Abstract
Background and objectives
Hypertension (HTN) is a leading cause of non-communicable disease in low- and middle-income countries, including Bangladesh. Thus, the objectives of this study were to investigate the associated risk factors for HTN and develop with validate a monogram model for predicting an individual's risk of HTN in Bangladesh.
Materials and methods
This study exploited the latest nationally representative cross-sectional BDHS, 2017–18 data, which consisted of 6569 participants. LASSO and logistic regression (LR) analysis were performed to reduce dimensionality of data, identify the associated risk factors, and develop a nomogram model for predicting HTN risk in the training cohort. The discrimination ability, calibration, and clinical effectiveness of the developed model were evaluated using validation cohort in terms of area under the curve (AUC), calibration plot, decision curve analysis, and clinical impact curve analysis.
Results
The combined results of the LASSO and LR analysis demonstrated that age, sex, division, physical activity, family member, smoking, body mass index, and diabetes were the associated risk factors of HTN. The nomogram model achieved good discrimination ability with AUC of 0.729 (95 % CI: 0.685–0.741) for training and AUC of 0.715 (95 % CI: 0.681–0.729)] for validation cohort and showed strong calibration effects, with good agreement between the actual and predicted probabilities (p-value = 0.231).
Conclusion
The proposed nomogram provided a good predictive performance and can be effectively utilized in clinical settings to accurately diagnose hypertensive patients who are at risk of developing severe HTN at an early stage in Bangladesh.
Keywords: Hypertension, LASSO, Logistic regression, Nomogram, Bangladesh
1. Introduction
Hypertension (HTN), also known as raised or high blood pressure, is a chronic condition and major contributor for developing different type of cardiovascular diseases (CVDs), such as coronary heart disease, stroke, peripheral arterial disease, cerebrovascular, aortic disease, myocardial infarction [[1], [2], [3], [4]]. It is the leading cause of illness, death, and disability and places a heavy burden on the healthcare system. Globally, the number of adults with HTN increased from 594 million in 1975 to 1.13 billion in 2015; this figure will be expected to 1.56 billion (29.2 %) in 2025 [5]. The World Health Organization (WHO) estimates that 1.28 billion adults aged 30–79 years worldwide have HTN, most (two-thirds) living in low- and middle-income countries [6]. According to the most recent survey in Bangladesh, among adults over 35 years old, about 26 % of people had HTN in 2011, and this proportion increased by 40 % in 2018 [7]. HTN tends to become more common with increasing individual's age. After age 35, the risk of developing high blood pressure increases significantly due to both age-related physiological changes (stiffening of blood vessels) and lifestyle-related factors (poor diet, reduced physical activity, weight gain, and prolonged stress). Moreover, non-communicable diseases, like HTN, claimed the lives of 41 million populaces worldwide, accounting for 74 % of all deaths [8]. In Bangladesh, HTN is one of the ten leading reported causes of death and approximately 4 % of deaths in Bangladesh occur due to complications related to hypertensive disorders [9]. In the upcoming years, it is expected that the prevalence of HTN will increase; raising medical and public health concerns that would necessitate early detection, proactive prevention, and treatment in Bangladesh.
Early detection of critical risk factors as well as accurate diagnosis the risk of HTN can play a key role for timely intervention with implementation in preventing HTN and other associated diseases [10]. It is therefore highly required to construct a model to identify the likelihood of HTN in order to aid in risk assessment and management. Over the past decade, a few studies have been done to develop a diagnosis model for predicting the risk of HTN in different countries, including Bangladesh based on different populations [[11], [12], [13], [14], [15], [16]]. The risk factors for HTN in these models differed significantly across studies. A risk prediction model of HTN was developed for a certain racial, ethnic, or national group may not consequently be directly applicable to other population, specially, failed to extend those models to general older adults with HTN. Additionally, there have been no attempts to utilize a nomogram model in Bangladesh to detect and predict the risk of HTN. The nomogram is a simple, effective visual prognosis tool, enabling the estimation of event risk by calculating a score derived from statistical models incorporating multiple factors. It is widely used in both cross sectional and prospective study designs to predict an individual's risk of several diseases [[17], [18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28]]. However, to our best knowledge, this is the first study in Bangladesh to develop a nomogram model for predicting the risk of HTN based on its associated risk factors. The proposed nomogram can help clinicians in early detection of patients who are at high risk of HTN. Consequently, this information can then be used as a guide for personalized prevention and treatment to delay or prevent the development of HTN among individuals in Bangladesh.
2. Materials and methods
2.1. Data source
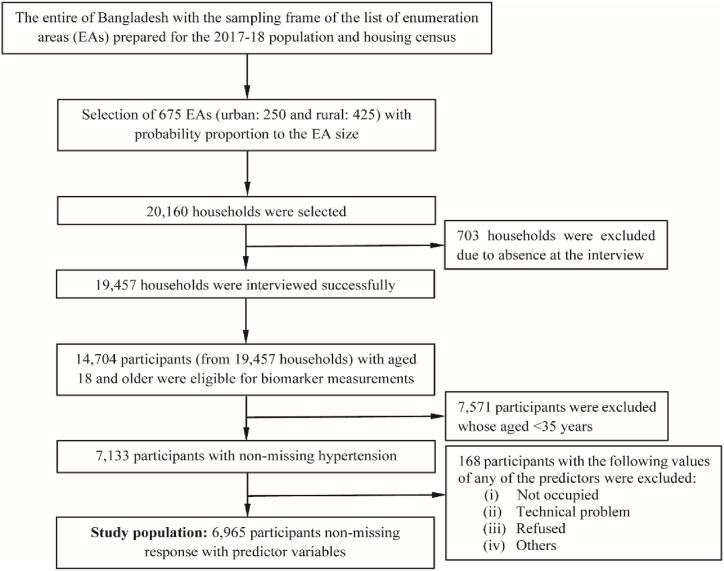
The data utilized in this investigation was obtained from the Bangladesh demographic and health survey (BDHS), 2017–18. Samples were taken from different households in BDHS, 2017-18 using a two-stage stratified cluster sampling technique [29]. In the first stage, 675 units (urban: 250 and rural: 425) were selected using a proportionate equal probability method based on the size of the enumeration area (EA). In the second stage, households were randomly selected from each EA utilizing a systematic random sampling method. 20,160 households were selected, of which 19,457 were successfully interviewed, containing a total of 14,704 participants (women: 8013 and men: 6691) with age 18 and older were eligible for biomarker measurements. The detailed description of the survey design, methodologies, sample size, questionnaires utilized, and findings can be found in the BDHS, 2017-18 report [29]. Our study included participants with aged 35 and older, totaling 7,133, for whom the biomarker data are available. After excluding the missing values of the response and predictor variables, a total of 6965 respondents were enrolled for the final analysis. The procedure for selecting samples was illustrated in Fig. 1.
Fig. 1.
Sample selection procedure and sample size. EA: Enumeration area.
2.2. Response variable
HTN was considered as a response variable, which was determined according to the 2003 American Heart Association (AHA) guidelines [30,31]. The guidelines are in line with other commonly used guidelines, like the International Society of Hypertension Global Hypertension Practice Guidelines (ISH), European Society of Cardiology/European Society of Hypertension Arterial Hypertension Guidelines (ESC/ESH), etc. [32]. Hypertensive patients were defined the following criteria: systolic blood pressure (SBP) of 140 mmHg or higher and/or diastolic blood pressure (DBP) of 90 mmHg or higher, and/or the use of antihypertensive medication during the survey [33].
2.3. Factors/explanatory variables
We considered demographic, socioeconomic, behavioral, and medical related explanatory variables as a risk factor for HTN based on the previous sittings [[34], [35], [36], [37], [38], [39]]. The factors include age, sex, residence, division, marital status (MS), education, working, physical activity (PA), wealth, family member (FM), smoking, body mass index (BMI), and diabetes. BMI was categorized as underweight (BMI<18.5 kgm−2), normal (18.5–24.9 kgm−2) and overweight/obese (25.0 kgm−2) [25]. Table 1 represents detailed description and categorizations of the chosen risk factors.
Table 1.
Factors description and class label.
| Factors | Description | Class label |
|---|---|---|
| Age | Age of the respondents (years) | 35-44, 45–54, 55–64, >64 |
| Sex | Sex of the respondents | Male, Female |
| Residence | Place of residence | Urban, Rural |
| Division | Region of the respondents | Dhaka, Barisal, Chattogram, Khulna, Mymensingh, Rajshahi, Rangpur, Sylhet |
| MS | Marital status | Never married, Married, Widowed, Divorced |
| Education | Level of education | No-education, Primary, Secondary, Higher |
| Working | Working status | No, Yes |
| PA | Physical activity | Physically inactive, Physically active |
| Wealth | Wealth index | Poorest, Poorer, Middle, Richer, Richest |
| FM | Family member | 1-3, 4–6, >6 |
| Smoking | Smoking habit | No, Yes |
| BMI | Body mass index (kg/m2) | Normal, Underweight, Overweight/Obese |
| Diabetes | Diabetes status | No, Yes |
2.4. Statistical analysis
The background characteristics of the study participants were reported as numbers (%) for the chosen factors. The chosen factors were presented as numbers (%) to depict the background characteristics of the study participants. The Pearson's test was employed to examine the association between several chosen factors and HTN status. Data analysis was carried out by using IBM SPSS and R.
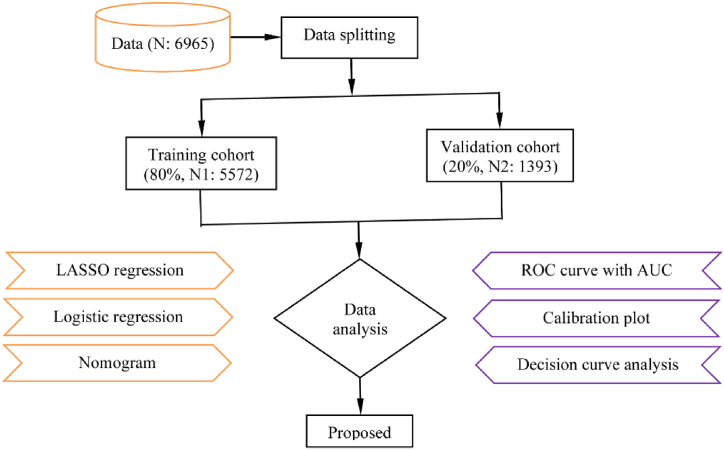
2.5. Data splitting
The dataset was partitioned into two cohorts as training and validation based on the stratified sampling with the ratio of 8:2 [40]. There were 5572 respondents (HTN: 1936, non-HTN: 3636) in the training cohort and 1393 (HTN: 479, non-HTN: 914) in the validation cohort.
2.6. Screening the risk factors
The widely applicable least absolute shrinkage and selection operator (LASSO) method with 10-fold cross validation protocol was used to screen the predictive risk factors of HTN in the training cohort [41]. The non-zero coefficients of the variables were selected as a prognostic risk factor of HTN in terms of the optimal lambda value. The optimal value of lambda ( showed the lowest possible prediction error.
2.7. Development of logistic regression for nomogram
Using the screening risk factors obtained from LASSO, logistic regression (LR) with backward elimination was adopted to develop a prediction model in the training cohort. The model can be stated as follows using the response variable and the screening risk factors .
where, , , …, were the parameters or coefficients. In this model, the parameters are often estimated via maximum likelihood estimation method. A risk factor with P-values<0.05 was considered the significantly associated determinants of HTN. A forest plot is used to display the significant risk factors of HTN. The significant risk factors were then used to develop a nomogram based on the LR model in the training cohort. The length of the line corresponding to each risk factor analyzed in the nomogram, indicated the degree to which variable influenced the predicted outcome of HTN [42].
2.8. Performance evaluation
The nomogram model's performance was assessed through the discriminatory power and calibration plot, utilizing 500 bootstraps resample in the validation cohort. The model's discrimination power was measured using the receiver operating characteristic (ROC) curve, along with the area under the ROC curve (AUC) or concordance index (C-index). AUC values typically range from 0.5 to 1, where 0.5 indicates no discrimination, 1 indicates perfect discrimination, and values ≥ 70 indicate good discrimination. Calibration analysis is crucial in clinical decision-making, because it demonstrates the consistency between the actual class label and the predicted outcome of the developed model. The model's calibration was assessed using a calibration curve and the Hosmer-Lemeshow test. A slope on the 45-degree line suggested that the calibration was perfect. The standard performance metrics (discrimination and calibration) for risk prediction models were unable to address the question of how useful the develop nomogram would be in clinically practice. Decision curve analysis (DCA) was then used to assess the model's clinical usefulness and efficacy to calculate the net benefits [43]. The overall study design flowchart is shown in Fig. 2.
Fig. 2.
Overall study design flowchart. LASSO: Least absolute shrinkage and selection operator; ROC: Receiver operating characteristic curve; AUC: Area under the curve; N: Total sample size; N1: Training sample size; N2: Validation sample size.
3. Results
3.1. Background characteristics
Table 2 represents the background characteristics of the study population. This study comprised of 6595 respondents with 13 HTN related predictor variables. The mean age of the respondents was . Over half of the participants (51.5 %) identified as female, while the remaining 48.5 % identified as male. Of the respondents, 84.7 % had married. The larger proportion (38.4 %) of the respondents had no education, whereas 32.2 % primary, 19.4 % secondary, and 10.0 % higher. The overall prevalence of HTN was 34.7 % (Table 2).
Table 2.
Background characteristics.
| Factors | Total n (%) | HTN Status |
p-value | |
|---|---|---|---|---|
| HTN n (%) | Non-HTN n (%) | |||
| Overall | 6965 (100) | 2415(34.7) | 4550(65.3) | |
| Age, >64, n(%) | 1194(17.1) | 587(49.2) | 607(50.8) | <0.001 |
| Sex, female, n(%) | 3589(51.5) | 1353(37.7) | 2236(62.3) | <0.001 |
| Residence, urban, n(%) | 2411(34.6) | 884(36.7) | 1527(63.3) | 0.0120 |
| Division, rangpur, n(%) | 922(13.2) | 350(38.0) | 572(62.0) | <0.001 |
| MS, widowed, n(%) | 965(11.0) | 463(48.0) | 502(52.0) | <0.001 |
| Education, higher, n(%) | 696(10.0) | 259(37.2) | 437(62.8) | 0.0280 |
| Working, no, n(%) | 23.85(30.4) | 1004(42.1) | 1381(57.9) | <0.001 |
| PA, inactive, n(%) | 4021(57.73) | 1580(39.3) | 2441(60.7) | <0.001 |
| Wealth, richest, n(%) | 1572(22.6) | 662(42.1) | 910(57.9) | <0.001 |
| FM, 1–3, n(%) | 1547(20.9) | 594(38.4) | 953(61.6) | <0.001 |
| Smoking, no, n(%) | 5436(78.0) | 1923(35.4) | 3513(64.6) | 0.0210 |
| BMI(Kg/m2), overweight/obese, n(%) | 1811(26.4) | 848(46.8) | 963(53.2) | <0.001 |
| Diabetes, yes, n(%) | 1047(15.0) | 456 (43.6) | 591 (56.4) | <0.001 |
MS: Marital status; PA: Physical activity; FM: Family member; BMI: Body mass index; HTN: Hypertension.
The predictor variable distribution by HTN status is presented in Table 2. Respondents aged 65 years and older had a higher prevalence of HTN. Women participants exhibited a higher prevalence of HTN compared to men. The prevalence rate of HTN was found to be higher among respondents residing in the Rangpur division (38.0 %), while the Mymensingh division exhibited the lowest prevalence rate (28.9 %). Widowed respondents showed higher prevalence of HTN (48.0 %), compeering to never married (20.8 %), married (32.5 %), and divorced (37.2 %). The prevalence of HTN was the highest in overweight/obese respondents (46.8 %) and the lowest underweight (24.1 %). Diabetes respondents (43.6 %) had more hypertensive than non-diabetes respondents (33.1 %).
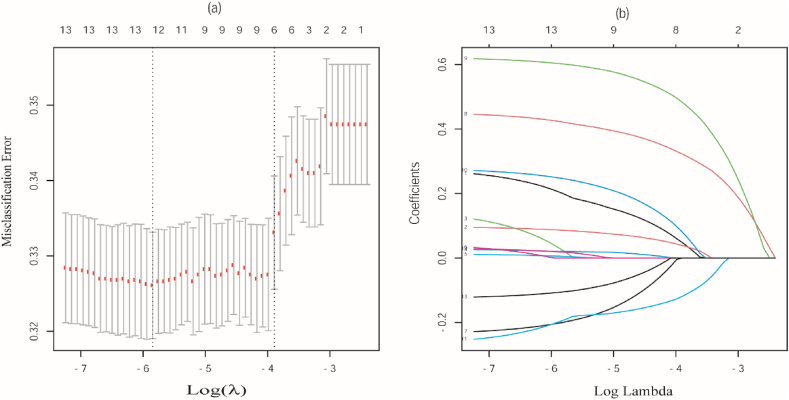
3.2. Risk factors selection
Fig. 3(a) represents the tuning parameters of the LASSO regression model and Fig. 3(b) represents the coefficient profiles are generated on the basis of the optimal tuning parameter (λ) in Fig. 3(a). We found that 12 relevant risk factors out of 13 for HTN by LASSO from the training cohort. The selecting risk factors are age, sex, division, MS, education, working, PA, wealth, FM, smoking, BMI, and diabetes. The selected risk factors were incorporated in LR analysis for developing the prediction model.
Fig. 3.
Identification of risk factors by the LASSO regression model. (a) Tuning parameter (); (b) Coefficient profiles are generated on the basis of the optimal tuning parameter () in (A).
3.3. Model development
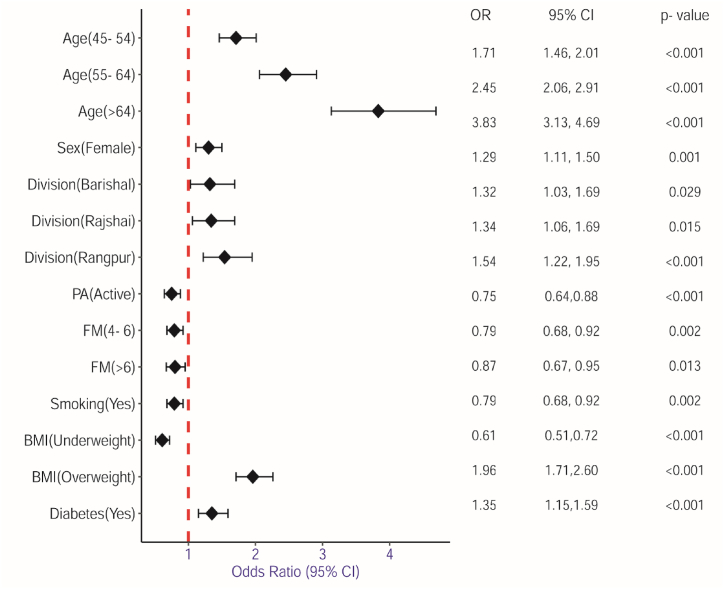
The results of the LR analysis have been presented in Table 3. The LR model indicated that individuals aged 45–54 (OR: 1.71, 95 % CI: 1.46–2.01, p < 0.001), 55–64 (OR: 2.45, 95 % CI: 2.06–2.91, p < 0.001), and >64 (OR: 3.83, 95 % CI: 3.13–4.69, p < 0.001) had significantly higher chances of having HTN compared to those aged 35–44 years. Female respondents (OR: 1.29, 95 % CI: 1.11–1.50, p = 0.001) exhibited more likely to have HTN compared to its counterpart. In comparison to respondents in Dhaka, respondents living in Barisal (OR: 1.32, 95 % CI: 1.03–1.69, p = 0.029), Rajshahi (OR: 1.34, 95 % CI: 1.06–1.69, p = 0.015), Rangpur (OR: 1.54, 95 % CI: 1.22–1.95, p < 0.001) showed higher odds of having HTN. Respondents with physically active (OR: 0.75, 95 % CI: 0.64–0.88, p < 0.001) found lower odds of having HTN than physically inactive. Respondents having 4–6 (OR:0.79, 95 % CI: 0.68–0.92, p = 0.002) and >6 (OR: 0.80, 95 % CI: 0.67–0.95, p = 0.013) FM showed lower chance of having HTN than 1–3. Respondents habits smoking found lower odds of getting risk of HTN than non-habit respondents (OR: 0.79, 95 % CI: 0.68–0.92, p = 0.002). Underweight (OR: 0.61, 95 % CI: 0.51–0.72, p < 0.001), respondents have lower odds of having HTN than normal while overweight (OR: 1.96, 95 % CI: 1.71–2.26, p < 0.001) respondents have odds of having HTN that are more than twice as high. In comparison to respondents without diabetes, those with diabetes had greater odds of having HTN (OR: 1.35, 95 % CI: 1.15–1.59, p < 0.001). Fig. 4 shows the risk factors for HTN that are significantly associated in LR model.
Table 3.
Predictive risk factors of HTN using LR model.
| Factors | OR |
95 % CI for OR |
p-value |
|
|---|---|---|---|---|
| Lower | Upper | |||
| Age | ||||
| 35-44® | 1.00 | |||
| 45–54 | 1.71 | 1.46 | 2.01 | <0.001 |
| 55–64 | 2.45 | 2.06 | 2.91 | <0.001 |
| >64 | 3.83 | 3.13 | 4.69 | <0.001 |
| Sex | ||||
| Male® | 1.00 | |||
| Female | 1.29 | 1.11 | 1.50 | 0.001 |
| Division | ||||
| Dhaka® | 1.00 | |||
| Barisal | 1.32 | 1.03 | 1.69 | 0.029 |
| Chattogram | 1.09 | 0.87 | 1.37 | 0.460 |
| Khulna | 1.12 | 0.89 | 1.39 | 0.342 |
| Mymensingh | 0.92 | 0.72 | 1.18 | 0.513 |
| Rajshahi | 1.34 | 1.06 | 1.69 | 0.015 |
| Rangpur | 1.54 | 1.22 | 1.95 | <0.001 |
| Sylhet | 1.035 | 0.80 | 1.32 | 0.846 |
| MS | ||||
| Never married® | 1.00 | |||
| Married | 1.79 | 0.51 | 6.34 | 0.366 |
| Widowed | 2.23 | 0.62 | 7.99 | 0.220 |
| Divorced | 2.44 | 0.64 | 9.34 | 0.193 |
| Education | ||||
| No-education® | 1.00 | |||
| Primary | 0.98 | 0.85 | 1.14 | 0.815 |
| Secondary | 1.13 | 0.94 | 1.36 | 0.179 |
| Higher | 0.96 | 0.75 | 1.22 | 0.722 |
| Working | ||||
| No® | 1.00 | |||
| Yes | 1.15 | 0.96 | 1.37 | 0.126 |
| PA | ||||
| Inactive® | 1.00 | |||
| Active | 0.75 | 0.64 | 0.88 | <0.001 |
| Wealth | ||||
| Poorest® | 1.00 | |||
| Poorer | 0.99 | 0.81 | 1.20 | 0.901 |
| Middle | 1.18 | 0.97 | 1.43 | 0.099 |
| Richer | 1.07 | 0.87 | 1.32 | 0.505 |
| Richest | 1.17 | 0.94 | 1.46 | 0.170 |
| FM | ||||
| 1-3® | 1.00 | |||
| 4–6 | 0.79 | 0.68 | 0.92 | 0.002 |
| >6 | 0.80 | 0.67 | 0.95 | 0.013 |
| Smoking | ||||
| No® | 1.00 | |||
| Yes | 0.79 | 0.68 | 0.92 | 0.002 |
| BMI | ||||
| Normal® | 1.00 | |||
| Underweight | 0.61 | 0.51 | 0.72 | <0.001 |
| Overweight | 1.96 | 1.71 | 2.26 | <0.001 |
| Diabetes | ||||
| No® | 1.00 | |||
| Yes | 1.35 | 1.15 | 1.59 | <0.001 |
MS: Marital status; PA: Physical activity; FM: Family member; BMI: Body mass index; OR: Odds ratio; CI: Confidence interval.
Fig. 4.
Forest plot for significantly associated risk factors of HTN. Risk factors is represented on the Y-axis and odds ratio represented on the X-axis. The red vertical line indicates the reference line at OR = 1. The black diamond in the forest plot illustrates the summary effect estimate and its confidence interval. MS: Marital status; PA: Physical activity; FM: Family member; BMI: Body mass index; OR: Odds ratio; CI: Confidence interval.
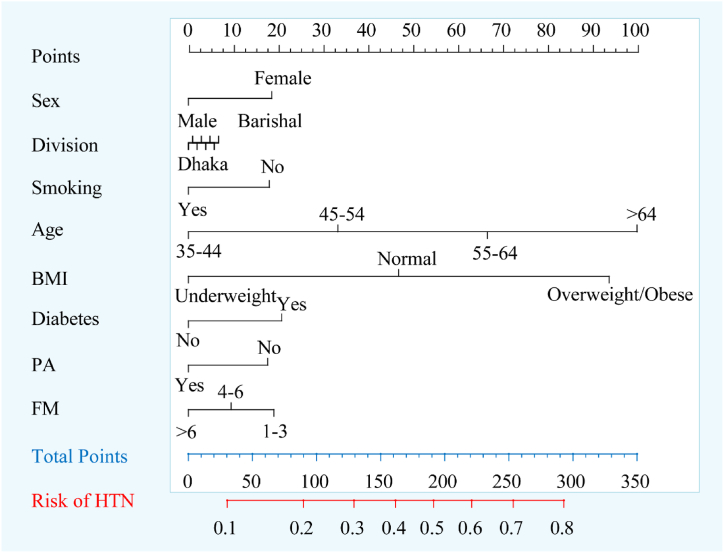
3.4. Nomogram development
Based on the results obtained from the LR analysis, the significant risk factors (age, sex, division, PA, FM, smoking, BMI, diabetes) were included in the construction of the nomogram to predict the risk of HTN (Fig. 5). There were 11 axes in the nomogram, with axis 2-9 represented each prognostic risk factors in the model. Each risk factor is assigned a different weighted score in the nomogram. The total points, which were presented in axis 10 and corresponded to the risk in the prediction of HTN in axis 11, were calculated by adding the single scores of each risk factor. The nomogram then displayed the risk of HTN as a percentage.
Fig. 5.
Nomogram for predicting individuals' risk of HTN. The value of an individual patient is represented on each variable axis, from which a line is drawn upward to determine the points assigned for each variable value. Sum the points from all the variables to get the total points, which is locate on the "Total Points" axis, and drawn a vertical line down from the total points to identify the corresponding risk of HTN. BMI: Body mass index; PA: Physical activity; FM: Family member; MS: Marital status; PA: Physical activity; FM: Family member; BMI: Body mass index; HTN: Hypertension.
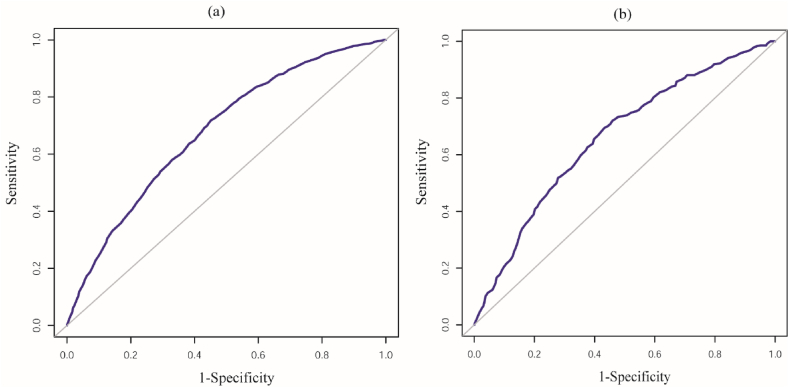
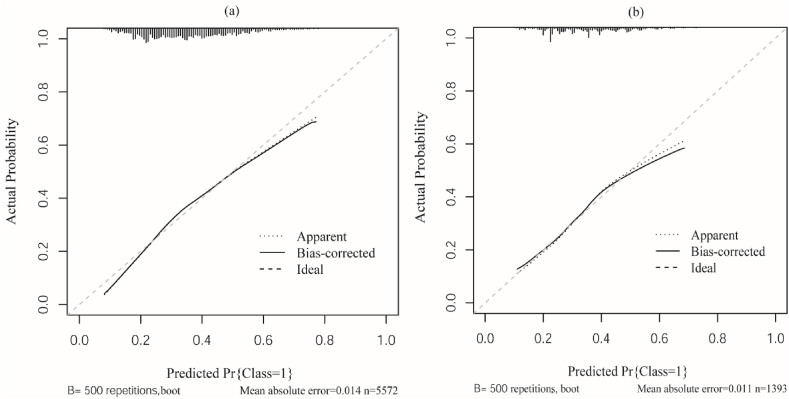
3.5. Performance of the developed nomogram
The model's capacity to discriminate well was shown by the AUC of the nomogram when using the above eight risk factors, which was AUC of 0.729 (95 % CI: 0.685–0.741) with sensitivity of 89.41 % for the training and AUC of 0.715 (95%CI: 0.681–0.729) with sensitivity of 87.75 % for the validation cohort. Fig. 6(a) and (b) depict the corresponding ROC curves for the training and validation cohort, respectively. The calibration plot of the model is presented in Fig. 7(a) for the training cohort and Fig. 7(b) for the validation cohort, showing that the plots are near to the diagonal line, indicating that the model's predictions and the actual class probabilities for HTN were highly consistent. The Hosmer-Lemeshow test indicated that the model exhibited a good fit ( = 9.653; p-value = 0.231).
Fig. 6.
ROC curve of the nomogram model (a) Training cohort and (b) Validation cohort. The X-axis represented 1-specificity, also known false positive rate (FPR), while Y-axis represented sensitivity, also known true positive rate (TPR). The diagonal gray line indicates no discrimination, where the model has no ability to distinguish between HTN and non-HTN. The blue ROC curves depict the models' performance across different threshold levels.
Fig. 7.
Calibration plot of the nomogram (a) Training cohort and (b) Validation cohort. The nomogram model's predicted probability of HTN was represented by the X-axis, and the actual probability was represented by the Y-axis. The ideal line, depicted as a diagonal dashed line, illustrated the predicted probability aligns perfectly with the actual probability under optimal condition. The apparent line represents the predicted probabilities of outcomes directly from the nomogram model and the bias-corrected line reflects the expected performance of the model on unseen data. Together, closer these two lines to the ideal line signifies an improved nomogram model and better calibration.
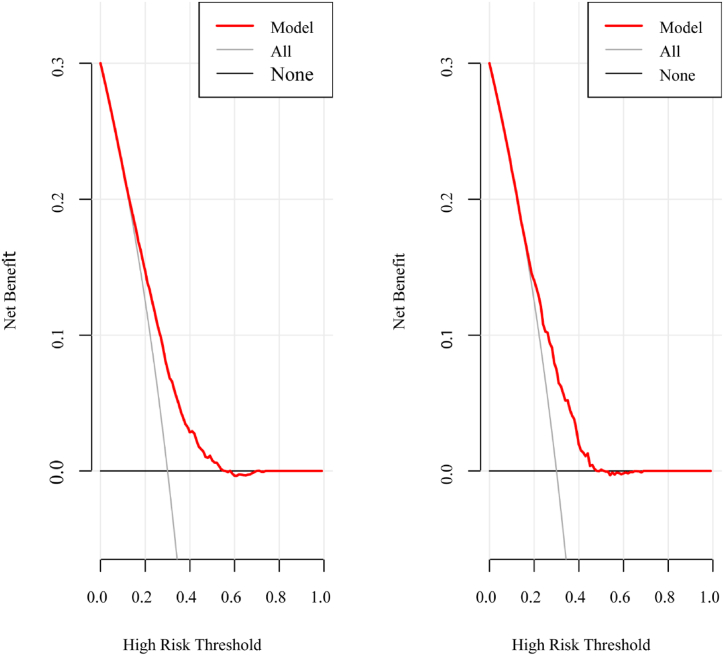
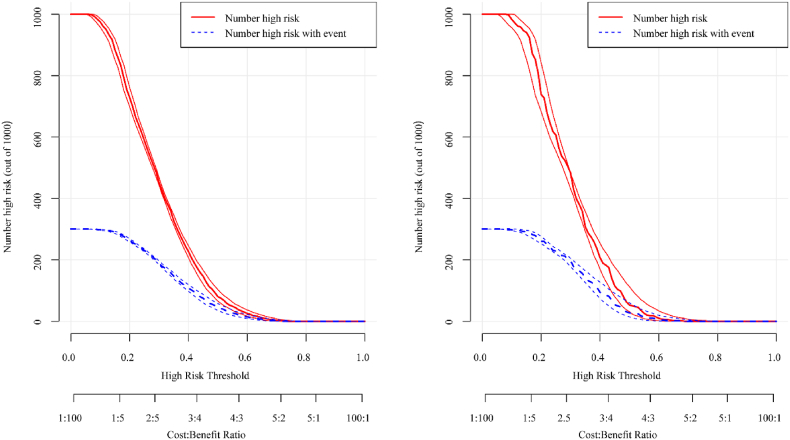
3.6. Clinical utility
According to the DCA curve, the nomogram provided larger net benefits for identifying HTN patients and assisting in clinical decisions for nearly all threshold probabilities in the training cohort (Fig. 8(a)) and validation cohort (Fig. 8 (b)). We generated clinical impact curves based on the DCA results to assess the nomogram clinical utility. The nomogram's clinical impact curves showed that the actual class probability and the predicted probability were nearly identical in the training cohort. (Fig. 9(a)). The validation cohort also yielded the similar findings (Fig. 9(b)).
Fig. 8.
Decision curve of the nomogram. (a) Training cohort and (b) Validation cohort. The X-axis represents different risk thresholds, while Y-axis represents net benefit. The red line indicates the net benefit of the nomogram model across different thresholds. The gray line (ALL), representing the "treat all as high risk", assumes that every individual is considered as high risk and therefore receives treatment or intervention. The gray-black line (None), representing the strategy where "no one is treated", assumes that no interventions are made based on the model.
Fig. 9.
Clinical impact curve of the nomogram. (a) Training cohort and (b) Validation cohort. The X-axis represents the high-risk threshold and the Y-axis represents the number of high-risk (out of 1000). The red line depicted the number of high-risk cases, while the blue line represented the number of high-risk cases associated with an event. The cost: benefit ratio represents the trade-off between the clinical costs of false positives (e.g., unnecessary treatments, tests) and the real benefits of true positives (e.g., correctly diagnosed cases, successful interventions).
4. Discussion
The data indicates that 34.70 % of people 35 years of age and older have HTN. The STEPwise approach to surveillance (STEPS) surveys conducted in a number of South Asian nations found alarming national prevalence levels of HTN, including Sri Lanka (26 % in 2015), Nepal (25 % in 2019), Bhutan (26 % in 2014), and Myanmar (26 % in 2014) [44]. The various STEPS surveys conducted in South Asia were not able to be compared with each other because of the wide range of ages among respondents and the varying time frames. However, the prevalence of HTN increased with age in Bangladesh, with rates of 24.9 % among those aged 35–44 years, 34.5 % among those aged 45–54 years, 40.4 % among those aged 55–64 years, and 49.2 % among those aged over 64 years. With increasing elderly populations and rising trends in HTN prevalence, Bangladesh undoubtedly bears a heavy burden of morbidity and mortality. Without addressing leading NCDs like HTN, it will be impossible to achieve the health-related Sustainable Development Goals by 2030. Therefore, this study investigates the associated risk factors of HTN and developed with validated a monogram prediction model for better predicting an individual with HTN risk based on the latest nationally representative, BDHS 2017-18 data in Bangladesh. Off all 13 risk factors, 8 (age, sex, division, PA, FM, smoking, BMI, diabetes) prognostic predictive risk factors were selected by combining LASSO and LR analysis, and finally incorporated to develop the nomogram model. By analyzing AUC and calibration plot in the training and validation cohort, the develop nomogram showed good predictive performance and high stability. DCA shown the model yielded a high clinical net benefit for defection of HTN, which can therefore demonstrate the good clinical usefulness.
4.1. Comparison of the current study with previously reported HTN risk prediction models
Previously several studies have been conducted in the literature to develop and validate a nomogram model for predicting the risk of HTN across different countries utilizing diverse datasets (Table 4).
Table 4.
Comparison of the current study with similar previously reported HTN risk prediction models.
| Author | Year | Country | Sample size | Data collected by | PIM | Predictors | AUC |
|---|---|---|---|---|---|---|---|
| Deng et al. [9] | 2021 | China | 6201 | Physical examination survey | LASSO & MLR | FH, Age, SBP, DBP, BMI, MCHC, MPV, TP, TBIL, and TG | Training: 0.750 Validation: 0.772 Training: 0.705 Validation: 0.697 |
| Xu et al. [45] | 2021 | China | 5327 | Health service centers | LASSO & MLR | Age, Smoking, AC, BMI, SBP, DBP, DSI, YBI, DOI, FVI, LDL, ADC, Cholesterol, and FH | Training: 0.803 Validation: 0.809 |
| Wang et al. [46] | 2023 | USA | 13,293 | NHANES | MLR | Age, Sex, Race, MS, Education, STW, PIR, Smoking, AC, ST, and HF | Training: 0.730 Validation: 0.680 |
| Wu et al. [47] | 2023 | China | 7200 | Community health service | LASSO & MLR | Age, WHR, and HDL | Training: 0.913 Validation: 0.920 |
| Yang et al. [48] | 2023 | USA | 17,125 | NHANES | LASSO &MLR | Age, MAN, SA, SP, CVD, Diabetes, CC, and HbA1C | Training: 0.800 Validation: 0.793 |
| Xu et al. [49] | 2023 | China | 18,367 | Physical examination centers | LASSO & MLR | Age, BMI, Waistline, Hipline, and RHR | Training: 0.693 Validation: 0.707 |
| Current study | Bangladesh | 6965 | BDHS | LASSO & MLR | Age, Sex, Division, PA, FM, Smoking, BMI, and Diabetes | Training: 0.729 Validation: 0.715 |
|
NHANES: National health and nutrition examination survey; BDHS: Bangladesh demographic health survey; PIM: Predictor identification method; LASSO: Least absolute shrinkage and selection operator; ULR: Univariate logistic regression; FH: Family history; BMI: Body mass index; MCHC: Mean cell hemoglobin concentration; MPV: Mean platelet volume; TP: Total protein; TBIL: Total bilirubin; TG: Triglycerides; AC: Alcohol consumption; SBP: Systolic blood pressure: DBP: Diastolic blood pressure; DSI: Daily salt intake; YBI: Yak-butter intake; DOI: Daily oil intake; FVI: Fruit and vegetable intake; LDL: Low-density lipoprotein; ADC: Abdominal circumference; MS: Marital status; STW: Sleep time on workdays; PIR: Poverty to income ratio; ST: Sedentary time; HF: Heart failure; WHR: Waist-height ratio; HDL: Heigh density lipoprotein; MAN: Monocytes and neutrophils; SA: Serum albumin; SP: Serum potassium; CVD: Cardiovascular disease; CC: Serum creatinine; HbA1C: Glycated hemoglobin; RHR: Resting heart rate; PA: Physical activity; FM: family member.
Deng et al. [9] conducted a study utilizing physical examination survey data from a sample of 6201 individuals in China. They utilized LASSO and MLR to identify the most critical predictors and subsequently develop nomograms model based on the training cohort for blood pressure measurements of 140/90 mmHg and 130/80 mmHg. The investigation revealed that FH, Age, SBP, DBP, BMI, MCHC, MPV, TP, TBIL, and TG serve as predictive indicators of HTN, which were then used to create the nomogram model. The AUC for the nomogram 140/90 was reported at 0.750 in the training cohort and 0.772 in the validation cohort. In contrast, the AUC for the nomogram 130/80 was 0.705 in the training cohort and 0.697 in the validation cohort. Thus, the nomogram 140/90 demonstrated a higher level of performance compared to the nomogram 130/80. Xu et al. [45] collected a HTN dataset from health service centers located in Xinjiang, China, which comprised a total of 5327 participants. They employed LASSO regression model to determine the predictive features associated with HTN, subsequently used MLR to identify high risk factors and construct a nomogram prediction model. In their modeling cohort, they identified 14 independent predictors of HTN, which included predictors such as age, smoking, AC, BMI, SBP, DBP, DSI, YBI, DOI, FVI, LDL, ADC, cholesterol, and FH. The AUC for both the training cohort and the validation cohort was found to be 0.803 and 0.809, respectively. Wang et al. [46] also utilized the NHANES dataset from 2007 to 2018, which comprised a total of 13,293 samples, to identify high-risk factors through a univariate logistic regression. They subsequently applied MLR to determine prominent risk predictors and create nomogram to predict HTN and assessing the model's efficacy using AUC. The findings indicated that age, sex, race, MS, education, STW, PIR, smoking, AC, ST, and HF were significant risk factors for hypertensive patients experiencing depression. These factors were incorporated into the nomogram model, with ROC analysis revealing an AUC of 0.730 for the training cohort and 0.680 for the validation cohort. Wu et al. [47] created a nomogram model utilizing data from 7200 hypertensive patients sourced from a community health service center, China. They employed the LASSO and MLR for feature selection and construct nomogram model. They indicated that age, WHR, and HDL were the significant predictors for HTN, demonstrating strong discrimination with AUC of 0.913 for the training cohort and 0.920 for the validation cohort. Yang et al. [48] employed data from the NHANES covering the period from 1999 to 2016. They utilized the LASSO and MLR to pinpoint the most significant predictors, subsequently creating a nomogram model. They identified various risk factors linked to HTN, such as age, MAN, SA, SP, CVD, diabetes, CC, and HbA1C. The nomogram model achieved an AUC of 0.800 for the training cohort and 0.793 for the validation cohort. Xu et al. [49] conducted a comprehensive series of questionnaire surveys involving 18,367 participants in China. The optimization of variable selection was achieved through the application of LASSO and MLR techniques. Following this, a nomogram model was constructed by incorporating the identified predictors. They showed that age, BMI, waistline, hipline, and RHR were the influencing predictors of HTN in men, achieving AUC of 0.693 in the training cohort and 0.707 in the validation cohort. The current study utilized data from the BDHS, 2017–18, which included a total of 6995 participants. We employed the LASSO model to determine the important predictors of HTN, subsequently applying MLR to identify the high-risk predictors and develop a nomogram model. The efficacy of the nomogram was assessed through AUC value based on the validation cohort. We found that age, sex, division, PA, FM, smoking, BMI, and diabetes are the high-risk predictors of HTN. The nomogram model attained an AUC of 0.729 for the training cohort and an AUC of 0.715 for the validation cohort. We found that our study's findings differed somewhat from those of previously reported studies because of the variation of the dataset (sample size), predictors/indicators, geographical regions and so on.
This study found older age ( 45 years) had considerably greater chances of developing HTN compared to younger adults. A statistically significant association between age and HTN was found in several recent investigations [[50], [51], [52]]. Increased rigidity of blood vessels, compromised immune system, and reduced physical activity could potentially contribute to the heightened risk of HTN in elderly individuals. Compared to male respondents, female respondents were more likely to develop HTN. The adults with age 35 year found the similar result in 2011, where around 1/3 (32 %) were hypertensive women and 1/5 (19 %) were male [53]. The risk of developing HTN in female adults increases with age or different ages, different biological and environmental factors, and usage of oral contraceptive pills (OCPs) [54]. Furthermore, mental stress and anxiety are associated with HTN, and hormonal factors such as menopause may make women more vulnerable to mental stress and anxiety [55]. Notably, the present study showed regional difference or division (Barisal, Rajshahi, Rangpur) had a significant association with the risk of developing HTN and this finding coincided with other earlier sittings [56,57]. Populaces living in Rangpur division found higher odds of having HTN risk than Dhaka. The reason why the residents of Rangpur division were more likely to develop HTN is still mostly unknown, but it may have to do with socioeconomic disparities like scarce resources, income inequality, low levels of education and social safety net programs, poor access to urban areas, and a lack of public infrastructure. It is essential for females to make lifestyle changes to reduce BMI, promote diet, and enhance physical activity. Furthermore, among adults in Bangladesh between 2011 and 2018, there was a higher chance of getting DM, HTN, and the coexistence of both conditions. The coexistence of both conditions accelerated the related complications and increases morbidity and mortality [58,59]. Unexpectedly, we found that smoking is a protective factor for HTN, which do not support the real-world situations. Smoking leads to arterial stiffness by promoting atherosclerosis and reducing the elasticity of blood vessels. Stiffer arteries result in higher systolic blood pressure and contribute to HTN. However, this finding is coincided with the previous studies [60,61]. The authors utilized data on HTN from Bangladesh and China, and revealed that individuals with a currently smoking habit exhibited a lower risk of developing HTN compared to those who do not smoke. Additionally, a recent study conducted by Asfikur Rahman et al. [62] using data from the BDHS, 2017-18 in Bangladesh, showed that smokers were less likely to develop HTN in comparison to non-smokers.
Beside the several strengths of this study, this investigation has some limitations, such as the utilization of cross-sectional data, which prevents us from examining the causal relationship between the variables. This study only included individuals aged 35 and above. In future, it might be the interest of analyzing the prevalence of HTN and its potential risk factors among young Bangladeshi adults aged between 18 and 34 years. This study was not considered several other factors like a family history of diabetes and HTN, dietary practice, lifestyle, alcohol consumption, medication history and so on due to unavailability of the data in the BDHS, 2017-18 database. The performance of the proposed nomogram will be improved by incorporating those factors.
5. Conclusion
This study explored a simple and practical nomogram for early warning patients with the risk of HTN based on the associated risk factors. The proposed nomogram model provided a good predictive performance, high consistency, and clinical applicability and can easily use as a valuable tool in clinical settings, enabling clinicians, policymakers, and even family members to accurately identify patients who may be susceptible to severe disease at an early stage. This information may be utilized in healthcare decision-making for the development of targeted treatment and individualized intervention to mitigate the load of HTN in Bangladesh.
CRediT authorship contribution statement
Merajul Islam: Writing – review & editing, Writing – original draft, Visualization, Validation, Software, Methodology, Investigation, Formal analysis, Data curation. Jahangir Alam: Writing – review & editing, Methodology, Formal analysis, Data curation, Conceptualization. Sujit Kumar: Writing – review & editing, Data curation. Ariful Islam: Writing – review & editing, Data curation. Muhammad Robin Khan: Writing – review & editing, Writing – original draft, Software, Formal analysis, Data curation. Symun Rabby: Writing – review & editing, Visualization, Investigation, Formal analysis. N.A.M. Faisal Ahmed: Writing – review & editing, Writing – original draft, Visualization, Supervision, Investigation, Formal analysis, Data curation. Dulal Chandra Roy: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Resources, Project administration, Investigation, Conceptualization.
Consent to participate
Written consent was attained from parents/caregivers of each study participants after giving details explanation of the goals and advantages of the study. The maintenance and assurance of anonymity and confidentiality were prioritized.
Ethical approval
This investigate utilized a publicly accessible survey dataset from the BDHS, 2017–18. The BDHS surveys have obtained ethical approval from the ICF Macro Institutional Review Board in Maryland, USA, as well as the National Research Ethics Committee of Bangladesh Medical Research Council (BMRC) in Dhaka, Bangladesh. Therefore, no further ethical approval is necessary for these surveys. The BDHS reports includes a comprehensive overview of the DHS program's (https://dhsprogram.com) ethical practices.
Data and code availability statement
Data or code will be made available on request.
Consent for publication
The submitted manuscript has been approved by all authors for publications.
Funding
No funding was received by the authors for this study.
Declaration of competing interest
The authors declare no conflict of interest.
Acknowledgements
The authors gratefully acknowledge the editor and reviewers for their valuable comments and suggestions, which have greatly improved the quality of this manuscript. We would also acknowledge Dr. Md. Maniruzzaman, Assistant Professor, Statistics Discipline, Khulna University, Khulna, Bangladesh as the internal reviewer.
Contributor Information
Merajul Islam, Email: merajul.stat4811@gmail.com.
Jahangir Alam, Email: jahangir.statru63@gmail.com.
Sujit Kumar, Email: sujit11214@gmail.com.
Ariful Islam, Email: ariful.stat.bio@gmail.com.
Muhammad Robin Khan, Email: khanmdrobin409@gmail.com.
Symun Rabby, Email: symunrabby1999@gmail.com.
N.A.M. Faisal Ahmed, Email: fahmed889@gmail.com.
Dulal Chandra Roy, Email: dulalroystat@yahoo.com.
References
- 1.Ahmed S., Tariqujjaman M., Rahman M.A., Hasan M.Z., Hasan M.M. Inequalities in the prevalence of undiagnosed hypertension among Bangladeshi adults: evidence from a nationwide survey. Int. J. Equity Health. 2019;18:1–2. doi: 10.1186/s12939-019-0930-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ali N., Akram R., Sheikh N., Sarker A.R., Sultana M. Sex-specific prevalence, inequality and associated predictors of hypertension, diabetes, and comorbidity among Bangladeshi adults: results from a nationwide cross-sectional demographic and health survey. BMJ Open. 2019;9(9) doi: 10.1136/bmjopen-2019-029364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.AlKaabi L.A., Ahmed L.S., Al Attiyah M.F., Abdel-Rahman M.E. Predicting hypertension using machine learning: findings from Qatar Biobank Study. PLoS One. 2020;15(10) doi: 10.1371/journal.pone.0240370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anjajo E.A., Workie S.B., Tema Z.G., Woldegeorgis B.Z., Bogino E.A. Determinants of hypertension among diabetic patients in southern Ethiopia: a case-control study. BMC Cardiovasc. Disord. 2023;23(1):233. doi: 10.1186/s12872-023-03245-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bener A., Saleh N.M., Bakir A., Bhugra D. Depression, anxiety, and stress symptoms in menopausal Arab women: shedding more light on a complex relationship. Ann. Med. Health Sci. Res. 2016;6(4):224–231. doi: 10.4103/amhsr.amhsr_341_15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen Y., Wang C., Liu Y., Yuan Z., Zhang W., Li X., Yang Y., Sun X., Xue F., Zhang C. Incident hypertension and its prediction model in a prospective northern urban Han Chinese cohort study. J. Hum. Hypertens. 2016;30(12):794–800. doi: 10.1038/jhh.2016.23. [DOI] [PubMed] [Google Scholar]
- 7.Chowdhury M.Z., Leung A.A., Sikdar K.C., O'Beirne M., Quan H., Turin T.C. Development and validation of a hypertension risk prediction model and construction of a risk score in a Canadian population. Sci. Rep. 2022;12(1) doi: 10.1038/s41598-022-16904-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chowdhury M.Z., Leung A.A., Walker R.L., Sikdar K.C., O'Beirne M., Quan H., Turin T.C. A comparison of machine learning algorithms and traditional regression-based statistical modeling for predicting hypertension incidence in a Canadian population. Sci. Rep. 2023;13(1):13. doi: 10.1038/s41598-022-27264-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Deng X., Hou H., Wang X., Li Q., Li X., Yang Z., Wu H. Development and validation of a nomogram to better predict hypertension based on a 10-year retrospective cohort study in China. Elife. 2021;10 doi: 10.7554/eLife.66419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Farhadi F., Aliyari R., Ebrahimi H., Hashemi H., Emamian M.H., Fotouhi A. Prevalence of uncontrolled hypertension and its associated factors in 50–74 years old Iranian adults: a population-based study. BMC Cardiovasc. Disord. 2023;23(1) doi: 10.1186/s12872-023-03357-x. 1-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fuchs F.D., Whelton P.K. High blood pressure and cardiovascular disease. Hypertension. 2020;75(2):285–292. doi: 10.1161/HYPERTENSIONAHA.119.14240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gupta R., Xavier D. Hypertension: the most important non communicable disease risk factor in India. Indian Heart J. 2018;70(4):565–572. doi: 10.1016/j.ihj.2018.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hannan J.A., Commodore‐Mensah Y., Tokieda N., Smith A.P., Gawlik K.S., Murakami L., Cooper J., Koob S., Wright K.D., Cassarino D., Arslanian‐Engoren C. Improving hypertension control and cardiovascular health: an urgent call to action for nursing. Worldviews Evidence-Based Nurs. 2022;19(1):6–15. doi: 10.1111/wvn.12560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hasan M., Sutradhar I., Akter T., Das Gupta R., Joshi H., Haider M.R., Sarker M. Prevalence and determinants of hypertension among adult population in Nepal: data from Nepal Demographic and Health Survey 2016. PLoS One. 2018;13(5) doi: 10.1371/journal.pone.0198028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hong W.S., Zhang Y.X., Lin Q., Sun Y. Risk factors analysis and the establishment of nomogram prediction model of hidden blood loss after total hip arthroplasty for femoral neck fracture in elderly women. Clin. Interv. Aging. 2022:707–715. doi: 10.2147/CIA.S363682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Do Nam K., Van N.B., Hoang L.V., Duc T.P., Ha T.T., Tuan V.T., Dinh P.P., Thu H.T., Show P.L., Nga V.T., Chu D.T. Hypertension in a mountainous province of Vietnam: prevalence and risk factors. Heliyon. 2020;6(2) doi: 10.1016/j.heliyon.2020.e03383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hossain F.B., Adhikary G., Chowdhury A.B., Shawon M.S. Association between body mass index (BMI) and hypertension in south Asian population: evidence from nationally-representative surveys. Clinical hypertension. 2019;25(1):1–9. doi: 10.1186/s40885-019-0134-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Iqbal A., Ahsan K.Z., Jamil K., Haider M.M., Khan S.H., Chakraborty N., Streatfield P.K. Demographic, socioeconomic, and biological correlates of hypertension in an adult population: evidence from the Bangladesh demographic and health survey 2017–18. BMC Publ. Health. 2021;21(1):1229. doi: 10.1186/s12889-021-11234-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Islam M.M., Rahman M.J., Menhazul Abedin M., Ahammed B., Ali M., Ahmed N.F., Maniruzzaman M. Identification of the risk factors of type 2 diabetes and its prediction using machine learning techniques. Health Systems. 2022:1–2. doi: 10.1080/20476965.2022.2141141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Islam M.M., Rahman M.J., Roy D.C., Maniruzzaman M. Automated detection and classification of diabetes disease based on Bangladesh demographic and health survey data, 2011 using machine learning approach. Diabetes Metabol. Syndr.: Clin. Res. Rev. 2020;14(3):217–219. doi: 10.1016/j.dsx.2020.03.004. [DOI] [PubMed] [Google Scholar]
- 21.Islam M.M., Rahman M.J., Roy D.C., Tawabunnahar M., Jahan R., Ahmed N.F., Maniruzzaman M. Machine learning algorithm for characterizing risks of hypertension, at an early stage in Bangladesh. Diabetes Metabol. Syndr.: Clin. Res. Rev. 2021;15(3):877–884. doi: 10.1016/j.dsx.2021.03.035. [DOI] [PubMed] [Google Scholar]
- 22.Islam S.M., Talukder A., Awal M., Siddiqui M., Umer M., Ahamad M., Ahammed B., Rawal L.B., Alizadehsani R., Abawajy J., Laranjo L. Machine learning approaches for predicting hypertension and its associated factors using population-level data from three south asian countries. Frontiers in Cardiovascular Medicine. 2022;9:762. doi: 10.3389/fcvm.2022.839379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Khan M.N., Oldroyd J.C., Chowdhury E.K., Hossain M.B., Rana J., Renzetti S., Islam R.M. Prevalence, awareness, treatment, and control of hypertension in Bangladesh: findings from national demographic and health survey, 2017–2018. J. Clin. Hypertens. 2021;23(10):1830–1842. doi: 10.1111/jch.14363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim J.G., Park S.M., Kim H.J., Yeom J.S. Development and validation of a risk-prediction nomogram for chronic low back pain using a national health examination survey: a cross-sectional study. Healthcare (Basel) 2023;11(4):468. doi: 10.3390/healthcare11040468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li J., Qiang W.M., Wang Y., Wang X.Y. Development and validation of a risk assessment nomogram for venous thromboembolism associated with hospitalized postoperative Chinese breast cancer patients. J. Adv. Nurs. 2021;77(1):473–483. doi: 10.1111/jan.14571. [DOI] [PubMed] [Google Scholar]
- 26.Li N., Zhan S., Liu C., Li T., Tu T., Chen B., He Y., Chen M., Zeng Z., Zhuang X. Development and validation of a nomogram to predict indolent course in patients with ulcerative colitis: a single-center retrospective study. Gastroenterology Report. 2022;10 doi: 10.1093/gastro/goac029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Liu Q., Yuan J., Bakeyi M., Li J., Zhang Z., Yang X., Gao F. Development and validation of a nomogram to predict type 2 diabetes mellitus in overweight and obese adults: a prospective cohort study from 82938 adults in China. International Journal of Endocrinology. 2020;2020:1–9. doi: 10.1155/2020/8899556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mills K.T., Stefanescu A., He J. The global epidemiology of hypertension. Nat. Rev. Nephrol. 2020;16(4):223–237. doi: 10.1038/s41581-019-0244-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.National Institute of Population Research and Training (NIPORT), and ICF . NIPORT and ICF; Dhaka, Bangladesh, and Rockville, Maryland, USA: 2020. Bangladesh Demographic and Health Survey 2017-18. [Google Scholar]
- 30.Committee Members, Cheitlin M.D., Armstrong W.F., Aurigemma G.P., Beller G.A., Bierman F.Z., Davis J.L., Douglas P.S., Faxon D.P., Gillam L.D., Kimball T.R. ACC/AHA/ASE 2003 guideline update for the clinical application of echocardiography: summary article: a report of the American college of Cardiology/American heart association task force on practice guidelines (ACC/AHA/ASE committee to update the 1997 guidelines for the clinical application of echocardiography) Circulation. 2003;108(9):146–1162. doi: 10.1161/01.CIR.0000073597.57414.A9. [DOI] [PubMed] [Google Scholar]
- 31.Whelton P.K., Carey R.M., Aronow W.S., Casey D.E., Collins K.J., Dennison Himmelfarb C., DePalma S.M., Gidding S., Jamerson K.A., Jones D.W., MacLaughlin E.J. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2018;71(19):e127–e248. doi: 10.1016/j.jacc.2017.11.006. [DOI] [PubMed] [Google Scholar]
- 32.Iqbal A., Ahsan K.Z., Jamil K., Haider M.M., Khan S.H., Chakraborty N., Streatfield P.K. Demographic, socioeconomic, and biological correlates of hypertension in an adult population: evidence from the Bangladesh demographic and health survey 2017–18. BMC Publ. Health. 2021;21(1):1229. doi: 10.1186/s12889-021-11234-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Montagna S., Pengo M.F., Ferretti S., Borghi C., Ferri C., Grassi G., Muiesan M.L., Parati G. Machine learning in hypertension detection: a study on World Hypertension Day data. J. Med. Syst. 2022;47(1):1. doi: 10.1007/s10916-022-01900-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Biswas R.K., Chowdhury S., Hossain S., Chowdhury P.B. Hypertension, diabetes, and hypercholesterolemia in Bangladesh: evaluating role of physical activity from cross‐sectional STEPS 2018 survey. Health Science Reports. 2024;7(7) doi: 10.1002/hsr2.2243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Oliveros E., Patel H., Kyung S., Fugar S., Goldberg A., Madan N., Williams K.A. Hypertension in older adults: assessment, management, and challenges. Clin. Cardiol. 2020;43(2):99–107. doi: 10.1002/clc.23303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ouyang F., Cheng X., Zhou W., He J., Xiao S. Increased mortality trends in patients with chronic non-communicable diseases and comorbid hypertension in the United States, 2000–2019. Front. Public Health. 2022;10 doi: 10.3389/fpubh.2022.753861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rahman M., Zaman M.M., Islam J.Y., Chowdhury J., Ahsan H.N., Rahman R., Hassan M., Hossain Z., Alam B., Yasmin R. Prevalence, treatment patterns, and risk factors of hypertension and pre-hypertension among Bangladeshi adults. J. Hum. Hypertens. 2018;32(5):334–348. doi: 10.1038/s41371-017-0018-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rahman M.A., Parvez M., Halder H.R., Yadav U.N., Mistry S.K. Prevalence of and factors associated with prehypertension and hypertension among Bangladeshi young adults: an analysis of the Bangladesh Demographic and Health Survey 2017–18. Clinical Epidemiology and Global Health. 2021;12 [Google Scholar]
- 39.Rapsomaniki E., Timmis A., George J., Pujades-Rodriguez M., Shah A.D., Denaxas S., White I.R., Caulfield M.J., Deanfield J.E., Smeeth L., Williams B. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1·25 million people. Lancet. 2014;383(9932):1899–1911. doi: 10.1016/S0140-6736(14)60685-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Roth G.A., Mensah G.A., Johnson C.O., Addolorato G., Ammirati E., Baddour L.M., Barengo N.C., Beaton A.Z., Benjamin E.J., Benziger C.P., Bonny A. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J. Am. Coll. Cardiol. 2020;76(25):2982–3021. doi: 10.1016/j.jacc.2020.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sathi N.J., Islam M.A., Ahmed M.S., Islam S.M. Prevalence, trends and associated factors of hypertension and diabetes mellitus in Bangladesh: evidence from BHDS 2011 and 2017–18. PLoS One. 2022;17(5) doi: 10.1371/journal.pone.0267243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shang X., Hill E., Zhu Z., Liu J., Ge B.Z., Wang W., He M. The association of age at diagnosis of hypertension with brain structure and incident dementia in the UK Biobank. Hypertension. 2021;78(5):1463–1474. doi: 10.1161/HYPERTENSIONAHA.121.17608. [DOI] [PubMed] [Google Scholar]
- 43.Sharma S., Singh H., Mehta K., Verma M., Goel S. Hypertension and its association with body mass index among the Indian population. Findings from a nationwide survey (NFHS-4), 2015-16. J. Fam. Med. Prim. Care. 2022;11(9):5826–5833. doi: 10.4103/jfmpc.jfmpc_168_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Singh S., Shankar R., Singh G.P. Prevalence and associated risk factors of hypertension: a cross-sectional study in urban Varanasi. Int. J. Hypertens. 2017;2017 doi: 10.1155/2017/5491838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Xu Y., Liu J., Wang J., Fan Q., Luo Y., Zhan H., Tao N., You S. Establishment and verification of a nomogram prediction model of hypertension risk in Xinjiang Kazakhs. Medicine. 2021;100(42) doi: 10.1097/MD.0000000000027600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wang Y., Zhang Y., Ni B., Jiang Y., Ouyang Y. Development and validation of a depression risk prediction nomogram for US Adults with hypertension, based on NHANES 2007–2018. PLoS One. 2023;18(4) doi: 10.1371/journal.pone.0284113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wu Y., Tan W., Liu Y., Li Y., Zou J., Zhang J., Huang W. Development and validation of a nomogram prediction model for hypertension-diabetes comorbidity based on chronic disease management in the community. Lipids Health Dis. 2023;22(1):135. doi: 10.1186/s12944-023-01904-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yang L., Shen X., Seyiti Z., Tang J., Kasimujiang A., Dejite T., Zhao L., Shan X.F., Gao X.M. Development and validation of a nomogram for predicting all-cause mortality in American adult hypertensive populations. Front. Pharmacol. 2023;14 doi: 10.3389/fphar.2023.1266870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Xu Y., Shi Z., Sun D., Munivrana G., Liang M., István B., Radak Z., Baker J.S., Gu Y. Establishment of hypertension risk nomograms based on physical fitness parameters for men and women: a cross-sectional study. Frontiers in cardiovascular medicine. 2023;10 doi: 10.3389/fcvm.2023.1152240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Talukder A., Hossain M.Z. Prevalence of diabetes mellitus and its associated factors in Bangladesh: application of two-level logistic regression model. Sci. Rep. 2020;10(1) doi: 10.1038/s41598-020-66084-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tasin I., Nabil T.U., Islam S., Khan R. Diabetes prediction using machine learning and explainable AI techniques. Healthc. Technol. Lett. 2023;10:1–10. doi: 10.1049/htl2.12039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Vickers A.J., van Calster B., Steyerberg E.W. A simple, step-by-step guide to interpreting decision curve analysis. Diagnostic and prognostic research. 2019;3(1):1–8. doi: 10.1186/s41512-019-0064-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wang C., Yuan Y., Zheng M., Pan A.N., Wang M., Zhao M., Li Y., Yao S., Chen S., Wu S., Xue H. Association of age of onset of hypertension with cardiovascular diseases and mortality. J. Am. Coll. Cardiol. 2020;75(23):2921–2930. doi: 10.1016/j.jacc.2020.04.038. [DOI] [PubMed] [Google Scholar]
- 54.Wu S., Xu Y., Zheng R., Lu J., Li M., Chen L., Huo Y., Xu M., Wang T., Zhao Z., Wang S. Hypertension defined by 2017 ACC/AHA guideline, ideal cardiovascular health metrics, and risk of cardiovascular disease: a nationwide prospective cohort study. The Lancet Regional Health–Western Pacific. 2022;20 doi: 10.1016/j.lanwpc.2021.100350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wu W., Zhang B., Li D., Yan M., Deng Q., Kang Y., Du J., Gao X., Yan H. Development and validation of nomogram for prediction of low birth weight: a large-scale cross-sectional study in northwest China. J. Matern. Fetal Neonatal Med. 2022;35(25):7562–7570. doi: 10.1080/14767058.2021.1956457. [DOI] [PubMed] [Google Scholar]
- 56.Xu H., Zhao X., Shi Y., Li X., Qian Y., Zou J., Yi H., Huang H., Guan J., Yin S. Development and validation of a simple-to-use clinical nomogram for predicting obstructive sleep apnea. BMC Pulm. Med. 2019;19:1–8. doi: 10.1186/s12890-019-0782-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yan C., Zheng Y., Zhang X., Gong C., Wen S., Zhu Y., Jiang Y., Li X., Fu G., Pan H., Teng M. Development and validation of a nomogram model for predicting unfavorable functional outcomes in ischemic stroke patients after acute phase. Front. Aging Neurosci. 2023;15 doi: 10.3389/fnagi.2023.1161016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zhou B., Perel P., Mensah G.A., Ezzati M. Global epidemiology, health burden and effective interventions for elevated blood pressure and hypertension. Nat. Rev. Cardiol. 2021;18(11):785–802. doi: 10.1038/s41569-021-00559-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wang H, Liu X, Long J, Huang J, Lyu S, Zhao X, Zhao B, He Q, An Z, Hao J. Development and validation of a nomogram predictive model for colorectal adenoma with low-grade intraepithelial neoplasia using routine laboratory tests: a single-center case-control study in China. Heliyon. e20996. 202;9(11). [DOI] [PMC free article] [PubMed]
- 60.Khanam R., Ahmed S., Rahman S., Al Kibria G.M., Syed J.R., Khan A.M., Moin S.M., Ram M., Gibson D.G., Pariyo G., Baqui A.H. Prevalence and factors associated with hypertension among adults in rural Sylhet district of Bangladesh: a cross-sectional study. BMJ Open. 2019;9(10) doi: 10.1136/bmjopen-2018-026722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Li G., Wang H., Wang K., Wang W., Dong F., Qian Y., Gong H., Hui C., Xu G., Li Y., Pan L. The association between smoking and blood pressure in men: a cross-sectional study. BMC Publ. Health. 2017;17:1–6. doi: 10.1186/s12889-017-4802-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Rahman M.A., Halder H.R., Yadav U.N., Mistry S.K. Prevalence of and factors associated with hypertension according to JNC 7 and ACC/AHA 2017 guidelines in Bangladesh. Sci. Rep. 2021;11:1–10. doi: 10.1038/s41598-021-94947-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data or code will be made available on request.