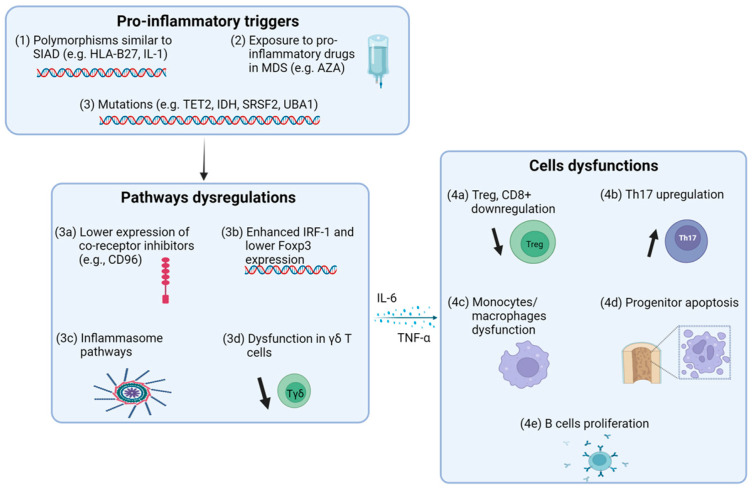
Figure 1.
Overview of pro-inflammatory homeostasis in MDS. (1) Genetic polymorphisms, such as HLA-B27 and IL-1, are shared between SIAD and MDS patients. (2) Some drugs used to treat MDS have pro-inflammatory effects. (3) Mutations identified in MDS patients predispose them to a pro-inflammatory state, leading to (3a) reduced expression of co-inhibitory receptors, such as CD96, (3b) increased IRF-1 and decreased Foxp3 expression, (3c) upregulation of inflammasome pathways, and (3d) dysfunction of γδ T cells, a subset of non-conventional T lymphocytes that are crucial for recognizing and eliminating stressed or transformed cells, including auto-reactive cells. This pro-inflammatory homeostasis ultimately results in (4a) downregulation of Tregs and CD8+ T cells, (4b) upregulation of Th17 CD4+ T cells, which are key players in inflammation and development of autoimmunity, (4c) dysfunction of monocytes and macrophages, (4d) pro-apoptotic effects on hematopoietic stem cells mediated by pro-inflammatory cytokines, such as interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α), and (4e) increased B cell proliferation (MDS: myelodysplastic syndrome).