Abstract
Background and Objective
Durvalumab plus tremelimumab (Durva/Treme) has recently been approved as a first-line or later-line treatment for patients with unresectable hepatocellular carcinoma (u-HCC) in Japan. We assessed the real-world outcomes of Durva/Treme for u-HCC, with a focus on treatment efficacy and safety.
Methods
We retrospectively evaluated 22 patients with u-HCC treated with Durva/Treme at Iwate Medical University during the period from 2023 to 2024, with a comparison of the clinical outcomes between patients who received Durva/Treme as first-line and later-line treatments. We further evaluated changes in the modified albumin-bilirubin (mALBI) grade during treatment.
Results
There were 10 patients in the first-line group and 12 patients in the later-line treatment group. During the follow-up with a median duration of 7.6 months, the median progression-free survival (first-line versus later-line: 4.7 months versus 2.9 months, p = 0.85), the objective response rate (0.0% versus 16.7%, p = 0.48), the disease control rate (60.0% versus 58.4%, p = 1.00), and the incidence of any adverse event (50.0% versus 75.0%, p = 0.38) were not statistically different between the two groups. The changes in the mALBI scores were not statistically significant (p = 0.75).
Conclusions
Durva/Treme may be effective and safe for patients with u-HCC, even in patients who receive Durva/Treme as a later-line treatment.
Key Points
| Durvalumab plus tremelimumab may be effective and safe for unresectable hepatocellular carcinoma, even in patients who receive it as a later-line treatment. |
| Hepatic functional reserve is well preserved in the early stages of durvalumab plus tremelimumab treatment. |
Introduction
Hepatocellular carcinoma (HCC) is responsible for a significant number of cancer-related deaths and is the sixth most common type of cancer worldwide [1]. In the past, transcatheter arterial chemoembolization (TACE) was recommended for patients with unresectable HCC (u-HCC), which is compatible with Barcelona Clinic Liver Cancer (BCLC)-B, at the time of the diagnosis [2, 3]. Sorafenib [4], a molecularly targeted agent (MTA), was approved in Japan as the first-line treatment for u-HCC in 2009, and it was used in combination with TACE during the subsequent 9 years. With the introduction of regorafenib in 2017 [5], the number of approved MTAs has recently been increasing with rapid expansions in the treatment options. Furthermore, in 2020, the combination of atezolizumab, an immune checkpoint inhibitor (ICI), and bevacizumab, an anti-angiogenesis inhibitor, became the first-line systemic therapy on the basis of IMbrave150 trial [6], showing significant increases in overall survival (OS) and progression-free survival (PFS) in comparison with sorafenib therapy.
In 2022, the HIMALAYA trial [7] showed that the combination of durvalumab, an anti-programmed cell death ligand 1 (PD-L1) inhibitor, and tremelimumab, an anti-cytotoxic T lymphocyte-associated protein 4 (CTLA-4) inhibitor, significantly increased OS in comparison with sorafenib. The combination therapy (Durva/Treme) has been shown to have an additive antitumor activity, which is associated with complementary immunostimulatory effects [8, 9]. Currently, the guidelines of American Society of Clinical Oncology and European Society for Medical Oncology list Durva/Treme as the first-line therapy for patients with gastrointestinal bleeding and esophageal bleeding, as well as the second-line or later-line treatment option [10, 11]. However, the HIMALAYA trial excluded patients who had been treated by MTAs or ICIs.
In the present study, we assessed the treatment results and safety profiles of Durva/Treme in patients, including those who had been treated with MTAs or ICIs, together with an analysis of changes in the modified albumin–bilirubin (mALBI) grade during treatment [12], which was not evaluated in the HIMALAYA trial.
Materials and Methods
Patients
This study retrospectively evaluated patients who were treated with Durva/Treme for u-HCC at Iwate Medical University between April and December 2023, and who were followed until March 2024. The inclusion criteria were as follows; (1) ability to provide informed consent; (2) u-HCC diagnosed by dynamic computed tomography (CT) [13], magnetic resonance imaging (MRI) [14, 15], and increasing course of alpha-fetoprotein (AFP) and/or pathological findings; (3) age > 18 years, (4) BCLC stages B or C [16], (5) Child–Pugh score of 5, 6, or 7, (6) Eastern Cooperative Oncology Group (ECOG) performance status score of 0 or 1, and (7) undergoing upper gastrointestinal endoscopy for the evaluation of gastroesophageal varices before treatment. The exclusion criteria were (1) cases in which data were not collected accurately, (2) cases that were followed for less than a month, and (3) having an autoimmune disease or interstitial pneumonia. Patients treated with Durva/Treme were classified into two groups on the basis of the line of treatment: the first-line group and the later-line group.
This study was approved by our institution’s local Ethics Committee (approval no.: MH2022-145). The patients provided their written informed consent prior to treatment, in accordance with the ethical standards of the 2013 Declaration of Helsinki and its subsequent amendments.
Hepatic Functional Reserve
The Child–Pugh classification [17] and mALBI grade [12] were used to evaluate the liver function. mALBI was calculated on the basis of serum albumin and total bilirubin values according to the following formula; mALBI score = (log10 bilirubin (µmol/L) × 0.66) + (albumin (g/L) × − 0.085) [18]. The score was classified into the following four grades; mALBI score ≤ − 2.6 (grade 1), between − 2.60 and − 2.27 (grade 2a), between − 2.27 and − 1.39 (grade 2b), and > − 1.39 (grade 3). The mALBI and Child–Pugh scores were calculated at the time when Durva/Treme was started, and then at weeks 2, 4, 6, and 8.
Treatment Protocol and Assessment of the Therapeutic Response
The Durva/Treme protocol consisted of tremelimumab (300 mg, 1 dose) plus durvalumab (1500 mg, every 4 weeks) according to the manufacturer’s guidelines [7]. Treatment induction was conducted on an inpatient basis, with the patient discharged on the third day after induction, and then followed weekly as outpatient for 4 weeks, and every 2 weeks thereafter. The initial therapeutic response was assessed using dynamic CT results at approximately 8 weeks after the introduction. Subsequently, dynamic CT examinations were added as needed, according to the patient’s condition.
The therapeutic response was evaluated by three senior hepatologists at our institutions (H. K., T. A., and T. O.) in accordance with Response Evaluation Criteria in Solid Tumors (RECIST) ver. 1.1 [19] and modified RECIST (mRECIST) [20]. The objective response rate (ORR) was defined as the proportion of patients with a complete response (CR) or partial response (PR). The disease control rate (DCR) was defined as the proportion of patients with CR, PR, or stable disease (SD).
Assessments of Adverse Events
The National Cancer Institute Common Terminology Criteria for Adverse Events (version 5.0) [21] were applied for the assessment of adverse events. Administration was discontinued in cases of unacceptable adverse events (AEs), serious AEs, or clinical progression of the tumor.
Statistical Analysis
Continuous variables are described as the median and interquartile range (IQR). Categorical variables are described as percentages. Continuous variables were compared using the Mann–Whitney U test, and categorical variables were compared using Fisher’s exact test. OS and PFS were estimated using Kaplan–Meier curves. To identify factors associated with OS and PFS, a multivariate analysis was performed using a Cox proportional hazards model for variables with p-values of < 0.10 in a univariate analysis. The results were reported as hazard ratios (HRs) with 95% confidence intervals (CIs). A mixed-effects regression model with random intercepts was used to test for differences in the rate of change in the mALBI score and Child–Pugh score at baseline and at weeks 2, 4, 6, and 8. The model included a random intercept for each patient and fixed effect over time. A global test was conducted to evaluate the overall significance of the time effect. This test assesses whether the coefficients for the timepoints are homogeneous. p-values were two-tailed, and p-values < 0.05 were considered statistically significant.
All statistical analyses were performed using EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan) for R (The R Foundation for Statistical Computing, Vienna, Austria), which is a modified version of the R commander designed to add statistical functions frequently used in biostatistics [22].
Results
Patient Characteristics
In total, 22 patients with u-HCC were the subjects of this study. Patient characteristics are summarized in Table 1. The median age was 75.9 years and 19 patients (86.4%) were male. Durva/Treme was administered as the first-line therapy in 10 patients (45%) and as the second-line or later-line therapy in 12 patients. Child–Pugh class was A in 18 patients (82%) and ALBI grade was 1 observed in 10 patients (46%). A total of 11 patients (50%) had BCLC Stage C disease. The median tumor size was 6.9 cm and the size exceeded the up-to-seven criteria in all patients. A total of 6 patients (27%) had macrovascular invasion and 11 (50%) had extrahepatic spread.
Table 1.
Characteristics of patients
| Variable | Overall patients (n = 22) | First-line patients (n = 10) | Later-line patients (n = 12) | p-value | |||
|---|---|---|---|---|---|---|---|
| Age, years | 75.6 | (68.0–88.0) | 75.6 | (70.6–80.5) | 76.1 | (70.0–80.1) | 0.84 |
| Male | 19 | (86) | 8 | (80) | 11 | (92) | 0.57 |
| Etiology, viral hepatitis | 13 | (59) | 7 | (70) | 6 | (50) | 0.41 |
| ECOG PS 0 | 20 | (90) | 9 | (90) | 11 | (92) | 1.00 |
| Prior treatment, Atez/Bev | 6 | (27) | 0 | (0) | 6 | (50) | |
| Treatment line 1st/2nd/3rd/4th/5th | 10/7/4/0/1 | ||||||
| Child–Pugh class A | 20 | (90) | 9 | (90) | 11 | (92) | 1.00 |
| mALBI score | − 2.43 | (− 2.66 ~ − 2.12) | −2.53 | (− 2.74 ~ − 2.14) | − 2.41 | (− 2.61 ~ − 2.15) | 0.95 |
| Grade 1/2a/2b | 10/5/7 | 5/1/4 | 3/5/4 | ||||
| BCLC stage C | 11 | (50) | 5 | (50) | 6 | (50) | 1.00 |
| AST, U/L | 33 | (25–42) | 29 | (23–40) | 39 | (29–43) | 0.28 |
| ALT, U/L | 25 | (21–41) | 24 | (19–34) | 29 | (23–43) | 0.53 |
| Albumin, g/dL | 3.6 | (3.3–3.9) | 3.7 | (3.2–4.1) | 3.6 | (3.5–3.8) | 0.97 |
| Total bilirubin, mg/dL | 0.6 | (0.4–0.8) | 0.6 | (0.5–0.8) | 0.6 | (0.4–0.8) | 0.97 |
| Prothrombin time, % | 89 | (60–75) | 86 | (53–101) | 75 | (37–108) | 0.72 |
| AFP, ng/mL | 36.8 | (6.2–2655.0) | 22.1 | (5.6–2025.0) | 66.7 | (8.7–5627.5) | 0.43 |
| DCP, mAU/mL | 499 | (120–2849) | 624 | (55.0–2849.0) | 566 | (273.8–2015.5) | 0.78 |
| Tumor size, cm | 6.9 | (3.5–8.6) | 7.6 | (5.8–13.1) | 7.4 | (6.0–9.7) | 0.57 |
| Tumor number, multiple | 20 | (91) | 10 | (100) | 10 | (83.3) | 0.48 |
| Macrovascular invasion | 9 | (40) | 5 | (50.0) | 4 | (33.3) | 0.66 |
| Extrahepatic spread | 11 | (50) | 6 | (60) | 7 | (58) | 1.00 |
| Observation period, months | 7.6 | (4.9–9.5) | 7.6 | (6.5–8.8) | 8.1 | (4.7–9.1) | 0.97 |
Data are presented as the median (interquartile range) or n (%).
AFP alpha-fetoprotein, mALBI modified albumin–bilirubin, ALT alanine aminotransferase, AST aspartate aminotransferase, Atez/Bev atezolizumab plus bevacizumab, BCLC Barcelona Clinic Liver Cancer, ECOG PS Eastern Cooperative Oncology Group performance status, DCP des-γ-carboxy prothrombin
On the basis of the background data, 10 patients (45%) were assigned to the first-line group and 12 patients (55%) were assigned to the later-line group. As presented in Table 1, no other items differed between the two groups.
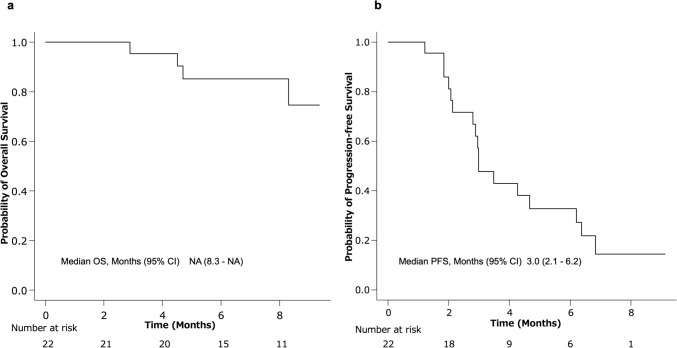
Therapeutic Efficacy of Durvalumab Plus Tremelimumab
During the observation period, 5 patients continued Durva/Treme, while 17 patients discontinued because of progressive disease (PD) in 12 patients and AEs in 4 patients. In total, three patients died of progressive HCC. The 95% confidence interval (95% CI) for OS in the patients could not be calculated due to small sample size (Fig. 1a). The 95% CI for PFS ranged from 2.1 to 6.2 months with a median of 3.0 months (Fig. 1b).
Fig. 1.
Kaplan–Meier curves for OS and PFS in the overall population of patients treated with durvalumab plus tremelimumab. a OS did not reach the median; b the median PFS was 3.0 months (95% CI 2.1–6.2). NA not applicable, OS overall survival, PFS progression-free survival, 95% CIs 95% confidence intervals
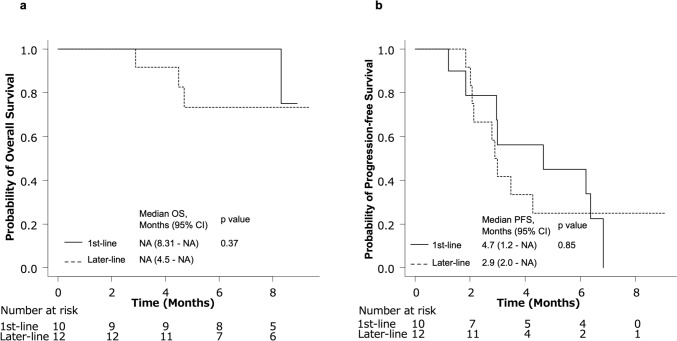
The median PFS of the first-line and later-line groups did not differ to a statistically significant extent (4.7 months and 2.9 months, respectively; p = 0.85) (Fig. 2b). The initial assessment of the therapeutic response at 8 weeks is presented in Table 2. The therapeutic response determined by RECIST ver. 1.1, was CR (n = 0; 0%), PR (n = 2; 9.1%), SD (n = 11; 50%), and PD (n = 9; 40.9%). Thus, the ORR was 9.1% and DCR was 59.1%. The response determined by mRECIST was CR (n = 0; 0%), PR (n = 2; 9.1%), SD (n = 13; 59.1%), and PD (n = 7; 31.8%), with the ORR of 9.1%, and DCR of 68.2%.
Fig. 2.
Kaplan–Meier curves for OS and PFS in the HIMALAYA-in and HIMALAYA-out groups. a OS did not reach the median; b the median PFS was 4.7 months (95% CI 1.2–6.4) in the HIMALAYA-in group; and 2.9 months (95% CI 2.0–6.8) in the HIMALAYA-out group. The difference was not statistically significant (p = 0.97). NA not applicable, OS overall survival, PFS progression-free survival, 95% CIs 95% confidence intervals
Table 2.
Initial assessment of the therapeutic response with RECIST ver. 1.1 and modified RECIST at 8 weeks
| RECIST ver. 1.1 | mRECIST | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall patients (n = 22) | First-line patients (n = 10) | Later-line patients (n = 12) | p-value | Overall patients (n = 22) | First-line patients (n = 10) | Later-line patients (n = 12) | p-value | |||||||
| CR | 0 | (0.0) | 0 | (0.0) | 0 | (0.0) | 0 | (0.0) | 0 | (0.0) | 0 | (0.0) | ||
| PR | 2 | (9.1) | 0 | (0.0) | 2 | (16.7) | 2 | (9.1) | 0 | (0.0) | 2 | (16.7) | ||
| SD | 11 | (50.0) | 6 | (60.0) | 5 | (41.7) | 13 | (59.1) | 7 | (70.0) | 6 | (50.0) | ||
| PD | 9 | (40.9) | 4 | (40.0) | 5 | (41.7) | 7 | (31.8) | 3 | (30.0) | 4 | (33.3) | ||
| ORR | 9.1% | 0.0% | 16.7% | 0.48 | 9.1% | 0.0% | 16.7% | 0.48 | ||||||
| DCR | 59.1% | 60.0% | 58.4% | 1.00 | 68.2% | 62.5% | 66.7% | 1.00 | ||||||
Data are presented as n (%).
CR complete response, DCR disease control rate, mRECIST modified RECIST, NE, ORR objective response rate, PD progressive disease, PR partial response, RECIST Response Evaluation Criteria in Solid Tumors, SD stable disease
The ORRs under RECIST ver. 1.1 and mRECIST were 0.0% in the first-line group and 16.7% in the later-line group (p = 0.48 and 0.48). The DCRs under RECIST ver. 1.1 and mRECIST were 60.0% and 58.4% (p = 1.00), respectively, in the first-line group and 62.5% and 66.7%, respectively, in the later-line group (p = 1.00). The ORRs and DCRs did not differ between the two groups.
Treatment After Durvalumab Plus Tremelimumab
In total, 14 (82%) of 17 patients who discontinued Durva/Treme were treated by further anticancer therapy. Lenvatinib was applied to seven patients, atezolizumab plus bevacizumab (Atz/Bev) to five patients, and cabozantinib and hepatic arterial infusion chemotherapy each to one patient; four patients who discontinued Durva/Treme due to AEs were eligible for post-treatment. The rates of conversion to post-treatment were 100% in the first-line group and 83% in the later-line group.
Adverse Events
A total of 25 AEs occurred in 14 (63.6%) patients. AEs of grade 3 or more occurred in four (18.2%) patients. A total of six (27.3%) patients discontinued Durva/Treme because of treatment-related AEs. None of the patients died of treatment-related AEs. The frequencies of overall AEs and AEs in the two groups are presented in Table 3. Infusion reactions (27.3%) were the most frequently observed, followed by fatigue (22.7%), diarrhea or colitis (18.2%), decreased appetite (13.6%), pruritus or rash (13.6%), and increase in AST or ALT level (9.1%); two patients with grade ≥ 3 colitis required steroid therapy with prednisolone at a dose of ≥ 0.5 mg/kg. The incidence of AEs in the first-line and later-line groups did not differ to a statistically significant extent.
Table 3.
Any grade and grade 3 or 4 treatment-related adverse events at our institution
| Any grade | Grade 3/4 | |||||||
|---|---|---|---|---|---|---|---|---|
| Overall patients (n = 22) | First-line patients (n = 10) | Later-line patients (n = 12) | p-value | Overall patients (n = 22) | First-line patients (n = 10) | Later-line patients (n = 12) | p-value | |
| Any cause | 14 (63.6) | 5 (50.0) | 9 (75.0) | 0.38 | 4 (18.2) | 3 (33.3) | 1 (8.3) | 0.27 |
| Infusion reaction | 6 (27.3) | 2 (20.0) | 4 (33.3) | 0.65 | 0 (0.0) | 0 (0.0) | 0 (0.0) | NA |
| Fatigue | 5 (22.7) | 0 (0.0) | 5 (41.6) | 0.06 | 0 (0.0) | 0 (0.0) | 0 (0.0) | NA |
| Diarrhea/colitis | 4 (18.2) | 3 (30.0) | 0 (0.0) | 0.13 | 2 (9.1)a | 2 (20.0)a | 0 (0.0) | 0.08 |
| Decreased appetite | 3 (13.6) | 1 (10.0) | 2 (16.6) | 1.00 | 1 (4.5) | 0 (0.0) | 1 (8.3) | 1.00 |
| Pruritus/rash | 3 (13.6) | 0 (0.0) | 3 (25.0) | 0.22 | 0 (0.0) | 0 (0.0) | 0 (0.0) | NA |
| AST, ALT increased | 2 (9.1) | 1 (10.0) | 1 (8.3) | 1.00 | 0 (0.0) | 0 (0.0) | 0 (0.0) | NA |
| Adrenal insufficiency | 1 (4.5) | 1 (10.0) | 0 (0.0) | 0.46 | 1 (4.5) | 1 (0.0) | 0 (0.0) | 0.46 |
| Hypothyroidism | 1 (4.5) | 1 (10.0) | 0 (0.0) | 0.46 | 0 (0.0) | 0 (0.0) | 0 (0.0) | NA |
ALT alanine aminotransferase, AST aspartate aminotransferase, NA not applicable
aSteroid use > 0.5 mg/kg of prednisolone
Contributing factors associated with overall survival and progression-free survival
In the multivariable analysis, viral hepatitis [hazard ratio (HR) 0.01; 95% confidence interval (CI) 0.00–040] was found to be a favorable factor for OS. Meanwhile, prior treatment with Atz/Bev (HR 27.48; 95% CI 1.92–391.50) and des-γ-carboxy prothrombin (HR 24.97; 95% CI 1.69–132.40) were found to be poor factors for OS (Table 4). The only poor factor for PFS was prior treatment with Atz/Bev (HR 6.25; 95% CI 1.16–33.71) (Table 5).
Table 4.
Multivariable Cox regression analysis for overall survival
| Univariable analysis | Multivariable analysis | |||||
|---|---|---|---|---|---|---|
| Hazard ratio | (95% CI) | p-value | Hazard ratio | (95% CI) | p-value | |
| Age ≥ 75, median | 0.14 | (0.03–0.73) | 0.02* | 0.07 | (0.01–1.01) | 0.05 |
| Male | 6.90 | (0.00–inf) | 0.99 | |||
| Etiology (non-viral versus viral hepatitis) | 0.18 | (0.03–0.99) | 0.05* | 0.01 | (0.00–0.40) | 0.02** |
| Prior treatment (others versus Atez/Bev) | 3.31 | (0.94–11.61) | 0.06* | 27.38 | (1.92–391.50) | 0.01** |
| First-line versus later-line | 2.54 | (0.65–9.95) | 0.18 | |||
| Child–Pugh grade (A versus B) | 0.53 | (0.06–4.39) | 0.56 | |||
| mALBI grade (1, 2a versus 2b, 3) | 0.47 | (0.09–2.37) | 0.36 | |||
| BCLC stage (B versus C) | 0.74 | (0.19–2.84) | 0.66 | |||
| AST, U/L | 1.02 | (0.99–1.05) | 0.12 | |||
| ALT, U/L | 1.01 | (0.99–1.02) | 0.48 | |||
| Albumin, g/dL | 1.16 | (0.20–6.87) | 0.87 | |||
| Total bilirubin, mg/dL | 4.46 | (0.78–25.54) | 0.09* | 0.28 | (0.01–6.39) | 0.42 |
| Prothrombin time, % | 0.98 | (0.95–1.02) | 0.28 | |||
| AFP (< 200 versus ≥ 200) | 1.25 | (0.35–4.49) | 0.73 | |||
| DCP (< 400 versus ≥ 400) | 4.42 | (0.94–20.89) | 0.06* | 14.97 | (1.69–132.40) | 0.01** |
| Tumor size, cm | 1.01 | (0.88–1.15) | 0.94 | |||
| Macrovascular invasion | 1.77 | (0.49–6.43) | 0.39 | |||
| Extrahepatic spread | 0.60 | (0.15–2.41) | 0.47 | |||
| Adverse events | 0.79 | (0.21–3.10) | 0.74 | |||
AFP alpha-fetoprotein, mALBI modified albumin–bilirubin, ALT alanine aminotransferase, AST aspartate aminotransferase, Atez/Bev atezolizumab plus bevacizumab, BCLC Barcelona Clinic Liver Cancer, CI confidence interval, ECOG PS Eastern Cooperative Oncology Group performance status, DCP des-γ-carboxy prothrombin, inf infinity
*Significant factors assessed by univariate analysis with p-values < 0.10. **Significant factor assessed by multivariate analyses with p-values < 0.05
Table 5.
Multivariable Cox regression analysis for progression-free survival
| Univariable analysis | Multivariable analysis | |||||
|---|---|---|---|---|---|---|
| Hazard ratio | (95% CI) | p-value | Hazard ratio | (95% CI) | p-value | |
| Age ≥ 75, median | 0.88 | (0.35–2.24) | 0.79 | |||
| Male | 1.98 | (0.45–8.65) | 0.37 | |||
| Etiology (non-viral versus viral hepatitis) | 1.18 | (0.45–3.04) | 0.74 | |||
| Prior treatment (others versus Atez/Bev) | 4.65 | (1.35–16.06) | 0.01* | 6.25 | (1.16–33.71) | 0.03** |
| First-line versus later-line | 1.63 | (0.63–4.20) | 0.32 | |||
| Child–Pugh grade (A versus B) | 8.54 | (1.54–47.21) | 0.01* | 4.12 | (0.19–90.57) | 0.37 |
| mALBI grade (1, 2a versus 2b, 3) | 1.05 | (0.39–2.80 | 0.93 | |||
| BCLC stage (B versus C) | 1.69 | (0.66–4.33) | 0.28 | |||
| AST, U/L | 1.04 | (1.01–1.07) | 0.01* | 0.97 | (0.90–1.05) | 0.50 |
| ALT, U/L | 1.02 | (1.01–1.04) | 0.01* | 1.03 | (1.00–1.07) | 0.05 |
| Albumin, g/dL | 0.95 | (0.32–2.83) | 0.93 | |||
| Total bilirubin, mg/dL | 2.13 | (0.53–8.554) | 0.28 | |||
| Prothrombin time, % | 1.00 | (0.97–1.02) | 0.77 | |||
| AFP (< 200 versus ≥ 200) | 1.59 | (0.62–4.07) | 0.34 | |||
| DCP (< 400 versus ≥ 400) | 1.83 | (0.71–4.76) | 0.21 | |||
| Tumor size, cm | 1.00 | (0.90–1.11) | 0.97 | |||
| Macrovascular invasion | 2.00 | (0.79–5.06) | 0.14 | |||
| Extrahepatic spread | 1.43 | (0.55–3.73) | 0.46 | |||
| Adverse events | 1.52 | (0.54–4.31) | 0.43 | |||
AFP alpha-fetoprotein, mALBI modified albumin–bilirubin, ALT alanine aminotransferase, AST aspartate aminotransferase, Atez/Bev atezolizumab plus bevacizumab, BCLC Barcelona Clinic Liver Cancer, CI confidence interval, ECOG PS Eastern Cooperative Oncology Group performance status, DCP des-γ-carboxy prothrombin
*Significant factors assessed by univariate analysis with p-values < 0.10. **Significant factor assessed by multivariate analyses with p-values < 0.05
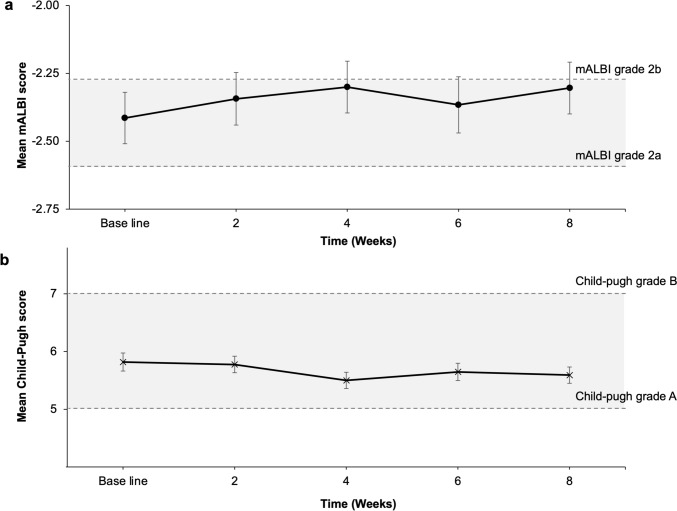
Effect of Durvalumab Plus Tremelimumab Treatment on the Hepatic Functional Reserve
The mean (standard error) scores for mALBI and Child–Pugh are indicated in Fig. 3. The mean mALBI score was maintained at mALBI grade 2a from baseline to 8 weeks (Fig. 3a). Similarly, the mean Child–Pugh score was maintained at Child-grade A (Fig. 3b). Overall, the results indicated that changes in mALBI and Child–Pugh scores over time were not statistically significant (mALBI score: p = 0.75, Child–Pugh score: p = 0.15). The fixed effect at each timepoint did not show significant deviation from the baseline in either mALBI or the Child–Pugh score.
Fig. 3.
The mean mALBI and Child–Pugh scores during the 8-week assessment period. a No effect on mALBI score change over time was observed at up to 8 weeks after the initiation of durvalumab plus tremelimumab (p = 0.75); b no effect on the Child–Pugh score change was observed at up to 8 weeks after the initiation of durvalumab plus tremelimumab (p = 0.15). Bars indicate standard error. Dotted lines indicate cutoff values for mALBI grades 2a and 2b, Child–Pugh grades A and B. ALBI albumin–bilirubin
Discussion
This is the first report to evaluate the efficacy and safety of Durva/Treme and to compare first-line and later-line treatment in patients with u-HCC in a real-world setting. In the present study, the PFS was 3.0 months, the value of which was similar to the PFS (3.8 months) in the clinical trial [7]. The ORRs, assessed according to RECIST ver. 1.1, were 9.1%, the former of which was lower than that in the clinical trial (20.1%) [7]. The low ORR found in our study may be explained by the small sample size, because only two patients showed a PR in this study. Comparing the first-line and later-line groups, we found no significant difference in the OS, PFS, ORR, and DCR between the two groups. In the multivariate analysis of OS and PFS, later-line therapy was not a poor prognostic factor. These observations suggest that the efficacy of Durva/Treme on u-HCC may not be associated with the preceding first- or later-line therapy. In contrast, patients who received Atz/Bev in the previous treatment were found to have poor OS and PFS (Tables 4 and 5). Resistance to ICIs is mainly caused by alterations in the tumor microenvironment (TME), which in turn supports angiogenesis and blocks immune cell antitumor activities, facilitating tumor cell evasion from host immunosurveillance [23]. Therefore, it is possible that durvalumab, an anti-PDL1 antibody similar to atezolizumab, functioned as an ICI, and that discontinuation of bevacizumab further promoted angiogenesis, resulting in tumor progression. Meanwhile, the combination of MTAs and ICIs has been reported to alter the TME and enhance antitumor effects relative to MTAs or ICIs alone [24]. Therefore, it may be better to consider introducing MTAs rather than changing them from Atz/Bev to Dur/Treme. Since our study is a small one, this hypothesis awaits further elucidation.
In anticancer therapy for HCC, the chance for the second- or later-line therapy can lead to improved survival rates [25]. In this study, 82% of the overall patients and all patients who experienced AEs during Durva/Treme therapy could be transferred to later-line therapy. However, the study could not confirm the prognostic value of later-line therapy following Durva/Treme. A combination of anti-PD-L1/PD-1 and anti-CTLA-4 has been reported to result in sustained priming of the immune response through anti-CTLA-4-induced proliferation of CD4+/Ki67+ and CD8+/Ki67+ T cells, which may promote long-term survival [26]. In addition, there have been clinical evidence indicating MTAs to induce the expression of PD-L1 in tumors [27, 28]. It thus seems necessary to re-evaluate the synergistic effects of Durva/Treme with other anti-PD-L1/PD-1 agents and the efficacy of Durva/Treme after MTAs.
Treatment-related AEs occurred in 63.6% of our patients. The incidence is slightly lower than that reported in clinical trials (75.8%) [7]. Furthermore, the incidence of grade 3 or 4 AEs (18.1%) was lower than in clinical trials (25.8%) [7]. The incidence of AEs was similar in the first-line group and later-line groups, even though patients in the late treatment group could tolerate treatment. The most frequent AE was infusion reactions (27.3%), followed by fatigue (22.7%) and diarrhea/colitis (18.2%). Notably, 50% of the patients with diarrhea/colitis were found to have immune-related colitis, which required prednisolone at dose of ≥ 0.5 mg/kg/day. Because colonoscopy with biopsy is essential for the diagnosis of immune-related colitis [29, 30], early and prompt interventions should be seriously considered in cases suspected of having the condition.
It has been reported that MTAs, such as sorafenib and lenvatinib, are the source of liver dysfunction [31, 32]. In contrast, in CheckMate 459, nivolumab, an ICI, was shown to be superior to sorafenib in preserving the liver function, as determined by ALBI and Child–Pugh scores [33]. It has also been shown that liver function is maintained during Atz/Bev [34, 35]. In HIMALAYA trial, however, temporal changes in hepatic function residue were not evaluated. We found that mALBI and Child–Pugh scores remained stable during the initial treatment course for 8 weeks in our patients. This observation seems to suggest that in the early stages Durva/Treme treatment, can be safely conducted, while long-term effect remains to be elucidated.
The present study was associated with several limitations. First, this was a single-center, hospital-based study with a small number of patients and short observation period. Thus, we could not assess OS. Second, we could not demonstrate the efficacy of the second- or later-line therapy following Durva/Treme. In particular, the optimal sequence of ICIs and MTAs together with the efficacy of -anti-CTLA-4 therapy after Durva/Treme needs to be examined further.
Conclusions
We showed the efficacy of Durva/Treme with an emphasis on the lack of a significant difference between the first-line and later-line groups. We were also able to show that hepatic functional reserve is well preserved in the early stages of the treatment. Taken together, we presume that Durva/Treme is a candidate as a universal therapeutic strategy and it is a potentially promising treatment option for patients with u-HCC. Further larger trials with long-term observation are needed to validate the speculation.
Acknowledgments
We would like to thank the Japan Medical Communication for editing the English language of this paper.
Declarations
Funding and conflict of interest
The authors declare no conflicts of interest or financial support associated with this study.
Ethics approval
This study was approved by local ethics committee of Iwate Medical University (approval no.: MH2022-145, approval date: 25 April 2023). The patients provided their written informed consent prior to treatment, in accordance with the ethical standards of the 2013 Declaration of Helsinki and its subsequent amendments.
Consent to participate
All participants provided written informed consent before participation.
Consent for publication
Not applicable.
Code availability
Not applicable.
Availability of data and material
The data presented in this study are available upon request from the corresponding author.
Author contributions
Y.F. designed the study and wrote the manuscript; H.K., K.K., and T.M. corrected the manuscript; Y.F. and T.A. created the database system; T.A., T.N., I.N., A.I., T.W., K.Y., H.S., A.S., K.E., Y.Y., T.O., K.K., K.S., and A.M. treated the patients; and H.K. and T.M. supervised the study. All authors discussed the results and contributed to the final manuscript. All the authors have read and agreed to the published version of the manuscript.
References
- 1.Bray F, Laversanne M, Sung H, Ferlay J, Siegel RL, Soerjomataram I, et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2024;74:229–63. [DOI] [PubMed] [Google Scholar]
- 2.Liver EAFTSOT, Cancer EOFRATO. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2012;56:908–43. [DOI] [PubMed] [Google Scholar]
- 3.Llovet JM, Bru C, Bruix J. Prognosis of hepatocellular carcinoma: the BCLC staging classification. Semin Liver Dis. 1999;19:329–38. [DOI] [PubMed] [Google Scholar]
- 4.Llovet JM, Ricci S, Mazzaferro V, Hilgard P, Gane E, Blanc JF, et al. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med. 2008;359:378–90. [DOI] [PubMed] [Google Scholar]
- 5.Bruix J, Qin S, Merle P, Granito A, Huang YH, Bodoky G, et al. Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2017;389:56–66. [DOI] [PubMed] [Google Scholar]
- 6.Finn RS, Qin S, Ikeda M, Galle PR, Ducreux M, Kim TY, et al. Atezolizumab plus bevacizumab in unresectable hepatocellular carcinoma. N Engl J Med. 2020;382:1894–905. [DOI] [PubMed] [Google Scholar]
- 7.Abou-Alfa GK, Lau G, Kudo M, Chan SL, Kelley RK, Furuse J, et al. Tremelimumab plus durvalumab in unresectable hepatocellular carcinoma. NEJM Evid. 2022;1:EVIDoa2100070. [DOI] [PubMed] [Google Scholar]
- 8.Zhao Y, Lee CK, Lin CH, Gassen RB, Xu X, Huang Z, et al. PD-L1:CD80 Cis-heterodimer triggers the co-stimulatory receptor CD28 while repressing the inhibitory PD-1 and CTLA-4 pathways. Immunity. 2019;51(1059–73): e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kudo M. Scientific rationale for combination immunotherapy of hepatocellular carcinoma with anti-PD-1/PD-L1 and anti-CTLA-4 antibodies. Liver Cancer. 2019;8:413–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ducreux M, Abou-Alfa GK, Bekaii-Saab T, Berlin J, Cervantes A, de Baere T, et al. The management of hepatocellular carcinoma. Current expert opinion and recommendations derived from the 24th ESMO/World Congress on Gastrointestinal Cancer, Barcelona, 2022. ESMO Open. 2023;8:101567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gordan JD, Kennedy EB, Abou-Alfa GK, Beal E, Finn RS, Gade TP, et al. Systemic therapy for advanced hepatocellular carcinoma: ASCO guideline update. J Clin Oncol. 2024;42:1830–50. [DOI] [PubMed] [Google Scholar]
- 12.Hiraoka A, Michitaka K, Kumada T, Izumi N, Kadoya M, Kokudo N, et al. Validation and potential of albumin–bilirubin grade and prognostication in a nationwide survey of 46,681 hepatocellular carcinoma patients in Japan: the need for a more detailed evaluation of hepatic function. Liver Cancer. 2017;6:325–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bruix J, Sherman M. Practice guidelines committee AeAftSoLD. Management of hepatocellular carcinoma. Hepatology. 2005;42:1208–36. [DOI] [PubMed] [Google Scholar]
- 14.Di Martino M, Marin D, Guerrisi A, Baski M, Galati F, Rossi M, et al. Intraindividual comparison of gadoxetate disodium-enhanced MR imaging and 64-section multidetector CT in the Detection of hepatocellular carcinoma in patients with cirrhosis. Radiology. 2010;256:806–16. [DOI] [PubMed] [Google Scholar]
- 15.Sano K, Ichikawa T, Motosugi U, Sou H, Muhi AM, Matsuda M, et al. Imaging study of early hepatocellular carcinoma: usefulness of gadoxetic acid-enhanced MR imaging. Radiology. 2011;261:834–44. [DOI] [PubMed] [Google Scholar]
- 16.Llovet JM, Villanueva A, Marrero JA, Schwartz M, Meyer T, Galle PR, et al. Trial design and endpoints in hepatocellular carcinoma: AASLD consensus conference. Hepatology. 2021;73:158–91. [DOI] [PubMed] [Google Scholar]
- 17.Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg. 1973;60:646–9. [DOI] [PubMed] [Google Scholar]
- 18.Johnson PJ, Berhane S, Kagebayashi C, Satomura S, Teng M, Reeves HL, et al. Assessment of liver function in patients with hepatocellular carcinoma: a new evidence-based approach-the ALBI grade. J Clin Oncol. 2015;33:550–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45:228–47. [DOI] [PubMed] [Google Scholar]
- 20.Lencioni R, Llovet JM. Modified RECIST (mRECIST) assessment for hepatocellular carcinoma. Semin Liver Dis. 2010;30:52–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.National Cancer Institute. Common terminology criteria for adverse events (CTCAE) v5.0. 2017. https://ctep.cancer.gov/protocolDevelopment/electronic_applications/ctc.htm#ctc_50. Accessed 1 Jun 2024.
- 22.Kanda Y. Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant. 2013;48:452–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vafaei S, Zekiy AO, Khanamir RA, Zaman BA, Ghayourvahdat A, Azimizonuzi H, et al. Combination therapy with immune checkpoint inhibitors (ICIs); a new frontier. Cancer Cell Int. 2022;22:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Adachi Y, Kamiyama H, Ichikawa K, Fukushima S, Ozawa Y, Yamaguchi S, et al. Inhibition of FGFR reactivates IFNγ signaling in tumor cells to enhance the combined antitumor activity of lenvatinib with anti-PD-1 antibodies. Cancer Res. 2022;82:292–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alsina A, Kudo M, Vogel A, Cheng AL, Tak WY, Ryoo BY, et al. Effects of subsequent systemic anticancer medication following first-line lenvatinib: a post hoc responder analysis from the phase 3 REFLECT study in unresectable hepatocellular carcinoma. Liver Cancer. 2020;9:93–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Song X, Kelley RK, Green M, Standifer N, Lim K, Zhou D, et al. Modeling of proliferating CD4 and CD8 T-cell changes to tremelimumab exposure in patients with unresectable hepatocellular carcinoma. Clin Pharmacol Ther. 2023;114:874–82. [DOI] [PubMed] [Google Scholar]
- 27.Liu J, Liu Y, Meng L, Liu K, Ji B. Targeting the PD-L1/DNMT1 axis in acquired resistance to sorafenib in human hepatocellular carcinoma. Oncol Rep. 2017;38:899–907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Deng H, Kan A, Lyu N, Mu L, Han Y, Liu L, et al. Dual vascular endothelial growth factor receptor and fibroblast growth factor receptor inhibition elicits antitumor immunity and enhances programmed cell death-1 checkpoint blockade in hepatocellular carcinoma. Liver Cancer. 2020;9:338–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Abe H, Endo K, Kuroda H, Oikawa T, Abe T, Ito A, et al. Immune checkpoint inhibitor-associated colitis in unresectable hepatocellular carcinoma: two cases of early onset after treatment with durvalumab plus tremelimumab. Clin J Gastroenterol. 2024;17:307–10. [DOI] [PubMed] [Google Scholar]
- 30.Yanai S, Toya Y, Sugai T, Matsumoto T. Gastrointestinal adverse events induced by immune-checkpoint inhibitors. Digestion. 2021;102:965–73. [DOI] [PubMed] [Google Scholar]
- 31.Terashima T, Yamashita T, Sunagozaka H, Arai K, Kawaguchi K, Kitamura K, et al. Analysis of the liver functional reserve of patients with advanced hepatocellular carcinoma undergoing sorafenib treatment: prospects for regorafenib therapy. Hepatol Res. 2018;48:956–66. [DOI] [PubMed] [Google Scholar]
- 32.Hiraoka A, Kumada T, Atsukawa M, Hirooka M, Tsuji K, Ishikawa T, et al. Early relative change in hepatic function with lenvatinib for unresectable hepatocellular carcinoma. Oncology. 2019;97:334–40. [DOI] [PubMed] [Google Scholar]
- 33.Yau T, Park JW, Finn RS, Cheng AL, Mathurin P, Edeline J, et al. Nivolumab versus sorafenib in advanced hepatocellular carcinoma (CheckMate 459): a randomised, multicentre, open-label, phase 3 trial. Lancet Oncol. 2022;23:77–90. [DOI] [PubMed] [Google Scholar]
- 34.Hiraoka A, Kumada T, Tada T, Hirooka M, Kariyama K, Tani J, et al. Early experience of atezolizumab plus bevacizumab treatment for unresectable hepatocellular carcinoma BCLC-B stage patients classified as beyond up to seven criteria—multicenter analysis. Hepatol Res. 2022;52:308–16. [DOI] [PubMed] [Google Scholar]
- 35.Iwamoto H, Shimose S, Noda Y, Shirono T, Niizeki T, Nakano M, et al. Initial experience of atezolizumab plus bevacizumab for unresectable hepatocellular carcinoma in real-world clinical practice. Cancers (Basel). 2021;13:2786. [DOI] [PMC free article] [PubMed] [Google Scholar]