spacing is widely recognized as a crucial factor for the health of women and their children [24]. Hence, it is crucial to identify factors that can influence the inter-pregnancy interval of women; especially in countries burdened with high fertility rates and maternal mortality rates (MMR) such as Ethiopia. The magnitude, determinants, and complications of short inter-pregnancy intervals have been primarily studied in underdeveloped countries, including Ethiopia. However, it is important to note that while one related systematic review and meta-analysis was conducted, the majority of primary research on the magnitude and determinant factors were not included [1, 15, 16, 26–28].
However, the reported findings regarding the magnitude, determinants, and complications of short inter-pregnancy intervals in Ethiopia are inconsistent. To the best of the investigators' knowledge, no systematic review or meta-analysis has been conducted to address the conflicting findings. Furthermore, addressing the magnitude, determinants, and complications of short inter-pregnancy intervals can help improve interventions and reduce the burden among pregnant mothers. Consequently, this systematic review and meta-analysis were carried out to analyze the magnitude, determinants, and complications of short inter-pregnancy intervals among pregnant mothers in Ethiopia.
Methods
Reporting
The findings of this review were presented in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) statement recommendations (see the Supplementary file-PRISMA checklist) and registered at Prospero with no CRD42023483960.
Searching strategy and information sources
During our research, we identified papers from reputable sources such as PubMed, the Cochrane library, and Google Scholar that presented data on the magnitude, determinants, and complications associated with short inter pregnancy intervals among pregnant mothers in Ethiopia. To enhance the search for additional publications, the search used Medical subject headings (MeSH) terms and keywords, combinations, and snowball searching in the references list of papers found through the data base search. Articles with missing or incorrect data were resolved by contacting the corresponding authors. Unpublished studies were obtained from international and local organizations' and universities' official websites.
Medical Subject Headings (MeSH) terms and keywords were utilized to conduct the search. The search phrases were used individually, in combination, or both, employing "OR" or "AND" operators. The main search terms and phrases included Ethiopia, inter-pregnancy, pregnancy interval, short pregnancy interval, optimal pregnancy interval, and pregnancy spacing. Various Boolean operators were employed to develop the search strategies. Notably, the following search strategy was employed to match the comprehensive PubMed database: (prevalence OR magnitude OR epidemiology) AND (causes OR determinants OR related factors OR predictors OR risk factors) AND (inter-pregnancy OR short pregnancy interval [MeSH Terms]) AND (optimal pregnancy, pregnancy interval, and pregnancy spacing [MeSH Terms] OR pregnancy timing) AND Ethiopia.
In addition, we conducted a thorough examination of the reference lists of the remaining papers to identify any new studies relevant to this review. To remove duplicate studies, we established specific criteria for study selection and eligibility. The extracted studies were then imported into the reference manager program EndNote version 21. Prior to retrieving full-text publications, two investigators (GY and BDT) independently assessed the selected studies based on their titles and abstracts. Subsequently, we screened the full-text papers using pre-determined inclusion criteria. In cases of disagreement, a consensus meeting involving additional reviewers (MA, ASB, BBA, ESL, ABZ and AW) was held to finalize the selection of studies to be included in the systematic review and meta-analysis.
Inclusion and exclusion criteria
All observational studies, including cross-sectional, case–control, and cohort studies, were considered for inclusion in the research. The study focused on research published in English between 2010 and 2023 in Ethiopia, examining the magnitude of the inter-pregnancy interval, one or more associated factors, and/or its complications. Unpublished works were also taken into consideration. The analysis excluded editorials, anonymous reports, qualitative studies, and citations without an abstract or full text. Additionally, studies that did not reveal significant findings were disregarded. The study included pregnant mothers who received prenatal care during the data collection period and met the inclusion and exclusion criteria of the selected studies. Women with less than two births, those with medical illnesses, and those unable to provide information due to illness were excluded.
Quality assessment
After integrating the database search results, duplicate articles were removed using EndNote (version 21). The quality appraisal checklist developed by the Joanna Briggs Institute (JBI) was used for assessing the quality of the included studies [29, 30]. The quality of the studies was assessed by four independent reviewers, and the appraisal process involved exchanging notes. In cases where there was disagreement among the reviewers, the scores were averaged to reach a consensus. One paper was evaluated by two authors. Studies that scored 5 or higher were considered low risk or of good quality. All studies meeting these criteria were included in the analysis. [29, 30] whereas, studies with a score of 4 or lower were considered high risk or of poor quality and therefore were excluded from the analysis.
Data extraction
The authors created an Excel file as the data extraction form, which contained the following information: author's name, publication year, research region, study design, sample size, magnitude of inter-pregnancy interval, and categories of reported factors. Four papers were randomly selected to test the data extraction sheet. After conducting the experiment, the extraction form was modified accordingly. The two authors worked collaboratively to extract the data using the revised extraction form. The accuracy of the extracted data was independently verified by the third, fourth, and fifth authors. If any disputes arose among the reviewers, discussions involving a third and fourth reviewer were held to resolve them. Data errors were rectified by cross-referencing with the included papers. In cases where incomplete data was received, the study was excluded after two email attempts to contact the corresponding author.
Outcome measurement
The inter-pregnancy interval was defined as the time in completed months from the reported date of live birth of the previous child to the self-reported last normal menstrual period (LNMP). Most participants were aware of the date of birth of their previous child and the LNMP of their current pregnancy. However, for participants who did not know the precise date of conception and/or the birth date of the previous child, the mid-date of the month was used as the birth date of the previous child or the date of conception for the current pregnancy. Consequently, the inter-pregnancy interval was calculated by subtracting the date of birth of the last child (previous child) from the date of conception of the current pregnancy (IPI = date of conception (LMP)—date of birth of the previous child). Therefore, a short inter-pregnancy interval was defined as an interval less than 24 months [31, 32].
Statistical analysis
After extracting the data in Microsoft Excel format, we imported it into STATA version 17.0 statistical software for further analysis. To calculate the standard error for each study, we employed the binomial distribution formula. For pooling the overall magnitude of short inter-pregnancy interval, a random-effects meta-analysis was utilized [33]. Forest plots were employed to present the pooled prevalence of short inter-pregnancy interval, along with 95% confidence intervals (CI), and the odds ratio (OR) with 95% CI to visualize the factors associated with short inter-pregnancy interval. To assess heterogeneity among the studies, we examined P-values, inverse variance (I2), and Cochrane's Q statistics (Chi-square) [34].
In this study, an I2 statistic value of zero indicates true homogeneity, meaning that there is no significant heterogeneity among the studies. The values of 25%, 50%, and 75% represent low, moderate, and high heterogeneity, respectively [33, 35, 36]. For the data identified as heterogeneous, we performed our analysis using a random-effects model. Additionally, subgroup analysis was conducted based on the study region, sample size, and year of publication. In cases where statistical pooling was not feasible, non-pooled data was presented in tabular form. To assess the impact of individual studies on the overall estimation, sensitivity analysis was employed. Publication bias was evaluated using a funnel plot and, more objectively, through Egger's regression test [34].
Result
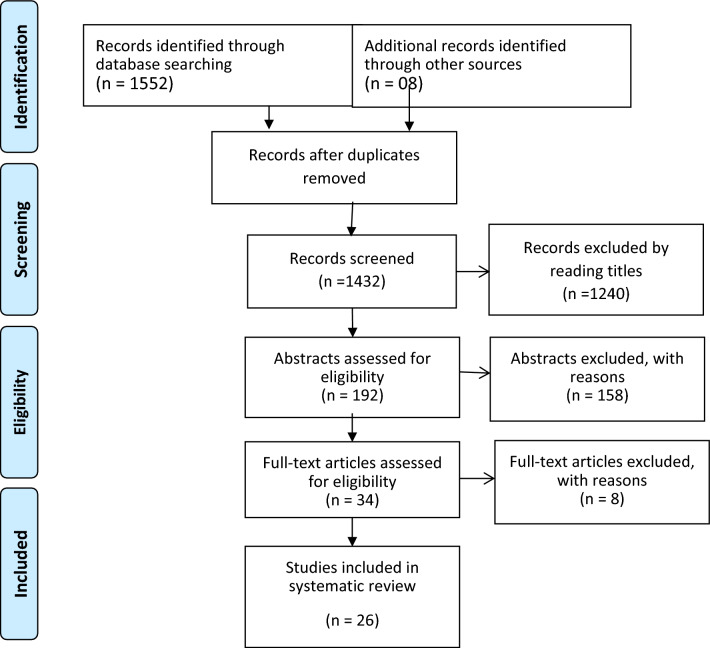
During the study selection process, a total of 1560 studies were identified through electronic searches of databases. After removing duplicates, 1432 studies conducted between 2010 and 2023 remained. Out of these, 1240 studies were excluded based on title screening alone. After reading the abstracts of the remaining 192 studies, 158 were further excluded. Finally, 34 studies underwent a full-text review, and 26 articles with a total of 35,226 study participants were selected for the analysis of the magnitude and/or determinant factors and its complication to short inter-pregnancy interval (Fig. 1).
Fig. 1.
PRISMA flow diagram showed the results of the search and reasons for exclusion
Characteristics of included studies
Table one summaries the characteristics of twenty six included Studies in the Systematic Review and Meta-Analysis [15, 16, 26–28, 37–57]. 08 studies were found in Amhara region [26, 41–43, 45, 52, 56, 57]. 05 in Oromia region, 04 in south nation nationalities people region [16, 27, 46, 51, 53], 06 in Ethiopia from EDHS report and meta-analysis [38, 40, 44, 47–49], 02 in Tigray [54, 55] and 01 in Somalia region [28]. Most of the studies were published between 2013 and 2021. The studies included participants, ranging from 299 [57] to 8448 [38] (Table 1).
Table 1.
Distribution of studies on the magnitude, determinant factors, and complications of short inter pregnancy interval among pregnant mothers (2010–2023)
| Author/References | Publication year | Region | study design | sample size | p | Quality score |
|---|---|---|---|---|---|---|
| Abdurahman Kedir et al. | 2021 | Somalie | Case control | 388 | 7/8 | |
| Belayneh Hamdela et al. | 2021 | SNNPS | Case Control | 365 | 810/ | |
| Desalegn Markos et al. | 2020 | Ethiopia | Cross Section | 8448 | 45.80 | 6/8 |
| Desta Hailu et al. | 2016 | SNNPS | Case control | 8/10 | ||
| Dereje Tsegaye et al. | 2017 | Oromia | Cross section | 811 | 51.2 | 7/8 |
| Gedefaye Nibret et al. | 2022 | Amhara | Case–control | 7/10 | ||
| Gemechu Edasa et al. | 2021 | SNNPS | Case–control | 7/10 | ||
| Getayeneh A(srma) et al. | 2022 | Ethiopia | SRMA | 3234 | 49.53 | 7/8 |
| Habtamu Shimels et al. | 2020 | Amhara | Case control | 654 | 8/10 | |
| Hana Mamoet al. | 2021 | Amhara | Cross-sectional | 496 | 40.9 | 7/8 |
| Jemberu Chane et al. | 2021 | Amhara | Cross-sectional | 482 | 7/8 | |
| Kalayu Brhane et al. | 2022 | Ethiopia | Cross-sectional | 3664 | 6.0 | 6/8 |
| Leta Gurmu et al. | 2022 | Amhara | Cohort | 438 | 8/11 | |
| Musa Mohammed et al. | 2022 | Oromia | Cross-sectional | 484 | 56 | 7/8 |
| Setognal Birara et al. | 2020 | Ethiopia | Cross sectional | 2683 | 46 | 7/8 |
| Shikur Mohammed et al. | 2020 | Ethiopia | SRMA | 1089 | 36.78 | 7/8 |
| Yitayish Damtie et al. | 2021 | Ethiopia | SRMA | 5682 | 46.9 | 7/8 |
| Samuel Yohannes et al. | 2011 | SNNPS | Cross sectional | 844 | 57 | 7/8 |
| Zenebu Begna et al. | 2013 | Oromia | Case control | 652 | 7/10 | |
| Gizachew Assefa et al. | 2013 | Amhara | Cohort | 613 | 7/11 | |
| Seifadin Ahmed et al. | 2019 | Oromia | Cross sectional | 647 | 49.1 | 7/8 |
| Merhawi Brhane et al. | 2019 | Tigray | Cohort | 460 | 8/11 | |
| Solomon Weldemariam | 2019 | Tigray | Cross sectional | 803 | 23.3 | 7/8 |
| Amare Genetu et al. | 2019 | Amhara | Cross sectional | 418 | 40.9 | 7/8 |
| Girma Bacha et al. | 2019 | Oromia | Cross sectional | 314 | 59.9 | 6/8 |
| Mulugeta Wodaje et al. | 2023 | Amhara | Cross section | 299 | 51.5 | 7/8 |
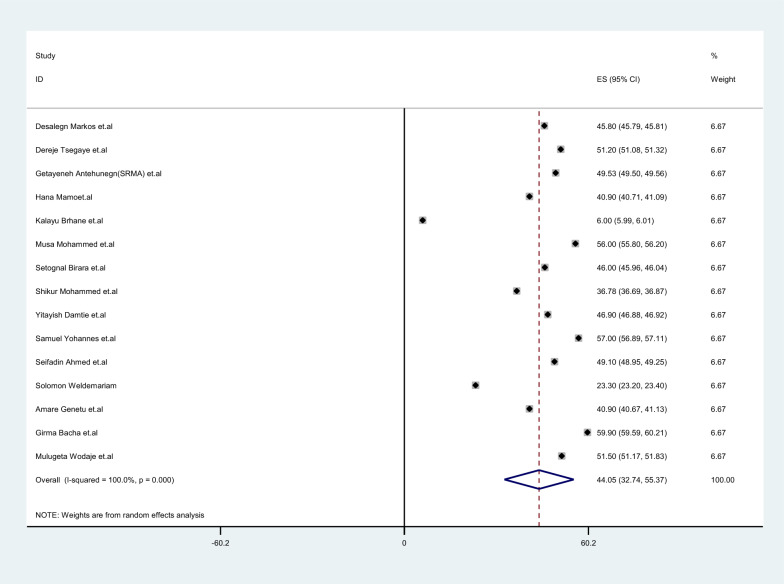
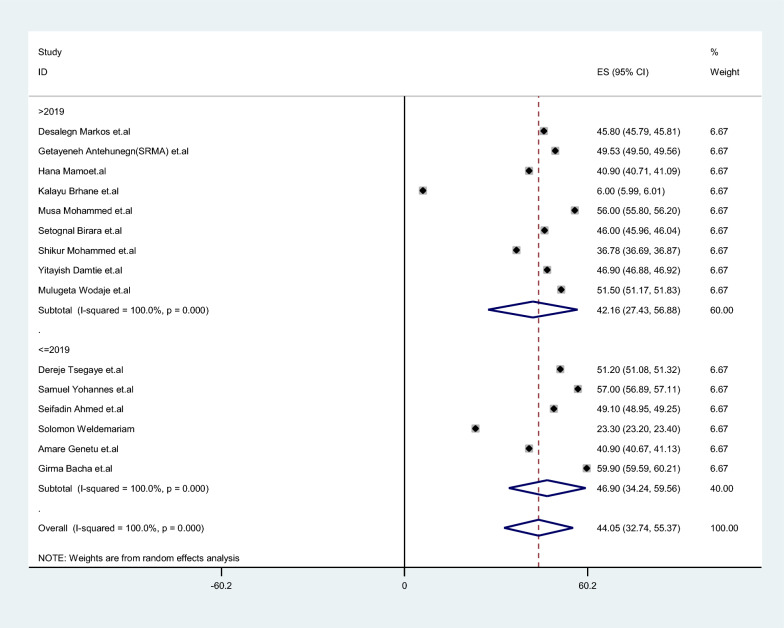
Meta-analysis magnitude determinates factors and its complication of short inter pregnancy interval among pregnant mother in Ethiopia. Most of the studies (n = 15) had reported the magnitude short inter pregnancy interval [16, 27, 38, 40, 42, 44, 46–50, 53, 55–57]. The magnitude of short inter pregnancy interval was ranged from 6.0% [44] up to 59.9% [16]. The random-effects model analysis from those studies revealed that, the pooled magnitude of short inter pregnancy interval among pregnant mother in Ethiopia was found to be 44.054% (95%CI (32.735–55.372); I2 = 100% %; P < 0.001) (Fig. 2).
Fig. 2.
The pooled magnitude of short inter pregnancy interval among pregnant mothers in Ethiopia
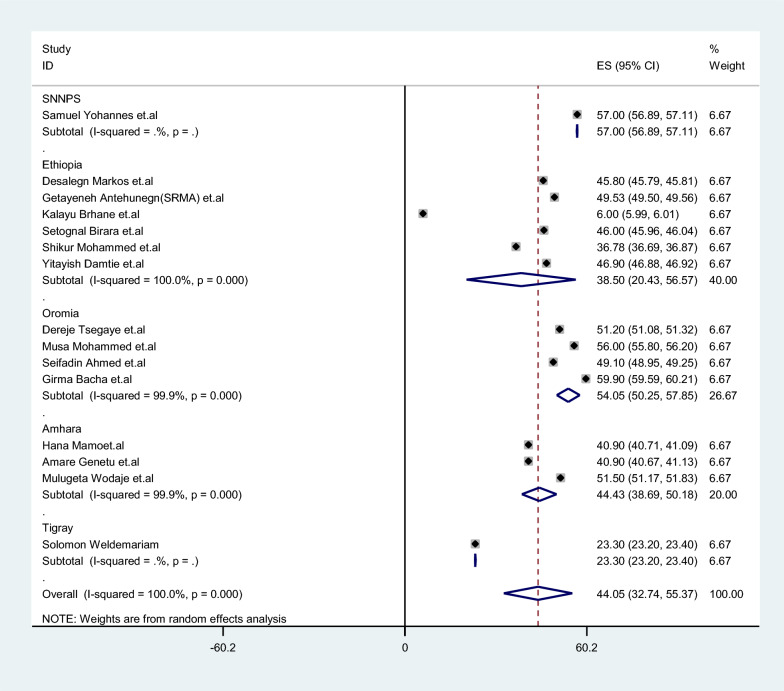
Subgroup analysis of the magnitude of short inter pregnancy interval among pregnant mother in Ethiopia
The subgroup analysis conducted in this meta-analysis involved stratifying the studies based on region, sample size, and year of publication. By doing so, the researchers were able to examine the magnitude of short inter pregnancy intervals among pregnant mothers in Ethiopia more closely. The results of the analysis revealed that the estimated magnitude of short inter pregnancy intervals among pregnant mothers in Ethiopia was found to be 44.054% (95% CI 32.735–55.37) (Fig. 2). Based on the subgroup analysis stratified by study region, the magnitude of short inter pregnancy intervals among pregnant mothers was found to be 57.00% (95% CI 56.885–57.115) in the South Nation and Nationality, 38.502% (95% CI 20.434–56.569) in Ethiopia EDHS data and meta-analysis, 54.048% (95% CI 50.246–57.85) in the Oromia region, 44.432% (95% CI 38.688–50.175) in the Amhara region, and 23.3% (95% CI 23.197–23.403) in the Tigray region (Fig. 3, Supplementary Table 1).
Fig. 3.
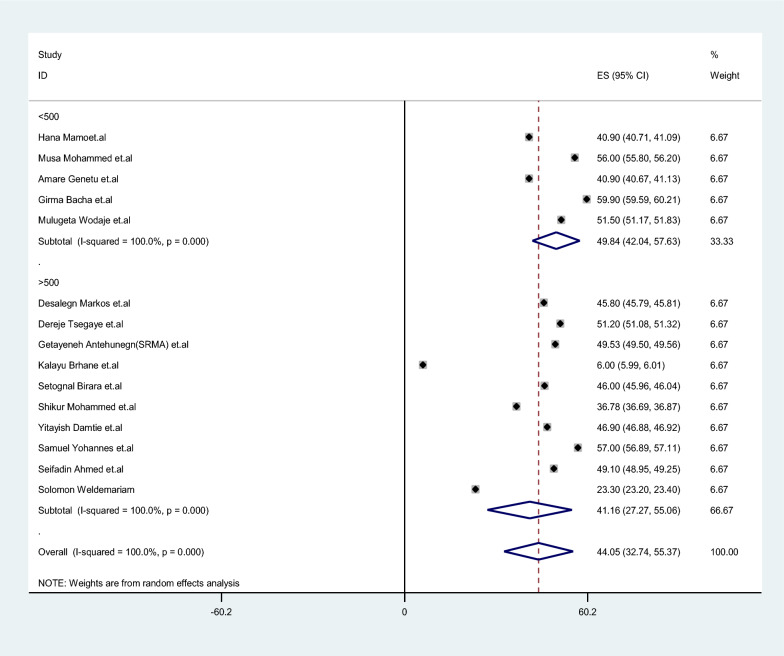
Subgroup analysis of the magnitude of short inter pregnancy interval among pregnant mothers in Ethiopia by region category
Based on the study sample size, the magnitude of short inter pregnancy intervals among pregnant mothers was found to be 49.84% (42.045–57.635) in samples with a size less than 500, while it was 41.161% (27.266–55.056) in samples with a size greater than 500 (Fig. 4, Supplementary Table 2). Moreover, based on the year of publication, the magnitude of short inter pregnancy intervals among pregnant mothers was found to be 42.157% (27.429–56.885) from 2019 up to 2023, while it was 46.9% (34.238–59.562) from studies conducted from 2010 up to 2018 (Fig. 5, Supplementary Table 3).
Fig. 4.
Subgroup analysis of short inter pregnancy interval among pregnant mothers in Ethiopia by sample size
Fig. 5.
Subgroup analysis of short inter pregnancy interval among pregnant mothers in Ethiopia by publication year
Sensitivity analysis
We conducted a leave-one-out sensitivity analysis to investigate the potential source of heterogeneity in the analysis of the magnitude of short inter pregnancy intervals among pregnant mothers. The results of this analysis demonstrated that our findings were not reliant on a single study. The pooled estimated magnitude of short inter pregnancy intervals among pregnant mothers ranged from 43.2% (95% CI 31.48–54.919) [46] to 46.769% (95% CI 44.98–48.55) after deletion of a single study (Table 2 and Supplementary Fig. 1).
Table 2.
A sensitivity analysis of the magnitude of short inter pregnancy interval among pregnant mothers in Ethiopia
| Study omitted | Coef. | [95% Conf. Interval] | |
|---|---|---|---|
| Abdurahman Kedir Roble et.al | 44.053909 | 32.735352 | 55.372471 |
| Belayneh Hamdela et al. | 44.053909 | 32.735352 | 55.372471 |
| Desalegn Markos et al. | 43.929211 | 30.402849 | 57.455574 |
| Desta Hailu et al. | 44.053909 | 32.735352 | 55.372471 |
| Dereje Tsegaye et al. | 43.543472 | 31.808764 | 55.278179 |
| Gedefaye Nibret et al. | 44.053909 | 32.735352 | 55.372471 |
| Gemechu Edasa et al. | 44.053909 | 32.735352 | 55.372471 |
| Getayeneh Antehunegn et al. | 43.662762 | 31.598547 | 55.726974 |
| Habtamu Shimels et al. | 44.053909 | 32.735352 | 55.372471 |
| Hana Mamoet al. | 44.279186 | 32.550213 | 56.008163 |
| Jemberu Chane et al. | 44.053909 | 32.735352 | 55.372471 |
| Kalayu Brhane et al. | 46.769745 | 44.981956 | 48.557529 |
| Leta Gurmu et al. | 44.053909 | 32.735352 | 55.372471 |
| Musa Mohammed et al. | 43.200623 | 31.482044 | 54.919205 |
| Setognal Birara et al. | 43.914906 | 31.885887 | 55.943928 |
| Combined | 44.05391 | 32.735351 | 55.372469 |
Publication bias
We conducted a publication bias assessment and observed that the funnel plot displayed a symmetrical distribution, indicating the absence of publication bias. This finding was further supported by the Egger’s regression test, which yielded a P-value of 0.55 (Supplementary Fig. 2 and Supplementary Table 4). Factors Associated with Short Inter pregnancy Interval among Pregnant Mothers Out of the total included studies, 21 studies revealed the factors associated with a short inter pregnancy interval among pregnant mothers (Table 1).
Factors associated with short inter pregnancy interval
No formal education
Out of the total included studies, eleven studies reported a significant association between no formal education and short inter pregnancy interval among pregnant mothers in Ethiopia (Table 3). Among these studies, the highest risk factor was an (AOR) of 5.28 (95% CI 2.26, 12.36) [28] and lowest risk factor AOR = 1.23 (1.05, 1.45) compared to educated mothers. Regarding the heterogeneity test for no formal education, the Galbraith plot revealed heterogeneity when combining the results of eleven studies. The forest plot displayed the overall estimate of the (AOR) for no formal education as 1.889 (95% CI 1.261–2.517) I2 3.4%, P 0.41.The I-squared (I2) value indicated heterogeneity of 3.42%, and the P-value was 0.41. These findings suggest the presence of heterogeneity in the study results. Furthermore, the I-squared (I2) and P-value also indicated the absence of publication bias (Supplementary Fig. 3).
Table 3.
Determinant factors associated with short inter pregnancy interval among pregnant mothers in Ethiopia
| Variables | Odds ratio (95%CI) | Author | Year | Pooled AOR (95%CI) | I2 (P-value) |
|---|---|---|---|---|---|
| No formal education | 5.28 (2.25, 12.36) | Abdurahman et al. [21] | 2021 | 1.889 (1.261–2.517) | 3.42 |
| 1.23 (1.05, 1.45) | Desalegn et al. [32] | 2020 | |||
| 2.36 (1.23, 4.52) | Desta et al. [26] | 2016 | |||
| 2.56 (1.6, 3.42) | Derejeet al. [31] | 2017 | |||
| 2.17 (0.92, 5.15) | Kalayu et al. | 2022 | |||
| 4.35 (2.12, 9.09) | Musa et al. | 2022 | |||
| 3.7 (1.85, 20) | Setognal et al. | 2020 | |||
| 1.89 (1.15, 3.37) | Zenebu et al. | 2013 | |||
| 3.05 (1.68, 3.83) | Girma et al. | 2019 | |||
| 5.25 (1.2, 17.1) | Mulugeta et al. | 2023 | |||
| 2.15 (1.19, 3.88) | Gedefaye et al. | 2022 | |||
| Never used contraceptive methods | 3.69 (2.02, 6.72) | Abdurahman et al. | 2021 | 3.38 (2.41–4.35) | 44.9 |
| 2.79 (1.58, 4.94) | Desta et al. | 2016 | |||
| 4.12 (2.71, 5.82) | Dereje et al. | 2017 | |||
| 11.2 (5.95, 21.5) | Habtamu | 2020 | |||
| 2.09 (1.12, 3.89) | Musa et al. | 2022 | |||
| 5.91 (4.02, 8.69) | Zenebu et al. | 2013 | |||
| 4.29 (3.0, 6.13) | Gizachew et al. | 2013 | |||
| 1.66 (1.07, 2.77) | Seifadin et al. | 2019 | |||
| 8.15 (4.17, 15.94) | Amare et al. | 2019 | |||
| 1.94 (1.09, 3.45) | Girma et al. | 2019 | |||
| 6.46 (3.882,23.008) | Mulugeta et al. | 2023 | |||
| 2.44 (1.55, 3.82) | Solomon et al. | 2019 | |||
| 2.51 (1.23, 3.71) | Hana et al. | 2021 | |||
| 3.87 (2.29, 6.53) | Yitayish et al. | 2021 | |||
| 1.56 (1.1, 2.21) | Samuel et al. | 2021 | |||
| 3.48 (1.74, 6.95) | Gedefaye et al. | 2022 | |||
| Duration of breastfeeding for lessthan24 | 66.03(34.6, 126) | Desalegn et al. | 2020 | 6.69(4.77–8.62) | 95.5 |
| 5.36 (3.43, 6.34) | Dereje et al. | 2017 | |||
| 3.59 (2.06, 6.24) | Gedefaye et al. | 2022 | |||
| 4.1 (1.83, 9.17) | Gemechu et al. | 2021 | |||
| 0.45 (0.245, 0.811) | Habtamu et al. | 2020 | |||
| 2.62 (1.32, 5.23) | Hana et al. | 2021 | |||
| 2.6 (1.53, 4.41) | Musa et al. | 2022 | |||
| 1.26 (1.21, 1.31) | Setognal et al. | 2020 | |||
| 16.9 (2.69, 106.4) | Yitayish et al. | 2021 | |||
| 4.56 (1.11, 18.69) | Samuel et al. | 2011 | |||
| 6.12 (2.79, 13.38) | Gizachew et al. | 2013 | |||
| 9.6 (8.93, 19.39) | Seifadin et al. | 2019 | |||
| 7.01 (3.64, 13.46) | Solomon et al. | 2019 | |||
| 4.72 (1.12, 20.6) | Amare et al. | 2019 | |||
| 3.09 (1.38, 6.96) | Girma et al. | 2019 |
Regarding the publication bias for no formal education, the funnel plot analysis indicated an asymmetrical distribution. To identify the potential source of heterogeneity in the analysis of the pooled estimate of no formal education as a risk factor for short inter pregnancy interval, we conducted a leave-one-out sensitivity analysis. The results of this analysis revealed that our findings were not reliant on a single study. The pooled estimate of no formal education varied between 1.889 (95% CI 1.26–2.51) and 2.75 (95% CI 1.811–3.698) after excluding each individual study.
Never used contraceptive methods
Out of the total studies, sixteen studies found a significant association between never using contraceptive methods and short inter pregnancy interval among pregnant mothers. Among these studies, the highest risk factor was an (AOR) of 11.2 (95% CI 5.95, 21.5) [41] and lowest risk factor AOR = 1.56 (1.1, 2.21) [50] compared to their counterparts (Table 3).
Regarding the heterogeneity test for never used contraceptive methods, the Galbraith plot demonstrated heterogeneity when combining the results of sixteen studies. The forest plot displayed the overall estimate of the (AOR) for never used contraceptive methods as 3.38 (95% CI 2.41–4.35), I2 44.9%, P 0.027. The I2 value indicated heterogeneity of 44.9%, and the P-value was also indicated the presence of publication bias (Supplementary Fig. 4). Regarding the publication bias for never used contraceptive methods, the funnel plot analysis revealed an asymmetrical distribution. To identify the potential source of heterogeneity in the analysis of the pooled estimate of never used contraceptive methods as a risk factor for short inter pregnancy interval, a leave-one-out sensitivity analysis was conducted. The results of this analysis showed that the findings were not reliant on a single study.
The pooled estimate of never used contraceptive methods varied between 1.56 (95% CI 0.051–3.069) and 11.2 (95% CI 6.084–16.316) after excluding each individual study. Due to the presence of publication bias, a trim and fill analysis was conducted, resulting in the addition of six studies. The total number of studies included in the analysis became twenty two. The pooled estimate of the Adjusted Odds Ratio (AOR) for never use contraceptive status was found to be 9.38 (95% CI 5.034, 17.4840). The I2 value indicated heterogeneity of 95.5%, and the P-value was 0.036 (Supplementary Fig. 5).
Duration of breastfeeding for lessthan24
Out of the total studies, fifteen studies were significantly associated with short inter pregnancy interval among pregnant mothers in Ethiopia. Among these studies, the highest risk factor was an (AOR) of 66.03 [95% CI 58.32–73.73)] [38] and lowest risk factor AOR = 1.26(0.826, 1.694) [47] compared to those who breastfed for a duration greater than 24 months. When the results of the fifteen studies were combined, the forest plot demonstrated an overall estimate of the (AOR) for duration of breastfeeding less than 24 months among pregnant mothers as 6.69 (95% CI 4.77–8.62) I2 95.5, P 0.00. The I2 value indicated a high level of heterogeneity at 95.5%, Suggesting substantial variability among the study results. The P-value was 0.00, indicating statistical significance. Additionally, both the I2 and P-value indicated the presence of heterogeneity and potential publication bias (Supplementary Fig. 6).
Regarding heterogeneity test, Galbraith plot showed heterogeneity regarding test of publication bias a funnel plot showed an asymmetrical distribution. Egger’s regression test P-value was 0.010, which indicated the presence of publication bias (Supplementary Fig. 7). Trim and fill analysis were done, and eight study were added and the total number of studies become 23 and the pooled estimate of AOR for Duration of breastfeeding for less than 24 was 2.155 [95%CI (1.704–2.725); I2 = 95.5%, P = 0.00] (Supplementary Fig. 8).
Residence
Out of the total studies, five studies demonstrated a significant association between residence and short inter pregnancy interval among pregnant mothers. Among these studies, the highest risk factor was an (AOR) of 6.9 (95% CI 3.32–14.59) [43] and lowest risk factor AOR = 1.47 (0.83, 2.61) [44] compared to those who resided in urban areas. When the results of the five studies were combined, the forest plot displayed an overall estimate of the (AOR) for residence as 2.369 (95% CI 1.048–3.689) I2 36.4%, P 0.185. The I2 value indicated a moderate level of heterogeneity at 35.4%, suggesting some variability among the study results. The P-value for heterogeneity was 0.185, indicating no statistically significant heterogeneity (Supplementary Fig. 9).
Furthermore, the Galbraith plots, used to assess heterogeneity, demonstrated homogeneity among the studies. The funnel plot, used to evaluate publication bias, displayed a symmetrical distribution, indicating the absence of publication bias. Additionally, the Egger's regression test resulted in a P-value of 0.214, further supporting the absence of publication bias. To explore the potential sources of heterogeneity, a leave-one-out sensitivity analysis was performed. The results of this analysis revealed that the findings were not heavily reliant on a single study, suggesting robustness in the pooled estimate of residence as a risk factor for short inter pregnancy interval.
Poor wealth index
Out of the total studies, four studies demonstrated a significant association between a poor wealth index and short birth interval among pregnant mothers. Among these studies, the highest risk factor was an (AOR) of 4.89 (95% CI 1.58–6.39) [15] and lowest risk factor AOR = 1.33 (1.26, 2.22) [51], compared to those who had a good wealth index (Table 3). Combining the results of three studies, the forest plot showed an overall estimate of the (AOR) for a poor wealth index as 2.686 (95% CI 0.916–4.456) I2 86.2, P 0.00. The I2 value indicated a high level of heterogeneity at 86.2%, suggesting substantial variability among the study results. The P-value for heterogeneity was 0.00, indicating statistical significance. Regarding publication bias, the funnel plot displayed an asymmetrical distribution, indicating the potential presence of publication bias. The Egger's regression test resulted in a P-value of 0.00, further supporting the presence of publication bias (Supplementary Fig. 10).
A leave-one-out sensitivity analysis was conducted to identify potential sources of heterogeneity in the analysis of the pooled estimate of a poor wealth index as a risk factor for a short inter pregnancy interval among pregnant mothers. The results of this analysis showed that the findings were not dependent on a single variable, suggesting some robustness in the results. Due to the presence of publication bias, a trim and fill analysis was performed, adding two studies to the analysis, resulting in a total of six studies. The pooled estimate of the AOR for a poor wealth index as a risk factor for a short inter pregnancy interval among pregnant mothers was calculated to be 5.1680 (95% CI 2.136–12.5060). The I2 value reduced to 16.4%, indicating a lower level of heterogeneity, and the P-value was 0.036, indicating statistical significance (Supplementary Fig. 11).
Preceding child being female
In eight studies, a significant association was found between the preceding child being female and a short birth interval among pregnant mothers. Among these studies, the highest risk factor was an AOR of 5.7 (95% CI 3.180–10.3) [15], and the lowest risk factor was an AOR of 1.13 (95% CI 0.74–1.71) [44], suggesting a smaller effect or no significant association compared to the counterpart. Regarding the heterogeneity test and combining the results of eight studies, the forest plot showed an overall estimate of the AOR for the preceding child being female as 1.45 (95% CI 0.88–2.015) I2 16.4%, P 0.301. The I2 value indicated a low level of heterogeneity at 16.4%, suggesting minimal variability among the study results. The P-value for heterogeneity was 0.301, indicating no significant heterogeneity (Supplementary Fig. 12). Regarding the heterogeneity test, the Galbraith plot showed homogeneity, which is consistent with the low level of heterogeneity indicated by the I2 value. Regarding publication bias, the funnel plot displayed a symmetrical distribution, suggesting the absence of publication bias. The Egger's regression test resulted in a P-value of 0.214, further supporting the absence of publication bias. A leave-one-out sensitivity analysis was conducted to identify potential sources of heterogeneity in the analysis of the pooled estimate of residence as a risk factor for a short inter pregnancy interval. The results of this analysis showed that the findings were not dependent on a single study, suggesting some robustness in the results.
Fetal complications
In five studies, a significant association was found between fetal complication and a short inter pregnancy interval among pregnant mothers. Among these studies, the highest risk factor was an AOR of 6.85 (95% CI 3.07–15.3) [54], and the lowest risk factor was an AORof 2.1 (95% CI 1.16–3.82) [45], compared to the counterpart. Regarding the heterogeneity test and combining the results of eight studies, the forest plot showed an overall estimate of the AORfor fetal complications as 3.55 (95% CI 1.986–5.122) I2 0.00, P 0.482. The I2 value indicated no heterogeneity at 0%, suggesting no significant variability among the study results. The P-value for heterogeneity was 0.482, further supporting the absence of of publication bias (Supplementary Fig. 13).
Regarding publication bias, the funnel plot displayed an asymmetrical distribution, suggesting the potential presence of publication bias. The Egger's regression test resulted in a P-value of 0.011, indicating the presence of publication bias. Due to the presence of publication bias, a trim and fill analysis was performed, adding two studies to the analysis, resulting in a total of seven studies. The pooled estimate of the AOR for adverse perinatal outcomes was calculated to be 2.94 (95% CI 1.347–4.540). The I2 value remained at 16.4%, indicating a low level of heterogeneity, and the P-value was 0.286, suggesting no significant heterogeneity (Supplementary Fig. 14).
Discussion
This systematic review and meta-analysis aimed to evaluate the magnitude of short inter pregnancy intervals, associated factors, and fetal complications among pregnant mothers in Ethiopia. The analysis included a total of 26 studies that met the inclusion criteria. Among the included studies, 15 of them reported the magnitude of short inter pregnancy intervals. After pooling the data from these studies, the meta-analysis found that the overall pooled magnitude of short inter pregnancy intervals among pregnant mothers in Ethiopia was estimated to be 44.054%, with a 95% (CI) ranging from 32.735 to 44.37%.
Although WHO recommended optimal pregnancy spacing to ensure the health of the mother and The newborn [2]. 44.054%, [95% CI (32.735, 44.37 of reproductive age women practiced short inter pregnancy interval in Ethiopia. The finding of this study is in line with the Ethiopian Demographic and Health Survey (EDHS) report (41.5%) [58], and a study done in Tanzania (48.4%) [59]. The consistency in the magnitude of short inter pregnancy intervals between Ethiopia and Tanzania could indeed be influenced by similarities in socio-economic status between the two countries. Socio-economic factors, such as poverty levels, education, healthcare access, and cultural norms, can significantly impact reproductive behaviors and family planning practices. But, the pooled magnitude of short inter pregnancy interval was higher than the studies conducted in Nepal (23%) [60], Bangladesh (24.6%) [61], and Iran (28.5%) [62]. This discrepancy might be due to differences in data analysis, study design, sampling methods, economic status, lifestyle, health service utilization, study settings, and measurement methods. Despite efforts by the national government to promote increasing birth intervals, short inter pregnancy intervals among reproductive-age women remain quite common in practice. This is concerning because babies born from mothers who have short inter pregnancy intervals are at an increased risk of experiencing various adverse outcomes, including low birth weight, being small for gestational age, preterm birth, and congenital anomalies [7, 61, 63–70]. Give special emphasis to them. In addition to increasing family planning utilization and promoting the duration of breastfeeding, clinicians can play a crucial role in identifying and addressing the specific risk factors that contribute to short inter pregnancy intervals.
This systematic review and meta-analysis also found that several factors contribute to an increased risk of short inter pregnancy intervals among pregnant women in Ethiopia. These factors include having no formal education, not using contraceptive devices, having a preceding female child, breastfeeding for less than 24 months, having a poor wealth index, residing in rural areas, and experiencing adverse fetal outcomes. The study further revealed that women who breastfeed their child for less than 24 months have higher chances of having shorter inter pregnancy intervals [38].
According to this systematic review and meta-analysis, the odds of a short inter pregnancy interval were nearly two times higher among women with no formal education compared to those who had attended secondary education or higher. This finding is consistent with evidence from studies conducted in Saudi Arabia, Nepal, Jordan, and Pakistan [32, 71–73].due to the fact that, educated women’s have a better knowledge and awareness regarding optimal healthcare choices and have access to better information about family planning, reproductive health, and the importance of spacing pregnancies to ensure maternal and child health.
The findings of the present study indicate that mothers who did not use modern contraceptive methods before becoming pregnant with their last child were more likely to have a short inter pregnancy interval compared to those who utilized contraception. This finding is consistent with studies conducted in Jordan, Manipur, Egypt, Southeastern Nigeria, and Mbarara Hospital. [72, 74–77]. The use of modern contraceptive methods plays a crucial role in family planning and pregnancy spacing. When women do not use effective contraception, they have a higher likelihood of becoming pregnant again soon after giving birth. This shorter inter birth interval can have potential adverse effects on maternal and child health outcomes.
According to the findings of this systematic review and meta-analysis, mothers who breastfed their preceding child for less than 24 months had a higher likelihood of experiencing a short inter pregnancy interval compared to mothers who breastfed for 24 months or more. This finding is consistent with evidence from studies conducted in Manipur, Iran, Jordan, Pakistan, Ahvaz (Iran), Egypt, and Nigeria. [72, 73, 76–80]. Breastfeeding has been shown to have a positive impact on birth spacing. Prolonged breastfeeding can delay the return of fertility in women, allowing for a longer inter pregnancy interval. On the other hand, when breastfeeding is discontinued early or not practiced at all, the chances of becoming pregnant sooner increase.
In this systematic review, residence was found to be a significant factor associated with the practice of short inters pregnancy intervals. Women living in rural settings were nearly two times more likely to practice short inter pregnancy intervals compared to their urban counterparts. This finding aligns with the recent report from the Ethiopian Demographic and Health Survey (EDHS), which also indicated a higher prevalence of short inter pregnancy intervals among rural women compared to urban women [81]. Rural areas often face challenges related to limited access to healthcare services, including family planning resources and information. This limited access may result in reduced utilization of contraception and family planning methods, leading to shorter intervals between pregnancies. Moreover, socio-cultural factors and norms prevalent in rural communities can influence reproductive behaviors.
In this systematic review and meta-analysis, the sex of the preceding child was found to be significantly associated with short inter pregnancy interval. The findings of the study indicated that mothers whose preceding birth was female had higher odds of having a short inter pregnancy interval compared to mothers who had male children. These findings are consistent with evidence from studies conducted in Manipur, Saudi Arabia, Babol, Jordan, and Tanzania [71, 72, 77, 78, 82]. The association between the sex of the preceding child and pregnancy interval suggests that cultural and societal factors may influence pregnancy spacing decisions. In some cultures or societies, there may be a preference for having children of a particular sex or a desire to have children of both sexes. This preference or desire could influence the timing of subsequent pregnancies.
In this systematic review and meta-analysis, the household wealth index was identified as an independent predictor of short inter pregnancy interval. The findings indicated that women from the poorest, households had a higher likelihood of experiencing a short inter pregnancy interval compared to women from the richest households. This finding aligns with the existing literature on the topic [19]. Socioeconomic factors, such as household wealth, play a significant role in shaping reproductive behaviors and birth spacing. Women from lower socioeconomic backgrounds may face various challenges, including limited access to healthcare services, including family planning resources and information. Financial constraints and resource limitations may hinder their ability to effectively plan and space their pregnancies.
Strength and limitations
This study has several strengths: Initially, a predetermined methodology was followed for the search strategy and data abstraction. Internationally recognized instruments were utilized for a critical appraisal system to evaluate the quality of individual investigations. Secondly, in order to determine the small study effect and the risk of heterogeneity, we used subgroup and sensitivity analysis depending on study location, study sample size, and publication year. However, there were certain restrictions on this review: Due to the exclusion of some grey literature and the fact that all included research is published in English, there may be biases related to publishing and language.
Conclusion and recommendation
Despite the World Health Organization's recommendation of a minimum inter-pregnancy interval of two years, a substantial number of women in Ethiopia continue to have a short inter-pregnancy interval. Factors such as lack of formal education, duration of breastfeeding, non-use of contraceptive methods, having a preceding female child, and residence were found to affect short inter pregnancy intervals. Based on these findings, it is important for healthcare providers to counsel women about the importance of optimal inter pregnancy spacing, breastfeeding, and contraceptive utilization during antenatal care, delivery, and postnatal care follow-up. Additionally, health extension workers should provide household education to improve contraceptive utilization and breastfeeding practices in the community.
Supplementary Information
Acknowledgements
We would like to thank the primary authors of the included studies.
Abbreviations
- CI
Confidence interval
- OR
Odds ratio
- WHO
World Health Organization
- DHS
Demographic and Health Surveys
- EDHS
Ethiopian Demographic and Health Survey
- AOR
Adjusted odds ratio
- SIPI
Short inter pregnancy interval
- PNC
Post-natal care
Author contributions
The study design and protocol, literature review, study selection, quality assessment, data extraction, statistical analysis, data interpretation, and development of the initial drafts of the manuscript were all performed by GY. The final draft of the manuscript was then prepared, read and approved the final version by all authors GY, BBA, ABZ, AW, ESL, MA, ASB and BD .
Funding
No funding was obtained for this study.
Availability of data and materials
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Tesema GA, Worku MG, Teshale AB. Duration of birth interval and its predictors among reproductive-age women in Ethiopia: Gompertz gamma shared frailty modeling. PLoS ONE. 2021;16(2): e0247091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Report of a WHO technical consultation on birth spacing: Geneva, Switzerland 13–15 June 2005. World Health Organization; 2007.
- 3.Chen I, Jhangri GS, Chandra S. Relationship between interpregnancy interval and congenital anomalies. Am J Obstet Gynecol. 2014;210(6):564.e1-e8. [DOI] [PubMed] [Google Scholar]
- 4.Conde-Agudelo A, Rosas-Bermúdez A, Kafury-Goeta AC. Birth spacing and risk of adverse perinatal outcomes: a meta-analysis. JAMA. 2006;295(15):1809–23. [DOI] [PubMed] [Google Scholar]
- 5.Stephansson O, Dickman PW, Cnattingius S. The influence of interpregnancy interval on the subsequent risk of stillbirth and early neonatal death. Obstet Gynecol. 2003;102(1):101–8. [DOI] [PubMed] [Google Scholar]
- 6.Aleni M, Mbalinda S, Muhindo R. Birth intervals and associated factors among women attending young child clinic in Yumbe Hospital, Uganda. Int J Reprod Med. 2020;2020:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Conde-Agudelo A, Rosas-Bermudez A, Castaño F, Norton MH. Effects of birth spacing on maternal, perinatal, infant, and child health: a systematic review of causal mechanisms. Stud Fam Plann. 2012;43(2):93–114. [DOI] [PubMed] [Google Scholar]
- 8.Boerma T, Ronsmans C, Melesse DY, Barros AJ, Barros FC, Juan L, et al. Global epidemiology of use of and disparities in caesarean sections. Lancet. 2018;392(10155):1341–8. [DOI] [PubMed] [Google Scholar]
- 9.Singh S, Darroch JE, Ashford LS, Vlassoff M. Adding it up: the costs and benefits of investing in family Planning and maternal and new born health. Guttmacher Institute; 2009.
- 10.Muluneh AA, Kassa ZY, Siyoum M, Gebretsadik A, Woldeyes Y, Tenaw Z. Determinants of sub-optimal birth spacing in Gedeo Zone, South Ethiopia: a case–control study. Int J Women’s Health. 2020;12:549–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Berta M, Feleke A, Abate T, Worku T, Gebrecherkos T. Utilization and associated factors of modern contraceptives during extended postpartum period among women who gave birth in the last 12 months in Gondar Town, Northwest Ethiopia. Ethiop J Health Sci. 2018;28(2):207–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Saccone G, Sendek K. Prenatal care. In: Berghella V, editor. Obstetric evidence based guidelines. Boca Raton: CRC Press; 2022. p. 15–33. [Google Scholar]
- 13.Casterline JB, Odden C. Trends in inter-birth intervals in developing countries 1965–2014. Popul Dev Rev. 2016;42:173–94. [Google Scholar]
- 14.Hailu D, Gultie T, Workineh Y. Barriers to adherence of optimal birth spacing: a qualitative study among mothers and their husbands in Arba Minch Zuria District, Ethiopia. Am J Health Res. 2014;2(4):188–95. [Google Scholar]
- 15.Hailu D, Gulte T. Determinants of short interbirth interval among reproductive age mothers in Arba Minch District, Ethiopia. Int J Reprod Med. 2016;2016:1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ayane GB, Desta KW, Demissie BW, Assefa NA, Woldemariam EB. Suboptimal child spacing practice and its associated factors among women of child bearing age in Serbo town, JIMMA zone, Southwest Ethiopia. Contracept Reprod Med. 2019;4(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dadi AF. A systematic review and meta-analysis of the effect of short birth interval on infant mortality in Ethiopia. PLoS ONE. 2015;10(5): e0126759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rasheed P, Al Dabal B. Birth interval: perceptions and practices among urban-based Saudi Arabian women. 2007. [PubMed]
- 19.DaVanzo J, Hale L, Razzaque A, Rahman M. Effects of interpregnancy interval and outcome of the preceding pregnancy on pregnancy outcomes in Matlab, Bangladesh. BJOG Int J Obstet Gynaecol. 2007;114(9):1079–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Molitoris J, Barclay K, Kolk M. When and where birth spacing matters for child survival: an international comparison using the DHS. Demography. 2019;56(4):1349–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hanley GE, Hutcheon JA, Kinniburgh BA, Lee L. Interpregnancy interval and adverse pregnancy outcomes. Obstet Gynecol. 2017;129(3):408–15. [DOI] [PubMed] [Google Scholar]
- 22.Pierrat V, Marchand-Martin L, Arnaud C, Kaminski M, Resche-Rigon M, Lebeaux C, et al. Neurodevelopmental outcome at 2 years for preterm children born at 22 to 34 weeks’ gestation in France in 2011: EPIPAGE-2 cohort study. BMJ. 2017;358: j3448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pimentel J, Ansari U, Omer K, Gidado Y, Baba MC, Andersson N, Cockcroft A. Factors associated with short birth interval in low-and middle-income countries: a systematic review. BMC Pregnancy Childbirth. 2020;20(1):1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tadele A, Abebaw D, Ali R. Predictors of unmet need for family planning among all women of reproductive age in Ethiopia. Contracept Reprod Med. 2019;4(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Headey D. An analysis of trends and determinants of child undernutrition in Ethiopia, 2000–2011. Gates Open Res. 2019;3(983):983. [Google Scholar]
- 26.Mihretie GN, Getie SA, Shiferaw S, Ayele AD, Liyeh TM, Kassa BG, Asferie WN. Interbirth interval practices among reproductive age women in rural and Urban kebeles in Farta Woreda: case-control study. PLoS ONE. 2022;17(1): e0256193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tsegaye D, Shuremu M, Bidira K. Practice of child spacing and its associated factors among women of child bearing age (15 to 49 years) in Illubabor zone, South West Ethiopia. Int J Nurs Midwifery. 2017;9(7):102–8. [Google Scholar]
- 28.Roble AK, Osman MO, Ibrahim AM, Wedajo GT, Abdi US. Determinants of short birth interval among ever married reproductive age women living in Jigjiga, Eastern Ethiopia 2020 (unmatched case–control study). SAGE Open Med. 2021;9:20503121211067870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Peters MD, Godfrey CM, McInerney P, Soares CB, Khalil H, Parker D. The Joanna Briggs Institute reviewers’ manual 2015: methodology for JBI scoping reviews. 2015.
- 30.Muche AA, Kassa GM, Berhe AK, Fekadu GA. Prevalence and determinants of risky sexual practice in Ethiopia: systematic review and meta-analysis. Reprod Health. 2017;14:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rahman MS, Howlader T, Masud MS, Rahman ML. Association of low-birth weight with malnutrition in children under five years in Bangladesh: do mother’s education, socio-economic status, and birth interval matter? PLoS ONE. 2016;11(6): e0157814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Suwal JV. Socio-cultural dynamics of birth intervals in Nepal. Contrib Nepalese Stud. 2001;28(1):11–34. [Google Scholar]
- 33.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58. [DOI] [PubMed] [Google Scholar]
- 34.Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ioannidis JP. Interpretation of tests of heterogeneity and bias in meta-analysis. J Eval Clin Pract. 2008;14(5):951–7. [DOI] [PubMed] [Google Scholar]
- 36.Asmamaw DB, Habitu YA, Negash WD, Desta DZ, Mekonnen EG. Effective breastfeeding technique and associated factors among lactating mothers in Gidan District, North-East, Ethiopia: a community-based cross-sectional study. BMJ Open. 2022;12(7): e059518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jena BH, Biks GA, Gete YK, Gelaye KA. The effect of inter-pregnancy interval on primary postpartum hemorrhage in urban South Ethiopia: a community-based matched nested case control study. 2021. [DOI] [PMC free article] [PubMed]
- 38.Shifti DM, Chojenta C, Holliday EG, Loxton D. Individual and community level determinants of short birth interval in Ethiopia: a multilevel analysis. PLoS ONE. 2020;15(1): e0227798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Edasa G. Inter-pregnancy interval and adverse perinatal outcomes among mothers who gave birth in public hospitals in Halaba Zone, Southern Ethiopia: HU; 2021.
- 40.Tesema GA, Teshale AB, Yeshaw Y, Angaw DA, Molla AL. Assessing the effects of duration of birth interval on adverse pregnancy outcomes in sub-Saharan Africa: a propensity score-matched analysis. BMJ Open. 2023;13(4): e062149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shimels Hailemeskel H, Assebe T, Alemayehu T, Belay DM, Teshome F, Baye A, Bayih WA. Determinants of short birth interval among ever married reproductive age women: a community based unmatched case control study at Dessie city administration, Northern Ethiopia. PLoS ONE. 2020;15(12): e0243046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mamo H, Dagnaw A, Sharew NT, Brhane K, Kotiso KS. Prevalence of short interpregnancy interval and its associated factors among pregnant women in Debre Berhan town, Ethiopia. PLoS ONE. 2021;16(8): e0255613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fetene JC, Mulat A, Wubet T. Adverse neonatal outcomes and its associated factors among mothers with short and recommended interpregnancy interval, in Awi Zone Public Hospitals, 2020. 2021.
- 44.Mruts KB, Tessema GA, Kassaw NA, Gebremedhin AT, Scott JA, Pereira G. Short interpregnancy interval and its predictors in Ethiopia: implications for policy and practice. Pan Afr Med J. 2022;42:199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gurmu L, Wakgari N, Kolola T, Danusa KT. Effect of short inter-pregnancy interval on perinatal outcomes among pregnant women in North-west Ethiopia: a prospective cohort study. Front Public Health. 2022;10:953481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wakeyo MM, Kebira JY, Assefa N, Dheresa M. Short birth interval and its associated factors among multiparous women in Mieso agro-pastoralist district, Eastern Ethiopia: a community-based cross-sectional study. Front Glob Women’s Health. 2022;3:801394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Aychiluhm SB, Tadesse AW, Mare KU, Abdu M, Ketema A. A multilevel analysis of short birth interval and its determinants among reproductive age women in developing regions of Ethiopia. PLoS ONE. 2020;15(8): e0237602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mohammed S, Abayneh M, Bekele D, Chan G, Worku A, Girma E. Short birth interval predicts the risk of preterm birth among pregnant women in Sub-Saharan Africa: a systematic review and meta-analysis. 2020.
- 49.Damtie Y, Kefale B, Yalew M, Arefaynie M, Adane B. Short birth spacing and its association with maternal educational status, contraceptive use, and duration of breastfeeding in Ethiopia: a systematic review and meta-analysis. PLoS ONE. 2021;16(2): e0246348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yohannes S, Wondafrash M, Abera M, Girma E. Duration and determinants of birth interval among women of child bearing age in Southern Ethiopia. BMC Pregnancy Childbirth. 2011;11(1):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Begna Z, Assegid S, Kassahun W, Gerbaba M. Determinants of inter birth interval among married women living in rural pastoral communities of southern Ethiopia: a case control study. BMC Pregnancy Childbirth. 2013;13:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tessema GA, Zeleke BM, Ayele TA. Birth interval and its predictors among married women in Dabat District, Northwest Ethiopia: a retrospective follow up study. Afr J Reprod Health. 2013;17(2):39–45. [PubMed] [Google Scholar]
- 53.Shallo SA, Gobena T. Duration of birth interval and associated factors among married women in Dodota Woreda, Arsi Zone, Ethiopia. J Health Educ Res Dev. 2019;7(1):10.4172. [Google Scholar]
- 54.Brhane M, Hagos B, Abrha MW, Weldearegay HG. Does short inter-pregnancy interval predicts the risk of preterm birth in Northern Ethiopia? BMC Res Notes. 2019;12:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gebrehiwot SW, Abera G, Tesfay K, Tilahun W. Short birth interval and associated factors among women of child bearing age in northern Ethiopia, 2016. BMC Womens Health. 2019;19(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ejigu AG, Yismaw AE, Limenih MA. The effect of sex of last child on short birth interval practice: the case of northern Ethiopian pregnant women. BMC Res Notes. 2019;12:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wodaje MSS, Yilak G, Tarekegn A. The magnitude of short interpregnancy intervals and associated factors among women who delivered in north Wollo Zone Public Hospitals, North Eastern Ethiopia. 2023. [DOI] [PMC free article] [PubMed]
- 58.Demographic E. Health survey: Addis Ababa. Ethiopia and Calverton, Maryland: Central Statistics Agency and ORC Macro. 2011.
- 59.Exavery A, Mrema S, Shamte A, Bietsch K, Mosha D, Mbaruku G, Masanja H. Levels and correlates of non-adherence to WHO recommended inter-birth intervals in Rufiji, Tanzania. BMC Pregnancy Childbirth. 2012;12:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Karkee R, Lee AH. Birth spacing of pregnant women in Nepal: a community-based study. Front Public Health. 2016;4:205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.De Jonge HC, Azad K, Seward N, Kuddus A, Shaha S, Beard J, et al. Determinants and consequences of short birth interval in rural Bangladesh: a cross-sectional study. BMC Pregnancy Childbirth. 2014;14(1):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Fallahzadeh H, Farajpour Z, Emam Z. Duration and determinants of birth interval in Yazd, Iran: a population study. Iran J Reprod Med. 2013;11(5):379. [PMC free article] [PubMed] [Google Scholar]
- 63.Grisaru-Granovsky S, Gordon E-S, Haklai Z, Samueloff A, Schimmel MM. Effect of interpregnancy interval on adverse perinatal outcomes—a national study. Contraception. 2009;80(6):512–8. [DOI] [PubMed] [Google Scholar]
- 64.Nerlander LM, Callaghan WM, Smith RA, Barfield WD. Short interpregnancy interval associated with preterm birth in US adolescents. Matern Child Health J. 2015;19:850–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kozuki N, Lee AC, Silveira MF, Victora CG, Adair L, Humphrey J, et al. The associations of birth intervals with small-for-gestational-age, preterm, and neonatal and infant mortality: a meta-analysis. BMC Public Health. 2013;13:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Cheslack-Postava K, Suominen A, Jokiranta E, Lehti V, McKeague IW, Sourander A, Brown AS. Increased risk of autism spectrum disorders at short and long interpregnancy intervals in Finland. J Am Acad Child Adolesc Psychiatry. 2014;53(10):1074-81.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Durkin MS, DuBois LA, Maenner MJ. Inter-pregnancy intervals and the risk of autism spectrum disorder: results of a population-based study. J Autism Dev Disord. 2015;45:2056–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Fotso JC, Cleland J, Mberu B, Mutua M, Elungata P. Birth spacing and child mortality: an analysis of prospective data from the Nairobi urban health and demographic surveillance system. J Biosoc Sci. 2013;45(6):779–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Dadi AF. Short birth intervals less than 2 years double under-one mortality in Ethiopia: evidence from a meta-analysis. Science. 2014;2(6):589–95. [Google Scholar]
- 70.Grundy E, Kravdal Ø. Do short birth intervals have long-term implications for parental health? Results from analyses of complete cohort Norwegian register data. J Epidemiol Community Health. 2014;68(10):958–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Abdel-Fattah M, Hifnawy T, El Said TI, Moharam MM, Mahmoud MA. Determinants of birth spacing among Saudi women. J Fam Community Med. 2007;14(3):103. [PMC free article] [PubMed] [Google Scholar]
- 72.Youssef RM. Duration and determinants of interbirth interval: community-based survey of women in southern Jordan. East Mediterr Health J. 2005;11(4):559–72. [PubMed] [Google Scholar]
- 73.Kamal A, Pervaiz MK. Determinants of higher order birth intervals in Pakistan. J Stat. 2012;19(1):54–82. [Google Scholar]
- 74.Dim C, Ugwu E, Iloghalu E. Duration and determinants of inter-birth interval among women in Enugu, south-eastern Nigeria. J Obstet Gynaecol. 2013;33(2):175–9. [DOI] [PubMed] [Google Scholar]
- 75.Mayanja Ronald M, Mubiru Musa M, MasembeSezalio M, Nkonwa I. Factors associated with short births intervals among women delivering at Mbarara Hospital. Age. 2016;15(19):20–30. [Google Scholar]
- 76.Baschieri A, Hinde A. The proximate determinants of fertility and birth intervals in Egypt: an application of calendar data. Demogr Res. 2007;16:59–96. [Google Scholar]
- 77.Singh SN, Singh SN, Narendra R. Demographic and socio-economic determinants of birth interval dynamics in Manipur: a survival analysis. Online J Health Allied Sci. 2011;9(4):3. [Google Scholar]
- 78.Hajian-Tilaki K, Asnafi N, Aliakbarnia-Omrani F. The patterns and determinants of birth interval in multiparous women in Babol, northern Iran. Southeast Asian J Trop Med Public Health. 2009;40(4):852. [PubMed] [Google Scholar]
- 79.Abdolrahman R, Majid M. The determinants of birth interval in Ahvaz-Iran: a graphical chain modeling approach. J Data Sci. 2007;5:555–7. [Google Scholar]
- 80.Kemi OB, Olurotimi OJ. Breastfeeding and child spacing among women in South West Nigeria. Int J Cross-Discip Subj Educ. 2011;2(2):414–21. [Google Scholar]
- 81.Csa I. Central statistical agency (CSA) [Ethiopia] and ICF. Ethiopia demographic and health survey, Addis Ababa, Ethiopia and Calverton, Maryland, USA. 2016;1.
- 82.Akim J, Mtur I. The determinants of birth intervals among non-contraceptive user Tanzanian women. Union Afr Popul Stud. 1997;12(2):1–12. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated or analysed during the current study.