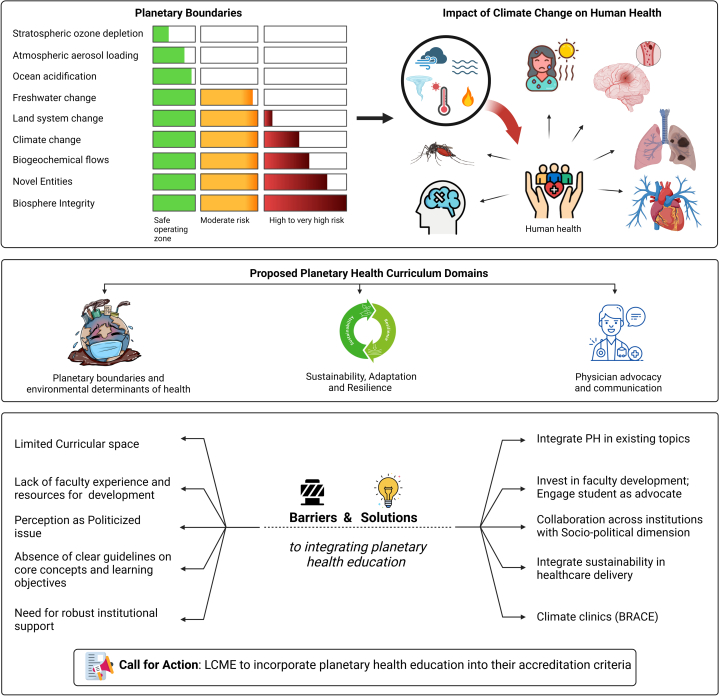
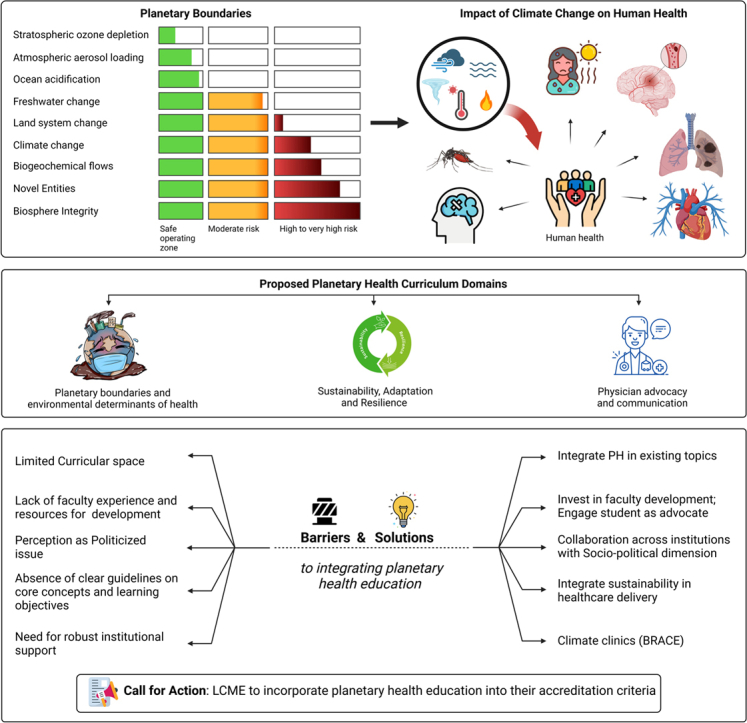
Graphical abstract
Key words: climate change, curriculum integration, medical education, planetary health, sustainability
The World Health Organization estimates that between 2030 and 2050, climate change alone will cause approximately 250,000 additional deaths per year from various causes, with estimated health costs of US$ 2 to 4 billion annually by 2030.1 The planetary boundaries framework identifies nine critical processes essential for maintaining the Earth's ecosystem stability and safe human existence.2 These include climate change, biosphere integrity, land-system change, freshwater use, biogeochemical flows, ocean acidification, atmospheric aerosol loading, stratospheric ozone depletion, and introduction of emerging exposures.2 Alarmingly, an analysis reported in 2023 found that six of these nine boundaries have been transgressed due to human activities, indicating that the planet has moved outside the safe operating zone for humanity in those areas.2 Violating these boundaries increases the risk of large-scale, abrupt, or irreversible environmental changes, which can have severe consequences for human health and well-being.2
With the growing urgency of this crisis, physicians require exposure not just to climate change but a broader perspective on planetary health to adequately care for patients. This shift in the focus from climate to planetary health is also needed to appreciate the interdependence of human wellbeing and planetary health and an integrated understanding of personal wellness with planetary wellbeing.3 This shift is also important as it encourages policies and actions that promote sustainability and resilience.3 Despite the urgency of the climate crisis, medical curricula are ill equipped to promote the interdependence of individual or community health with planetary health, with only 15% of medical schools worldwide including planetary health in their curricula.4 As the world faces increasingly dire consequences of exceeding planetary boundaries, it is crucial that medical education adapts to equip future health care providers with the knowledge and skills necessary to mitigate and manage the resulting health impacts while also promoting sustainable practices within the health care sector.3
A survey of 600 medical students at 12 medical schools in the United States further underscores this interest.5 Hampshire et al5 found that 83.9% of medical student respondents believed climate change and its health effects should be included in the core medical school curriculum. However, only 13.0% felt their school currently provides adequate education on the topic.3 Strikingly, just 6.3% of students felt “very prepared” to discuss how climate change can affect health with a patient. This study highlights a significant gap between student demand and current educational offerings.5 The 2020 to 2021 Liaison Committee on Medical Education (LCME) annual survey of topics included in medical school courses showed that only 54 out of 155 (35%) medical schools had preclerkship offerings that are almost entirely climate-focused.3 Current preclinical and clinical curricula often lack references to the mechanisms through which transgression of planetary boundaries acts as a risk multiplier for human diseases.5 A critical gap in current medical education also exists regarding preparedness for health challenges related to climate change or, more importantly, driven by the transgression of planetary boundaries.
There are currently numerous barriers that preclude careful consideration of topics that would address gaps in understanding of the impact of planetary disruption on human health. These include limited time and space for such topics within already packed medical, nursing, and pharmacy curricula.3 There is a lack of appropriate transdisciplinary expertise that is able to provide training in approaches such as systems dynamics, sustainability, ecological, and environmental science that is able to impart these skills to students.6 Systems thinking courses and tools are currently not required in medical school curricula and should be. A systems framework can also help identify the connections between personal and planetary health and engage multiple stakeholders, including patients, policymakers, and the public, in understanding the environmental impact of health care decisions and developing solutions that are acceptable to all.7 Training medical students in systems dynamics modeling and other modes of simulation, including life cycle analysis, can help engage and facilitate the incorporation of sustainability approaches in value-based health care. Many educators may not have received training on these topics themselves, making it difficult for them to develop and deliver high-quality, evidence-based curricula.6 Additionally, they may lack access to appropriate educational resources, such as assessment tools, case studies, and interactive modules, further compounding the challenge of integrating planetary health into their courses.6 Building upon initiatives by medical schools worldwide, institutions can integrate planetary health education by developing longitudinal curricula that introduce and develop the fundamental connections between biosphere health in preclinical years and reinforce them during clinical training.8 This can be achieved by integrating climate content into existing courses, utilizing case-based learning and clinical scenarios, offering elective courses and specialized tracks, encouraging interprofessional education, providing faculty development, engaging students as advocates, and fostering research and community partnerships.8
Climate change is also a politicized issue with the potential to hinder the largess of some donors.5 Thus the shift in the emphasis on planetary health and emphasis on the intricate connections between the biosphere and societal health can be helpful. Indigenous knowledge and centuries-old traditions from a variety of ancient cultures have largely been overlooked in medical school curricula but represent collective, holistic, community-based, land-informed ways of knowing that are inherently interconnected with people and the environment. In this regard, both the ontology (ie, way of being) and epistemology (ie, way of knowing) of such disciplines emphasize systems thinking, in a direct contrast to the human-centric worldview that continues to permeate modern conceptualizations of health and wellbeing. Currently, although some medical schools offer perspectives through courses in indigenous health, their rich connection with planetary health is not explicit.
A lack of clarity on the core competencies and must-have skills for ensuring understanding of a broad array of topics is a fundamental challenge, especially given the inherent complexities of planetary health frameworks, the evolving nature of the science, and the broad expertise required to understand the intricate connections between the planet and health, much of which continues to evolve. Thus, it can be challenging for educators to determine the appropriate content and depth to include in their curricula.5 This lack of standardization can lead to inconsistent integration across programs and institutions. Finally, appropriate resource allocation for curriculum design, implementation, and appropriate investment in faculty training is warranted. Without financial investment, advocacy, and strong leadership support and commitment to this issue, efforts to infuse climate change throughout education may face an uphill battle.5
A potentially helpful strategy is to incorporate sustainability into established quality improvement (QI) education and institutional value frameworks. Sustainability in QI (SusQI) is a framework that embeds environmental, social, and economic sustainability into QI methodology. It equips learners with practical skills to improve health care holistically, assessing quality and value through a “triple bottom line” of health outcomes weighed against environmental, social, and financial impacts.8 SusQI education can be delivered through interactive workshops, online self-study, or the use of teaching materials that introduce the concept, framework, and technical skills, such as carbon calculation.8 Learners can be tasked with writing project proposals or undertaking sustainable quality improvement projects within their clinical settings.8
To address the urgent need for comprehensive planetary health education in medical training, we propose a curriculum that not only encompasses key aspects of this critical issue but also intends to bridge the gap between student interest and current educational offerings. The proposed curriculum domains (illustrated in Figure 1) are structured to provide a thorough understanding of the interconnections between planetary health and human well-being while also emphasizing practical skills for sustainable health care practices and advocacy. Integration of planetary health should fulfill several criteria in order to be successful. First, it should be comprehensive yet concise, providing essential knowledge without overwhelming students. As medical school curriculums are crowded with mandatory material, prioritizing planetary health over more seemingly pressing topics may be viewed skeptically. Second, the content should be integrated via phases throughout the 4 years of medical school rather than isolated in a single course or module for deeper understanding over time. Third, the curriculum should be practical, emphasizing real-world applications and clinical relevance. Fourth, it should frame health problems through a planetary health lens, helping students understand the broader environmental context of diseases and health outcomes. Finally, successful integration involves transdisciplinary collaboration, connecting planetary health concepts to various medical specialties and basic sciences. This approach ensures that planetary health is not seen as a separate topic but as an integral part of medical education that may inform clinical decision-making, patient care, and public health strategies.
Figure 1.
Overview of Planetary Health, Its Relationship to Human Health, and Barriers and Solutions to Integrating Planetary Health Education Into Medical Curricula
BRACE = Building Resilience Against Climate Effects; LCME = Liaison Committee on Medical Education.
Overcoming barriers: solutions for integrating climate change curriculum in medical education
-
A.
Integrating planetary health into existing topics: Integrating planetary health into existing medical topics like cardiovascular, respiratory, neurological, and infectious diseases curriculum can help overcome the barrier of limited time in a busy schedule. By embedding environmental concepts into traditional medical education, students can simultaneously learn about the impact of planetary health on various medical conditions and the importance of sustainable practices. For instance, understanding how air pollution exacerbates cardiovascular or how climate change affects neurological disorders allows students to grasp the broader context of these diseases without needing additional dedicated courses.9 This integrated approach ensures a comprehensive education while efficiently utilizing the limited time available.
-
B.
Invest in faculty development: Institutions should invest in faculty development programs, such as workshops, courses, and mentorships, to equip educators with the knowledge and skills needed to teach this complex topic confidently. Collaborating with experts in relevant fields can ensure faculty have access to the most current and pertinent information, which can lead to meaningful integration of climate change curriculum.8
-
C.
Sociopolitical dimensions: When incorporating climate change into curricula, educators should emphasize the strong scientific consensus on its reality, causes, and health impacts while also acknowledging the sociopolitical factors that shape public perceptions and policy responses. This balanced approach will help trainees develop a comprehensive understanding of the scientific and social dimensions of climate and health.
-
D.
Collaborate across institutions: To develop a shared set of core competencies and learning objectives for climate health education, professional organizations should collaborate across institutions and disciplines. By convening working groups that include educators, clinicians, researchers, and students, these associations can establish a common framework that ensures consistent training and facilitates the exchange of best practices and resources.
-
E.
Engage students as advocates: Students, as future health care professionals, are often passionate advocates for addressing climate change and its health impacts. Engaging them as partners in curricular reform can provide valuable insights into the knowledge and skills they feel are most essential. Institutions should consider supporting student-led initiatives, such as climate health interest groups, research projects, and community outreach efforts, recognizing the power of student voices in driving educational change.
-
F.
Integrating sustainability in health care delivery: By incorporating eco-friendly practices and emphasizing the interconnectedness of human and environmental health, students can gain a deeper understanding of how sustainable initiatives, such as reducing hospital waste, optimizing energy use, and promoting green spaces, contribute to better patient outcomes and global well-being.6,10 This hands-on experience in sustainable healthcare fosters a holistic approach to medicine, preparing future physicians to address both clinical and environmental determinants of health, ultimately promoting a healthier planet and population.
-
G.
Climate clinics: Building climate clinics that incorporate the Centers for Disease Control and Prevention's BRACE (Building Resilience Against Climate Effects) framework can significantly enhance medical education by providing a practical, structured approach to addressing climate-related health issues.10 These clinics would serve as experiential learning environments where students can see firsthand the impact of climate change on public health and learn to implement adaptive strategies. Through the BRACE framework, students would gain skills in assessing climate vulnerabilities, projecting health impacts, and developing interventions to mitigate these effects.10 This hands-on experience not only enriches their understanding of planetary-human health connections but also equips them with the knowledge and tools to promote resilience in their future medical practice.
We urge the LCME to incorporate planetary health education into their accreditation criteria, recognizing its crucial role in preparing physicians for current and future health care challenges.4 This could be integrated into existing standards related to public health, health disparities, and medical ethics.4 Tying planetary health to accreditation would incentivize medical schools to develop robust curricula, ensuring all students receive this critical training. LCME endorsement would highlight the topic's importance, potentially spurring resource allocation and faculty development. Schools can also learn from existing climate change content, interest groups, and research projects at various institutions.4 By aligning with LCME standards and integrating these strategies, medical schools can create comprehensive climate change education programs, equipping future physicians to address this pressing public health challenge. These efforts will build on prior calls to introduce environmental and climate curricula in graduate medical education programs.
Comprehensive integration of planetary health and sustainability in care delivery concepts throughout medical school curricula is crucial for building a resilient workforce. This workforce would not only understand the interactions between human and planetary health and be equipped to address illnesses related to planetary boundary violations but also actively work to reduce the health care sector’s contributions to environmental harm. By embedding these principles in medical education, future health care professionals will be better prepared to mitigate adverse environmental impacts and promote a sustainable future.
Funding support and author disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Contributor Information
Sadeer Al-Kindi, Email: sal-kindi@houstonmethodist.org.
Sarju Ganatra, Email: Sarju.Ganatra@Lahey.org.
References
- 1.Miller M.R., Landrigan P.J., Arora M., Newby David E., Münzel T., Kovacic Jason C. Environmentally not so friendly: global warming, air pollution, and wildfires. J Am Coll Cardiol. 2024;83(23):2291–2307. doi: 10.1016/j.jacc.2024.03.424. [DOI] [PubMed] [Google Scholar]
- 2.Richardson K., Steffen W., Lucht W., et al. Earth beyond six of nine planetary boundaries. Sci Adv. 2023;9(37) doi: 10.1126/sciadv.adh2458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Khraishah H., Ganatra S., Al-Kindi S.G. Climate change, environmental pollution, and the role of cardiologists of the future. J Am Coll Cardiol. 2023;81(11):1127–1132. doi: 10.1016/j.jacc.2022.10.040. [DOI] [PubMed] [Google Scholar]
- 4.Greenwald L., Blanchard O., Hayden C., Sheffield P. Climate and health education: a critical review at one medical school. Front Public Health. 2022;10 doi: 10.3389/fpubh.2022.1092359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hampshire K., Ndovu A., Bhambhvani H., Iverson N. Perspectives on climate change in medical school curricula—a survey of U.S. medical students. J Climate Change Health. 2021;4 doi: 10.1016/j.joclim.2021.100033. [DOI] [Google Scholar]
- 6.Ganatra S., Dani S.S., Al-Kindi S.G., Rajagopalan S. Health care and climate change: challenges and pathways to sustainable health care. Ann Intern Med. 2022;175(11):1598–1600. doi: 10.7326/m22-1241. [DOI] [PubMed] [Google Scholar]
- 7.Pongsiri M.J., Bassi A.M. A systems understanding underpins actions at the climate and health nexus. Int J Environ Res Public Health. 2021;18(5):2398. doi: 10.3390/ijerph18052398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stanford V., Barna S., Gupta D., Mortimer F. Teaching skills for sustainable health care. Lancet Planet Health. 2023;7(1):e64–e67. doi: 10.1016/S2542-5196(22)00330-8. [DOI] [PubMed] [Google Scholar]
- 9.Khadke S., Kumar A., Al-Kindi S., et al. Association of environmental injustice and cardiovascular diseases and risk factors in the United States. J Am Heart Assoc. 2024;13(7) doi: 10.1161/JAHA.123.033428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lemon S.C., Joseph H.A., Williams S., et al. Reimagining the role of health departments and their partners in addressing climate change: revising the building resilience against climate effects (BRACE) framework. Int J Environ Res Public Health. 2023;20(15):6447. doi: 10.3390/ijerph20156447. [DOI] [PMC free article] [PubMed] [Google Scholar]