Abstract
Background
Phosphatidylinositol-3,4,5-triphosphate (PtdInsP3) signaling is elevated in many tumors due to loss of the tumor suppressor PTEN, and leads to constitutive activation of Akt, a kinase involved in cell survival. Reintroduction of PTEN in cells suppresses transformation and tumorigenicity. While this approach works in-vitro, it may prove difficult to achieve in-vivo. In this study, we investigated whether inhibition of growth factor signaling would have the same effect as re-expression of PTEN.
Methods
Dominant negative IGF-I receptors were expressed in CHO and U87 cells by retroviral infection. Cell proliferation, transformation and tumor formation in athymic nude mice were assessed.
Results
Inhibition of IGF-IR signaling in a CHO cell model system by expression of a kinase-defective IGF-IR impairs proliferation, transformation and tumor growth. Reduction in tumor growth is associated with an increase in apoptosis in-vivo. The dominant-negative IGF-IRs also prevented growth of U87 PTEN-negative glioblastoma cells when injected into nude mice. Injection of an IGF-IR blocking antibody αIR3 into mice harboring parental U87 tumors inhibits tumor growth and increases apoptosis.
Conclusion
Inhibition of an upstream growth factor signal prevents tumor growth of the U87 PTEN-deficient glioma to the same extent as re-introduction of PTEN. This result suggests that growth factor receptor inhibition may be an effective alternative therapy for PTEN-deficient tumors.
Background
Phosphatidylinositol-(3,4,5)-trisphosphate (PIP3) is one of the major intracellular second messengers regulating growth, metabolism and vesicular trafficking [for reviews see refs [1-3]]. The level of (PIP3) in the cell is determined by the balance of kinase and phosphatase activity. PI-3Kinase activity is acutely regulated and a number of isoforms have been cloned that are activated in response to various stimuli [4]. The major phosphatidylinositol-3-phosphate phosphatase in cells is the tumor suppressor PTEN [5,6]. This protein has a tonic inhibitory effect on PI-3Kinase signaling by reversing the 3'-phosphorylation. PTEN is altered or deleted in many human cancers [7-10]. In-vitro, cells that are deficient in PTEN show elevated PI-3Kinase signaling [11]. Reintroduction of PTEN in a variety of cancer cells, including glioma, breast, bladder and ovarian cancer cells, causes G1 arrest, inhibits tumorigenesis, and promotes anoikis [12-14]. Mechanistically, Akt activity is decreased, cell motility is decreased, expression of two cyclin-dependent kinase inhibitors p27 and p21 is increased, cyclin D1 is down-regulated, Rb phosphorylation is inhibited, and signaling via Grb2/SOS is suppressed [11,15]. The link between PTEN and cell growth is underscored by genetic experiments in mice. PTEN knockout mice die in-utero due to extensive overgrowth of the cephalic and caudal regions [12,16]. PTEN +/- heterozygous mice have a predisposition to tumors in multiple tissues often with loss of the second allele [17,18]. In-vitro, PTEN-/- embryonic stem cells and fibroblasts display increased proliferation and decreased sensitivity to apoptosis.
The PI-3Kinase-dependent activation of Akt is thought to play a central role in the cell survival pathway in many cells [7,19,20]. Elevated Akt activity and protein is found in many PTEN-deficient cancer cells. Akt directly phosphorylates and inactivates the pro-apoptotic proteins ASK1, BAD, caspase 9 [21-24]. Akt also induces the expression of the anti-apoptotic Bcl-2 and c-FLIP proteins, and suppresses the cell cycle inhibitor p27KIP[25-28]. This later effect is via the phosphorylation and inactivation of the forkhead family of transcription factors AFX, FKHR and FKHR-L1. Although it is often assumed that elevated Akt activity is responsible for the increased survival of cancer cells, Akt activity is not the only pathway that is essential for cell survival. The MAPK pathway can also protect cells from apoptosis, as can constitutive activation of Stat3 signaling [29,30].
The IGF-I Receptor is a member of the large family of tyrosine kinase growth factor receptors. Signaling by the IGF-IR has been studied in many different cell types and is important for proliferation, survival, motility, adhesion, transformation, tumor formation and metastasis [for reviews see refs [31,32]]. The receptor can directly phosphorylate the insulin receptor substrate 1 (IRS-1) and Shc proteins in the intact cell causing activation of PI-3Kinase and ras signaling [33]. More recently, it has been shown that the IGF-IR signals via the Gβγ subunits of the heterotrimeric Gi complex to stimulate PI-3Kinase and ras, and also activates the JAK/Stat pathway to cause phosphorylation of Stat3 [34,35].
What is the evidence for the involvement of IGF-IR signaling in proliferation and cancer? Elegant studies in knockout mice have delineated the contribution of IGF-I, IGF-II and the IGF-I receptor to fetal growth [for review see ref [36]]. Embryonic fibroblasts derived from IGF-IR knockout embryos (R-cells) do not grow in serum-free medium, despite supplementation with a wide variety of other growth factors, and grow more slowly in media containing serum than wild-type cells [for reviews see refs [37,38]]. Additionally, all phases of the cell cycle are prolonged in the null cells suggesting that the IGF-IR is required throughout the cell cycle. A functional IGF-I receptor is required for successful cell transformation. IGF-IR-/- cells are not transformed by overexpression of SV40 T antigen, activated ras, or EGF or PDGF receptors. Transformation appears to involve autocrine stimulation as IGF-I production and secretion is increased in normal cells following transformation by SV40 T antigen, but the null cells cannot respond to the IGF-I so do not transform.
Interfering with the IGF signaling system can inhibit the growth of cancer cells in-vitro and in-vivo. Treatment with antagonistic peptide analogs of IGF-I, antisense oligos, or an adenovirus expressing IGF-IR antisense cRNA, prevents proliferation of cells in monolayers, transformation, and growth in athymic nude mice. This includes multiple human tumor cell lines including glioblastoma, melanoma, ovarian carcinoma, prostatic carcinoma, and breast carcinomas). [for reviews see refs [31],[39-41]]. The IGF-IR appears to function in transformation both by preventing apoptosis through activation of Akt and by stimulating proliferation through the ras-MAPK cascade. IGF-I can prevent c-myc-induced apoptosis in rat-l fibroblasts, and neuronal apoptosis due to serum-starvation. IGF-IR-/- cells can proliferate in monolayers in the presence of serum but undergo apoptosis when put in suspension and are more sensitive to chemotherapeutic reagents. There is also evidence implicating the IGF-IR in metastasis. IGF-I produces a chemotactic response in human melanoma cells and antisense to the IGF-IR mRNA prevents metastasis in the murine carcinoma cell H-59.
In this study, we wanted to determine if disruption of IGF-I signaling could prevent growth of a tumor cell lacking PTEN. Elevated PI-3Kinase can be normalized by reintroduction of PTEN to reduce PIP3 levels, but it has not been shown that this effect can also be achieved by disruption of an upstream signal that stimulates PI-3Kinase activity. We have previously demonstrated the overexpression and hormone-independent activation of the IGF-IR in primary breast cancers [42]. Similar overexpression of the IGF-IR and the ligands IGF-I and IGF-II have been seen in human gliomas and astrocytomas [43-46]. Because of the important role for the IGF-IR in cell survival, we investigated whether a dominant negative IGF-IR could inhibit growth of the U87 glioma. This glioma is deficient in PTEN and shows constitutive activation of Akt, which can be inactivated by re-introduction of PTEN [47].
Materials and Methods
Materials and Cell Culture
Antiphosphotyrosine antibodies (pY20) were from BD-Transduction Labs (Lexington, KY). Matrigel was from Becton-Dickinson (Bedford, MA) Athymic nude mice were purchased from Charles River (Wilmington, MA). Enhanced chemiluminescence reagents were from Amersham (Piscataway, NJ). [3H]-thymidine (20 Ci/mmol) was from Perkin-Elmer/NEN Life Sciences (Boston, MA). Unless noted, all other reagents were supplied by Sigma Chemical Co. (St. Louis, MO) or Fisher Scientific Co. (Springfield, NJ). CHO cells were maintained in Hams F12 with 25 mM glucose with 50 units/ml penicillin, 50 μg/ml streptomycin, and 10% FCS in a 10 % CO2 environment. U87 glioma cells were maintained in MEM-Earle's medium with non-essential amino acids, 1 mM sodium pyruvate, 10% FCS, 2 mM Glutamax and gentamycin sulphate in a 10% CO2 environment.
Immunoblotting
Cells were serum starved for 16 h in 12-well plates, then stimulated with IGF-I (10 or 100 ng/ml) for 5 min at 37°C. The cells were washed with ice-cold phosphate-buffered saline and solubilized in 2 × SDS-sample buffer containing 2 mM sodium orthovanadate and 200 mM sodium fluoride. The proteins were denatured by boiling for 5 min, then were separated by electrophoresis on 7.5% SDS-PAGE, and transferred to PVDF membranes. The filter was blocked with 3% BSA in TBS with 0.1% Tween 20 (T-TBS) for 30 min and incubated with the anti-phosphotyrosine antibodies at a dilution of 1:1000. The filters were washed with T-TBS for 30 min and incubated with horseradish-peroxidase conjugated secondary antibodies, and tyrosine-phosphorylated proteins were visualized by enhanced chemiluminescence.
Measurement of thymidine incorporation
Cells were grown to 75% confluence in six-well cluster plates. The growth medium was replaced with serum-free Ham's F12 for 36 h. Cells were stimulated with IGF-I at the indicated concentrations for 18 h. Cells were pulsed with [3H]-thymidine, 2 μCi/ml, for 1 h at 37°C. The cells were washed five times in PBS, solubilized, the DNA precipitated with 10% trichloroacetic acid at 4°C, and counted in an scintillation counter.
Production of pseudo-typed retrovirus
The wild-type IGF-IR cDNA or a mutant cDNA, which contained a methionine substitution for lysine 1003 in the ATP-binding site of the kinase domain, were cloned into the retroviral vector pLPONL [57]. The pseudo-typed viruses were generated and purified by the UCSD Viral Vector Core. The plasmids were co-transfected into 293 cells with an expression vector for the Vesicular Stomatitis Virus-G protein. This coat protein allows the virus to be concentrated and confers greater tropism. Cell culture supernatants and cells were harvested and the virus concentrated. Viruses were titered on NIH3T3 cells and the number of G418 resistant colonies counted. A control virus containing the E. coli β-galactosidase gene was obtained from the Viral Vector Core.
Growth in Soft Agar
Cells were trypsinized and 104 cells plated in 35 mm petri dishes in complete medium containing 0.35% agarose over a layer of 0.7% agarose in complete medium. Cells were allowed to grow for 14–21 days or until colonies were >125 μm in diameter. Fresh medium was layered above the agarose every 3–5 days. Colonies were stained with Crystal Violet and counted.
Tumor Growth in Athymic Nude Mice
Housing and all procedures using nude mice were approved by the animal care committee at UCSD. The cells for injection were trypsinized in sterile PBS, pelleted by centrifugation at 300 × g for 2 min. and washed twice in sterile saline. Cells were resuspended in 100 μl sterile saline and counted using a hemacytometer. The appropriate number of cells was diluted into 50 μl sterile saline and then added to an equal volume of sterile Matrigel on ice. This suspension was injected subcutaneously on the rear flank of athymic nude mice using a sterile syringe and 22-gauge needle. Mice were observed on a twice-weekly basis to check for tumor growth. Tumors were measured with calipers in three dimensions and tumor volume calculated assuming the tumors were ellipsoid. At the end of the study, the tumors were excised, measured, weighed, and then fixed in 10% formalin. Tumors were embedded in paraffin, sectioned and stained with hematoxylin-eosin or for apoptosis using the TUNEL assay (Roche, Indianapolis, IN).
Results and Discussion
Inhibition of the IGF-I receptor by expression of a kinase inactive mutant inhibits proliferation of Chinese hamster ovary (CHO) cells
Before embarking on studies in human tumor cells, we verified that our dominant negative approach would work in a model system. To inhibit the IGF-IR, we took advantage of the fact that the IGF-I receptor is a hetero-tetramer. Activation of the native receptor requires the trans-phosphorylation of two kinase domains [48]. Hence, expression of an excess of kinase-defective IGF-I receptors causes the formation of hybrid molecules containing one half an endogenous wild-type receptor and the other half a kinase-defective transfected receptor. These hybrids should be kinase inactive and signaling incompetent. Similar approaches have been used successfully in other studies [49-52].
Initially, we tested Chinese hamster ovary (CHO) cells that had been stably transfected with expression vectors for kinase-inactive or wild type IGF-I receptors [53]. The parental CHO cell line expresses ~50,000 endogenous IGF-IRs, the transfected wild-type (CHO-WT) cell line expresses ~250,000 IGF-IRs, and the kinase-defective (CHO-MK) cell line expresses ~250,000 mutant IGF-IRs. Thus, the transfected cells express the human IGF-IR at approximately five fold higher levels than the endogenous receptor. The mutant receptor contains a lysine to methionine (MK) point mutation at position 1003 in the ATP binding site of the kinase domain and has no measurable kinase activity. Two clonal lines expressing the MK receptor were used with identical results.
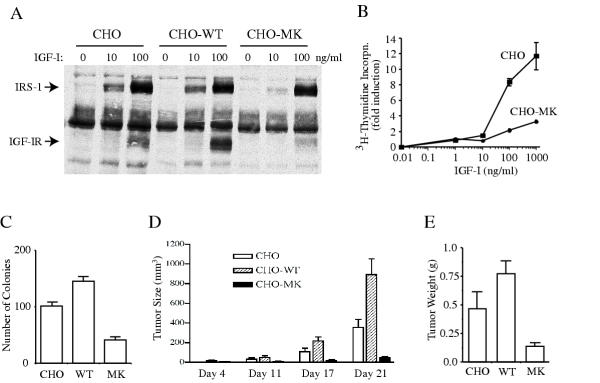
We assessed the ability of the IGF-IRs of each cell line to undergo autophosphorylation in response to increasing concentrations of IGF-I. Cells were stimulated with increasing concentrations of IGF-I, and whole cell lysates immunoblotted for tyrosine-phosphorylated proteins. As expected, autophosphorylation of the IGF-IRs was observed in the CHO and CHO-WT cells but very little was seen in two different clones of CHO-MK cells, indicating that the kinase-defective receptors inhibited the endogenous wild-type hamster receptors (Figure 1A). The inhibition was not complete however, as phosphorylation of IRS1, the major endogenous substrate in these cells, is still preserved at the higher dose of IGFI but inhibited at the lower dose. This is likely due to the level of receptor expression. The transfected receptors are expressed at four fold the level of the endogenous receptors. Assuming stochastic assembly of tetramers, 4% of receptors should be homodimers of signaling competent receptors that can phosphorylate IRS1. To confirm that the kinase-defective receptors were functioning in a dominant-negative fashion, we studied the ability of CHO and CHO-MK cells to incorporate 3H-thymidine into DNA in response to IGF-I stimulation. Serum-starved cells were stimulated with increasing concentrations if IGF-I and then pulsed with 3H-thymidine. The ability of the CHO-MK cells to incorporate thymidine in response to IGF-I is markedly diminished as compared to the parental cell line (Figure 1B).
Figure 1.
Expression of a kinase inactive IGF-IR impairs tumorigenesis. CHO cells express 5 × 104 IGF-IRs, CHO-WT cells express 2 × 105 wild-type IGF-IRs, and the CHO-MK cells express 2 × 105 mutant IGF-IRs that contain a Lysine to Methionine point mutation in the ATP-binding site (MK1003). Panel A: IGF-I stimulated whole cell tyrosine phosphorylation. Serum-starved cells were stimulated with IGF-I (10 or 100 ng/ml) for 5 min and whole cell extracts immunoblotted for phosphotyrosine. The positions of the β-subunit of the IGF-IR and IRS-1 are indicated. Panel B: Serum-starved CHO or CHO-MK cells were stimulated with increasing concentrations of IGF-I for 18 h then pulsed with 3H-thymidine for 1 h. DNA was precipitated with TCA and counted. Panel C: ten thousand cells were plated in soft agar in complete medium for 14–21 days. Colonies > 125 μm in diameter were counted after staining with crystal violet. Panel D: ten million cells were injected subcutaneously into the rear flank of athymic nude mice. Tumor size was measured with calipers every few days. Graph shows mean tumor volume (± SEM) as a function of time. Panel E: Mice were euthanized after 21 days and the tumors excised, weighed and fixed for staining. Graph shows mean tumor weight (± SEM).
We then tested colony formation in soft agar as an indicator of cellular transformation. Cells were trypsinized, counted and equivalent numbers of cells plated in soft agar in complete medium. Cells were cultured for 14 – 21 days and then the number of colonies counted. Overexpression of the wild-type IGF-IRs increased the number of colonies, and overexpressing the kinase-defective receptors reduced the number of colonies by 60% (Figure 1C). Not only did we observe a difference of the number of colonies, but CHO-MK colonies were smaller than either the parental CHO or CHO-WT colonies (data not shown).
We next studied the ability of each of these cell lines to form tumors in athymic nude mice. Ten million (107) cells from each cell line were injected subcutaneously into the flanks of five athymic nude mice. Tumor size was measured biweekly. The mice were euthanized at the end of three weeks and the tumors excised and weighed (Figure 1D &1E). At this high level of innoculum, there was no difference in tumor incidence (data not shown). However, expression of the wild-type IGF-IR accelerated tumor growth and tumors were larger at sacrifice. The kinase defective IGF-IR, on the other hand, delayed the appearance of tumors and smaller tumors were found at sacrifice.
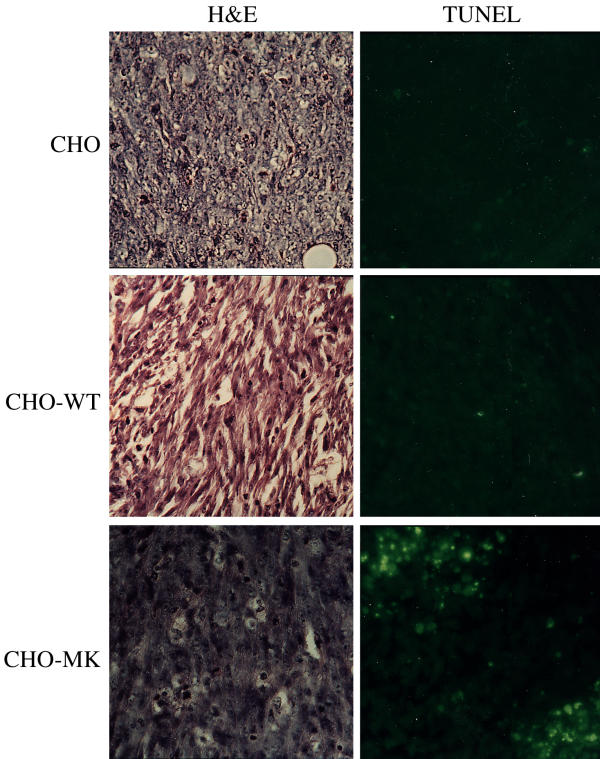
The tumors were imbedded in paraffin and sections were stained with hematoxylin and eosin (Figure 2, left panels). The sections were also stained for the presence of apoptosis using the TUNEL method. Apoptotic cells image as fluorescent green (Figure 2, right panels). The typical histology of CHO tumors is shown in panel A. Cells transfected with the wild-type IGF-IR have a more streaming morphology characteristic of human ovarian tumors (Panel B). Cells transfected with the kinase-defective IGF-IR showed a more benign morphology with no invasion of the capsule (Panel C and data not shown). Very few apoptotic cells are seen in the CHO parental and CHO-WT cells, whereas apoptotic cells are seen throughout the tumor from the kinase-defective CHO-MK cells. These results confirm that the kinase defective IGF-IR is able to inhibit tumor growth in a model system.
Figure 2.
Staining of CHO cell tumors. Left panels: hematoxylin-eosin staining of sections of CHO (panel A), CHO-WT (panel B), and CHO-MK (panel C) tumors. Right panels: TUNEL staining for apoptotic cells. Apoptotic cells were detected with a fluorescein labeled secondary antibody and show green fluorescence.
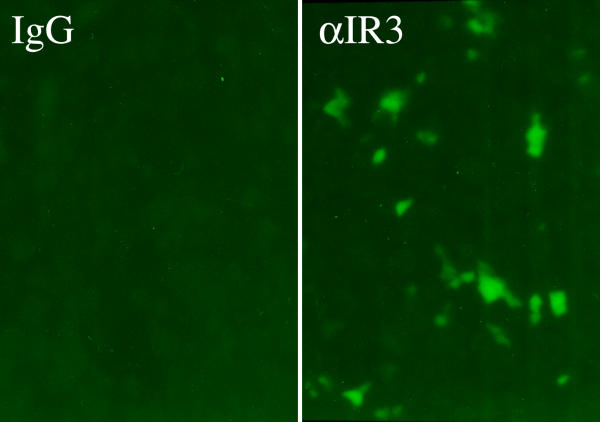
An inhibitory antibody to the IGF-IR inhibits growth of U87 tumors
Adenoviral expression of wild-type PTEN can inhibit U87 tumor growth indicating that elevated PI-3Kinase signaling is responsible for the increased proliferation and survival of these cells [47,54]. Our subsequent studies were designed to test whether interruption of an upstream growth factor signal would have the same growth inhibitory effect as reintroduction of PTEN. To test initially whether the PTEN-deficient U87 glioma cells might be susceptible to inhibition of the IGF-IR, we measured colony formation and tumor growth in the presence of an inhibitory antibody to the human IGF-IR (αIR3). This antibody prevents binding of IGF-I or IGF-II to the extracellular domain of the IGF-IR, and has been shown to prevent the formation of MDA231 tumors in nude mice [55]. U87 cells were plated in soft agar in the presence of αIR3 or a control antibody. Cells were cultured for 14 days and the number of colonies counted. The presence of the inhibitory antibody reduced the number of colonies growing in soft agar but the control antibody had no effect (Table 1). U87 cells were then injected into nude mice as before. Mice received biweekly intraperitoneal injections of 100 μg of αIR3 or control antibody starting 3 days after injection of the cells. The αIR3 injections reduced the number of tumors by >60% (Table 1). The tumors were excised, fixed and stained for apoptosis. Tumors from mice treated with the αIR3 antibody showed extensive apoptosis unlike control tumors (Figure 3). These results confirm that inhibition of IGF-I signaling by an inhibitory antibody can suppress growth of a PTEN-deficient glioma cell line.
Table 1.
Effect of antibody αIR3 on transformation and tumor growth.
| Untreated | αIR3 | Mouse IgG | |
| Colonies in soft agar | 28 ± 3 | 11 ± 2 | 27 ± 2 |
| Tumors in nude mice | - | 4/16 (25%) | 11/16 (69%) |
Figure 3.
Treatment with an inhibitory antibody against the IGF-IR. One million U87 cells were injected subcutaneously into the rear flanks of athymic nude mice. Mice received intraperitoneal injections of 100 μg of αIR3 or control IgG every two days starting on the third day after inoculation with cells. Each group consisted of eight mice that each received two injections of cells. Tumors were excised, fixed, sectioned and stained for apoptosis using the TUNEL assay. Left panel shows tumor from mice treated with control IgG; right panel shows tumor from mice treated with αIR3. TUNEL positive cells show green fluorescence.
Retroviral expression of the kinase inactive IGF-I Receptor inhibits growth of U87 glioblastoma cells in-vivo
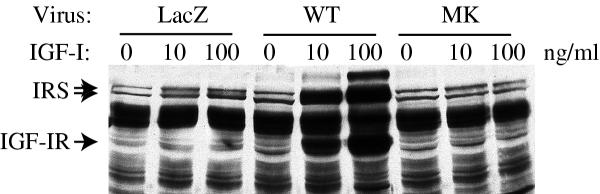
To make expression of kinase defective IGF-I receptors in different cell lines more tractable, we generated pseudotyped retroviruses expressing either the kinase-defective (MK) or wild-type (WT) IGF-I receptors. We also obtained a virus expressing the beta-galactosidase (LacZ) protein to measure infection efficiency and serve as a virus control. U87 cells were infected with the MK, WT or LacZ viruses and selected with G418. Pools of cells containing stably integrated retroviruses were then used in transformation and tumor growth experiments. Binding studies showed that the U87-LacZ cells express 105 endogenous IGF-IRs per cell, while the U87-WT and U87-MK cells express 3 × 106 and 2 × 106 receptors per cells respectively. Thus, the retrovirus allows 20 to 30-fold overexpression of the transfected receptor.
To test the function of the virally encoded receptors, we measured IGF-I stimulated autophosphorylation of the IGF-IR and phosphorylation of IRS-1. Phosphorylation IRS-1 was evident in the LacZ infected cells but little IGF-IR phosphorylation was seen as the cells express few receptors (Figure 4). Infection with the WT virus leads to a large increase in IGF-IR and IRS-1 tyrosine phosphorylation. Infection with the MK virus eliminated the IGF-I stimulated phosphorylation of IRS-1 confirming that the expressed receptor was acting as a dominant negative to inhibit the endogenous receptors. The dominant negative effect is much greater in these cells than the CHO cells (Figure 1) as the virus expresses the transfected receptors at a much higher level.
Figure 4.
Retroviral expression of wild-type and mutant IGF-IRs in U87 glioma cells. U87 cells stably infected with pseudotyped retroviruses expressing β-galactosidase (LacZ), wild-type IGF-IR (WT) or kinase defective IGF-IR (MK) were rendered quiescent by serum-starvation then stimulated with IGF-I (10 or 100 ng/ml) for 5 min. Whole cell extracts were immunoblotted for phosphotyrosine. The positions of the β-subunit of the IGF-IR and the IRS proteins are indicated.
The three infected U87 glioma cells were then injected into nude mice. Eight to twelve mice were studied for each cell line and each mouse received two injections. In two different experiments, mice were inoculated with 106 or 5 × 105 cells. Tumors were excised after 6 or 10 weeks and weighed (Table 2). The WT-infected cells had the highest frequency of tumor formation and the MK-infected cells the lowest in both cases. WT-infected cells gave the largest tumors in both experiments demonstrating that overexpression of the IGF-IR in a malignant cell can enhance tumor formation as we observed for the CHO cells. The MK-infected cells gave fewer tumors in both experiments, but more importantly, those tumors that did form were much smaller. The results obtained with the dominant negative IGF-IR are identical to published results reintroducing PTEN, hence, inhibition of upstream PI-3Kinase signaling might be a useful approach for PTEN-deficient tumors.
Table 2.
Growth of infected U87 cells in nude mice.
| U87 | U87-WT | U87-MK | ||||
| # cellsa | #tumors (%) | Weight (g) | #tumors (%) | Weight (g) | #tumors (%) | Weight (g) |
| 5 × 105 | 4/14 (29%) | 0.48 ± 0.11 | 11/16 (69%) | 0.67 ± 0.15 | 2/14 (14%) | 0.13* ± 0.02 |
| 106 | 16/24 (67%) | 0.43 ± 0.13 | 16/18 (89%) | 0.57 ± 0.1 | 11/24 (46%) | 0.12* ± 0.02 |
Weight is given as mean ± SEM. (a) mice with 5 × 105 cells sacrificed after 10 weeks, mice with 106 cells sacrificed after 6 weeks. Asterisks denote statistical significance (P < 0.05) versus parental cells
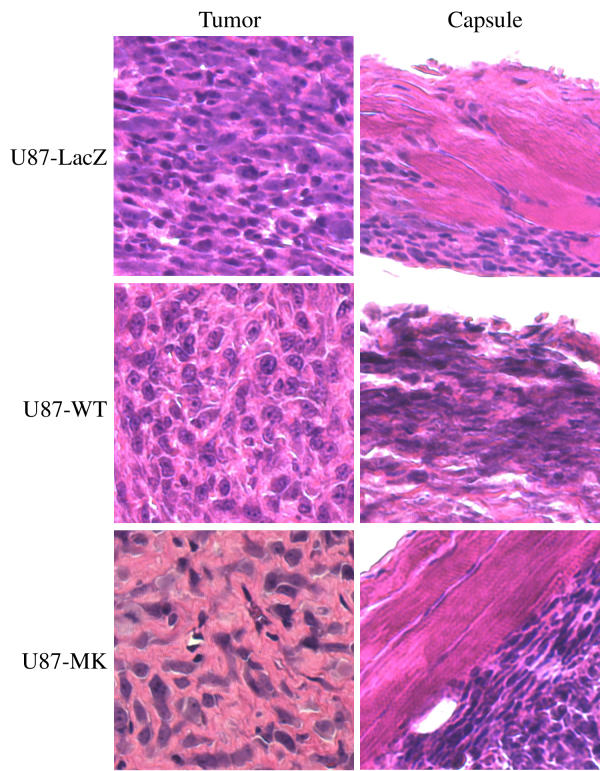
The tumors were imbedded in paraffin and sections were stained with hematoxylin and eosin (Figure 5). The U87-LacZ tumors are very cellular with small regular nuclei (left panel) and show some invasion of the capsule by tumor cells (right panel). The tumors from U87 cells infected with the IGF-IR virus are also very cellular, but the cells have larger nuclei (left panel) and have completely invaded the capsule (right panel). The tumors from U87 cells infected with the kinase inactive IGF-IR are less cellular with larger areas of stroma (left panel). Numerous irregular nuclei are apparent. There is no invasion of the capsule by tumor cells (right panel). The irregular nuclei and intact capsule are consistent with data from other cells showing that inhibition of IGF-IR expression causes apoptosis and prevents metastasis.
Figure 5.
Staining of U87 tumors. Tumors were fixed, sectioned and stained with hematoxylin-eosin. Left panels: staining of central tumor section. Right panels: staining of tumor capsule. White arrows indicate infiltration of tumor cells into the capsule. Tumors from U87-LacZ cells are shown in the top panels, tumors from U87-WT cells (wild-type IGF-IR) in the middle panels, and tumors from U87-MK cells (kinase defective IGF-IR) in the bottom panels.
The idea that the IGF-IR might be a valuable target for the treatment of brain tumors is supported by a recent pilot study in twelve patients with malignant astrocytomas [56]. All patients had grade 3 or 4 astrocytomas and had failed on standard therapy. The PTEN status of their primary tumors was not known. After surgery, autologous glioma cells were collected and treated ex-vivo with IGF-IR antisense oligos and re-implanted in diffusion chambers for 24 h. Clinical and radiological improvements were seen in eight of the twelve patients. Five patients showed a lymphocytic infiltration after antisense treatment indicating that knocking out the IGF-IR induced an immune response. It would be interesting to determine whether response to this treatment correlated with loss of PTEN in the primary tumors.
Conclusions
Loss of PTEN is a very common occurrence in human tumors. Restoring PTEN protein or function to reduce PI-3Kinase signaling prevents tumor growth in animal models. However, it may not be possible to restore PTEN in human tumors. Direct inhibition of PI-3Kinase activity may not be feasible either as it is likely to have severe side effects. Our results suggest that a therapeutic strategy to inhibit the upstream stimulus for PI-3Kinase through blockade of growth factor receptors may provide a workable alternative.
Abbreviations
PIP3: Phosphatidyl-3,4,5-triphosphate; DMEM: Dulbecco's Modified Eagle's Medium; PI-3Kinase: phosphatidylinositol-3-kinase; MAPK: mitogen-activated protein kinase; IGF: insulin-like growth factor; PTEN: phosphatase and tensin homolog deleted from chromosome 10; SOS: son-of-sevenless ras exchange factor; ASK: apoptosis stimulating kinase; FKHR: forkhead related protein; cFLIP: cellular FLICE interacting protein; BSA: bovine serum albumin; TBS: tris buffered saline; PVDF: polyvinylidene difluoride
Competing Interests
None declared.
Author Contributions
B.L.S. conducted the studies on CHO cells and the inhibitory antibody studies on U87 cells. G.S. performed the tumor growth studies with the U87 cells. N.J.G.W. constructed the pseudotyped retroviruses and drafted the manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Acknowledgments
Acknowledgements
This research was supported by a NIH Clinical Investigator Award (to B.L.S.) and a CapCURE award (to N.J.G.W.). We would like to acknowledge the expert technical assistance of Donna Reichart. N.J.G.W. is a faculty member of the UCSD Biomedical Sciences Graduate Program. B.L.S. current address is ProDuct Health Inc., Menlo Park, CA.
Contributor Information
B Lynn Seely, Email: lseely@producthealth.com.
Goli Samimi, Email: gsamimi@ucsd.edu.
Nicholas JG Webster, Email: nwebster@ucsd.edu.
References
- Rameh LE, Cantley LC. The role of phosphoinositide 3-kinase lipid products in cell function. J Biol Chem. 1999;274:8347–8350. doi: 10.1074/jbc.274.13.8347. [DOI] [PubMed] [Google Scholar]
- Katso R, Okkenhaug K, Ahmadi K, White S, Timms J, Waterfield MD. Cellular function of phosphoinositide 3-kinases: implications for development, homeostasis, and cancer. Annu Rev Cell Dev Biol. 2001;17:615–675. doi: 10.1146/annurev.cellbio.17.1.615. [DOI] [PubMed] [Google Scholar]
- Cantrell DA. Phosphoinositide 3-kinase signalling pathways. J Cell Sci. 2001;114:1439–1445. doi: 10.1242/jcs.114.8.1439. [DOI] [PubMed] [Google Scholar]
- Vanhaesebroeck B, Waterfield MD. Signaling by distinct classes of phosphoinositide 3-kinases. Exp Cell Res. 1999;253:239–254. doi: 10.1006/excr.1999.4701. [DOI] [PubMed] [Google Scholar]
- Leslie NR, Downes CP. PTEN: The down side of PI 3-kinase signalling. Cellular Signalling. 2002;14:285–295. doi: 10.1016/S0898-6568(01)00234-0. [DOI] [PubMed] [Google Scholar]
- Maehama T, Dixon JE. PTEN: a tumour suppressor that functions as a phospholipid phosphatase. Trends Cell Biol. 1999;9:125–128. doi: 10.1016/S0962-8924(99)01519-6. [DOI] [PubMed] [Google Scholar]
- Cantley LC, Neel BG. New insights into tumor suppression: PTEN suppresses tumor formation by restraining the phosphoinositide 3-kinase/AKT pathway. Proc Natl Acad Sci U S A. 1999;96:4240–4245. doi: 10.1073/pnas.96.8.4240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liaw D, Marsh DJ, Li J, Dahia PL, Wang SI, Zheng Z, et al. Germline mutations of the PTEN gene in Cowden disease, an inherited breast and thyroid cancer syndrome. Nat Genet. 1997;16:64–67. doi: 10.1038/ng0597-64. [DOI] [PubMed] [Google Scholar]
- Ali IU, Schriml LM, Dean M. Mutational spectra of PTEN/MMAC1 gene: a tumor suppressor with lipid phosphatase activity. J Natl Cancer Inst. 1999;91:1922–1932. doi: 10.1093/jnci/91.22.1922. [DOI] [PubMed] [Google Scholar]
- Dahia PL. PTEN, a unique tumor suppressor gene. Endocr Relat Cancer. 2000;7:115–129. doi: 10.1677/erc.0.0070115. [DOI] [PubMed] [Google Scholar]
- Davies MA, Koul D, Dhesi H, Berman R, McDonnell TJ, McConkey D, et al. Regulation of Akt/PKB activity, cellular growth, and apoptosis in prostate carcinoma cells by MMAC/PTEN. Cancer Res. 1999;59:2551–2556. [PubMed] [Google Scholar]
- Di Cristofano A, Pandolfi PP. The multiple roles of PTEN in tumor suppression. Cell. 2000;100:387–390. doi: 10.1016/s0092-8674(00)80674-1. [DOI] [PubMed] [Google Scholar]
- Yamada KM, Araki M. Tumor suppressor PTEN: modulator of cell signaling, growth, migration and apoptosis. J Cell Sci. 2001;114:2375–2382. doi: 10.1242/jcs.114.13.2375. [DOI] [PubMed] [Google Scholar]
- Teng DH, Hu R, Lin H, Davis T, Iliev D, Frye C, et al. MMAC1/PTEN mutations in primary tumor specimens and tumor cell lines. Cancer Res. 1997;57:5221–5225. [PubMed] [Google Scholar]
- Ramaswamy S, Nakamura N, Vazquez F, Batt DB, Perera S, Roberts TM, et al. Regulation of G1 progression by the PTEN tumor suppressor protein is linked to inhibition of the phosphatidylinositol 3-kinase/Akt pathway. Proc Natl Acad Sci U S A. 1999;96:2110–2115. doi: 10.1073/pnas.96.5.2110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suzuki A, de la Pompa JL, Stambolic V, Elia AJ, Sasaki T, del Barco Barrantes I, et al. High cancer susceptibility and embryonic lethality associated with mutation of the PTEN tumor suppressor gene in mice. Curr Biol. 1998;8:1169–1178. doi: 10.1016/S0960-9822(07)00488-5. [DOI] [PubMed] [Google Scholar]
- Stambolic V, Tsao MS, Macpherson D, Suzuki A, Chapman WB, Mak TW. High incidence of breast and endometrial neoplasia resembling human Cowden syndrome in pten+/- mice. Cancer Res. 2000;60:3605–3611. [PubMed] [Google Scholar]
- Podsypanina K, Ellenson LH, Nemes A, Gu J, Tamura M, Yamada KM, et al. Mutation of Pten/Mmac1 in mice causes neoplasia in multiple organ systems. Proc Natl Acad Sci U S A. 1999;96:1563–1568. doi: 10.1073/pnas.96.4.1563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Testa JR, Bellacosa A. AKT plays a central role in tumorigenesis. PNAS. 2001;98:10983–10985. doi: 10.1073/pnas.211430998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Datta SR, Brunet A, Greenberg ME. Cellular survival: a play in three Akts. Genes Dev. 1999;13:2905–2927. doi: 10.1101/gad.13.22.2905. [DOI] [PubMed] [Google Scholar]
- Datta SR, Dudek H, Tao X, Masters S, Fu H, Gotoh Y, et al. Akt phosphorylation of BAD couples survival signals to the cell-intrinsic death machinery. Cell. 1997;91:231–241. doi: 10.1016/S0092-8674(00)80405-5. [DOI] [PubMed] [Google Scholar]
- del Peso L, Gonzalez-Garcia M, Page C, Herrera R, Nunez G. Interleukin-3-induced phosphorylation of BAD through the protein kinase Akt. Science. 1997;278:687–689. doi: 10.1126/science.278.5338.687. [DOI] [PubMed] [Google Scholar]
- Kim AH, Khursigara G, Sun X, Franke TF, Chao MV. Akt phosphorylates and negatively regulates apoptosis signal-regulating kinase 1. Mol Cell Biol. 2001;21:893–901. doi: 10.1128/MCB.21.3.893-901.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cardone MH, Roy N, Stennicke HR, Salvesen GS, Franke TF, Stanbridge E, et al. Regulation of cell death protease caspase-9 by phosphorylation. Science. 1998;282:1318–1321. doi: 10.1126/science.282.5392.1318. [DOI] [PubMed] [Google Scholar]
- Cheney IW, Neuteboom ST, Vaillancourt MT, Ramachandra M, Bookstein R. Adenovirus-mediated gene transfer of MMAC1/PTEN to glioblastoma cells inhibits S phase entry by the recruitment of p27Kip1 into cyclin E/CDK2 complexes. Cancer Res. 1999;59:2318–2323. [PubMed] [Google Scholar]
- Weng LP, Brown JL, Eng C. PTEN coordinates G(1) arrest by down-regulating cyclin D1 via its protein phosphatase activity and up-regulating p27 via its lipid phosphatase activity in a breast cancer model. Hum Mol Genet. 2001;10:599–604. doi: 10.1093/hmg/10.6.599. [DOI] [PubMed] [Google Scholar]
- Winter RN, Kramer A, Borkowski A, Kyprianou N. Loss of Caspase-1 and Caspase-3 Protein Expression in Human Prostate Cancer. Cancer Res. 2001;61:1227–1232. [PubMed] [Google Scholar]
- Pugazhenthi S, Nesterova A, Sable C, Heidenreich KA, Boxer LM, Heasley LE, et al. Akt/protein kinase B up-regulates Bcl-2 expression through cAMP-response element-binding protein. J Biol Chem. 2000;275:10761–10766. doi: 10.1074/jbc.275.15.10761. [DOI] [PubMed] [Google Scholar]
- Scrimgeour AG, Blakesley VA, Stannard BS, LeRoth D. Mitogen-activated protein kinase and phosphatidylinositol 3-kinase pathways are not sufficient for insulin-like growth factor I-induced mitogenesis and tumorigenesis. Endocrinology. 1997;138:2552–2558. doi: 10.1210/en.138.6.2552. [DOI] [PubMed] [Google Scholar]
- Ni Z, Lou W, Leman ES, Gao AC. Inhibition of Constitutively Activated Stat3 Signaling Pathway Suppresses Growth of Prostate Cancer Cells. Cancer Res. 2000;60:1225–1228. [PubMed] [Google Scholar]
- Baserga R. The IGF-I receptor in cancer research. Exp Cell Res. 1999;253:1–6. doi: 10.1006/excr.1999.4667. [DOI] [PubMed] [Google Scholar]
- LeRoith D, Baserga R, Helman L, Roberts CT. Insulin-like growth factors and cancer. Ann Intern Med. 1995;122:54–59. doi: 10.7326/0003-4819-122-1-199501010-00009. [DOI] [PubMed] [Google Scholar]
- LeRoith D, Werner H, Beitner-Johnson D, Roberts CTJ. Molecular and cellular aspects of the insulin-like growth factor I receptor. Endocr Rev. 1995;16:143–163. doi: 10.1210/er.16.2.143. [DOI] [PubMed] [Google Scholar]
- Luttrell LM, Van Biesen T, Hawes BE, Koch WJ, Touhara K, Lefkowitz RJ. G beta gamma subunits mediate mitogen-activated protein kinase activation by the tyrosine kinase insulin-like growth factor 1 receptor. J Biol Chem. 1995;270:16495–16498. doi: 10.1074/jbc.270.28.16495. [DOI] [PubMed] [Google Scholar]
- Zong CS, Zeng L, Jiang Y, Sadowski HB, Wang LH. Stat3 plays an important role in oncogenic Ros- and insulin-like growth factor I receptor-induced anchorage-independent growth. J Biol Chem. 1998;273:28065–28072. doi: 10.1074/jbc.273.43.28065. [DOI] [PubMed] [Google Scholar]
- Accili D, Nakae J, Kim JJ, Park BC, Rother KI. Targeted gene mutations define the roles of insulin and IGF-I receptors in mouse embryonic development. J Pediatr Endocrinol Metab. 1999;12:475–485. doi: 10.1515/jpem.1999.12.4.475. [DOI] [PubMed] [Google Scholar]
- Baserga R. The insulin-like growth factor I receptor: a key to tumor growth? Cancer Res. 1995;55:249–252. [PubMed] [Google Scholar]
- Baserga R, Hongo A, Rubini M, Prisco M, Valentinis B. The IGF-I receptor in cell growth, transformation and apoptosis. Biochim Biophys Acta. 1997;1332:F105–126. doi: 10.1016/S0304-419X(97)00007-3. [DOI] [PubMed] [Google Scholar]
- Baserga R, Resnicoff M, Dews M. The IGF-I receptor and cancer. Endocrine. 1997;7:99–102. doi: 10.1007/BF02778073. [DOI] [PubMed] [Google Scholar]
- Pollak M, Beamer W, Zhang JC. Insulin-like growth factors and prostate cancer. Cancer Metastasis Rev. 1999;17:1998–383. doi: 10.1023/a:1006154108619. [DOI] [PubMed] [Google Scholar]
- Yee D. The insulin-like growth factor system as a target in breast cancer. Breast Cancer Res Treat. 1994;32:85–95. doi: 10.1007/BF00666209. [DOI] [PubMed] [Google Scholar]
- Resnik JL, Reichart DB, Huey K, Webster NJ, Seely BL. Elevated insulin-like growth factor I receptor autophosphorylation and kinase activity in human breast cancer. Cancer Res. 1998;58:1159–1164. [PubMed] [Google Scholar]
- Ogino S, Kubo S, Abdul-Karim FW, Cohen ML. Comparative immunohistochemical study of insulin-like growth factor II and insulin-like growth factor receptor type 1 in pediatric brain tumors. Pediatr Dev Pathol. 2001;4:23–31. doi: 10.1007/s100240010112. [DOI] [PubMed] [Google Scholar]
- Antoniades HN, Galanopoulos T, Neville-Golden J, Maxwell M. Expression of insulin-like growth factors I and II and their receptor mRNAs in primary human astrocytomas and meningiomas; in vivo studies using in situ hybridization and immunocytochemistry. Int J Cancer. 1992;50:215–222. doi: 10.1002/ijc.2910500210. [DOI] [PubMed] [Google Scholar]
- Gammeltoft S, Ballotti R, Nielsen FC, Kowalski A, Van Obberghen E. Receptors for insulin-like growth factors in the central nervous system: structure and function. Horm Metab Res. 1988;20:436–442. doi: 10.1055/s-2007-1010854. [DOI] [PubMed] [Google Scholar]
- Sandberg AC, Engberg C, Lake M, von Holst H, Sara VR. The expression of insulin-like growth factor I and insulin-like growth factor II genes in the human fetal and adult brain and in glioma. Neurosci Lett. 1988;93:114–119. doi: 10.1016/0304-3940(88)90022-5. [DOI] [PubMed] [Google Scholar]
- Wick W, Furnari FB, Naumann U, Cavenee WK, Weller M. PTEN gene transfer in human malignant glioma: sensitization to irradiation and CD95L-induced apoptosis. Oncogene. 1999;18:3936–3943. doi: 10.1038/sj.onc.1202774. [DOI] [PubMed] [Google Scholar]
- Lammers R, Van Obberghen E, Ballotti R, Schlessinger J, Ullrich A. Transphosphorylation as a possible mechanism for insulin and epidermal growth factor receptor activation. J Biol Chem. 1990;265:16886–16890. [PubMed] [Google Scholar]
- Treadway JL, Morrison BD, Soos MA, Siddle K, Olefsky J, Ullrich A, et al. Transdominant inhibition of tyrosine kinase activity in mutant insulin/insulin-like growth factor I hybrid receptors. Proc Natl Acad Sci USA. 1991;88:214–218. doi: 10.1073/pnas.88.1.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seely BL, Reichart DR, Takata Y, Yip C, Olefsky JM. A functional assessment of insulin/insulin-like growth factor-I hybrid receptors. Endocrinology. 1995;136:1635–1641. doi: 10.1210/en.136.4.1635. [DOI] [PubMed] [Google Scholar]
- Kalebic T, Blakesley V, Slade C, Plasschaert S, Leroith D, Helman LJ. Expression of a kinase-deficient IGF-I-R suppresses tumorigenicity of rhabdomyosarcoma cells constitutively expressing a wild type IGF-I-R. Int J Cancer. 1998;76:223–227. doi: 10.1002/(SICI)1097-0215(19980413)76:2<223::AID-IJC9>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- Burgaud JL, Resnicoff M, Baserga R. Mutant IGF-I receptors as dominant negatives for growth and transformation. Biochem Biophys Res Commun. 1995;214:475–481. doi: 10.1006/bbrc.1995.2311. [DOI] [PubMed] [Google Scholar]
- Hsu D, Knudson PE, Zapf A, Rolband GC, Olefsky JM. NPXY motif in the insulin-like growth factor-I receptor is required for efficient ligand-mediated receptor internalization and biological signaling. Endocrinology. 1994;134:744–750. doi: 10.1210/en.134.2.744. [DOI] [PubMed] [Google Scholar]
- Cheney IW, Johnson DE, Vaillancourt MT, Avanzini J, Morimoto A, Demers GW, et al. Suppression of tumorigenicity of glioblastoma cells by adenovirus-mediated MMAC1/PTEN gene transfer. Cancer Res. 1998;58:2331–2334. [PubMed] [Google Scholar]
- Arteaga CL, Kitten LJ, Coronado EB, Jacobs S, Kull FC, Allred DG, et al. Blockade of the type I somatomedin receptor inhibits growth of human breast cancer cells in athymic mice. J Clin Invest. 1989;84:1418–1423. doi: 10.1172/JCI114315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrews DW, Resnicoff M, Flanders AE, Kenyon L, Curtis M, Merli G, et al. Results of a Pilot Study Involving the Use of an Antisense Oligodeoxynucleotide Directed Against the Insulin-Like Growth Factor Type I Receptor in Malignant Astrocytomas. J Clin Oncol. 2001;19:2189–2200. doi: 10.1200/JCO.2001.19.8.2189. [DOI] [PubMed] [Google Scholar]
- Friedmann T, Yee JK. Pseudotyped retroviral vectors for studies of human gene therapy. Nat Med. 1995;1:275–277. doi: 10.1038/nm0395-275. [DOI] [PubMed] [Google Scholar]