Hairdressing is one of the occupations most hazardous to the skin.1 Various efforts have been made in Germany in the past 10 years to reduce the incidence of occupational skin diseases among hairdressers.2,3 Two legislative regulations introduced as Technical Rules for Hazardous Substances 530 “Hairdressing trade” and 531 “Endangerment of the skin by work in the wet environment (wet work)” came fully into force in September 1992 and September 1996.
Because of the high cost of medical treatment, professional retraining, and disability pensions for hairdressers with an occupational skin disease, the Statutory Accident Insurance Institution for the Health and Welfare Services (workers' compensation board) coupled the new technical rules with information campaigns and passed a resolution in 1994 to strengthen “secondary individual prevention,” in accordance with the Ordinance on Industrial Disease. Sensitisation to glyceryl monothioglycolate is common, and in 1995 hair cosmetics manufacturers agreed with the hairdressers' guild to stop the use of this allergen in permanent wave solutions. The Health and Safety Authority in Bavaria started educational and enforcement activities to ensure that the new regulations were put into practice.
We analysed data from our register of occupational skin diseases in Northern Bavaria1 to determine whether a downward trend in the annual incidence of occupational skin disease in hairdressers could be observed.
Methods and results
We identified hairdressers from all initial reports of occupational skin diseases (5285 cases) registered between 1990 and 1999. Of the 997 initial reports of occupational skin disease in hairdressers, 856 (85.9%) cases had a confirmed occupational cause.
Because of asymmetry, we used median and quartiles (Q1, Q3) for statistical description of distributions. We calculated incidences as the number of occupational skin diseases per 10 000 workers per year. We calculated asymptotic 95% confidence intervals according to standard theory. To test for linear trend of rates we used the Cochran-Armitage trend test.4 We used SAS 8.1 (SAS Institute, Cary, NC) for data analysis.
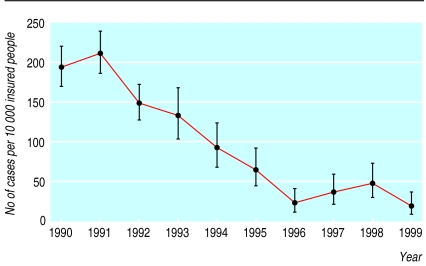
The hairdressers with a stated occupational skin disease had a median age of 20 (Q1 18, Q3 22) years and a median occupational period of exposure of 24 (Q1 12, Q3 48) months. The annual incidence fell from 194 to 18 cases per 10 000 workers between 1990 and 1999 (figure), which is not only highly significant (P<0.0001) but also of clinical importance as it corresponds to a 10-fold decline in the annual incidence.
Comment
An impressive downward trend in cases of occupational skin diseases in hairdressers has occurred in Northern Bavaria over the past decade. This seems to reflect improvements in working conditions due to new legislation and intensified preventive measures rather than a change in the natural history of occupational skin disease.5 Because of the size of the region studied and the sampling scheme, the findings can be generalised and applied to Germany as a whole.2,3
Although the prognosis for recovery from occupational skin disease has not changed significantly over the past five decades,5 cooperation between dermatologists, government physicians, employers, employees, the competent workers' compensation board, the hairdressers' guild, hair cosmetics manufacturers, and legislative authorities has led to a reduction in occupational skin diseases in hairdressing. However, to achieve a longlasting reduction, interdisciplinary cooperation must be continued and primary prevention should start as early as possible, preferably by legally binding supplementary medical pre-employment examination.2 The Principle G24 “Skin diseases (other than skin cancer)” is under discussion in Germany.
Figure.
Annual incidence (95% confidence interval) of hairdressers with a stated occupational skin disease. Data are for Upper Palatinate, Upper-Franconia, Middle-Franconia, and Lower-Franconia (Northern Bavaria) from 1990 to 1992 and, after governmental reorganisation, for Upper-Franconia and Middle-Franconia from 1993 to 1999
Footnotes
Funding: None.
Competing interests: None declared.
References
- 1.Dickel H, Kuss O, Blesius CR, Schmidt A, Diepgen TL. Occupational skin diseases in Northern Bavaria between 1990 and 1999: a population-based study. Br J Dermatol. 2001;145:453–462. doi: 10.1046/j.1365-2133.2001.04377.x. [DOI] [PubMed] [Google Scholar]
- 2.Schlesinger T, Revermann K, Schwanitz HJ. Contact dermatitis in hairdresser trainees in Lower Saxony, Germany: a comparison between 1989, 1994 and 1999 [in German] Dermatol Beruf Umwelt. 2001;49:185–192. [Google Scholar]
- 3.Stresemann E, Lücke A, Brauel R, Scharrer E. Did the Regulation for Hazardous Materials (German TRGS 530) contribute to the diminution of dermatoses in hairdressers? [in German] Dermatosen. 1998;46:166–169. [Google Scholar]
- 4.Agresti A. Categorical data analysis. 1st ed. Chichester: John Wiley and Sons; 1990. [Google Scholar]
- 5.Hogan DJ. The prognosis of occupational contact dermatitis. Occup Med. 1994;9:53–58. [PubMed] [Google Scholar]