Abstract
Objective
To develop a medication literacy intervention program for glaucoma and test its effects on medication literacy, medication self-efficacy and medication adherence.
Methods
The intervention was constructed according to the Information-Motivation-Behavioral skills Model and the Health Belief Model. Preliminary protocols were revised through expert group meetings and pre-experiments to form a formal intervention plan. Subsequently, 66 patients with glaucoma were enrolled and randomly assigned to the control and intervention groups. The control group was received with routine follow-up and education for glaucoma patients, while the intervention group was given an 8-weeks medication literacy intervention for glaucoma patients. Before the implementation of the intervention and at the end of the 8th week of the intervention, the Chinese Version of the Medication Literacy Scale, the Short Version of the Glaucoma Medication Self-Efficacy Questionnaire and the Chinese version of the Morisky Medication Adherence Scale-8 were used to evaluate the medication literacy level, medication self-efficacy and medication adherence of glaucoma patients in the intervention group and the control group.
Results
We developed an 8-weeks multi-component medication literacy intervention for glaucoma. Before the start of the intervention, there were no statistically significant differences in the scores of medication literacy, medication self-efficacy and medication adherence between the control group and the intervention group. After the intervention, the medication literacy, medication self-efficacy, and medication adherence of the intervention patients were significantly better than those of the control group (P<0.05).
Conclusion
The 8-weeks multi-component intervention for glaucoma patients can improve their medication literacy, medication self-efficacy, and medication adherence.
Keywords: glaucoma, medication adherence, medication literacy, nursing evaluation research, self-efficacy
Introduction
Glaucoma, a multifactorial, complex optic nerve degenerative eye disease, is the leading cause of irreversible blindness worldwide.1 The global prevalence of glaucoma in people aged 40 to 80 years is estimated to be 3.5%. With the growing number and proportion of older persons in the population, it is projected that 111.8 million people will have glaucoma in 2040.2 For glaucoma, pathological elevated intraocular pressure is the primary risk factor for disease progression.3,4 And the use of eye drops to control intraocular pressure is currently the main means to delay the development of glaucoma.5–7 The standardized use of eye drops can effectively prevent further visual damage in about 60% of glaucoma patients, and it is also an important part of the secondary prevention of glaucoma and a key factor affecting the outcome of the disease.8–10
Although the standardized use of eye drops is essential for remission in patients with glaucoma, several studies have shown that the current medication situation for patients with glaucoma is not ideal. One study found that about 27% of patients with glaucoma had poor medication adherence.11 Another survey of 14,648 glaucoma patients showed that 48.1% of respondents failed to use their eye drops as prescribed.12 In addition, studies have also shown that the instillation technique in glaucoma patients is not sufficient to enable them to properly complete the instillation of eye drops.13,14 Therefore, how to effectively regulate the medication behavior of glaucoma patients is an urgent visual health problem to be solved. The gradual rise of medication literacy research provides new ideas for solving this problem.
Medication literacy (ML), first mentioned in a government document in the UK in 2005, is a subdivision of health literacy in the field of pharmacy.15 Medication literacy is defined as
the degree to which individuals can obtain, comprehend, communicate, calculate and process patient-specific information about their medications to make informed medication and health decisions in order to safely and effectively use their medications, regardless of the mode by which the content is delivered. (e.g. written, oral and visual)
16 Medication literacy involves the knowledge literacy, attitude literacy, ability literacy, and behavior literacy of the patient in the process of medication.17 It can serve as an important predictor of rational medication use.18,19 Some studies have shown that patients with lower medication literacy have more irregular medication behavior.20–22 Some interventional studies have also shown that improving the medication literacy level of patients can better regulate their medication behavior.23–25
However, there are currently no reports on intervention studies specifically targeting medication literacy in glaucoma. This study developed an intervention specifically designed to improve medication literacy in glaucoma, which we named “G-MedLit intervention”. The G-MedLit intervention were designed and assessed through a randomized controlled trial design.
Methods
Building Intervention
Intervention Model Development
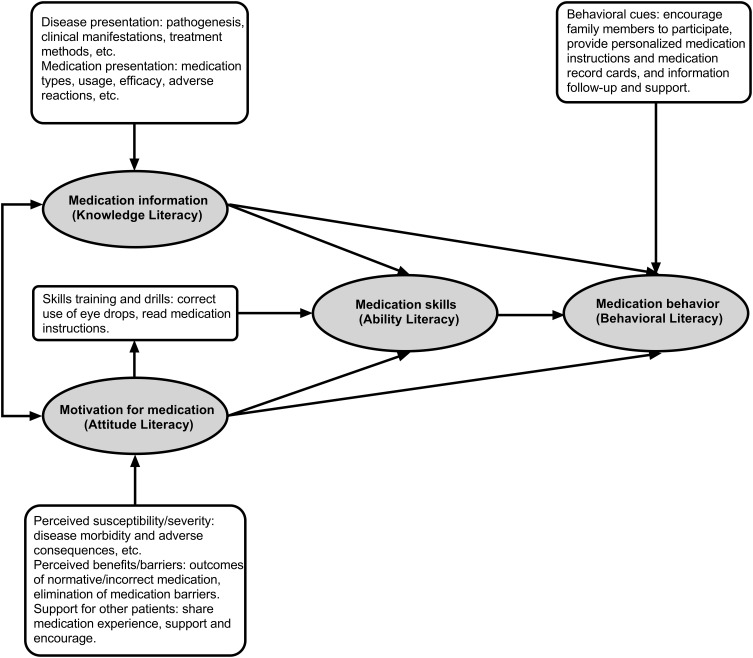
The model of G-MedLit intervention was based on the Information-Motivation-Behavioral skills Model (IMB) and the Health Belief Model (HBM). IMB explores the relationship between the four core elements of information, motivation, skills, and behavior. IMB believes that healthy behaviors will be initiated and maintained when individuals have sufficient health information, sufficient motivation to take healthy actions, and have relevant behavioral skills.26 It is similar to the four elements (Knowledge literacy, Attitude literacy, Ability literacy, Behavior literacy) in medication literacy. So IMB was used as the theoretical basis for the building of G-MedLit intervention. HBM is an important theory for exploring individual health behavior. It strengthens people internal health beliefs by clarifying the perception of danger (perceived susceptibility, perceived severity), emphasizing the perceived benefits, and eliminating perception barriers, and improving patients’ motivation and willingness to adopt healthy behaviors.27 In this study, HBM was introduced to fully mobilize the enthusiasm of glaucoma to participate in G-MedLit intervention and help patients maintain standardized medication behavior for a long time. Eventually, we built the model of G-MedLit intervention, as detailed in Figure 1. And the specific implementation content of the intervention (first edition) was constructed under the guidance of this model.
Figure 1.
The model of G-MedLit intervention.
Revising Intervention
A multidisciplinary expert team that included ophthalmologists, nurses, pharmacists, and methodologists acted as the multidisciplinary steering group for the revision of G-MedLit intervention. They were not involved in the build process of the first version of G-MedLit intervention. The multidisciplinary steering group convened an expert group meeting to discuss, evaluate and revise the necessity, scientificity and feasibility of the first edition of G-MedLit intervention, and formed the second edition of G-MedLit intervention. The expert inclusion criteria were as follows: (1) has work experience in the field of ophthalmology, nursing, or pharmacy for 10 years or more; (2) has a master’s or higher degree or an associate senior or higher rank in any of the fields; (3) has an intermediate and above professional title in the related field; (4) has been informed and consented to participate in this study.
Subsequently, we invited 10 glaucoma patients to participate in a pre-pilot study to obtain patient feedback on G-MedLit intervention. Based on the recommendations of these patients, we refined the second edition of G-MedLit intervention. Eventually, we built the final version of G-MedLit intervention.
The details of G-MedLit intervention are presented in the Electronic Supplementary Material 1.
Evaluation of the Effect of Intervention
Study Design
This was a 2-group, randomized controlled trial. We tested the efficacy of G-MedLit intervention on glaucoma’s medication literacy, medication self-efficacy and medication adherence.
The patients in the control group were treated with routine follow-up and education procedures for glaucoma outpatients. Specific steps: (1) Establish a follow-up file for each patient. (2) The follow-up nurse of the glaucoma group of the department adds the patients’ WeChat (a popular cross-platform communication tool in China), and the patients can consult through the WeChat if they have any disease problems during their stay at home. (3) Use follow-up WeChat moments to push glaucoma-related knowledge to patients once a month. (4) Send reminder text messages to patients who need to come to the hospital for a follow-up one week in advance.
The intervention group was given the 8-weeks G-MedLit intervention. Each week, patients were provided with a specific theme of intervention: (1) Communication and Assessment, (2) Accumulation and Motivation Stimulation - Disease Knowledge, (3) Information Accumulation and Motivation Stimulation - Knowledge of Medication, (4) Medium-term Feedback and Incentives, (5) Share and Communicate, (6) Skills Training 1 - Proper Use of Eye Drops, (7) Skills Training 2 - Read the Medication Leaflet, (8) Final Evaluation and Feedback. And at the same time, the objectives and specific content of the intervention were set for each theme. The details of G-MedLit intervention are presented in the Electronic Supplementary Material 1.
Participants and Setting
The participants were recruited from the Eye Clinic of Southwest Hospital, China. Written informed consent was obtained from all participants before their engagement in the study. In this study, patients were eligible for inclusion in the study if they: (1) diagnosed with glaucoma by an ophthalmologist; (2) using eye drops for more than 2 months; (3) older than 18 years; (4) able to recognize all the words mentioned in this research questionnaire; (5) able to use smartphones and WeChat; (6) Voluntary participation in this study. Participants were excluded if they were unwilling to stay in the study, developed serious health conditions, or failed to participate in the study intervention twice in a row.
Sample Size
The sample size was calculated using the sample size calculation formula for comparing the mean of two independent samples
Sampling and Randomization
A total of 248 glaucoma patients were evaluated for eligibility prior to the start of the study. Eventually, 66 eligible glaucoma patients were randomly allocated to an intervention group and a control group through block randomization. The allocation sequence was generated using the Statistical Package for Social Sciences (SPSS, version 26.0). Subsequently, based on generated random sequence, cards A (intervention) and B (control) were placed in an opaque envelope. Participants were divided into either an intervention or a control group based on the results in the envelope until the number of patients in both groups reached 33.
Data Collection
We developed the general information questionnaire for glaucoma patients, which included 8 items of demographic factors (age, gender, place of residence, education level, nature of work, marital status, whether they live alone, family income) and 7 items of disease-related factors (duration of illness, family history of glaucoma, history of glaucoma surgery, type of medication, number of daily medications, medication education, and presence of other chronic diseases).
The primary outcome in this study was the patient’s medication literacy and the secondary outcomes were the patient’s self-efficacy and adherence of medication. The primary and secondary outcomes were measured at the beginning of the study and eight weeks afterward. Data collection tools were the Chinese Version of the Medication Literacy Scale (CVMLS), the Short Version of the Glaucoma Medication Self-Efficacy Questionnaire (SVGMSEQ) and the Chinese version of the Morisky Medication Adherence Scale-8 (C-MMAS-8).
The Chinese Version of the Medication Literacy Scale was used for medication literacy assessment. The Medication Literacy Assessment in English and Spanish (MedLitRxSE) was developed by Sauceda et al from the University of Texas in 2012.15 The scale is a universal scale used to measure the medication literacy of patients. It has good reliability and validity, and is the best assessment tool for medication literacy at present.28 The scale consists of four scenarios: injectable medication for diabetes, medication for children, antibiotic use, and over-The-counter and supplementary prescriptions. The scale consists of 14 items, with 1 point for each item answered correctly and 0 points for incorrect answers; the maximum score for the scale is 14 points; higher scores indicate superior medication literacy. In 2016, the MedLitRxSE was translated into Chinese by Zheng et al.29 The test-retest reliability of the Chinese version of the Medication Literacy Assessment Scale is 0.885, the split-half reliability is 0.840, and the correlation coefficient between each item of the scale and the total score of the scale is 0.427–0.587.
The Short Version of the Glaucoma Medication Self-Efficacy Questionnaire (SVGMSEQ) was used to measure the Glaucoma Medication Self-Efficacy. To our knowledge, this questionnaire is currently the only specialized assessment tool for glaucoma medication self-efficacy and has good reliability and validity. It was developed by Sleath et al from the University of North Carolina in 2012.30 The questionnaire consists of two subscales, which evaluate the confidence of glaucoma patients in following medical advice in 10 possible situations that may hinder medication and the confidence of correctly completing 6 eye drops procedures. All 16 items are scored on a 3-point Likert scale as the following: “not at all confident” = 1, “somewhat confident” = 2, “very confident” = 3; and the higher the total score, the higher the glaucoma medication self-efficacy. Our research team translated the questionnaire into Chinese and verified its reliability and validity.31 The Cronbach′s α coefficients of the two subscales were 0.924 and 0.818, the half-way reliability was 0.892 and 0.827, and the test-retest reliability was 0.842 and 0.903.
The eight-item Morisky Medication Adherence Scale (MMAS-8) was used for medication adherence assessment. The MMAS-8 instrument is a structured self-reported measure of medication-taking behavior that has been widely used in various countries for a number of different conditions.32–34 In this scale, yes and no are the answer options for seven items, and the last question is answered on a 5-point Likert scale. The total score on this scale ranges from 0–8. Higher scores represent better adherence to glaucoma medication. Morisky’s suggested cut-off point of 6 was applied: MMAS score < 6 (low adherence), score = 8 (high adherence), and score ≥ 6, and < 8 (medium adherence). The Chinese version of the MMAS-8 (C-MMAS-8) was translated by Yan.35 It has good reliability and validity (Cronbach’s α = 0.77, Test-retest reliability r = 0.88) in Yan’s study. Our team had obtained the license of the MMAS-8.
Statistical Analysis
Data analysis was performed using the Statistical Package for Social Sciences (SPSS, version 26.0). According to the characteristics of the data, the t-test, the Mann–Whitney U-test, the Chi square test or the Fisher’s test were selected to compare the differences between the data. All statistical analyses were performed at a significance level of less than 0.05.
Ethics Approval
The verbal and written consent of the patients to participate in this study were obtained before their interview. This study was registered at clinicaltrials.gov with Identification Number ChiCTR2300070522, was approved by the Ethics Committee of the First Affiliated Hospital of Army Medical University (NO. KY202276), and was conducted in accordance with the Declaration of Helsinki. The participants were informed that they had the right to withdraw from the study at any time. All of them were assured that their names, interview transcripts, and other personal data would be kept confidential.
Results
Sample Characteristics
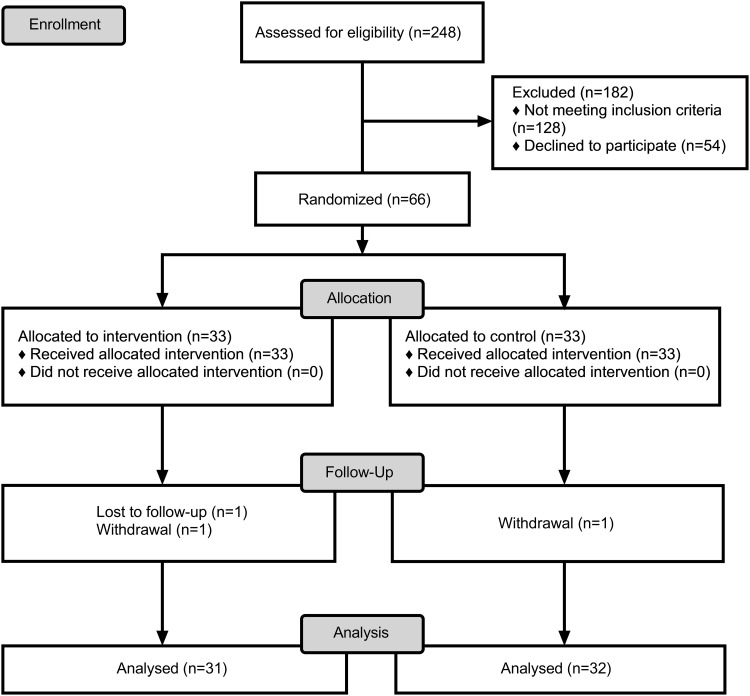
In total, 248 patients were assessed for eligibility, among them 128 were ineligible and 54 did not consent for participation. The remaining 66 patients were evenly allocated to the study groups. However, two patients from the intervention group were excluded due to either unwillingness to receive the study intervention (n = 1) or not participating in the intervention measures twice in a row (n = 1). Moreover, one patient from the control group voluntarily withdrew from the study and hence, was excluded. Consequently, the study was completed with 31 participants in the intervention group and 32 participants in the control group. The adherence rate of the intervention group was 93.93% (31/33). The flow of study participants is detailed in Figure 2. Table 1 contains complete participant characteristics and pre-intervention comparisons between groups. Groups did not differ on demographic factors and disease-related factors at baseline.
Figure 2.
The flow of participants in the study (CONSORT Flow Diagram).
Table 1.
Baseline Characteristics of Participants [M (P25, P75) / n (%)]
| Characteristic | Intervention (n=31) | Control (n=32) | P-Value | |
|---|---|---|---|---|
| Age, years | 55.00(40.00,64.00) | 58.00(40.75,67.75) | 0.550a | |
| Gender | 0.367b | |||
| Man | 19(61.29) | 16(50.00) | ||
| Woman | 12(38.71) | 16(50.00) | ||
| Place of residence | 0.535b | |||
| Countryside | 15(48.39) | 13(40.63) | ||
| City | 16(51.61) | 19(59.37) | ||
| Education | 0.253c | |||
| Junior high school and below | 22(70.97) | 20(62.50) | ||
| Technical secondary school and high school | 2(6.45) | 6(18.75) | ||
| College | 4(12.90) | 1(3.13) | ||
| Bachelor’s degree or above | 3(9.68) | 5(15.62) | ||
| Nature of work | 0.476b | |||
| Mental | 9(29.03) | 12(37.50) | ||
| Physical | 22(70.97) | 20(62.50) | ||
| Marital status | 0.638d | |||
| Single | 4(12.90) | 2(6.25) | ||
| Married | 27(87.10) | 30(93.75) | ||
| Residency | 0.179b | |||
| Living alone | 8(25.81) | 4(12.50) | ||
| Living with family/friends | 23(74.19) | 28(87.50) | ||
| Per capita monthly household income (RMB) | 0.400c | |||
| <3000 | 4(12.90) | 1(3.13) | ||
| 3000–4999 | 18(58.07) | 18(56.25) | ||
| 5000–8000 | 9(29.03) | 12(37.50) | ||
| >8000 | 0(0.00) | 1(3.12) | ||
| Duration of illness (months) | 0.410b | |||
| <6 | 13(41.94) | 10(31.25) | ||
| 6–11 | 5(16.13) | 7(21.88) | ||
| 12–36 | 6(19.35) | 5(15.62) | ||
| >36 | 7(22.58) | 10(31.25) | ||
| Family history of glaucoma | 1.000d | |||
| Yes | 1(3.23) | 2(6.25) | ||
| No | 30(96.77) | 30(93.75) | ||
| Glaucoma surgery | 0.382b | |||
| Yes | 16(51.61) | 13(40.63) | ||
| No | 15(48.39) | 19(59.37) | ||
| Type of medication | 0.429c | |||
| 1 | 1(3.23) | 1(3.12) | ||
| 2 | 7(22.58) | 13(40.63) | ||
| 3 | 14(45.16) | 12(37.50) | ||
| >3 | 9(29.03) | 6(18.75) | ||
| Number of doses per day | 0.599c | |||
| 2 | 1(3.23) | 1(3.12) | ||
| 3 | 4(12.90) | 8(25.00) | ||
| >3 | 26(83.87) | 23(71.88) | ||
| Education on medication | 0.514b | |||
| Yes | 9(29.03) | 7(21.87) | ||
| No | 22(70.97) | 25(78.13) | ||
| Other chronic medical conditions | 0.348b | |||
| Yes | 4(12.90) | 7(21.87) | ||
| No | 27(87.10) | 25(78.13) | ||
Notes: aThe results of the Mann–Whitney U-test, bThe results of the chi-square test, cThe results of the Fisher’s test, dThe results of the Calibration chi-square test.
Intervention Effect
At baseline, there was no difference between the groups in medication literacy, self-efficacy and adherence of medication. After the 8 weeks of G-MedLit intervention, the level of medication literacy in the intervention group was significantly higher than that in the control group. Moreover, the medication self-efficacy and medication adherence in the intervention group were also significantly higher than those in the control group after the intervention. Table 2 shows the comparison of CVMLS, SVGMSEQ and MMAS-8 scores between the two groups before and after the intervention.
Table 2.
Comparing the Scores of CVMLS, SVGMSEQ and MMAS-8
| Group Outcomes | Intervention (n = 31) | Control (n = 32) | P-Value | |
|---|---|---|---|---|
| CVMLS |
Pre-test | 7.48±3.62 | 7.44±3.29 | 0.958a |
| Post-test | 10.65±2.58 | 7.63±3.41 | <0.001a | |
| P-value | <0.001c | 0.084c | ||
| SVGMSEQ [M (P25, P75)] | Pre-test | 38.00(30.00,41.00) | 39.00(32.00,41.00) | 0.918b |
| Post-test | 44.00(40.00,46.00) | 39.50(34.50,42.00) | 0.001b | |
| P-value | <0.001c | <0.001c | ||
| MMAS-8 |
Pre-test | 5.10±1.60 | 5.12±1.72 | 0.977a |
| Post-test | 6.27±1.05 | 5.23±1.59 | 0.003a | |
| P-value | <0.001c | 0.256c |
Notes: aThe results of the t-text, bThe results of the Mann–Whitney U text, cThe results of the Wilcoxon Signed Rank Test.
In addition, outcomes of each group were compared before and after 8 weeks. The medication literacy, medication self-efficacy and medication adherence in the intervention group were significantly higher than those before the intervention (Table 2). There was also a small improvement in medication self-efficacy in the control group after the intervention. There was no significant change in the medication literacy and adherence of the control group before and after the intervention.
Discussion
Although some cross-sectional studies have shown that patients with higher medication literacy had more standardized medication behavior.20–22 But as far as we know, our study is the first intervention study targeting medication literacy in the glaucoma population. Our study shows that the medication literacy of glaucoma patients is significantly improved after the 8 weeks of G-MedLit intervention.
Our findings also show that the G-MedLit intervention can improve medication self-efficacy in glaucoma. The possible reason for this may be that the improvement of medication literacy level in the intervention group patients has provided them with richer pharmaceutical knowledge and medication skills, making it easier for them to solve the obstacles and difficulties encountered during the medication process, which is conducive to the establishment and strengthening of their medication beliefs and self-confidence. At the same time, we also found that the control group also had an increase in medication self-efficacy after the intervention, which may be related to the increase in the duration of illness in patients.30 However, compared with the control group, the improvement of medication self-efficacy in the intervention group was significantly better than that in the control group.
In addition, our study also found that medication adherence improved significantly in patients in the intervention group after receiving the intervention, which is consistent with the results of other similar studies.23,36 This may be because increasing medication literacy can help patients better understand the importance of drug therapy in delaying their visual impairment, so they have stronger motivation to take medication. On the other hand, richer pharmaceutical knowledge and skills are also beneficial for maintaining standardized medication in the long term.
The advantage of this study is that it fills a gap in interventional research on patients’ medication literacy. The G-MedLit intervention has a scientific theoretical framework. At the same time, the actual needs of glaucoma patients were fully considered in the intervention content. In addition, the intervention methods are more diverse, fully considering the possibility of visual impairment in glaucoma patients, so more video and audio lectures are used instead of traditional written educational materials. This intervention also utilizes mobile medical technology to break through time and space limitations and benefit more glaucoma patients who have already left the medical environment.
Our study has several limitations. First, the study was only conducted in a tertiary hospital, which may have regional limitations and sample representativeness deficiencies. Second, this study only assessed the effect at the end of the intervention and did not validate the long-term effect of the intervention.
Conclusion
Compared with the control group, after the 8 weeks of G-MedLit intervention, the medication literacy, medication self-efficacy and medication adherence of glaucoma patients in the control group were significantly improved. This result demonstrated the effectiveness of this intervention. In the future, we should extend the intervention to a wider group of glaucoma patients, and should be applied in more settings such as wards, communities, families, etc. In conclusion, this study is an important step forward in the study of medication literacy intervention, and will provide reference and guidance for standardizing the medication of glaucoma patients.
Acknowledgments
The authors would like to express their sincere thanks to the experts of this project: Xi Ying, Wei Sun, Lin Li, Xiaolei Wang, Xiaoqin Zhang, Wenmei Guo, Miao Zhen. The MMAS-8 instrument, content, name, and trademarks are protected by US copyright and trademark laws. Permission for use of the scale and its coding is required. A license agreement is available from Donald E. Morisky, Sc.D., M.S.P.H., Sc.M.; philip.morisky@adherence.cc.
Funding Statement
There is no funding to report.
Abbreviations
IMB, Information-Motivation-Behavioral skills Model; HBM, Health Belief Model; CVMLS, Chinese Version of the Medication Literacy Scale; SVGMSEQ, Glaucoma Medication Self-Efficacy Questionnaire; C-MMAS-8, Chinese version of the morisky medication adherence scale-8; ML, Medication literacy; MedLitRxSE, Medication Literacy Assessment in English and Spanish.
Data Sharing Statement
All data generated or analysed during this study are included in this published article.
Consent form, questionnaire form, and record form will be available when requested.
Ethics Statement
The studies involving human participants were reviewed and approved by the academic ethics review boards of the First Affiliated Hospital of Army Medical University (NO. KY202276). The patients/participants provided their written informed consent to participate in this study.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. The person(s) providing consent have been shown the article contents to be published.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Jonas JB, Aung T, Bourne RR. et al. Glaucoma. Lancet. 2017;390(10108):2183–2193. doi: 10.1016/S0140-6736(17)31469-1 [DOI] [PubMed] [Google Scholar]
- 2.Tham YC, Li X, Wong TY, et al. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014;121(11):2081–2090. doi: 10.1016/j.ophtha.2014.05.013 [DOI] [PubMed] [Google Scholar]
- 3.Blumberg D, Skaat A, Liebmann JM. Emerging risk factors for glaucoma onset and progression. Prog Brain Res. 2015;221:81–101. [DOI] [PubMed] [Google Scholar]
- 4.Quigley HA. Glaucoma. Lancet. 2011;377(9774):1367–1377. doi: 10.1016/S0140-6736(10)61423-7 [DOI] [PubMed] [Google Scholar]
- 5.Newman-Casey PA, Salman M, Lee PP, et al. Cost-Utility Analysis of Glaucoma Medication Adherence. Ophthalmology. 2020;127(5):589–598. doi: 10.1016/j.ophtha.2019.09.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Blaschke TF, Osterberg L, Vrijens B, et al. Adherence to medications: insights arising from studies on the unreliable link between prescribed and actual drug dosing histories. Annu Rev Pharmacol Toxicol. 2012;52(1):275–301. doi: 10.1146/annurev-pharmtox-011711-113247 [DOI] [PubMed] [Google Scholar]
- 7.Mansberger SL. Are you compliant with addressing glaucoma adherence? Am J Ophthalmol. 2010;149(1):1–3. doi: 10.1016/j.ajo.2009.08.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gamiochipi-Arjona JE, Azses-Halabe Y, Tolosa-Tort P, et al. Depression and Medical Treatment Adherence in Mexican Patients With Glaucoma. J Glaucoma. 2021;30(3):251–256. doi: 10.1097/IJG.0000000000001739 [DOI] [PubMed] [Google Scholar]
- 9.Newman-Casey PA, Niziol LM, Gillespie BW, et al. The Association between Medication Adherence and Visual Field Progression in the Collaborative Initial Glaucoma Treatment Study. Ophthalmology. 2020;127(4):477–483. doi: 10.1016/j.ophtha.2019.10.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weinreb RN, Aung T, Medeiros FA. The Pathophysiology and Treatment of Glaucoma: a Review. JAMA. 2014;311(18):1901–1911. doi: 10.1001/jama.2014.3192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Newman-Casey PA, Robin AL, Blachley T, et al. The Most Common Barriers to Glaucoma Medication Adherence. Ophthalmology. 2015;122(7):1308–1316. doi: 10.1016/j.ophtha.2015.03.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jang Y, Jee D, Lee D, et al. Medication Adherence and Persistence of Open-Angle Glaucoma Patients in Korea: a Retrospective Study Using National Health Insurance Claims Data. Int J Environ Res Public Health. 2021;18(8):4106. doi: 10.3390/ijerph18084106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Davis SA, Sleath B, Carpenter DM, et al. Drop instillation and glaucoma. Curr Opin Ophthalmol. 2018;29(2):171–177. doi: 10.1097/ICU.0000000000000451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sam-Oyerinde OA, Onyekwelu OM, Musa KO, et al. Assessment of eye drop instillation techniques among patients with primary open angle glaucoma in a Nigerian tertiary hospital. Int Ophthalmol. 2022;42(4):1031–1040. doi: 10.1007/s10792-021-02085-5 [DOI] [PubMed] [Google Scholar]
- 15.Sauceda JA, Loya AM, Sias JJ, et al. Medication literacy in Spanish and English: psychometric evaluation of a new assessment tool. J Am Pharm Assoc. 2012;52(6):e231–e240. doi: 10.1331/JAPhA.2012.11264 [DOI] [PubMed] [Google Scholar]
- 16.Pouliot A, Vaillancourt R, Stacey D, et al. Defining and identifying concepts of medication literacy: an international perspective. Res Social Adm Pharm. 2018;14(9):797–804. doi: 10.1016/j.sapharm.2017.11.005 [DOI] [PubMed] [Google Scholar]
- 17.Zhong Z, Shi S, Duan Y, et al. The Development and Psychometric Assessment of Chinese Medication Literacy Scale for Hypertensive Patients (C-MLSHP). Front Pharmacol. 2020;11:490. doi: 10.3389/fphar.2020.00490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Raynor DKT. Medication Literacy Is a 2-Way Street. Mayo Clin Proc. 2008;83(5):520–522. doi: 10.1016/S0025-6196(11)60721-0 [DOI] [PubMed] [Google Scholar]
- 19.Cordina M, Hämeen-Anttila K, Lauri J, et al. Health and medication literacy and the desire to participate in pharmacotherapy decision making - comparison of two countries. Res Social Adm Pharm. 2018;14(9):817–823. doi: 10.1016/j.sapharm.2018.06.009 [DOI] [PubMed] [Google Scholar]
- 20.Lu M, Ma J, Lin Y, et al. Relationship between patient’s health literacy and adherence to coronary heart disease secondary prevention measures. J Clin Nurs. 2019;28(15–16):2833–2843. doi: 10.1111/jocn.14865 [DOI] [PubMed] [Google Scholar]
- 21.Zheng F, Ding S, Lai L, et al. Relationship Between Medication Literacy and Medication Adherence in Inpatients With Coronary Heart Disease in Changsha, China. Front Pharmacol. 2020;10:1537. doi: 10.3389/fphar.2019.01537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu H, Yao Z, Shi S, et al. The Mediating Effect of Self-Efficacy on the Relationship Between Medication Literacy and Medication Adherence Among Patients with Type 2 Diabetes. Patient Prefer Adherence. 2023;17:1657–1670. doi: 10.2147/PPA.S413385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shen ZY, Ding SQ, Zheng F, et al. Development and implementation of a medication literacy promotion program for patients with hypertension. J Nurs Sci. 2019;34:87–91. [Google Scholar]
- 24.Raynor DK. Addressing medication literacy: a pharmacy practice priority. Int J Pharm Pract. 2009;17(5):257–259. doi: 10.1211/ijpp.17.05.0001 [DOI] [PubMed] [Google Scholar]
- 25.Wu J, Mark B, Knafl GJ, et al. A multi-component, family-focused and literacy-sensitive intervention to improve medication adherence in patients with heart failure–A randomized controlled trial. Heart Lung. 2019;48(6):507–514. doi: 10.1016/j.hrtlng.2019.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fisher JD, Fisher WA, Williams SS, et al. Empirical tests of an information-motivation-behavioral skills model of AIDS-preventive behavior with gay men and heterosexual university students. Health Psychol. 1994;13(3):238–250. doi: 10.1037/0278-6133.13.3.238 [DOI] [PubMed] [Google Scholar]
- 27.Saunders GH, Frederick MT, Silverman S, et al. Application of the health belief model: development of the hearing beliefs questionnaire (HBQ) and its associations with hearing health behaviors. Int J Audiol. 2013;52(8):558–567. doi: 10.3109/14992027.2013.791030 [DOI] [PubMed] [Google Scholar]
- 28.Gentizon J, Hirt J, Jaques C, et al. Instruments assessing medication literacy in adult recipients of care: a systematic review of measurement properties. Int J Nurs Stud. 2021;113:103785. doi: 10.1016/j.ijnurstu.2020.103785 [DOI] [PubMed] [Google Scholar]
- 29.Zheng F, Zhong Z, Ding S, et al. Modification and evaluation of assessment of medication literacy. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2016;41(11):1226–1231. doi: 10.11817/j.issn.1672-7347.2016.11.019 [DOI] [PubMed] [Google Scholar]
- 30.Sleath B, Blalock SJ, Stone JL, et al. Validation of a short version of the glaucoma medication self-efficacy questionnaire. Br J Ophthalmol. 2012;96(2):258–262. doi: 10.1136/bjo.2010.199851 [DOI] [PubMed] [Google Scholar]
- 31.Ge W, Bian W, Zhang X, et al. Sinicization and reliability and validity test of Short Version of the Glaucoma Medication Self-Efficacy Questionnaire. Chin Nurs Res. 2022;36(24):4358–4363. [Google Scholar]
- 32.Akazawa M, Sato T, Ebata N, et al. Factors Related to Treatment Non-Adherence Among Caregivers of Pediatric and Adolescent Growth Hormone Deficiency Patients in Japan. Patient Prefer Adherence. 2024;18:607–622. doi: 10.2147/PPA.S446649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Berlowitz DR, Foy CG, Kazis LE, et al. Effect of Intensive Blood-Pressure Treatment on Patient-Reported Outcomes. N Engl J Med. 2017;377(8):733–744. doi: 10.1056/NEJMoa1611179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bress AP, Bellows BK, King JB, et al. Cost-Effectiveness of Intensive versus Standard Blood-Pressure Control. N Engl J Med. 2017;377(8):745–755. doi: 10.1056/NEJMsa1616035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yan J, You LM, Yang Q, et al. Translation and validation of a C hinese version of the 8-item M orisky medication adherence scale in myocardial infarction patients. Journal of Evaluation in Clinical Practice. 2014;20(4):311–317. doi: 10.1111/jep.12125 [DOI] [PubMed] [Google Scholar]
- 36.Kaup S, Oomman SS, Shivalli S. Determinants of medication adherence to topical ocular hypotensives and application of health belief model among glaucoma patients visiting a tertiary care hospital in coastal Karnataka, India. Indian J Ophthalmol. 2018;66(8):1229–1230. doi: 10.4103/ijo.IJO_80_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analysed during this study are included in this published article.
Consent form, questionnaire form, and record form will be available when requested.